Abstract
On December 31, 2019, the Chinese government announced an outbreak of a novel coronavirus, recently named COVID‐19. During the following weeks the international medical community has witnessed with unprecedented coverage the public health response both domestically by the Chinese government, and on an international scale as cases have spread to dozens of countries. While much regarding the virus and the Chinese public health response is still unknown, national and public health institutions globally are preparing for a pandemic. As cases and spread of the virus grow, emergency and other front‐line providers may become more anxious about the possibility of encountering a potential case. This review describes the tenets of a public health response to an infectious outbreak by using recent historical examples and also by characterizing what is known about the ongoing response to the COVID‐19 outbreak. The intent of the review is to empower the practitioner to monitor and evaluate the local, national and global public health response to an emerging infectious disease.
1. INTRODUCTION
Since the December 31, 2019 report of 44 cases of “pneumonia of unknown etiology” by national authorities in China to the World Health Organization (WHO), over 30,000 cases of coronavirus disease 2019 (COVID 19, formerly 2019 novel Coronavirus or 2019‐nCoV) have been confirmed. 1 , 2 While the virus’ behavior, clinical features, and management have been described in reports elsewhere, less has been done to detail the public health response to the crisis. Mimicking the rapid spread of the virus, the hourly expansion of misinformation on television, news reports, and social media have obscured the actual communication by international health authorities to medical professionals and the wider public. 3 While the health community mobilizes to contain the virus, emergency providers outside China have a duty to address the growing public fear with accepted principles of public health. To do so, we must understand the expected progression of the response to an outbreak.
This review is intended to parse through the ever‐evolving details of the COVID‐19 crisis and explain the expected evolution of the international public health response. We look back at past pandemics, their economic and societal impacts, the players in a public health response to address such a crisis, and how those tools are being utilized in the COVID‐19 outbreak.
2. PAST PANDEMICS AND THEIR IMPACT
2.1. Looking back: a review of SARS‐2003
To better understand the current novel coronavirus outbreak as well as the robust Chinese public health response, it is useful to examine the initial local and national reactions to the 2003 Severe Acute Respiratory Syndrome (SARS) coronavirus outbreak. The apparent index case starting the SARS epidemic was reported in Guangdong Province, a coastal province in South China, in November 2002. After a local government official became ill, then succumbed to the infection, several other cases were reported in surrounding cities. 4
In mid‐December 2002, local health authorities took notice, followed by rapid notification of the provincial government and the national Ministry of Health by January 2003. Initial investigative reports of the outbreak were marked “top secret” and could only be opened by high‐ranking officials. No public notifications had been made at this point and no mention was made of the outbreak in the news media until at least February 2003. This “fatal period of hesitation” led to wide‐spread speculation and fear among the local population and rumors of a “deadly flu” began to spread, undermining public trust in the government's response. Even following initial news conferences describing the outbreak, government officials continued to minimize the risks of the outbreak. Not until April 2003 did the Chinese Center for Disease Control and Prevention (CDC) issue a nationwide bulletin on preventing spread of the illness, by which time outbreaks had already occurred in Hong Kong, Vietnam, Singapore, and Toronto, Canada, among others.
Once mobilized, the Chinese public health machine was able to quickly control and ultimately eliminate the outbreak within a year. 5 It remains unclear how much damage could have been avoided had the Chinese government been able and willing to communicate accurate outbreak data in a transparent and timely manner. One of the most striking features of the current COVID‐19 outbreak are the reports of detainment of journalists, threats to whistleblowers, punishment of government officials, and deletion of social media posts in apparent efforts to control the image of the outbreak. This has contributed to a widespread distrust of the communications by the Chinese government and public health officials reminiscent of the SARS epidemic. 6
2.2. The health care, economic, and social impact of a pandemic
As illustrated by the SARS epidemic, outbreaks have impacts beyond the immediate effects of case fatality. They set into motion broader and indirect health consequences, short‐ and long‐term economic impacts, and social disturbances which are far‐reaching and predictable.
2.2.1. The impact on health care
During the initial period of outbreak, health care resources are often diverted away from providing routine care and shifted to outbreak management. During the 2014–2015 Ebola crisis in West Africa, the health care systems of Liberia, Sierra Leone, and Guinea resulted in a reduction in the ability to provide routine care for HIV/AIDS, malaria, and tuberculosis. 7 One author estimated this reduction in services cost >10,600 additional lives, rivaling the total death toll due to Ebola of the 3 countries combined. 8 , 9 Although some of this increased mortality is likely due to the limitations of health care in that region, an issue not shared by China, developed nations are also at risk for indirect increases in mortality. During the 2009 H1N1 influenza pandemic, US‐based emergency departments saw surges in visits. Despite a lack of increased admissions, study hospitals still experienced statistically a higher number of inpatient deaths attributable to stroke and myocardial infarction. 10
2.2.2. The economic impact
The SARS outbreak ultimately led to >700 deaths, affected 37 countries and resulted in an estimated cost to the world economy of US$40 billion. 7 , 8 While the full extent of its impact remains to be seen, the COVID‐19 will have short term financial impacts primarily derived from the cost of sentinel case identification and containment. Additional personnel hours are needed to isolate infectious cases and implement effective case tracing. Bedside care of these cases expends disposable medical dollars (medications, single‐use personal protective equipment and care delivery items). Yet these direct costs pale in comparison to indirect economic expenditures. In 2015, the World Bank estimated that the 3 Ebola epicenter countries experienced a loss of >US$1.6 billion which reflected 12% of their gross domestic product (GDP). Low‐ and middle‐income countries (LMIC) have decreased ability to maintain tax revenue streams during stalled economic activity and government implemented curfews and quarantines, although it is yet unclear if this will apply to a high‐income country like China. 9 Neighboring LMICs to an epidemic will likely experience economic stunting. Despite not having a single confirmed case of Ebola, The Gambia reported a 65% reduction in hotel bookings and a cancelation of 50% of inbound planes. 11 However, high income countries are not totally immune to fiscal shocks during outbreaks. Despite hospitalizing only 186 people, the Middle East respiratory syndrome (MERS) coronavirus cost the Republic of Korea >US$2.6 billion in lost tourism wages. 12 Economic fallout will likely be tangible worldwide, as 2018 data indicates China has the world's second largest economy, with a GDP of >US$13.6 trillion, 16% of the global economy. 13
2.2.3. The societal impact
There is a large penumbra of social capital at risk during the COVID‐19 outbreak. Public health emergencies splash constantly across news headlines and social media platforms. In a positive sense, researchers have demonstrated the ability to harness this open source information and created an entire field called “digital epidemiology.” Twitter data has been used to track surveillance for outbreaks and responses to interventions. 14 Alternatively, misinformation, perceived versus actual risk and fear‐based communication strategies can become normative. The recent Zika emergency revealed that repetitive exposures to media messages can demonstrably augment fear. 15 This fear may lead to palpable changes in behavior patterns. Retrospective analysis of prior outbreaks shows both over‐ and under‐reaction to health information. In response to alarm‐based messaging the populace has both mass‐exited and not complied with quarantines, burdened and underutilized health systems, and ignored and demanded extraordinary precautionary measures. Locations and people groups that are low risk for being threats experience fallout and social ostracism. 16 The COVID‐19 has followed suit with accounts of uninformed acts of racism against French Asians, detainments of 6000 cruise ship passengers, airline route suspensions, and country border closures. 17 , 18 , 19 On February 2nd, the WHO released a situation report stating they are in a fight against an “infodemic” (overabundance of information of varying accuracy) and will utilize multiple media platforms to inform the public. 20
3. THE PUBLIC HEALTH RESPONSE
3.1. Players in a public health response
The global public health response is less a structured hierarchy than a complex web of organizations with specific roles working together to address specific issues. 21 Table 1 and Figure 1 detail the primary roles of some key stakeholders, and illustrate their interactions.
TABLE 1.
Global health governance
| Organization | COVID‐19 outbreak role |
|---|---|
| Global | |
| World Health Organization 22 |
|
| National/Regional | |
|
China Center for Disease Control and Prevention 23 (Chinese NPHI a ) |
|
|
United States Center for Disease Control and Prevention 24 (U.S.A. NPHI) |
|
|
European Center for Disease Control and Prevention 25 (NPHI for European Union States) |
|
| Non‐governmental/philanthropic | |
| Non‐governmental organizations providing emergency response care such as Medecins San Frontieres | No defined role in this outbreak |
| Philanthropic foundations such as Gates Foundation or individual contributors | Research and development grants |
Key stakeholders and their role in the COVID‐19 outbreak.
National Public Health Institute. PUI: persons under investigation.
FIGURE 1.
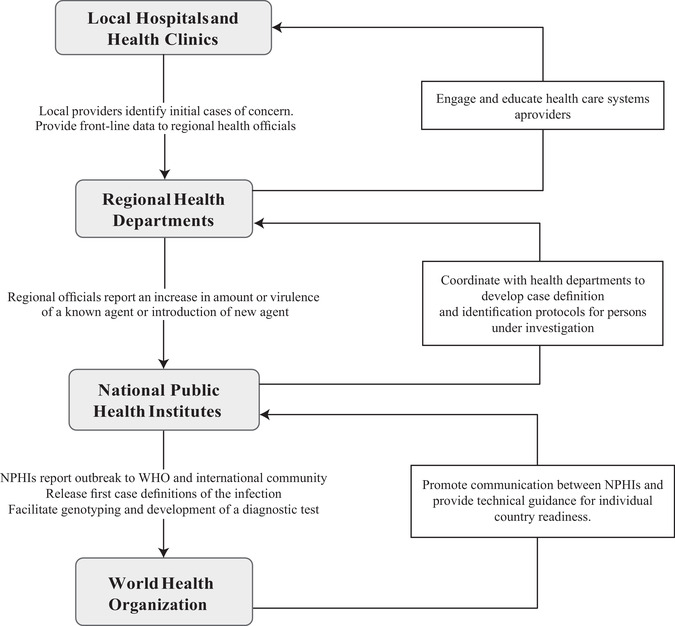
Progression of a global health response
3.1.1. The World Health Organization
The WHO, an agency of the United Nations and empowered by the International Health Regulations 2005 (IHR 2005), serves as the primary international body coordinating the public health response to major multi‐national outbreaks. The IHR 2005 is a legally binding international treaty signed by all WHO members compelling governments and allowing non‐governmental organizations to report outbreaks to the WHO, and compelling states to take an active role in disease surveillance. 21 The WHO functions as a central repository and conduit for information about new diseases and outbreaks, releasing updates, and providing urgent international expertise through its Global Outbreak Alert and Response Network (GOARN). 27 A given outbreak may then be declared a Public Health Emergency of International Concern (PHEIC), which “constitutes a public health risk to other states and potentially requires an international response” and serves as a call to urgent action, international expertise, attention, and funding, though these are not legally bound as with the IHR. 27 , 28 , 29
3.1.2. National public health institutes
National public health institutes (NPHI) perform many of the practical functions of surveillance and containment in public health and function independently of any international organization, but NPHIs communicate voluntarily with the WHO for the purpose of monitoring and surveillance. 30 In the case of COVID‐19, the Chinese CDC has functioned as the NPHI involved in the crisis.
3.1.3. United States CDC
The U.S. CDC, as with other national governmental bodies, has the explicit goal of preventing sustained outbreaks like COVID‐19 within the borders of its own country, but also contributes significantly to ongoing publicly shared research in disease transmission, diagnostics, vaccine development, and therapeutics, as well as by offering guidelines to front‐line clinicians, and coordinating with both the WHO and local health departments. 31
3.1.4. Government ministries and non‐governmental organizations
Government agencies such as departments of health, defense, and immigration are often involved in investigation, vaccination, diagnosis, traveler screening, enforcing travel restrictions or quarantine, and logistics support.
With a large number of stakeholders and the WHO functioning as more of a network and data conduit, a certain amount of decentralization is inevitable. This decentralization, as well as inherent uncertainty, fear, and potential mistrust of government officials by the public (or by individual governments towards international bodies) in the early days of a public health emergency requires significant transparency to build trust and allow collaboration. 21 , 32 Officials and agencies must fully disclose what is, and what is not, known about a public health emergency to facilitate the most robust yet proportionate response. There are often no clear incentives for states to declare epidemics, and governments already struggling to meet the long‐term needs of citizens and facing trade limitations or damage to their tourist industries may be hesitant to do so, further underscoring the need for transparency. 29 , 33
3.2. Strategies in a public health response
3.2.1. Identifying and characterizing an outbreak
The process of establishing the existence of an outbreak begins with the report of a cluster of cases that is unusual in incidence, location, or in relation to each other. 34 The report is followed by implementation of a plan. Outcomes improve when countries have a pandemic plan and move quickly to establish protocols that limit the spread of an outbreak. 35 These include establishing case definitions, designating persons under investigation (PUI), pursuit of diagnostic tests, continuing incidence surveillance, and characterization of morbidity and case fatality rate (CFR). These key characteristics for COVID‐19 are listed in Table 2.
TABLE 2.
Characteristics of COVID‐19 outbreak
| Element | COVID‐19 outbreak | |
|---|---|---|
|
Case definition (confirmed case) |
Positive diagnostic test (PCR of viral mRNA) in a PUI | |
| Person under investigationa (PUI) |
Clinical features Fever and/or signs/symptoms of respiratory illness |
Epidemiologic risk
|
| Incubation period | 2‐14 days | |
| Mode of transmission |
Origin: possibly bats in Wuhan food market Person‐to‐person spread: likely via droplets Areas of investigation: airborne transmission, fomite duration, and other modes of transmission |
|
| Incidence |
>30,000 persons in >25 countries 2 confirmed Some estimates >75,000 cases 38 |
|
| Case fatality rate |
∼20% with severe disease ∼0.18% to 4% estimated overall CFR 36 ∼15% CFR in hospitalized patients 36 |
|
A person under investigation is a patient who meets criteria for diagnostic testing. Level of epidemiologic risk inherent in exposure determines the number of clinical features required to constitute a PUI. See CDC guidelines for up‐date information regarding PUI: https://www.cdc.gov/coronavirus/ COVID‐19/hcp/clinical‐criteria.html
Determining the criteria for a PUI is a particular concern for emergency and other frontline medical providers. A patient who meets criteria for a PUI should initiate hospital protocols for infection control, provider PPE donning/doffing protocols, and immediate notification of state or other relevant public health entities for guidance in diagnostic testing and management. Patients who do not meet these criteria generally can forgo quarantine and testing at the provider and public health officials’ discretion. The current CDC criteria for PUI are updated regularly on their website: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html.
Knowing the contagiousness of an infectious disease can aid with predicting its transmission and spread. Epidemiologists use the term R0 to indicate the number of people who are at risk for infection from a single infected individual. Epidemics become controlled when the R0 for a disease falls below 1. The R0 for COVID‐19 has been estimated at 1.4–2.7. 36 , 37 , 38 By comparison the R0 for SARS was 3 and MERS was considered to be <1.
3.2.2. Containing an outbreak
Containment of past outbreaks such as SARS and Ebola has relied on the traditional public health strategies of evaluation of persons under investigation (those suspected but not confirmed of having the disease), exposure mapping or contact tracing, isolating and treating affected patients, and potentially quarantining those exposed but not symptomatic. 35 , 40 The unusually long incubation period (median 5.2 days, IQR 4.1–7, with 95th percentile at 12.5 days) has led to the WHO and CDC recommendation to quarantine certain individuals exposed to asymptomatic persons with potential COVID‐19 for up to 14 days after exposure. 36 The recommendations have informed the decisions by multiple NPHIs to quarantine returned travelers in government facilities and to quarantine cruise ship passengers onboard multiple vessels. 41 , 42
Rapid, specific, reliable, and inexpensive diagnostics, as well as vaccines and targeted anti‐virals, are also likely to be very helpful. 33 If and when vaccines become available, public health officials employ a concept called ring vaccination where priority is given to people living within a preset radius of the outbreak epicenter. 41 However, even when vaccines have been developed before an outbreak occurs, there are often insufficient quantities or import restrictions limiting distribution. Significant progress was made in the rapid development of an efficacious Ebola virus vaccine, leading to the creation of a research and development blueprint that will theoretically improve research and development of new vaccines to emerging infectious diseases such as COVID‐19. 40 , 42 While research is ongoing for effective antiviral medications, public health entities may also pursue compassionate use of existing antiviral medications. Examples of this include the use of remdesivir in the United States and lopinavir/ritonavir in Asia. 43 , 44 , 45 See Table 3 for further discussion of public health interventions.
TABLE 3.
Typical public health strategies for epidemic containment
| Strategy | COVID‐19 response |
|---|---|
| Symptom screening |
Airport temperature measurements 46 Drone‐equipped thermal cameras 47 Emergency department and clinic triage screening 48 |
| Quarantine |
Wuhan city‐wide quarantine 49 Maritime and cruise ship quarantine 50 U.S. military base quarantine 51 |
| Travel restrictions |
Russia and Hong Kong border closure 52 Airline cancellations 53 Traveler evacuations from Hubei Province 54 |
| Future considerations |
Vaccine research and development 55 Ring vaccination program Use and development of Antivirals 56 |
4. THE INITIAL COVID‐19 PUBLIC HEALTH RESPONSE
On January 30, 2020 the World Health Organization (WHO) took the “last resort” step of declaring a PHEIC, only the 6th time the WHO has been galvanized to take such an action. 57 The announcement came amid reports of evacuation, lockdown, quarantine, travel restrictions and international border closures. The COVID‐19 has demonstrated the challenges and successes when applying these public health principles to an ongoing crisis.
4.1. Challenges in the COVID‐19 public health response
Shortcomings often emerge in the first few weeks of an outbreak and have emerged in COVID‐19 pandemic. 58 Incomplete or poorly communicated preliminary data may hamper the national and international response. For example, the relatively low CFR rate (∼2% compared to >60% in Ebola Virus cases, >30% in MERS‐CoV cases, and >9% in SARS‐CoV cases) raises concerns for subclinical and unreported infections. 59 This restricts public health officials’ ability to determine whether this ongoing Chinese epidemic (widespread disease transmission within a nation) has yet made the jump to a pandemic (widespread disease transmission occurring in multiple nations). Similarly, the competence of the Chinese CDC in identifying the outbreak and implementing rapid control measures is threatened by reports of “narrative controlling” preventing effective communication between frontline practitioners and the global outbreak response. 60 In an outbreak that seems to change hourly, a delay of days or weeks diminishes the responders’ ability to truly assess the impact, transmissibility, extent of spread, and virulence of the disease. As such, much of the characterizations of COVID‐19 should be understood as preliminary and subject to change as data becomes more readily available.
These persistent knowledge gaps regarding the outbreak remain concerning. The European Center for Disease Prevention and Control (ECDC) rapid risk assessment publication on January 22, 2020 points out that “in the absence of detailed information from the ongoing outbreak investigations in China, it is not possible to quantify the extent of human‐to‐human transmission.” A similar concern exists regarding the Chinese algorithm for testing, case definitions, means of identifying PUIs, or surveillance of contacts. 61 Without this information it remains difficult for NPHIs to determine specific risk of transmission, quantify virulence, or estimate CFR with any certainty. Some of the more extreme policies enacted by individual governments may stem from this deficit in effective communication and transparency.
In addition to a lack of transparency, some experts have also called into question the specific measures employed by the Chinese government. A recent review of the efficacy of travel checkpoint temperature screening during the Ebola Virus and SARS outbreaks revealed that no cases were identified by these measures. 62 The complete lockdown of the city of Wuhan is an unprecedented intervention, and its efficacy will be of great interest to the public health community.
4.2. Successes in the COVID‐19 public health response
There are some improvements in the Chinese response to the crisis as compared to prior public health events. In contrast to the decisions made by Chinese health authorities and government officials during the 2003 SARS outbreak, the existence of the initial patient cluster was rapidly reported to the WHO China Office in December 2019, with a novel coronavirus being identified by early January 2020. The speed of cluster identification and pathogen isolation is likely due to additional investment in public health resources and infrastructure by China's CDC. 8 The Chinese government has demonstrated commitment to controlling spread of the virus, including closure of the seafood market in Wuhan, cessation of public transport, screening at travel checkpoints, travel restrictions, closure of cultural landmarks and businesses, and cancellation of the Lunar New Year celebrations. 61 , 63 Media sources and inhabitants of Wuhan have described the situation as “complete lockdown” in a city of >11 million people, representing an “unprecedented public health intervention.” 61
5. CONCLUSION
As hospital systems and emergency departments monitor and prepare for the COVID‐19 outbreak, there are still many unanswered questions. The situation is dynamic with cases identified nearly hourly. The stakes are high, as the CFR and morbidity of the virus appears to be higher than influenza. The extent of media coverage regarding this outbreak means that the management of any cases identified outside of China will be heavily scrutinized both regarding disease‐related outcomes and the adherence to public health guidelines for protection of the larger population. It is imperative that providers are familiar with the public health considerations of encountering a person under investigation or confirmed case. To this end, providers should take care to consume accurate and timely information to inform their respective institution's triage and treatment practices. For links to updated guidelines please see Appendix A. While progression to a pandemic may not be inevitable, emergency and other front‐line medical providers have an obligation to stand in readiness.
CONFLICT OF INTEREST
None to disclose.
Biography
Christopher Greene, MD, MPH, is Assistant Professor and Fellowship Director, Global Health and International Emergency Medicine, at the University of Alabama at Birmingham.
APPENDIX A. RESOURCES FOR PROVIDERS
A.1.
CDC Guidelines for Healthcare Professionals: https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html
WHO technical guidelines for Healthcare Professionals: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
Up to date case map from Johns Hopkins University: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
Greene CJ, Burleson SL, Crosby JC, Heimann MA, Pigott DC. Coronavirus disease 2019: International public health considerations. JACEP Open 2020;1:70–77. 10.1002/emp2.12040
Meeting: None to disclose.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Henry E. Wang, MD, MS.
REFERENCES
- 1. World Health Organization . Situation Report 1. Novel Coronavirus (2019‐nCoV). https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf. Published January 21, 2020. Accessed February 3, 2020.
- 2. 2019‐nCoV Global Cases by Johns Hopkins CSSE . https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed February 3, 2020.
- 3. Neporent L. Hashtag medicine: coronavirus fear goes viral on social media. Medscape Medical News. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf Published January 31, 2020. Accessed February 3, 2020. [Google Scholar]
- 4. Zhao Z, Zhang F, Xu M, et al. Description and clinical treatment of an early outbreak of severe acute respiratory syndrome (SARS) in Guangzhou, PR China. J Med Microbiol. 2003;52(Pt 8):715‐720. [DOI] [PubMed] [Google Scholar]
- 5. Huang Y. The SARS epidemic and its aftermath in China: a political perspective In: Knobler S. et al. eds. Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary. National Academies Press, 2004. [PubMed] [Google Scholar]
- 6. Ignatius D. The Coronavirus outbreak shows the vulnerability of the ‘Chinese Model.’ The Washington Post. February 4, 2020. https://www.washingtonpost.com/opinions/global-opinions/the-coronavirus-outbreak-shows-the-vulnerability-of-the-chinese-model/2020/02/04/e1213d22-4792-11ea-8124-0ca81effcdfb_story.html. Accessed February 10, 2020.
- 7. Nkengasong J. China's response to a novel coronavirus stands in stark contrast to the 2002 SARS outbreak response. Nat Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee J‐W, McKibbin WJ. In: Knobler S. et al. eds. Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary. National Academies Press, 2004; https://www.ncbi.nlm.nih.gov/books/NBK92473/ [PubMed] [Google Scholar]
- 9. Madhav N, Oppenheim B, Gallivan M, Mulembakani P, Rubin E, Wolfe N. Pandemics: risks, impacts, and mitigation In: Jamison DT, Gelband H, Horton S, et al., eds. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. Washington (DC): The International Bank for Reconstruction and Development/The World Bank; 2017. [PubMed] [Google Scholar]
- 10. Parpia AS, Ndeffo‐Mbah ML, Wenzel NS, Galvani AP. Effects of response to 2014–2015 Ebola outbreak on deaths from malaria, HIV/AIDS, and tuberculosis, West Africa. Emerg Infect Dis. 2016;22(3):433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thomas MR, Smith G, Ferreira FHG, et al. 2015. The Economic Impact of Ebola on Sub‐Saharan Africa: Updated Estimates for 2015 (English). Washington, DC: World Bank Group; http://documents.worldbank.org/curated/en/541991468001792719/The-economic-impact-of-Ebola-on-sub-Saharan-Africa-updated-estimates-for-2015 [Google Scholar]
- 12. Joo H, Maskery BA, Berro AD, Rotz LD, Lee YK, Brown CM. Economic impact of the 2015 MERS outbreak on the Republic of Korea's tourism‐related industries. Health Secur. 2019;17(2):100–108. 10.1089/hs.2018.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Bank . China Dataset. https://data.worldbank.org/country/china. Published 2018. Accessed February 1, 2020.
- 14. Towers S, Afzal S, Bernal G, et al. Mass media and the contagion of fear: the case of Ebola in America. PLoS One. 2015;10(6):e0129179. Published Jun 11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yang C, Dillard JP, Li R. Understanding Fear of Zika: personal, interpersonal, and media influences. Risk Anal. 2018;38(12):2535–2545. [DOI] [PubMed] [Google Scholar]
- 16. Blendon RJ, Benson JM, DesRoches CM, Raleigh E, Taylor‐Clark K. The public's response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38(7):925–931. [DOI] [PubMed] [Google Scholar]
- 17. BBC News . Coronavirus: French Asians hit back at racism with ‘I'm not a virus’. https://www.bbc.com/news/world-europe-51294305. Published 2020. Accessed February 1st, 2020.
- 18. USA Today . Not coronavirus: 6,000 cruise ship passengers given OK to disembark after passenger diagnosed with flu. https://www.usatoday.com/story/travel/news/2020/01/30/coronavirus-costa-cruise-ship-passengers-held-onboard-amid-tests/4618718002/. Published 2020. Accessed February 1, 2020.
- 19. NY Times . Coronavirus Live Updates: Death in Philippines Is First Outside China. https://www.nytimes.com/2020/02/02/world/asia/china-coronavirus.html. Published 2020. Accessed February 1, 2020.
- 20. WHO Situation . Novel Coronavirus (2019‐nCoV) Situation Report ‐ 13. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf?sfvrsn=195f4010_6. Published 2020. Accessed February 3, 2020.
- 21. Youde J. MERS and global health governance. International Journal: Canada's Journal of Global Policy Analysis. 2015;70(1):119‐136. [Google Scholar]
- 22. Novel Coronavirus (2019‐nCoV) . WHO website. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (Accessed February 6, 2020)
- 23. China CDC Weekly . China CDC Website http://www.chinacdc.cn/en/ (Accessed February 6, 2020)
- 24. 2019 novel coronavirus (2019‐nCoV) situation summary . CDC website https://www.cdc.gov/coronavirus/2019-nCoV/summary.html#cdc-response (Accessed February 6, 2020)
- 25. Novel coronavirus . European Center for Disease Prevention and Control website. https://www.ecdc.europa.eu/en/novel-coronavirus-china (Accessed February 6, 2020).
- 26. Guiding principles for an international outbreak alert and response . WHO website. https://www.who.int/csr/outbreaknetwork/guidingprinciples/en/. Accessed February 1, 2020.
- 27. Global Outbreak Alert and Response Network . GOARN Website https://www.who.int/ihr/alert_and_response/outbreak-network/en/ (Accessed February 1, 2020).
- 28. What are the international health regulations and emergency committees? WHO website. https://www.who.int/news-room/q-a-detail/what-are-the-international-health-regulations-and-emergency-committees (Accessed February 2, 2020).
- 29. Rull M, Kickbusch I, Lauer H. Policy debate. international responses to global epidemics: Ebola and beyond. Int Dev Pol. 6(2). [Google Scholar]
- 30. Koplan JP, Butler Jones D, Tsang T, Yu W. Public health lessons from severe acute respiratory syndrome a decade later. Emerg Infect Dis. 2013;19(6):861‐863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. 2019 novel coronavirus (2019‐nCoV) situation summary . CDC website https://www.cdc.gov/coronavirus/2019-nCoV/summary.html#cdc-response (Accessed February 1, 2020)
- 32. Gostin L, Lucy D. Middle East Respiratory Syndrome: a global health challenge. JAMA. 2015;314(8):771‐772. [DOI] [PubMed] [Google Scholar]
- 33. Knobler S, Mahmoud A, Lemon S, Mack A, Stivitz L, and Oberholtzer K, eds. Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary. Washington, DC: Institute of Medicine, National Academic Press, 2004. [PubMed] [Google Scholar]
- 34. Dicker R. Principles of Epidemiology in Public Health Practice. 3rd ed Atlanta: Centers for Disease Control and Prevention; 2004. https://www.cdc.gov/csels/dsepd/ss1978/index.html. Accessed February 3, 2020. [Google Scholar]
- 35. Azziz‐Baumgartner E, Smith N, Gonzalez‐Alvarez R, et al. National pandemic influenza preparedness planning. Influenza Other Respir Viruses. 2009;3(4):189‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China of novel coronavirus ‐ infected pneumonia. N Engl J Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mahase E. China Coronavirus: what do we know so far? BMJ. 2020;12(2):pii: E130. [DOI] [PubMed] [Google Scholar]
- 38. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019‐nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;pii:S0140‐6736(20)30260‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kieny MP. Lessons learned from Ebola vaccine R&D during a public health emergency. Hum Vaccin Immunother. 2018;14(9):2114‐2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Berlinger J, Emiko J. Diamond Princess cruise ship in Japan quarantined after passenger diagnosed with coronavirus. CNN World. 2020. https://www.cnn.com/2020/02/04/asia/coronavirus-japan-cruise-intl-hnk/index.html, Accessed February 10, 2020. [Google Scholar]
- 41. Associated Press . Nearly 200 evacuees to leave coronavirus quarantine in US. ABC News. February 11, 2020. https://abcnews.go.com/Health/wireStory/200-evacuees-leave-coronavirus-quarantine-us-68901452. Accessed February 11, 2020. [Google Scholar]
- 42. Sawari AR, Khakoo RA. Emerging diseases and antimicrobial resistance In: Markle WH, Fisher MA, Smego RA, Jr, eds. Understanding Global Health. 2nd ed New York, NY: McGraw‐Hill; 2014. [Google Scholar]
- 43. Holshude ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chan KS, Lai ST, Chu CM, et al. Treatment of SARS with lopinavir/ritonavir: a multicenter retrospective matched cohort study. Hong Kong Med J. 2003;9:399‐406. [PubMed] [Google Scholar]
- 45. Chu CM, Cheng VC, Hung IF, et al. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax. 2004;59:252–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Burton TM. U.S. expands airport screening for coronavirus; officials add risk of extensive infections is low. The Wall Street Journal. https://www.wsj.com/articles/risk-of-new-coronavirus-infections-in-u-s-is-low-health-officials-say-11580231743. Published January 29, 2020. Accessed February 7, 2020. [Google Scholar]
- 47. Mailonline TYF. China uses drones with THERMAL CAMERAS to check quarantined residents' temperatures. Daily Mail Online. https://www.dailymail.co.uk/news/article-7974935/China-uses-drones-THERMAL-CAMERAS-check-quarantined-residents-temperatures.html. Published February 6, 2020. Accessed February 7, 2020. [Google Scholar]
- 48. Coronavirus Clinical Alert . ACEP. https://www.acep.org/by-medical-focus/infectious-diseases/coronavirus/. Accessed February 7, 2020.
- 49. Qin A, Myers SL, Yu E. China tightens Wuhan lockdown in ‘Wartime’ battle with coronavirus. The New York Times. https://www.nytimes.com/2020/02/06/world/asia/coronavirus-china-wuhan-quarantine.html. Published February 6, 2020. Accessed February 7, 2020. [Google Scholar]
- 50. Kwai I. Day 2 of a Cruise Ship Quarantine: permission to breathe. The New York Times. https://www.nytimes.com/2020/02/06/world/asia/coronavirus-cruise-ship.html. Published February 6, 2020. Accessed February 7, 2020. [Google Scholar]
- 51. William Wan LS. Quarantined on military bases, U.S. evacuees resort to Zumba, stairwell races, accounting classes. The Washington Post. https://www.washingtonpost.com/health/quarantined-on-military-bases-us-evacuees-resort-to-zumba-stairwell-races-accounting-classes/2020/02/06/359d9df6-490e-11ea-bdbf-1dfb23249293_story.html. Published February 7, 2020. Accessed February 7, 2020. [Google Scholar]
- 52. Ellyatt H. Russia closes border with China to prevent spread of the coronavirus. CNBC. https://www.cnbc.com/2020/01/30/coronavirus-russia-closes-border-with-china-to-prevent-spread.html. Published January 30, 2020. Accessed February 7, 2020. [Google Scholar]
- 53. Mansoor S, Carlisle M. Airlines in 3 continents cancel flights to and from China. Time. https://time.com/5774906/airlines-ground-flights-coronavirus/. Published February 3, 2020. Accessed February 7, 2020. [Google Scholar]
- 54. Woo S, Lin L. China logs deadliest day for coronavirus as U.S. plans last flights from Wuhan. The Wall Street Journal. https://www.wsj.com/articles/u-s-plans-last-flights-from-wuhan-as-china-logs-deadliest-day-for-coronavirus-11580990006. Published February 6, 2020. Accessed February 7, 2020. [Google Scholar]
- 55. Mazumdar T. Coronavirus: scientists race to develop a vaccine. BBC News. https://www.bbc.com/news/health-51299735. Published January 30, 2020. Accessed February 7, 2020. [Google Scholar]
- 56. Grady D. China begins testing an antiviral drug in coronavirus patients. The New York Times. https://www.nytimes.com/2020/02/06/health/coronavirus-treatments.html. Published February 6, 2020. Accessed February 7, 2020. [Google Scholar]
- 57. Wee S‐L, McNeil DG, Hernandez JC. W.H.O. declares global emergency as Wuhan coronavirus spreads. New York Times. 2020. https://www.nytimes.com/2020/01/30/health/coronavirus-world-health-organization.html. Published January 30, 2020. Accessed February 2, 2020. [Google Scholar]
- 58. Mounier‐Jack S. Progress and shortcomings in European national strategic plans for pandemic influenza. Bull World Health Organ. 2007;85(12):923‐929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Munster VJ, et al. A novel coronavirus emerging in China — key questions for impact assessment. N Engl J Med. 2020. [DOI] [PubMed] [Google Scholar]
- 60. Buckley C, Myers SL. As new coronavirus spread, China's old habits delayed fight. New York Times. 2020. [Google Scholar]
- 61. Crossley G. Wuhan lockdown unprecedented, shows commitment to contain virus: WHO representative in China. Thomson Reuters. January 23, 2020. https://www.reuters.com/article/us-china-health-who-idUSKBN1ZM1G9. Accessed February 3, 2020. [Google Scholar]
- 62. Mouchtouri VA, Christoforidou EP, an der Heiden M, et al. Exit and entry screening practices for infectious diseases among travelers at points of entry: looking for evidence on public health impact. Int J Environ Res Public Health. 2019;16(23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Fifield A, Sun L. Chinese cities cancel New Year Celebrations, travel ban widens in effort to stop coronavirus outbreak. The Washington Post. January 23, 2020. https://www.washingtonpost.com/world/coronavirus-china-wuhan-latest/2020/01/23/2dc947a8-3d45-11ea-afe2-090eb37b60b1_story.html. Accessed February 3, 2020. [Google Scholar]


