Abstract
Background and Objectives
Integration in one’s social community may depend in part upon feeling safe and secure within one’s physical community, or neighborhood. Moreover, high-quality neighborhoods may serve as a supportive resource, potentially “buffering” against the harmful influence of experiences such as discrimination or depression that could otherwise erode adults’ sense of belonging. This study examines longitudinal associations of perceived neighborhood quality, daily discrimination, and depression with social integration among midlife and older adults, and tests whether perceived neighborhood quality is of increased importance with age and/or in the contexts of discrimination and depression.
Research Design and Methods
Multilevel random intercept models analyzed 6,016 observations of 3,102 individuals drawn from the 3 waves of the National Survey of Midlife Development in the United States (MIDUS, 1995–2014).
Results
Perceived neighborhood quality was associated with greater social integration throughout adulthood, though its impact was slightly attenuated with age. Moreover, depression was harmful for social integration across the age range, yet its influence was significantly buffered by perceived neighborhood quality. Daily discrimination was not associated with social integration, net of covariates.
Discussion and Implications
Findings underscore the importance of physical place and person-environment fit for social well-being throughout adulthood, and confirm the deleterious effects of depression for adults’ social integration. Further, results highlight perceived neighborhood quality as a critical component for successful “aging in place,” particularly as a social resource adults may call upon in the context of depression.
Keywords: Social isolation, Social support, Stress process, Well-being
Social integration is an important feature of adults’ lives and their well-being. Social integration refers to one’s connectedness to a broader community, and to the quality of that connection (Keyes, 1998). This study uses Keyes’ (1998) definition of social integration, which is a subjective measure of perceived cohesion or connectedness rather than an objective measure of social embeddedness (see, e.g., Berkman, Glass, Brissette, & Seeman, 2000). Such perceptions of belonging, however, reflect positive relations with community and social network members and can promote adults’ physical, psychological, and emotional well-being (e.g., Moorman, Stokes, & Morelock, 2017; Stokes, 2019a).
As with networks of intimate ties, social integration depends, in part, upon the availability of high-quality and supportive people and places, including neighborhoods (Bromell & Cagney, 2014; Cramm, van Dijk, & Nieboer, 2013; Moorman et al., 2017). Indeed, although integration within social communities is not necessarily limited by geography, the neighborhood remains a primary context for social engagement, particularly as individuals enter later life and depend increasingly on their neighbors for social contact (Aneshensel, 2009; Cornwell, Laumann, & Schumm, 2008). In fact, older adults spend upwards of 75% of daytime hours in their homes and neighborhoods (Oswald & Wahl, 2005). Adults with negative perceptions of their own neighborhoods may feel socially isolated or disconnected as a result, perhaps even “stuck” in place (e.g., Cramm et al., 2013; Haney, 2007).
Additionally, adults’ sense of worth and belonging may be undermined by experiences of day-to-day discrimination, whether in one’s neighborhood, workplace, or elsewhere (Charles, 2010; Schmitt, Branscombe, Postmes, & Garcia, 2014). This may result in social isolation, especially if individuals feel rejected by their own communities, and remove themselves from physical and social contexts where discriminatory interactions may occur (e.g., Carstensen, Fung, & Charles, 2003). Similarly, experiences of depression may undermine social well-being as well. Depression is associated with less frequent participation in social activities, lower social engagement, and inferior perceptions of social support and acceptance (Achterberg et al., 2003; Holtfreter, Reisig, & Turanovic, 2017; Kim & Thomas, 2017). However, the negative impacts of both discrimination and depression may be buffered by social support (e.g., Holtfreter et al., 2017; Pascoe & Richman, 2009), potentially including that derived from high-quality neighbors and neighborhoods.
This study uses the theoretical frameworks of person-environment fit (e.g., Wahl, Iwarsson, & Oswald, 2012) and the stress process (Pearlin, Menaghan, Lieberman, & Mullan, 1981) to examine longitudinal associations between perceived neighborhood quality and social integration throughout adulthood, and to further examine whether perceived neighborhood quality is of heightened importance with age and/or in the contexts of daily discrimination and depression.
Neighborhoods and Social Integration
Social integration, like some other aspects of social well-being, tends to increase overall with age (Keyes, 1998). Such improvement over time may reflect the process of socioemotional selectivity, whereby adults focus more on their best and most rewarding relationships as they age, removing themselves from relationships and social contexts that lead to negative or discriminatory interactions (Carstensen et al., 2003). Socioemotional selectivity has limits, however, and many social network reductions are unchosen and difficult to replace (Rook, 2009). In the absence of other social ties, older adults increasingly seek out social contact with people in their neighborhoods, religious communities, and volunteer organizations (Cornwell et al., 2008). Neighborhoods that foster feelings of trust and safety may thus improve social integration by providing opportunities for positive, supportive social relationships to develop outside the home (Haney, 2007). Particularly given age-based reductions in social network size, the perceived quality of one’s neighborhood may be of critical importance for adults’ social integration.
Recent findings concerning perceived neighborhood quality and age have produced mixed results. For instance, one recent study found that perceived neighborhood quality was more strongly linked with life satisfaction among the oldest-old than the young-old (Oswald, Jopp, Rott, & Wahl, 2011). However, another study found that the effects of perceived neighborhood quality on life satisfaction and negative affect were consistent throughout adulthood (Stokes, 2019b). Despite these inconsistencies, perceptions of neighborhood quality have been repeatedly linked with greater well-being (Cramm et al., 2013; Haney, 2007; Oswald et al., 2011; Stokes, 2019b). Building upon this prior literature, the present study analyzes longitudinal data to examine associations between perceived neighborhood quality and social integration across the years of middle and later life, and further examines whether perceived neighborhood quality is of increased importance for social integration with age.
Daily Discrimination, Depression, and Neighborhood Quality
Perceived day-to-day discrimination is a psychosocial stressor (Pearlin et al., 1981) with well-established implications for both physical and psychological well-being (Pascoe & Richman, 2009; Schmitt et al., 2014). In contrast to major discriminatory events, daily discrimination reflects more minor experiences of being treated with less respect, less courtesy, or more distrust than others (Williams, Yu, Jackson, & Anderson, 1997). Such discriminatory interactions may erode individuals’ sense of worth and belonging, and thereby harm social well-being, as well (e.g., Charles, 2010; Stokes, 2019a).
Similarly, experiences of depression can isolate individuals, and may thus also erode or impede social well-being. Depression reduces social engagement and participation, and makes individuals more sensitive to instances of social rejection (e.g., Achterberg et al., 2003; Holtfreter et al., 2017; Steger & Kashdan, 2009). As a major symptom of stress and a potential consequence of discrimination (Pascoe & Richman, 2009; Pearlin et al., 1981), depression may likewise have detrimental implications for adults’ social integration.
The stress process model (Pearlin et al., 1981) suggests that the harmful effects of discrimination and other stressors may be reduced, or buffered, by factors such as social support. That is, those who have access to supportive social ties are less harshly affected by negative stimuli (e.g., Pascoe & Richman, 2009). While family and friends are important sources of social support, neighborhoods may also serve as a social resource that can protect or buffer against stressful interactions (e.g., Aneshensel, 2009; Oswald et al., 2011). Similarly, the framework of person-environment fit (e.g., Wahl et al., 2012) asserts that the importance of environmental and neighborhood features for adults’ well-being may depend in part on individuals’ own needs, desires, and characteristics. For instance, aspects of neighborhood built environment such as walkability and accessibility may be most impactful for older residents or those with physical limitations (Oswald et al., 2011). In the present case, neighborhoods that foster a sense of safety and trust may be of greater import for social integration among adults experiencing depression or facing stressors such as discrimination.
Recent studies concerning discrimination on the basis of age and race/ethnicity have found neighborhood features to be protective, either by reducing the likelihood of experiencing discrimination in the first place (e.g., Bécares et al., 2012; Stokes & Moorman, 2016), or by buffering against its harmful effects (e.g., Bécares, Nazroo, & Stafford, 2009). However, these studies explored aspects of neighborhood age and racial/ethnic composition, rather than subjective perceptions of neighborhood quality, as potential stress buffers. Likewise, research concerning neighborhoods and depression has largely focused on the extent to which neighborhood features, such as disadvantage and disorder, may protect against (or expose individuals to) depressive symptoms, and for whom (Aneshensel, 2009; Kim, 2008). Little research has examined whether perceptions of neighborhood context may moderate associations between depression and social well-being. However, recent research has noted that high-quality relationships, in particular from family, may buffer against the negative influence of depression on participation in social activities (Holtfreter et al., 2017). Moreover, depressed individuals appear more sensitive to positive as well as negative social stimuli (Steger & Kashdan, 2009), making perceived neighborhood quality a potentially valuable social resource for depressed adults.
Study Aims
This study builds upon prior research and incorporates both person-environment fit (Wahl et al., 2012) and stress process (Pearlin et al., 1981) frameworks to examine whether perceptions of neighborhood quality promote greater social integration throughout adulthood, and whether this effect is of increased importance with age and/or in the context of experiencing daily discrimination or depression. Specifically, this study tests four main hypotheses:
Hypothesis 1: Perceived neighborhood quality (+), daily discrimination (-), and depression (-) will be significantly associated with social integration over the 19-year study period.
Hypothesis 2: The association of perceived neighborhood quality with social integration will be stronger at older ages.
Hypothesis 3: The association of perceived neighborhood quality with social integration will be stronger at higher levels of daily discrimination.
Hypothesis 4: The association of perceived neighborhood quality with social integration will be stronger among adults experiencing depression.
Methods
Data and Sample
Data for the present study were drawn from the three waves of the National Survey of Midlife Development in the United States (MIDUS, 1995–2014). MIDUS began in 1995–1996 with a random digit dial (RDD) probability sample of noninstitutionalized, English-speaking residents of the contiguous United States between the ages of 24 and 74 (Ryff et al., 2017). A second wave was administered from 2004 to 2006, with a third wave occurring in 2013–2014. Both phone interviews and self-administered questionnaires (SAQ) were utilized (Ryff et al., 2017). Items of interest for this study came from the SAQ; thus, the analytic sample comprised those who completed both the phone interview and the SAQ at one or more waves of MIDUS.
The response rate for the RDD sample at baseline was 70%, with 87% of those participants also completing the SAQ (N = 3,034; Ryff et al., 2017). This number was reduced to 1,805 participants (59% of the Wave 1 total) at Wave 2, and to 1,177 (65% of the Wave 2 total) at Wave 3. This includes the small number of individuals who answered the phone interview and SAQ for the first time at either Wave 2 or Wave 3. Correlates of attrition from Wave 1 to Wave 2 included perceived neighborhood quality, daily discrimination, social integration, and age, as well as family and friend support, instrumental activities of daily living (IADL), self-rated health, gender, education, race, homeownership status, and marital status. Attrition from Wave 2 to Wave 3 was predicted by perceived neighborhood quality and age, as well as by friend support, income, IADL, self-rated health, education, race, homeownership status, marital status, and employment status. The final analytic sample included 6,016 observations of 3,102 individuals.
Measures
Social integration
Social integration was measured using a three-item scale (Keyes, 1998). Participants were asked to respond on a scale from 1 (Strongly agree) to 7 (Strongly disagree) to the following: “I feel close to other people in my community,” “My community is a source of comfort,” and “I don’t feel I belong to anything I’d call a community”. Social integration was generated as a mean-score scale (α = .77), with items coded such that higher values indicated greater social integration. This and all other multi-item scales were set to missing if fewer than half of the scale items were answered.
Perceived neighborhood quality
Perceived neighborhood quality was measured using a four-item scale (Keyes, 1998). Response options ranged from 1 (Not at all) to 4 (A lot) for the following: “I feel safe being out alone in my neighborhood at night,” “I feel safe being out alone in my neighborhood during the daytime,” “I could call on a neighbor for help if I needed it,” and “People in my neighborhood trust each other.” Perceived neighborhood quality was generated as a mean-score scale, with higher values indicating greater perceived quality (α = .65). Perceived neighborhood quality was mean-centered for analysis.
Daily discrimination
Daily discrimination was measured using a nine-item mean-score scale concerning the frequency of participants’ day-to-day experiences of all-cause discrimination, with responses ranging from 1 (Never) to 4 (Often) (Williams et al., 1997). Sample items include “People act as if they think you are not smart” and “People act as if they think you are not as good as they are”. Approximately 40% of participants reported no discrimination, causing substantial positive skew. Therefore daily discrimination was recoded such that 1 = Never, 2 = More than never to rarely, 3 = More than rarely to sometimes, and 4 = More than sometimes to often. Daily discrimination was mean-centered for analysis.
Depression
Participants were asked a series of Yes/No questions concerning symptoms of depressed affect and anhedonia, both subscales of depression (e.g., “During two weeks in the past 12 months, when you felt sad, blue, or depressed, did you have more trouble falling asleep than usual?”) (Wang, Berglund, & Kessler, 2000). Dichotomous indicators were created for both subscales, based on the number and severity of symptoms reported (Ryff et al., 2017). A dichotomous indicator of depression was used to indicate whether participants experienced significant symptoms of depressed affect and/or anhedonia (Ryff et al., 2017).
Age
Age was measured as a continuous variable, in years, and was mean-centered for analysis.
Covariates
Family (α = .83) and friend support (α = .87) were measured as self-reported four-item mean-score scales. Years lived in neighborhood was self-reported and measured in years. Gender was measured using dichotomous indicators for male (reference) and female. Race was measured using three dichotomous indicators for white (reference), black, and other race. Ethnicity was measured using dichotomous indicators for Non-Hispanic (reference) and Hispanic. Education was measured using dichotomous indicators for less than high school, high school degree, some college (reference), college degree, and some education beyond college. Marital status was measured using dichotomous indicators for married (reference), divorced/separated, widowed, and never married. Parental status was measured using dichotomous indicators of whether a participant had any children or did not have any children (reference). Employment status was measured using dichotomous indicators for employed (reference), retired, and not employed. Homeownership status was measured using dichotomous indicators for owns home outright, paying on a mortgage (reference), and rents home. Income was self-reported in reference to the previous year in U.S. dollars, and was standardized at each wave separately to ensure comparability across waves (Stokes, 2019b). Self-rated health was a single-item self-report ranging from 1 (Poor) to 5 (Excellent). Neuroticism was measured using a four-item mean-score scale (α = .73) ranging from 1 (Lowest) to 4 (Highest) (Lachman & Weaver, 1997). Neuroticism was mean-centered for analysis, with a squared term included to model significant curvilinearity. Lastly, dichotomous controls for data collection wave (reference = Wave 1) were included to assess period effects.
Analytic Strategy and Missing Data
The majority of valid cases (64%) had complete data for all measures included in the analysis. However, 21% of observations were missing data concerning Hispanic ethnicity, largely because there was no direct question about Hispanic ethnicity at Wave 1. To correct for this, Wave 1 observations were coded as “Hispanic” or “Not Hispanic” based on longitudinal participants’ Wave 2 or Wave 3 responses (Stokes, 2019b). Values were set to missing for those lacking valid Wave 2 or Wave 3 data, or who were missing data on this item at all waves. Excluding Hispanic ethnicity, 82% of valid cases had complete data on all measures included in the final analysis. Missing data diagnostics were performed, and no other patterns of item-missingness were detected. Therefore, missing data were addressed using multiple imputation by chained equations (Royston, 2005). All variables used in the final analyses, including the outcome measure, were included in the imputation equations. A total of 10 complete data sets were generated for analysis. To assess the potential impact of attrition on findings, a sensitivity analysis was performed, which imputed data for all cases missing at one or more waves (N obs. = 9,306). All significant findings of interest were stable and consistent with those presented subsequently.
Multilevel random intercept models were used for this analysis, to account for the non-independence of observations nested within individuals. An autoregressive residual structure was modeled, as well, to account for the correlation of individuals’ residual errors from wave to wave.
Analysis began with a model that included all predictors of interest—excluding perceived neighborhood quality, family support, and friend support—along with all covariates. Model 2 then added the perceived neighborhood quality, family support, and friend support measures to Model 1, to assess potential mediation. Interactions were then tested between perceived neighborhood quality and (a) age (Model 3), (b) daily discrimination (Model 4), and (c) depression (Model 5). Lastly, Model 6 simultaneously estimated all main effects of interest, all covariate effects, and all significant interactions detected in Models 3 through 5.
Results
Descriptive Statistics
Participants’ reports of social integration and neighborhood quality varied significantly across waves, but remained relatively positive throughout. For instance, social integration was significantly higher at Wave 1 compared to Waves 2 and 3 (p < .001 and p < .01, respectively), yet was consistently between 4.67 and 4.85 on the 7-point scale. Wave 1 perceptions of neighborhood quality were worse than those at Wave 2 or 3 (both p < .001), but still averaged 3.39 on the four-point scale. Depression was greatest at Wave 1 and significantly lower at Waves 2 and 3 (p < .05 and p < .001, respectively), but never exceeded 14% of the sample. Daily discrimination did not vary significantly across waves, but was consistently low, averaging between 1.70 and 1.75 on the four-point scale across waves. The average age of respondents increased from 47 at baseline to nearly 65 at Wave 3. Table 1 reports descriptive statistics for all measures included in the analysis.
Table 1.
Descriptive Statistics, National Study of Midlife Development in the United States, 1995–2014 (N = 6,016 Observations of 3,102 Individuals)
| Wave 1 (n = 3,034) | Wave 2 (n = 1,805) | Wave 3 (n = 1,177) | |
|---|---|---|---|
| Mean (SD), or % | Mean (SD), or % | Mean (SD), or % | |
| Social integration | 4.67 (1.45) | 4.86 (1.33) | 4.85 (1.33) |
| Perceived neighborhood quality | 3.40 (0.54) | 3.47 (0.52) | 3.48 (0.52) |
| Daily discrimination | 1.75 (0.72) | 1.74 (0.67) | 1.70 (0.68) |
| Experienced depression | 13.78% | 11.36% | 10.20% |
| Age | 47.06 (13.12) | 56.85 (12.62) | 64.72 (11.37) |
| Family support | 1.58 (0.62) | 1.50 (0.61) | 1.52 (0.60) |
| Friend support | 1.78 (0.68) | 1.74 (0.67) | 1.69 (0.63) |
| Years lived in neighborhood | 14.28 (17.38) | 16.82 (14.84) | 20.78 (15.95) |
| Gender | |||
| Female | 51.52% | 54.68% | 53.27% |
| Male | 48.48% | 45.32% | 46.73% |
| Race | |||
| White | 85.23% | 89.92% | 91.33% |
| Black | 6.62% | 5.43% | 4.59% |
| Other race | 8.14% | 4.65% | 4.08% |
| Ethnicity | |||
| Hispanic | 3.54% | 3.89% | 3.66% |
| Not Hispanic | 96.46% | 96.11% | 96.34% |
| Education | |||
| Less than high school | 9.93% | 7.10% | 5.27% |
| High school degree | 29.29% | 27.23% | 24.83% |
| Some college | 31.20% | 28.62% | 29.59% |
| College degree | 16.99% | 18.86% | 20.75% |
| Some education beyond college | 12.60% | 18.19% | 19.56% |
| Marital status | |||
| Married | 64.04% | 67.37% | 63.83% |
| Divorced/separated | 18.46% | 16.54% | 16.68% |
| Widowed | 5.93% | 8.60% | 11.91% |
| Never married | 11.57% | 7.49% | 7.57% |
| Parental status | |||
| Has children | 82.43% | 87.04% | 87.26% |
| No children | 17.57% | 12.96% | 12.74% |
| Employment status | |||
| Employed | 59.49% | 49.28% | 47.75% |
| Retired | 15.72% | 27.76% | 29.12% |
| Not employed | 24.79% | 22.97% | 23.13% |
| Home ownership status | |||
| Owns home outright | 24.52% | 36.19% | 44.29% |
| Paying on a mortgage | 51.37% | 51.40% | 42.69% |
| Rents home | 24.11% | 12.41% | 13.02% |
| Incomea | $14,609 ($7,050) | $25,969 ($17,798) | $25,234 ($21,161) |
| IADL | 1.62 (0.81) | 1.83 (0.90) | 2.04 (0.98) |
| Self-rated health | 3.45 (1.00) | 3.50 (1.00) | 3.38 (1.06) |
| Neuroticism | 2.25 (0.66) | 2.09 (0.63) | 2.10 (0.63) |
Notes: IADL = instrumental activities of daily living.
aIncome reported in U.S. dollars, calculated from the raw scores. Income was transformed into wave-specific standardized scores for analysis.
Longitudinal Analyses
Results of multilevel random intercept models are presented in Table 2. Model 1 indicated that social integration increased somewhat with age (B = 0.01, p < .001), and that perceived daily discrimination (B = −0.13, p < .001) and depression (B = −0.16, p < .001) were both associated with lower social integration across the 19-year study period. Among covariates, years lived in neighborhood (B = 0.01, p < .001), female gender (B = 0.21, p < .001), black (B = 0.24, p < .01) and other race (B = 0.23, p < .05), having less than a high school education (B = −0.18, p < .05), a college degree (B = 0.26, p < .001) or education beyond college (B = 0.22, p < .001), being divorced/separated (B = −0.12, p < .01), renting one’s home (B = −0.24, p < .001), IADL (B = −0.08, p < .01), self-rated health (B = 0.04, p < .05), linear (B = −0.33, p < .001) and quadratic (B = −0.08, p < .05) neuroticism, and Wave 3 data collection (B = −0.15, p < .01) were significantly associated with social integration.
Table 2.
Multilevel Random Intercept Models Concerning Perceived Neighborhood Quality, Daily Discrimination, Depression, and Social Integration From 1995 to 2014 (N = 6,016 Observations of 3,102 Individuals)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | |
| Predictors of interest | ||||||
| Perceived neighborhood qualitya | - | 0.62*** (0.03) | 0.61*** (0.03) | 0.61*** (0.03) | 0.59*** (0.04) | 0.58*** (0.04) |
| Daily discriminationa | −0.13*** (0.03) | −0.02 (0.02) | −0.02 (0.02) | −0.01 (0.02) | −0.02 (0.02) | −0.01 (0.02) |
| Experienced depressionb | −0.16** (0.05) | −0.16** (0.05) | −0.16** (0.05) | −0.16** (0.05) | −0.14** (0.05) | −0.14** (0.05) |
| Agea | 0.01*** (0.00) | 0.01** (0.00) | 0.01** (0.00) | 0.01** (0.00) | 0.01** (0.00) | 0.01** (0.00) |
| Interaction terms | ||||||
| Perceived neighborhood qualitya × agea | - | - | −0.01** (0.00) | - | - | −0.01** (0.00) |
| Perceived neighborhood qualitya × daily discriminationa | - | - | - | 0.06 (0.04) | - | - |
| Perceived neighbohood qualitya × experienced depressionb | - | - | - | - | 0.18* (0.08) | 0.16* (0.08) |
| Covariates | ||||||
| Family supporta | - | 0.23*** (0.03) | 0.23*** (0.03) | 0.23*** (0.03) | 0.23*** (0.03) | 0.23*** (0.03) |
| Friend supporta | - | 0.43*** (0.03) | 0.43*** (0.03) | 0.43*** (0.03) | 0.43*** (0.03) | 0.43*** (0.03) |
| Years lived in neighborhood | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) | 0.01*** (0.00) |
| Femalec | 0.21*** (0.05) | 0.11** (0.04) | 0.10** (0.04) | 0.11** (0.04) | 0.11** (0.04) | 0.10* (0.04) |
| Blackd | 0.24** (0.09) | 0.31*** (0.08) | 0.31*** (0.08) | 0.32*** (0.08) | 0.31*** (0.08) | 0.30*** (0.08) |
| Other raced | 0.23* (0.10) | 0.31** (0.10) | 0.31** (0.10) | 0.31** (0.10) | 0.30** (0.10) | 0.30** (0.10) |
| Hispanice | −0.10 (0.14) | −0.08 (0.14) | −0.08 (0.14) | −0.08 (0.14) | −0.08 (0.14) | −0.07 (0.14) |
| Less than high schoolf | −0.18* (0.08) | −0.11 (0.07) | −0.12 (0.07) | −0.11 (0.07) | −0.11 (0.07) | −0.12 (0.07) |
| High school degreef | −0.04 (0.05) | −0.01 (0.04) | −0.01 (0.04) | −0.01 (0.04) | −0.01 (0.04) | −0.02 (0.04) |
| College degreef | 0.26*** (0.06) | 0.24*** (0.05) | 0.24*** (0.05) | 0.24*** (0.05) | 0.24*** (0.05) | 0.24*** (0.05) |
| Education beyond collegef | 0.22*** (0.06) | 0.23*** (0.06) | 0.24*** (0.06) | 0.23*** (0.06) | 0.24*** (0.06) | 0.24*** (0.06) |
| Divorced/separatedg | −0.12* (0.05) | −0.11* (0.05) | −0.11* (0.05) | −0.11* (0.05) | −0.11* (0.05) | −0.11* (0.05) |
| Widowedg | −0.09 (0.07) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) |
| Never marriedg | −0.11 (0.08) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) | −0.12 (0.07) |
| Has childrenh | 0.10 (0.07) | 0.07 (0.06) | 0.06 (0.06) | 0.07 (0.06) | 0.07 (0.06) | 0.06 (0.06) |
| Retiredi | 0.08 (0.06) | 0.03 (0.05) | 0.03 (0.05) | 0.03 (0.05) | 0.03 (0.05) | 0.03 (0.05) |
| Not employedi | 0.04 (0.05) | 0.06 (0.04) | 0.06 (0.04) | 0.06 (0.04) | 0.06 (0.04) | 0.06 (0.04) |
| Owns home outrightj | −0.04 (0.04) | −0.04 (0.04) | −0.03 (.04) | −0.04 (0.04) | −0.04 (0.04) | −0.03 (0.04) |
| Rents homej | −0.24*** (0.05) | −0.04 (0.05) | −0.02 (0.05) | −0.04 (0.05) | −0.04 (0.05) | −0.03 (0.05) |
| Incomek | −0.02 (0.02) | −0.05* (0.02) | −0.05* (0.02) | −0.05* (0.02) | −0.05* (0.02) | −0.05* (0.02) |
| IADL | −0.08** (0.02) | −0.04 (0.02) | −0.04 (0.02) | −0.04 (0.02) | −0.04 (0.02) | −0.05* (0.02) |
| Self-rated health | 0.04* (0.02) | 0.01 (0.02) | 0.01 (0.02) | 0.01 (0.02) | 0.01 (0.02) | 0.01 (0.02) |
| Neuroticisma | −0.33*** (0.03) | −0.23*** (0.03) | −0.23*** (0.03) | −0.23*** (0.03) | −0.23*** (0.03) | −0.23*** (0.03) |
| Neuroticism2, a | −0.08* (0.03) | −0.07* (0.03) | −0.07* (0.03) | −0.07* (0.03) | −0.07* (0.03) | −0.07* (0.03) |
| Wave 2l | −0.05 (0.03) | −0.05 (0.03) | −0.05 (0.03) | −0.05 (0.03) | −0.05 (0.03) | −0.05 (0.03) |
| Wave 3l | −0.15** (0.05) | −0.15** (0.05) | −0.15** (0.05) | −0.15** (0.05) | −0.15** (0.05) | −0.15** (0.05) |
| Model fit | ||||||
| Level 2 variance | 0.67*** | 0.45*** | 0.45*** | 0.45*** | 0.45*** | 0.45*** |
| Level 1 variance | 1.05*** | 0.96*** | 0.95*** | 0.96*** | 0.96*** | 0.95*** |
| Autocorrelation (ρ) | 0.17*** | 0.15*** | 0.15*** | 0.15*** | 0.15*** | 0.14*** |
| F; df | 22.17***; 27 | 56.69***; 30 | 55.25***; 31 | 55.04***; 31 | 55.25***; 31 | 53.83***; 32 |
Notes: IADL = instrumental activities of daily living.
aMean-centered variable.
bReference group is No depression.
cReference group is Male.
dReference group is White.
eReference group is Not Hispanic.
fReference group is Some college.
gReference group is Married.
hReference group is No children.
iReference group is Employed.
jReference group is Paying on a mortgage.
kStandardized variable.
lReference group is Wave 1.
*p < .05, **p < .01, ***p < .001.
Model 2 added the perceived neighborhood quality and family and friend support measures to Model 1. Perceived neighborhood quality was linked with significantly greater social integration (B = 0.62, p < .001). Moreover, daily discrimination was attenuated to non-significance (B = −0.02, p > .05). Supplemental analyses (not shown) indicated that this attenuation was partly due to perceived neighborhood quality, but more strongly driven by family and friend support. The effect of depression was unchanged (B = −0.16, p < .001). Among covariates, the coefficients for less than high school degree, renting one’s home, IADL, and self-rated health were reduced to nonsignificance, whereas income (B = −0.05, p < .05) became significant. Family (B = 0.23, p < .001) and friend support (B = 0.43, p < .001) were both significantly linked with greater social integration.
In Model 3, an interaction between perceived neighborhood quality and age was tested. This interaction (B = −0.01, p < .05) was significant and indicated that the association between perceived neighborhood quality and social integration weakened slightly with age. No significant coefficients were changed from Model 2.
In Model 4, an interaction between perceived neighborhood quality and daily discrimination was tested, but was not significant when added to Model 2.
In Model 5, an interaction between perceived neighborhood quality and depression was tested. This interaction was significant (B = 0.18, p < .05) and indicated that the positive influence of perceived neighborhood quality on social integration was strongest among depressed participants. Once again, no significant coefficients were altered from Model 2.
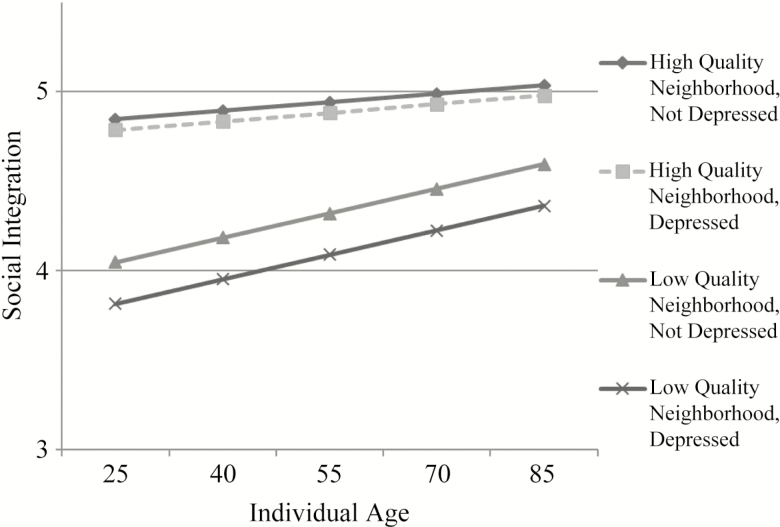
Lastly, in Model 6 the significant interaction terms detected in Models 3 through 5 were simultaneously added to Model 2. All coefficients of interest and all significant covariate coefficients were unchanged from Model 2, with the exception of IADL (B = −0.05, p < .05). The main effects of perceived neighborhood quality (B = 0.58, p < .001), depression (B = −0.14, p < .01), and age (B = 0.01, p < .01) remained significant. Daily discrimination remained non-significant. Moreover, the interactions between perceived neighborhood quality and age (B = −0.01, p < .01) and between perceived neighborhood quality and depression (B = 0.16, p < .05) remained significant. Figure 1 illustrates the intersecting associations of perceived neighborhood quality, depression, and age with social integration over the two-decade study period.
Figure 1.
Perceived neighborhood quality, depression, and social integration over the life course. Note: “High” and “low” values of perceived neighborhood quality defined as ±1 SD. All other covariates set to zero. Y-axis truncated.
Discussion
The present study examined associations between perceived neighborhood quality, daily discrimination, depression, and social integration over a 19-year span among a sample of midlife and older adults. Results established significant longitudinal associations of both perceived neighborhood quality and depression with social integration. Further, perceived neighborhood quality became less influential for social integration with age, but was more influential for social integration among depressed adults. The implications of these findings for theory, future research, and the promotion of effective “aging in place” initiatives are discussed subsequently.
Neighborhood Quality and Social Integration
As anticipated by Hypothesis 1, perceived neighborhood quality was strongly associated with social integration throughout adulthood. Integration within and attachment to one’s social community depends in part upon the perceived quality of one’s physical community (e.g., Bromell & Cagney, 2014; Cramm et al., 2013). Having a neighborhood in which one feels comfortable and secure may facilitate better social relations and interactions, in part by fostering a physical atmosphere in which adults feel safe engaging with others outside of their homes (e.g., Haney, 2007).
Interestingly, perceived neighborhood quality interacted with age, such that links between perceived neighborhood quality and social integration were actually weaker among older participants. This was in contrast to the expectation of Hypothesis 2 that older adults would be more strongly affected by perceptions of their neighborhoods since they spend more time within their neighborhoods and depend more on neighbors for social contact than do adults in midlife (Cornwell et al., 2008; Oswald & Wahl, 2005). Indeed, although prior research concerning neighborhood quality and well-being produced mixed findings, previous studies found evidence of either age-consistent effects (e.g., Stokes, 2019b) or heightened effects among the oldest-old (e.g., Oswald et al., 2011), contrary to the results of this study. This may be due to the use of social integration as an outcome, rather than aspects of psychological well-being (e.g., life satisfaction). Older adults progressively engage in socioemotional selectivity, eliminating relationships, and avoiding contexts that are straining or unfulfilling (Carstensen et al., 2003). It is possible, therefore, that individuals aging in lower-quality neighborhoods compensate for this fact, and rely on alternative—and more positive—networks for their social integration. Future research should further examine the possibility that neighborhood context matters more—or less—for social well-being at later ages.
Daily Discrimination, Depression, and Neighborhood Quality
In keeping with prior research examining physical and psychological well-being (Pascoe & Richman, 2009; Schmitt et al., 2014), this study found that daily discrimination was associated with worse social well-being over a two-decade span, as well. However, this association was attenuated to nonsignificance once perceived neighborhood quality and family and friend support were accounted for, offering only limited support to Hypothesis 1. This finding suggests that experiences of day-to-day discrimination may have limited impact when individuals seek out social support, whether from their neighbors or from family and friends (Bécares et al., 2009; Pascoe & Richman, 2009). Moreover, the effect of daily discrimination on social integration did not vary according to perceived neighborhood quality, failing to offer support for Hypothesis 3.
The deleterious effect of depression on social integration was more robust, however, and was not attenuated by social support measures. This offers support for Hypothesis 1 and coheres with prior research, which indicated that experiencing depression is related with poorer social engagement, less frequent participation in social activities, and more negative views of social acceptance and support (Achterberg et al., 2003; Holtfreter et al., 2017; Kim & Thomas, 2017). In keeping with the person-environment fit perspective, perceived neighborhood quality was significantly more beneficial for social integration among depressed adults, offering support for Hypothesis 4. That is, the harmful effect of depression on social integration was buffered by perceived neighborhood quality (e.g., Holtfreter et al., 2017). As Figure 1 illustrates, depression had little to no effect on social integration among those living in high-quality neighborhoods, but had a clear, if modest, influence on social integration for those reporting poor neighborhood quality. This suggests that perceived neighborhood safety and trust can be protective social resources that may be of particular value among those least likely to engage in social activities and interactions without the right environmental context.
Implications for Research and “Aging in Place”
Social connections, integration, and support are instrumental throughout the life course (e.g., Berkman et al., 2000). As the results of the present study indicate, the promotion of positive social ties and the reduction of negative social interactions and their consequences both depend upon the quality of place, specifically adults’ neighborhoods (Aneshensel, 2009). This makes access to safe, high-quality neighborhood settings a key component for any effective “aging in place” initiative (e.g., Cramm et al., 2013; Oswald & Wahl, 2005; Oswald et al., 2011).
Likewise, although treated as a covariate in this study, stability within neighborhoods appeared as an important element as well. Most older adults who wish to age in place have strong attachments to their physical neighborhoods (Oswald & Wahl, 2005; Oswald et al., 2011), and the results of this study suggest strong social attachments as well. In addition to the average increase in social integration with age detected in this study, there was also a consistent significant association between years lived in current neighborhood and social integration across all six models. That is, social integration did not only improve with age, it also improved with each additional year of residential stability within a neighborhood. If fostering social integration in later life is a priority for successful aging (e.g., Cramm et al., 2013; Stokes, 2019a), then not only access to high-quality neighborhoods, but the ability to remain within such neighborhoods appears crucial.
The effect of residential stability was independent of the influence of perceived neighborhood quality, as well, indicating that stability in one’s neighborhood was beneficial for social integration irrespective of that neighborhood’s perceived quality. In other words: Quality of place matters for social well-being, but so too does consistency and familiarity with said place. Older adults often lack the social resources necessary to initiate new social ties, or rekindle lapsed relationships (Rook, 2009); their neighborhoods may provide just such a resource, particularly if those neighborhoods are long lived in (Cramm et al., 2013; Cornwell et al., 2008). However, future research should also attend closely to ways in which changes to neighborhood features and demographics (e.g., gentrification, redevelopment, depopulation) may affect the association between residential stability and social integration over time, as such changes may reduce the “consistency and familiarity” noted earlier.
Limitations
This study retains a number of limitations. Foremost among these is attrition, particularly since social integration, perceived neighborhood quality, and daily discrimination were correlates of attrition at one or more waves. While this speaks to the importance of these factors for health and longevity, it also raises the risk of potential bias. Although a sensitivity analysis that imputed for missing and attrited cases produced results consistent with those presented, future research analyzing samples that include the oldest-old and collect longitudinal data at shorter intervals to minimize attrition will be required to confirm the validity of this study’s findings.
Further, adults select non-randomly into neighborhoods, and are differentially exposed to discrimination and depression across the life course (e.g., Pascoe & Richman, 2009; Stokes, 2019b). The all-cause discrimination measure may also overlook substantive differences between various forms and reasons for discrimination, and it is unclear whether discrimination and/or social engagement occurred within the neighborhood or elsewhere. Additionally, the items of interest in this study were self-reported. Although both subjective and objective aspects of neighborhood quality are known to have unique influences on well-being (e.g., Haney, 2007), certain neighborhood characteristics may result in differing evaluations of neighborhood quality across groups (e.g., Wahl et al., 2012). Future studies using nested data from individuals with varying characteristics who share neighborhood settings, and which utilize objective neighborhood data alongside self-reports, will be better suited to identifying neighborhood features and amenities that promote better perceptions of neighborhood quality, reduce or buffer against experiences of discrimination and depression, and foster greater social integration (both objectively and subjectively) across different social and demographic groups (e.g., Bécares et al., 2009; 2012; Oswald et al., 2011).
Conclusion
Despite these limitations, the present study offers new and interesting information concerning the importance of physical place for adults’ social well-being. Specifically, this study revealed that perceptions of neighborhood quality influence social integration throughout adulthood, with a slight attenuation of this effect with age. Moreover, depression undermines adults’ social integration consistently across the age range. Perceived neighborhood quality, however, serves as a protective social resource that buffers against the negative influence of depression on social integration. Taken together, these results underscore the importance of neighborhood setting for social well-being across the life course, and offer useful information for theory, future research, and the promotion of successful “aging in place” initiatives.
Funding
Since 1995, the MIDUS study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), and National Institute on Aging (U19-AG051426).
Conflict of Interest
None reported.
References
- Achterberg W., Pot A. M., Kerkstra A., Ooms M., Muller M., & Ribbe M (2003). The effect of depression on social engagement in newly admitted Dutch nursing home residents. The Gerontologist, 43, 213–218. doi:10.1093/geront/43.2.213 [DOI] [PubMed] [Google Scholar]
- Aneshensel C. S. (2009). Neighborhood as a social context of the stress process. In Avison W. R., Aneshensel C. S., Schieman S., Wheaton B. (Eds.), Advances in the Conceptualization of the Stress Process (pp. 35–52). New York, NY: Springer. [Google Scholar]
- Bécares L., Shaw R., Nazroo J., Stafford M., Albor C., Atkin K.,…Pickett K (2012). Ethnic density effects on physical morbidity, mortality, and health behaviors: A systematic review of the literature. American Journal of Public Health, 102, e33–e66. doi:10.2105/AJPH.2012.300832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L., Nazroo J., & Stafford M (2009). The buffering effects of ethnic density on experienced racism and health. Health & Place, 15, 670–678. doi:10.1016/j.healthplace.2008.10.008 [DOI] [PubMed] [Google Scholar]
- Berkman L. F., Glass T., Brissette I., & Seeman T. E (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51, 843–857. doi:10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bromell L., & Cagney K. A (2014). Companionship in the neighborhood context: Older adults’ living arrangements and perceptions of social cohesion. Research on Aging, 36, 228–243. doi:10.1177/0164027512475096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen L. L., Fung H. H., & Charles S. T. (2003). Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion, 27, 103–123. doi: 10.1023/A:1024569803230 [Google Scholar]
- Charles S. T. (2010). Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin, 136, 1068–1091. doi:10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B., Laumann E. O., & Schumm L. P. (2008). Thesocial connectedness of older adults: A national pro file. American Sociological Review, 73, 185–203.doi:10.1177/000312240807300201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm J. M., van Dijk H. M., & Nieboer A. P (2013). The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. The Gerontologist, 53, 142–152. doi:10.1093/geront/gns052 [DOI] [PubMed] [Google Scholar]
- Haney T. J. (2007). ‘Broken windows’ and self-esteem: Subjective understandings of neighborhood poverty and disorder. Social Science Research, 36, 968–994. doi:10.1016/j.ssresearch.2006.07.003 [Google Scholar]
- Holtfreter K., Reisig M. D., & Turanovic J. J (2017). Depression and infrequent participation in social activities among older adults: The moderating role of high-quality familial ties. Aging & Mental Health, 21, 379–388. doi:10.1080/13607863.2015.1099036 [DOI] [PubMed] [Google Scholar]
- Keyes C. L .M. (1998). Social well-being. Social Psychology Quarterly, 61, 121–140. doi: 10.2307/2787065 [Google Scholar]
- Kim D. (2008). Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews, 30, 101–117. doi:10.1093/epirev/mxn009 [DOI] [PubMed] [Google Scholar]
- Kim S., & Thomas P. A (2017). Direct and indirect pathways from social support to health? The Journals of Gerontology: Series B. doi:10.1093/geronb/gbx084 [DOI] [PubMed] [Google Scholar]
- Lachman M. E., & Weaver S. L (1997). The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Waltham, MA: Brandeis University. [Google Scholar]
- Moorman S. M., Stokes J. E., & Morelock J. C (2017). Mechanisms linking neighborhood age composition to health. The Gerontologist, 57, 667–678. doi:10.1093/geront/gnv687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald F., Jopp D., Rott C., & Wahl H. W (2011). Is aging in place a resource for or risk to life satisfaction? The Gerontologist, 51, 238–250. doi:10.1093/geront/gnq096 [DOI] [PubMed] [Google Scholar]
- Oswald F., & Wahl H-W (2005). Dimensions of the meaning of home in later life. In Rowles G. D. & Chaudhury H. (Eds.), Home and Identity in Later Life: International Perspectives (pp. 21–46). New York: Springer. [Google Scholar]
- Pascoe E. A., & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135, 531–554. doi:10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L. I., Lieberman M. A., Menaghan E. G., & Mullan J. T (1981). The stress process. Journal of Health and Social Behavior, 22, 337–356. doi:10.2307/2136676 [PubMed] [Google Scholar]
- Rook K. S. (2009). Gaps in social support resources in later life: An adaptational challenge in need of further research. Journal of Social and Personal Relationships, 26, 103–112. doi:10.1177/0265407509105525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston P. (2005). Multiple imputation of missing values: Update of ice. Stata Journal, 5, 527–536. doi: 10.1177/1536867X0500500404 [Google Scholar]
- Ryff C. D., Almeida D. M., Ayanian J. S., Binkley N., Carr D. S., Coe C.,…,Williams D (2017). Midlife in the United States (MIDUS 3), 2013–2014. ICPSR36346-v6. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2017-11-21. [Google Scholar]
- Schmitt M. T., Branscombe N. R., Postmes T., & Garcia A (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140, 921–948. doi:10.1037/a0035754 [DOI] [PubMed] [Google Scholar]
- Steger M. F., & Kashdan T. B (2009). Depression and everyday social activity, belonging, and well-being. Journal of Counseling Psychology, 56, 289–300. doi:10.1037/a0015416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes J. E. (2019a). Social integration, perceived discrimination, and self-esteem in mid- and later life: Intersections with age and neuroticism. Aging & Mental Health, 23, 727–735. doi:10.1080/13607863.2018.1450834 [DOI] [PubMed] [Google Scholar]
- Stokes J. E. (2019b). Trajectories of perceived neighborhood quality across the life course: Sociodemographic determinants and implications for well-being. Social Science Research, 79, 181–193. doi:10.1016/j.ssresearch.2018.11.001 [DOI] [PubMed] [Google Scholar]
- Stokes J. E., & Moorman S. M (2016). Who are the people in your neighborhood? Neighborhood age composition and age discrimination. Social Psychology Quarterly, 79, 68–80. doi:10.1177/0190272515626569 [Google Scholar]
- Wahl H. W., Iwarsson S., & Oswald F (2012). Aging well and the environment: Toward an integrative model and research agenda for the future. The Gerontologist, 52, 306–316. doi:10.1093/geront/gnr154 [DOI] [PubMed] [Google Scholar]
- Wang P. S., Berglund P., & Kessler R. C (2000). Recent care of common mental disorders in the United States: Prevalence and conformance with evidence-based recommendations. Journal of General Internal Medicine, 15, 284–292. doi:10.1046/j.1525-1497.2000.9908044.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Yan Y., Jackson J. S., & Anderson N. B (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2, 335–351. doi:10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]