Abstract
The surge of patients in the pandemic of COVID‐19 caused by the novel coronavirus SARS‐CoV‐2 may overwhelm the medical systems of many countries. Mask‐wearing and handwashing can slow the spread of the virus, but currently, masks are in shortage in many countries, and timely handwashing is often impossible. In this study, the efficacy of three types of masks and instant hand wiping was evaluated using the avian influenza virus to mock the coronavirus. Virus quantification was performed using real‐time reverse transcription‐polymerase chain reaction. Previous studies on mask‐wearing were reviewed. The results showed that instant hand wiping using a wet towel soaked in water containing 1.00% soap powder, 0.05% active chlorine, or 0.25% active chlorine from sodium hypochlorite removed 98.36%, 96.62%, and 99.98% of the virus from hands, respectively. N95 masks, medical masks, and homemade masks made of four‐layer kitchen paper and one‐layer cloth could block 99.98%, 97.14%, and 95.15% of the virus in aerosols. Medical mask‐wearing which was supported by many studies was opposed by other studies possibly due to erroneous judgment. With these data, we propose the approach of mask‐wearing plus instant hand hygiene (MIH) to slow the exponential spread of the virus. This MIH approach has been supported by the experiences of seven countries in fighting against COVID‐19. Collectively, a simple approach to slow the exponential spread of SARS‐CoV‐2 was proposed with the support of experiments, literature review, and control experiences.
Keywords: coronavirus, COVID‐19, hand hygiene, mask, pandemic, soap
1. INTRODUCTION
The emerging disease COVID‐19 caused by the new coronavirus SARS‐CoV‐2 was first identified in Wuhan, China in December 2019. 1 , 2 The virus has led to thousands of deaths in China, and the outbreak of COVID‐19 has been well controlled in China through tremendous efforts. 2 However, the virus has sparked a pandemic and is spreading rapidly in many countries. 3 To avoid the tragedy of Wuhan in this February that the surge of too many patients overwhelmed the medical systems, 2 , 3 , 4 , 5 , 6 , 7 a simple and effective approach to slow the spread of the virus is emergently desired worldwide.
Handwashing and mask‐wearing are important to slow the spread of SARS‐CoV‐2. 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 However, it is often difficult to wash hands in time, and current medical masks which are usually called surgical masks are in shortage in many countries. People in some countries have been encouraged to make masks by themselves at home to guard against SARS‐CoV‐2, but it remains unclear whether these homemade masks are effective to block the virus. Moreover, many people have been confused about the claims of some politicians and scientists that medical masks are not useful to protect humans from the infection of SARS‐CoV‐2.
In this study, we evaluated the efficacy of three types of masks in blocking avian influenza virus (AIV) in aerosols and the efficacy of instant hand wiping in removing AIV from hands. AIV was used to mock SARS‐CoV‐2 because they are both enveloped and pleomorphic spherical viruses with a diameter of around 80 to 120 nm. We also reviewed previous reports regarding the efficacy of masks. 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 With these data, we propose a simple approach to slow the spread of the pandemic coronavirus.
2. MATERIALS AND METHODS
Low pathogenic AIV A/chicken/Qingdao/211/2019 was isolated from Qingdao live bird market in 2019. The virus was propagated using embryonated eggs. Virus quantification was performed using a real‐time TaqMan reverse transcription‐polymerase chain reaction (RT‐PCR) assay reported previously. 16
The efficacy of instant hand wiping in removing AIV from hands was evaluated using a towel soaked in water containing soap powder or sodium hypochlorite.
Type 403 nebulizer (Yuyue Medical Equipment & Supply Company, Jiangsu, China) was used to produce aerosols. The aerosols have the median diameters 3.9 μm, and 65% of the aerosols have the diameters less than 5.0 μm, as given in the specification of the nebulizer. The top parts of 60‐mL syringes were removed and then wrapped with the tested masks, namely one‐layer polyester cloth, a homemade mask made of one‐layer polyester cloth plus four‐layer kitchen paper (Hengan Company, Fujian, China; each layer contains three thin layers), a medical mask (AMMEX Company, Shanghai, China), and an N95 mask (Type: New 2001, Jiande Chaomei Daily Chemical Company, Zhejiang, China), respectively (Figure 1). QVS facial cleaning sponge (8‐mm thick; Watsons Company, Guangdong, China) made of hydrophilic polyvinyl alcohol was set inside the syringe behind the mask (Figure 1) for collecting the virus passing through the masks. The four syringes were then aligned and bound seamlessly together.
Figure 1.
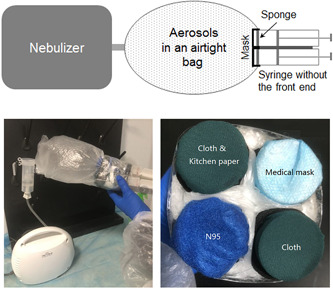
The system mocking human breath for evaluation of the efficacy of masks
3. RESULTS
3.1. Virus quantification using real‐time RT‐PCR
In principle, if the virus amount declines by 50%, the C t value of the real‐time TaqMan RT‐PCR shall increase by 1. Our experiment with three repeats showed that the virus amount declined by 50%, the C t value increased by 0.96 (95% confidence interval: 0.86‐1.04), using 1:8 serially diluted allantoic fluid of inoculated embryonated eggs containing the AIV. Taken together, we presumed that the virus amount declines by 50% if the C t value increases by 1, and the virus amount declines by (100 × (1 − 1/(2^Y)))% if the C t value increases by Y, in this study.
3.2. Efficacy of hand wiping
We put 5 μL of the undiluted allantoic fluid containing the AIV on the hand of one author of this study, and spread the fluid around the palm, and kept for 3 minutes. We then wiped the palm three times from the root of the palm to the tips of the fingers, using a towel soaked in water containing soap or sodium hypochlorite and then wrung to remove most of the water inside. We eluted the hand using 5 mL phosphate‐buffered saline (PBS), and RNA from 200 μL of the eluted PBS was extracted for the detection of the amount of the virus using the TaqMan RT‐PCR. Each treatment and the control without wiping were conducted independently for three times. Table 1 showed, as compared with the control without the towel wiping, the virus on the palm declined by 98.36%, 96.62%, and 99.98% through wiping using the wet towel soaked in water containing 1.00% (g/g) soap powder, 0.05% (g/g) active chlorine from sodium hypochlorite, or 0.25% (g/g) active chlorine from sodium hypochlorite, respectively. All the relevant C t values in Table 1 were of significant difference (P < .01) by the t test, except those two pertaining to 1.00% soap powder and 0.05% active chlorine.
Table 1.
Percentage of AIV removed through instant wiping as compared without wiping
| Material for towel soaking | C t increase ( ± SD) | Percentage removed (95% CI) |
|---|---|---|
| 1.00% Soap powder | 5.93 ± 1.24 | 98.36% (96.11%‐99.31%) |
| 0.05% Active chlorine | 4.89 ± 0.74 | 96.62% (94.37%‐97.97%) |
| 0.25% Active chlorine | 12.01 ± 1.25 | 99.98% (99.94%‐99.99%) |
Abbreviations: AIV, avian influenza virus; CI, confidence interval; SD, standard deviation.
3.3. Efficacy of masks
The allantoic fluid containing the AIV was 1:10 diluted using PBS. The fluid was added into the nebulizer for producing the aerosols containing the virus. The aerosols were collected using a seamless plastic bag (Figure 1). The nebulizer was paused when the bag was bulging. The air containing the aerosols was inhaled into and out of the syringes for 100 times through the synchronous piston movement of the four syringes, to mock human breath. Then the mask was unwrapped, and the sponge inside the syringe was taken out and added with 2 mL PBS. The sponge was pressed for five times using a 200‐μL pipette tip. RNA from 1 mL of the PBS was extracted for the detection of the amount of the virus using the TaqMan RT‐PCR. Each treatment was conducted independently for four times. Table 2 showed that, as compared with the polyester cloth, the N95 mask blocked 99.98% of the virus, and the medical mask blocked 97.14% of the virus, and the homemade mask blocked 95.15% of the virus. All the relevant C t values were of significant difference (P < .01) by the t test, except those two pertaining to the medical masks and the homemade masks.
Table 2.
Percentage of AIV blocked by masks as compared with one layer of cloth
| C t increase ( ± SD) | Percentage blocked (95% CI) | |
|---|---|---|
| N95 mask | 12.49 ± 0.33 | 99.98% (99.98%‐99.99%) |
| Medical mask | 5.13 ± 0.98 | 97.14% (94.36%‐98.55%) |
| Homemade mask | 4.37 ± 0.90 | 95.15% (90.97%‐97.39%) |
Abbreviations: AIV, avian influenza virus; CI, confidence interval; SD, standard deviation.
4. DISCUSSION
Because clean water is often unavailable at hand, people can be infected through hand‐mouth, hand‐nose, or hand‐eye contact before handwashing. In this sense, it is important to have one item at hand, such as 75% alcohol, hand sanitizer gel, disinfecting wipes, for instant hand hygiene after we have touched something possibly contaminated by the virus. This is more important for those traveling long‐distance using public vehicles or having touched some items frequently touched by other people. This study suggested that instant hand wiping using a wet towel containing soap or sodium hypochlorite removed most viruses from hands. Water containing 1.00% soap powder is not only helpful for wiping away the virus using its surfactant activity but also efficiently inactivates enveloped viruses including coronavirus, as proved by multiple previous studies. 17 , 18 , 19 Moreover, water containing 1.00% soap powder is safe for skin and other items including clothes. It is worth noting that the concentration of soap powder and sodium hypochlorite is vital for their wiping and virucidal effects.
Various studies have suggested that SARS‐CoV‐2 can be transmitted through droplets and aerosols, 1 , 2 , 3 , 4 , 5 , 6 , 7 and so hand hygiene is inadequate to prevent infection of SARS‐CoV‐2, and blocking masks are needed. This study showed that N95 masks blocked nearly all the mock virus, and medical masks blocked approximately 97% of the virus, and the homemade mask blocked approximately 95% of the virus. Therefore, the medical masks are not fully protective in hospitals but are useful for common social occasions. When medical masks are in shortage, the homemade masks made of four‐layer kitchen paper (each layer contains three thin layers) and one layer of polyester cloth should be helpful, as indicated by this study. The kitchen paper is effective in blocking the virus possibly because of its multiple layers, nonwoven structure, and virus‐absorbing property. As we have tested by ourselves, the tested homemade masks are more breathable than the N95 masks. One advantage of the homemade mask is that the kitchen paper can be changed frequently. It is worth noting that the homemade masks shall be of less blocking efficacy if made of fewer layers of kitchen paper. Other types of homemade masks, especially those made of cloth alone, may be unable to block the virus and thus confer no protection against the virus. 20 , 21 Additionally, although a person inhales much more than 100 times a day, the mocking data are reliable because aerosols containing the virus to be inhaled by a person on most common social occasions are fewer than in this experiment.
Some randomized controlled trials (RCTs) did not support the efficacy of medical masks because medical masks could not reduce infection rates of some viral respiratory diseases. 14 , 15 Consequently, people in some countries opposed to using medical masks on common social occasions. In effect, the conclusions of these RCTs could be erroneous, as reflected by the following assumed scenario. Supposed the virus could have ten opportunities to infect a human during a period of 30 days, wearing medical masks could block three of the 10 opportunities and thus reduce the infection risk by 30%, although it itself could not block the other seven opportunities during the 30 days. Therefore, the fact that medical mask‐wearing did not reduce the infection rate could suggest that medical mask‐wearing is inadequate to prevent the infection, rather than useless for reducing the infection risk. Some other RCTs and many nonrandomized studies regarding the use of medical masks supported the notion that wearing medical masks could reduce infection risks of some viral respiratory diseases. 8 , 9 , 10 , 11 , 12 , 13 , 14 Moreover, medical mask‐wearing can enhance one's vigilance, prevent direct hand‐mouth or hand‐nose contact, and reduce air contamination of pathogens from infected people.
With the above data and discussion, we propose herein the approach of mask‐wearing and instant hand hygiene (MIH), namely that common people should wear effective masks and bring an appropriate item for instant hand hygiene when needed, to slow the rapid spread of the virus worldwide. This is crucial for the world to reduce severe and fatal cases of the virus before successful marketing of the effective vaccines against the coronavirus, and avoid the tragedy of medical systems being overwhelmed by a surge of too many patients. As indicated in this study, when medical masks and disinfectants are in shortage, the homemade masks made of kitchen paper can be used to temporally surrogate medical masks, and so soap powder is used for instant hand hygiene.
From the news we know that the MIH approach has been implemented in China, Republic of Korea, and Japan, where mask‐wearing is widely accepted and items for instant hand hygiene are usually accessible in public areas. The spread of the coronavirus in all these three countries has been well controlled. 3 , 6 In contrast, Iran, Italy, Spain, and the USA did not implement the MIH approach in the beginning weeks, and many people in those countries are reluctant to wear medical masks. None of these four countries have decelerated the spread of the coronavirus so far. 3 , 5
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTION
Design: JMC, QXM, HS; experiment: QXM, HLZ, GML, RMY; data analysis: JMC, QXM, HS; funding: HS; manuscript writing: JMC, HS.
ETHICS STATEMENT
The article does not contain the participation of animals and humans other than the authors.
ACKNOWLEDGMENTS
We thank Meng Yang and Randong Li for their helpful advice and assistance. This research was funded by the National Key R&D Program for the 13th Five‐Year Plan of China (2016YFD050110404 and 2016YFD0500707‐7); the Shandong Key Research and Development Program in China (2019GNC106074); the Shandong Team‐training Program for Talents of Superior Disciplines at Colleges in China (1119029). The funders do not have any role in the design, conduct, and report of this study.
Ma Q‐X, Shan H, Zhang H‐L, Li G‐M, Yang R‐M, Chen J‐M. Potential utilities of mask‐wearing and instant hand hygiene for fighting SARS‐CoV‐2. J Med Virol. 2020;92:1567–1571. 10.1002/jmv.25805
This work was conducted in the College of Veterinary Medicine, Qingdao Agricultural University.
DATA AVAILABILITY STATEMENT
The derived data supporting the findings of this study are available within the article, and the raw data supporting the findings of this study are available from the corresponding author JC on request.
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chinese National Health Commission (NHC) . Update of the outbreak of the SARS‐CoV‐2. http://www.nhc.gov.cn/xcs/yqfkdt/gzbd_index.shtml
- 3. World Health Organization (WHO) . Novel coronavirus (SARS‐CoV‐2) situation reports. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports/
- 4. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:NEJMoa2002032. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet. 2020;395, 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Choi SC, Ki M. Estimating the reproductive number and the outbreak size of novel coronavirus disease (COVID‐19) using mathematical model in Republic of Korea. Epidemiol Health. 2020;12:e2020011. 10.4178/epih.e2020011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID‐19 based on current evidence. J Med Virol. 2020;92:jmv.25722. 10.1002/jmv.25722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cowling BJ, Chan KH, Fang VJ, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151(7):437‐446. 10.7326/0003-4819-151-7-200910060-00142 [DOI] [PubMed] [Google Scholar]
- 9. Zhou SS, Lukula S, Chiossone C, Nims RW, Suchmann DB, Ijaz MK. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J Thorac Dis. 2018;10(3):2059‐2069. 10.21037/jtd.2018.03.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta‐analysis. Clin Infect Dis. 2017;65(11):1934‐1942. 10.1093/cid/cix681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. MacIntyre CR, Wang Q, Cauchemez S, et al. A cluster randomized clinical trial comparing fit‐tested and non‐fit‐tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respir Viruses. 2011;5(3):170‐179. 10.1111/j.1750-2659.2011.00198.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta‐analysis. CMAJ. 2016;188(8):567‐574. 10.1503/cmaj.150835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;35:h694. 10.1136/bmj.h694 [DOI] [PubMed] [Google Scholar]
- 14. Xiao J, Shiu EYC, Gao H, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings‐personal protective and environmental measures. Emerg Infect Dis. 2020;26(5), 10.3201/eid2605.190994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. SMART AIR . What are the best materials for making DIY masks? https://smartairfilters.com/en/blog/best‐materials‐make‐diy‐face‐mask‐virus/
- 16. Zhang Z, Liu D, Sun W, et al. Multiplex one‐step real‐time PCR by Taqman‐MGB method for rapid detection of pan and H5 subtype avian influenza viruses. PLoS One. 2017;12(6):e0178634. 10.1371/journal.pone.0178634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lai MY, Cheng PK, Lim WW. Survival of severe acute respiratory syndrome coronavirus. Clin Infect Dis. 2005;41(7):e67‐e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li JZ, Mack EC, Levy JA. Virucidal efficacy of soap and water against human immunodeficiency virus in genital secretions. Antimicrob Agents Chemother. 2003;47(10):3321‐3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saknimit M, Inatsuki I, Sugiyama Y, Yagami K. Virucidal efficacy of physico‐chemical treatments against coronaviruses and parvoviruses of laboratory animals. Jikken Dobutsu. 1988;37(3):341‐345. [DOI] [PubMed] [Google Scholar]
- 20. Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7(4):413‐418. 10.1017/dmp.2013.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4):e006577. 10.1136/bmjopen-2014-006577 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The derived data supporting the findings of this study are available within the article, and the raw data supporting the findings of this study are available from the corresponding author JC on request.


