Abstract
Background and Objectives
Frail and disabled individuals, including assisted living (AL) residents, are embedded in care convoys composed of dynamic networks of formal and informal care partners. Yet, little is known about how care convoys operate over time, especially when health changes occur. Thus, our aim was to provide an in-depth understanding of care convoy communication during times of residents’ health changes in AL.
Research Design and Methods
Data for this analysis come from a Grounded Theory study that involved 50 residents and their care convoy members (n = 169) from 8 diverse AL communities followed over 2 years. Researchers conducted formal and informal interviewing, participant observation, and record review.
Results
We identified “communicative competence” as an explanatory framework in reference to a resident’s or care partner’s ability, knowledge, and action pertaining to communication and health change. Individual and collective competencies were consequential to timely and appropriate care. Communication involved: identifying; assessing significance; informing, consulting or collaborating with others; and responding to the change. Variability in communication process and properties (e.g., pace and timing; sequencing, timing, content, and mode of communication) depended on multiple factors, including the nature of the change and resident, informal and formal caregiver, convoy, AL community, and regulatory influences.
Discussion and Implications
Formal and informal care partners need support to establish, enhance, and maintain communicative competence in response to health changes. Findings reinforce the need for timely communication, effective systems, and well-documented accessible health care directives and have implications that are applicable to AL and other care settings.
Keywords: Care convoys, Health communication, Long-term care
Although assisted living (AL) is primarily a social, not medical, care setting, AL residents experience increasing frailty and have significant health care needs (Khatutsky et al., 2016; Kistler et al., 2017). Most have multiple chronic conditions, with cognitive impairment estimates varying between 40% (Caffrey et al., 2012) and 70% (Zimmerman, Sloane, & Reed, 2014). Frequent health status changes occur, including falls with injuries, that lead to emergency department (ED) visits, hospitalization, and time in nursing or rehabilitation centers (Kemp et al., 2018; Khatutsky et al., 2016). AL also increasingly is where residents age in place, receive end-of-life care, and die (Ball, Kemp, Hollingsworth, & Perkins, 2014; Vandenberg et al., 2018).
As with other long-term care recipients, AL residents are embedded in care convoys (i.e., networks) composed of residents and their formal and informal care partners, who may change over time in number, configuration, and care roles in response to residents’ changing health status and care needs and may provide assistance with instrumental activities of daily living, activities of daily living, socio-emotional support, monitoring, and health care (Kemp, Ball, & Perkins, 2013). Most hands-on care in AL is provided by unlicensed personal care aides (66%) and certified nursing assistants (34%) (Kelly, Morgan, Kemp, & Deichert, 2018). Although licensed nurses are a growing presence in AL, most states’ AL regulations prohibit AL staff from providing skilled care, while many states are expanding care levels through regulatory and policy changes (Carder, O’Keeffe, & O’Keeffe, 2015). Recent research demonstrates the growing complexity of health care in AL, including an AL study in 22 states that documents service types, ranging from basic (e.g., vital signs) to more complex (e.g., injections) and specialized (e.g., x-ray), with registered and practical nurses being used extensively (Beeber et al., 2014). National research (Harris-Kojetin et al., 2016) reports the widespread availability of nursing, pharmacy, podiatry, social work, mental health, dental, and hospice services, as well as physical, occupational, and speech therapies in the majority of AL communities.
Our in-depth, longitudinal research (Kemp, Ball, & Perkins, 2019, p .647) shows that residents’ health care in AL largely involves four domains (routine, acute, rehabilitative, and end-of-life), is individualized, and involves an “evolving mosaic” of arrangements, varying by type, frequency, amount, timing, location, provider, and outcomes (Kemp et al., 2019, p. 4). This research illuminates the centrality of informal caregivers in handling health care needs, particularly service access. AL staff typically assist with medication management, health monitoring, and therapeutic support, and various external providers contribute to the management of chronic conditions and identification of acute problems. Separate analysis aimed at understanding convoy function, labels AL residents’ care convoys as being cohesive, fragmented, or discordant, largely based on consensus surrounding care goals and the overall effectiveness of convoy communication and collaboration among residents and their care partners (Kemp et al., 2018).
Convoy member communication, particularly surrounding residents’ health status changes, is a critical component of AL care delivery (Kemp et al., 2019; Kemp et al., 2018). Other research, in care settings ranging from home (Ball & Whittington, 1995) to nursing home (Powell et al., 2018) and hospital (Coiera, 2006), also finds communication among care partners to be critical to care delivery outcomes. A key factor dictating communication’s significance is the complexity of care systems, especially those encompassing health care (Institute of Medicine, 2013). The concept of communication space, described as “that portion of the total number of information transactions that involve interpersonal connection” (Coiera, 2006, p. 90), illuminates the relationship between system complexity and communication. Communication can involve multiple modes, with the possible number of conversations occurring at any one time determined by the number of people needing to communicate. Even small care teams can create large and complex communication spaces (Coiera, 2006). AL is an increasingly complex health care environment and communication space where residents interact with a range of health care professionals across multiple disciplines, together with their informal and AL care partners, augmenting the need for information sharing among care providers (Kemp et al., 2019; Kemp et al., 2018).
Communication efficacy in care systems has bases beyond system complexity, including characteristics of providers and recipients, their relationships, and modes of communication (Gordon, Deland, & Kelly, 2015; Vermeir et al., 2015). Health care research underscores the importance of care professionals’ communication competence, including modes of speaking and listening, for patients’ health literacy (Belim & De Almeida, 2018). Declines in ability to hear, remember, and process information common with aging can hinder older persons’ communication competence and overall communication effectiveness (Nussbaum, Baringer, & Kundrat, 2003).
Here we use data from the 5-year study, “Convoys of Care: Developing Collaborative Care Partnerships in Assisted Living,” to build on and extend our previous work examining resident care in AL generally (Kemp et al., 2018) and with a focus on health care delivery (Kemp et al., 2019). Our own and other AL research establishes the increasing frailty, comorbidity, and health status instability of AL residents, along with the growing presence of onsite health care delivery, and the escalating complexity of care networks, all lending greater significance to communication among care partners for care outcomes. No research to date, however, focuses on the communication processes surrounding residents’ health change. Thus, our specific aims are to: (a) understand the processes of communication when residents experience changes in their physical and mental health; (b) identify the factors influencing these communication processes; and (c) determine the relationships between communication processes, factors, and outcomes.
Methods
Our research is guided by a grounded theory approach (Corbin & Strauss, 2015), with simultaneous data collection, hypothesis generation, and analysis. Consistent with this approach, this analysis builds cumulatively on our previous analysis. The study was approved by Georgia State University’s Institutional Review Board. All sites and participants have pseudonyms to provide anonymity.
Study Setting and Participants
The study was set in eight care communities, purposively selected to provide maximum variation (Patton, 2015) in ownership, capacity, licensing, location, resident profile, resources, and availability of memory care (see Table 1). Seven were licensed as personal care homes and one as an AL community, which in the state of Georgia, allows higher levels of resident care. Executive directors provided written consent for access.
Table 1.
Select Study Home Characteristics by Setting
| Data collection period 2013–2015 | Data collection period 2016–2018 | |||||||
|---|---|---|---|---|---|---|---|---|
| Hillside | Feld House | Garden House | Oakridge Manor | Camellia’s Cottage | Thames Place | Magnolia Gardens | Riverview Estates | |
| Capacity | 11 | 46 | 54 | 99 | 2 | 12 | 19 | 48 |
| Ownership | Private | Foundation | Private | Corporate | Private | Private | Private | Corporate |
| Licensurea | PCH | PCH | PCH | ALC | PCH | PCH | PCH | PCH |
| Location | Rural | Suburban | Small town | Urban | Urban | Urban | Urban | Suburban |
| MCU | No | No | Yes | Yes | No | No | No | Yes |
| Monthly fee range (U.S.$) | 1,800– 4,000 | 3,145–5,505 | 2,650– 4,050 | 2,595–5,973 | 1,000– 1,800 | 1,750–2,250 | 1,995– 3,049 | 2,750– 4,750 |
| Resident race/ culture | All White | All White/ Jewish | Most White | All African American | African American | African American and White | African American and White | Most White |
Notes: MCU = memory care unit.
aGeorgia’s licensing categories include: Assisted Living Community (ALC) and Personal Care Home (PCH).
Participants included 50 focal residents and 169 care convoy members, including 91 informal caregivers, 49 AL administrative and care staff, and 29 formal external care partners. Table 2 provides select personal and health characteristics of residents; Table 3 describes convoy member participants by relationship type.
Table 2.
Residents’ Select Personal and Health Characteristics at Baseline (N = 50)
| Resident characteristic | Range | Mean/median |
|---|---|---|
| Age (years) | 57–96 | 82/85 |
| N | % | |
| Gender | ||
| Female | 29 | 58 |
| Male | 21 | 42 |
| Marital statusa | ||
| Married | 7 | 14 |
| Widowed | 29 | 58 |
| Divorced/separated | 11 | 22 |
| Never married | 3 | 6 |
| Race | ||
| White | 34 | 68 |
| Black | 15 | 30 |
| Asian | 1 | 2 |
| Educationa | ||
| Less than high school | 2 | 4 |
| High school diploma | 20 | 40 |
| Some college | 9 | 18 |
| College | 7 | 6 |
| Post graduate | 11 | 22 |
| Care needs | ||
| Needs help with three or more ADLs | 28 | 56 |
| Needs help with three or more IADLs | 38 | 76 |
| Needs help with medications | 41 | 81 |
| Use of wheelchair | 17 | 34 |
| Health conditions | ||
| High blood pressure | 34 | 68 |
| Dementiab | 29 | 58 |
| Heart disease | 18 | 36 |
| Depression | 14 | 28 |
| Osteoarthritis | 18 | 36 |
| Diabetes | 9 | 18 |
| Emphysema, chronic bronchitis, COPD | 5 | 10 |
| Cancer | 7 | 14 |
| Stroke | 8 | 16 |
| Other conditions | 47 | 94 |
| Total number of comorbidities among residents | Min–max | Mean per resident |
| 283 | 1–10 | 5.66 |
Notes: ADL = activities of daily living; COPD = chronic obstructive pulmonary disease; IADL = instrumental activities of daily living.
aOne missing case.
bDementia diagnoses were as follows: unspecified dementia (n = 20); Alzheimer’s disease (n = 2); Lewy body dementia (n = 3); Parkinson’s-related (n = 1); Vascular (n = 2); Behavior variant frontotemporal dementia (n = 1).
Table 3.
Care Convoy Members by Participant Type (N = 169)
| Convoy member type | N | C% |
|---|---|---|
| Formal convoy members | ||
| Assisted living workers | ||
| Executive directors | 10 | 20 |
| Licensed nurse | 2 | 4 |
| Resident services directors | 4 | 8 |
| Direct care workers/ medication techs | 19 | 39 |
| Activity personnel | 9 | 18 |
| Maintenance/transportation | 2 | 4 |
| Housekeeping/food services | 3 | 6 |
| 49 | 100 | |
| External care workers | ||
| Physicians | 3 | 10 |
| Registered nurses | 2 | 7 |
| Nurse practitioners | 3 | 10 |
| Physical, occupational, speech therapists | 6 | 20 |
| Hospice personnel | 13 | 27 |
| Private care aides | 1 | 3 |
| Mental health professionals | 1 | 3 |
| 29 | 100 | |
| Informal convoy members | ||
| Daughters | 32 | 35 |
| Sons | 13 | 14 |
| Spouses | 3 | 3 |
| Parents | 1 | 1 |
| Grandchildren | 6 | 7 |
| Siblings | 7 | 8 |
| Friends | 9 | 10 |
| Other kina | 18 | 20 |
| Volunteers | 2 | 2 |
| 91 | 100 | |
| Informal participants per resident convoy | Min–max | Mean per resident |
| 0–5 | 1.82 |
Note: aIncludes: step-children (1); daughters- (5), sons- (2), sisters- (2), brother- (1) and mothers- (1) in-law; nieces (2); aunts (1); uncles (1); cousins (1); ex-wife (1).
Data Collection
Between 2013 and 2018, trained gerontologists and sociologists, collected data in each site for 2 years using participant observation, informal and formal interviewing, and review of residents’ records. Initially, we interviewed the executive director to learn about the home’s residents, staff, organizational characteristics, and care environment. Participant observation and informal interviewing of residents, staff, and any visitors were ongoing. Formal interviews with residents inquired about histories, personal and health characteristics, relationships, and care needs and experiences. Convoy member interviews addressed their care roles and relationships and provided additional resident information. Earlier work (Kemp et al., 2017) provides detailed information about consent and assent procedures, including for individuals without consent capacity (n = 15). We followed residents and their care convoys for 2 years or until they were discharged (n = 2), moved out (n = 12), or died (n = 9), attempting to interview all informal caregivers and a range of AL staff and external care providers connected to focal residents. Consent was an ongoing process. While engaged in participant observation researchers sought assent from individuals to speak with or sit near them and entered private spaces such as residents’ apartments only with their permission. Researchers made a total of 1,561 field visits with 3,738 observation hours, all recorded in detailed notes, and after formal interviews followed up with residents and staff weekly and twice monthly, when possible, with other convoy members to monitor health status and care need changes. Ongoing record review added information about health conditions, care plans, and care providers.
Data Analysis
Following Corbin & Strauss’ (2015) Grounded Theory Method (GTM), we used a three-pronged coding procedure beginning with line-by-line “open coding” of all data pertaining to communication in the context of resident change. Initial codes, included, for example, “acute change,” “experiencing,” or “recognizing change,” “waiting to see,” “acting quickly,” “seeking help,” and “getting appropriate care.” Next, we used axial coding to connect categories and link data, indicating communication processes, conditions, contexts, and consequences. We found, for instance, that regulatory influences intersected with AL residence, convoy, and caregiver and resident factors and the health change itself influenced communication processes and outcomes. In our final analytic stage, we identified the centrality of “communicative competence” in explaining communication processes that surround resident change and organized our categories around this core category.
Consistent with GTM, we revisited the literature and found that anthropologist Dell Hymes (1966) coined the term “communicative competence” in reference to the abilities and knowledge involved in human communication. Providing a theory of sociolinguistics, Hymes emphasized the importance of individuals’ language skills and competence for interacting appropriately given specific participants and social scenario. Here, we borrow and expand communicative competence, moving it beyond language and interaction to also include knowing what information to communicate, when, to whom, and how, and situating competence in the dynamic and complex contexts of long-term care and care convoys (i.e., networks).
Findings
Communicative Competence
Our core category, communicative competence, offers a framework for explaining the processes and outcomes associated with the physical and mental health status changes experienced by AL residents within the context of communication. Communicative competence refers to residents’ or care partners’ actions pertaining to communication when resident health changes occur. Individual and collective competencies of residents and caregivers were consequential to residents’ receipt of timely and appropriate care in situations of health transitions. Competencies ranged from low to high and fluctuated over time by resident and caregiver, based on multiple influential factors we identified.
Resident Health Changes
Changes in health status were common across sites, occurring among 47 of 50 resident participants. Those with no change relocated to different AL residences between months 9 and 10 of data collection. Health changes occurred singly and in combination and varied on multiple dimensions, including: body state (physical or mental); cause (illness or injury); organ system involved (e.g., respiratory, circulatory, gastrointestinal); pace of onset (gradual to acute); degree of severity (serious to inconsequential), how change manifested (visibility of signs and symptoms), and, if a discrete event, location and timing.
Our data provide abundant examples of residents’ health changes across these dimensions, including: Dot, a resident with a chronic vein condition, who over 1 month, experienced gradual, escalating swelling and pain in her leg, the result of an undiagnosed break sustained during an off-site fall, which ultimately left her immobile and requiring surgery; Doris whose sudden onset of disorientation and hallucinations were traced, after a few days, to medication prescribed for an acute illness; Gerald, a resident with dementia, who fell in his room one night, resulting in a broken hip, hospitalization, and eventual death; and Joel, who vomited during dinner and was hospitalized and diagnosed with a hiatal hernia. The nature of change had significant influence on the response to and ultimate outcomes of change, but, regardless of specifics, care partner communication figured prominently in how resident health changes were handled and their consequences.
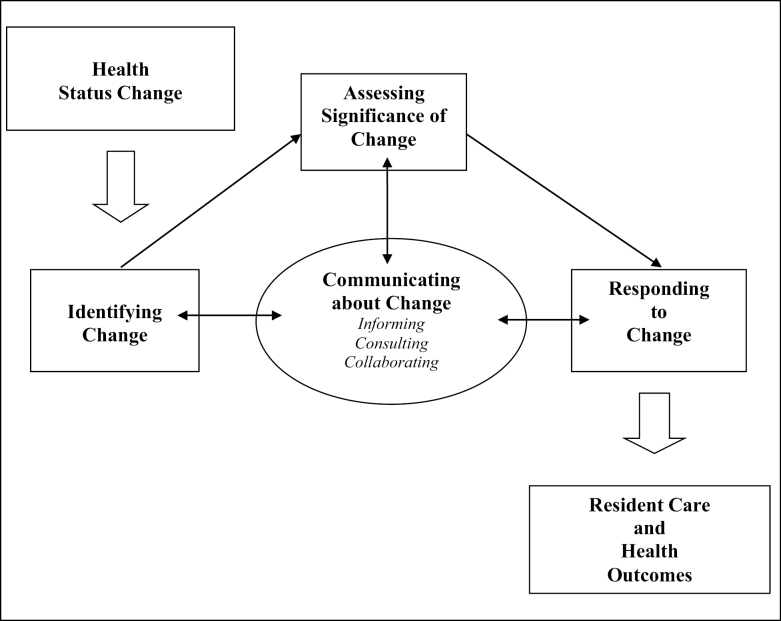
Communication and Health Status Change
As Figure 1 shows, communicating about residents’ health status changes involved four fundamental and interrelated processes: (a) identifying change; (b) assessing the significance of change; (c) responding to change; and (d) informing, consulting, or collaborating regarding change. Despite overall commonality of processes, individual situations varied in the occurrence, character, and sequencing of processes. Communication, in the form of informing, consulting, and collaboration, often was integrated into any or all of the other three processes, shaping the evolution of each and the outcomes for residents and care convoys. As noted, the nature of the change was fundamental to the evolution and character of each process. Other influences included the content and mode of communication and the configuration of care partners involved. These and numerous additional factors pertaining to residents and their care partners, AL homes, and the wider community will be elucidated subsequently in the discussion of the four processes.
Figure 1.
Health status change and the communication process.
Identifying
Health status change was identified through a resident experiencing change and the resident and/or others (e.g., co-residents, AL staff, informal caregivers, external care workers) being aware of various signs and symptoms accompanying change. These indicators ranged from subtle to overt, depending on the type and source of change. Changes associated with acute illness or injury (e.g., cardiac arrest, fractures) generally were more readily identified than those with subtler signs related to chronic conditions, such as gradual weight loss or increased confusion of a resident living with dementia. Other factors, for instance when and where a change occurred and who was present, also could affect awareness. For example, when Doris, fell in her room in the afternoon, a passing resident witnessed the event through her open door. Jean’s stroke, however, happened at night with no one aware of her condition until morning.
Expressions of pain were common among residents, frequently signifying flare-up of chronic conditions, such as arthritis, or acute problems, for example related to infections or injuries. Other common signs of acute or chronic illness included fever, coughing, wheezing, and vomiting. Sometimes residents failed to communicate less apparent changes, withholding information for fear of burdening staff or, more commonly, family. Such was the situation of Alma, who routinely concealed pain to avoid burdening her only son, and Joel, who neglected reporting a cough, delaying a pneumonia diagnosis. Although both residents had cohesive convoys, they also had strong values for independence, which sometimes impeded communication about health changes.
Change also was identified by care workers during routine monitoring of vital signs and blood sugar, oxygen, and weight levels. Among convoy members, AL staff, owing to their regular presence, were most likely to identify change, although our data show the full spectrum of caregivers were involved in identification, especially when AL staff overlooked, failed to understand, or ignored signs of change or residents had difficulty communicating. For example, Mable’s hospice nurse discovered her higher than normal blood pressure during a routine visit. Informal caregivers also were integral. Riverview resident Peter’s wife noticed he had not eaten and seemed “sick” and alerted the resident services director; his fever was 103. In the subsequent ED visit, doctors suspected a possible stroke and multiple transient ischemic attacks; Peter was hospitalized for 2 weeks and ultimately transferred to a skilled nursing facility.
Assessing significance of change
Once identified, the significance of the change was assessed, typically based on type and severity, to determine the appropriate response, if any. If only the resident was aware of a change, she or he initially made an independent assessment before deciding whether or not to inform and involve others. An example is Jane, who, after falling in her bathroom at night, decided no help was needed. The following day, however, an AL care worker noticed blood on her sheet from a cut on her arm, questioned her about the injury, and consequently involved Jane’s daughter and hospice nurse. As expected, health changes of greater severity, particularly pertaining to physical problems, such as Beatrice’s cardiac arrest, were more readily assessed and understood. Assessment of the significance of cognitive or psychological change often required consultation, as when Jane exhibited increased confusion related to a urinary tract infection (UTI); assessment involved consultation with long time AL worker, Sheila, and Jane’s daughter, whose familiarity with Jane’s typical behaviors and routines enhanced detection competence. Similarly, a care worker’s observation of Paul’s refusal of a favorite food led to a UTI diagnosis. Care partner health literacy and staffing levels also affected understanding of change significance, particularly subtle change, for example, when Jean manifested changes days prior to her stroke. A fieldnote memo indicates the interplay of factors contributing to outcomes:
Staff had noticed small changes but not alerted anyone. When I asked why Jean was [using] a wheelchair last week, Joanne [AL staff] had just told me that “her legs did not work.” This also is the time that Florence [Resident Services Director] was gone. . . . This situation is a good example of lack of communication about health changes. I also wonder whether if Jean had not been taken off of hospice if her nurse would have noticed that she had the smaller strokes and prevented the big one. She went off [hospice] the end of February and died less than a month later.
Responding
As previous examples illustrate, responses to change were formulated and enacted by residents and care partners. The nature of the response—who, when, where, how—depended on a combination of factors, including the type, severity, timing, and location of the change, who was involved in identification and assessment, and residents’ care goals and plans. If a change was deemed insignificant or non-addressable, no further action was taken, as with Mable after a fall. Although she suffered bruising, AL staff, in consultation with her daughter, decided not to seek medical care. No response had variable outcomes, in some cases preventing ED visits, often difficult for older, frail residents (Kemp et al., 2018). However, sometimes inaction frustrated residents and led to suffering or avoidable adverse events. For instance, Leonard, with considerable disability from cerebral palsy, routinely complained about pain to staff, family and friends, and doctors, despite pain specialist visits and pain medications. He said, “I don’t think I can stand this pain—it is all I think about. I am tired of [living here] and I am tired of hearing people say, ‘just think of something else instead of your pain.’ You can’t do that when the pain is this severe.” In other situations, the response to change was “wait and see,” which frequently involved monitoring symptom escalation or abatement or reassessment and further consultation within the convoy.
In certain scenarios, especially in the “case of an accident or sudden adverse change” Georgia Department of Community Health (2013) regulations stipulate that, “a home must take the actions appropriate to the specific circumstances to address the needs of the resident.” In critical situations, for example accidents with injury or acute illness with symptoms such as unresponsiveness, slurred speech, respiratory distress, or chest pain, 911 was called and the resident typically was taken to the ED. One care worker explained:
The rule is if you have like the person fell, they have a broken leg, you can tell sometimes, you open the door, you can tell that one leg is shorter than the other. Or the person tells you, “I can’t move. I hurt my hip.” Right there, then, something is wrong so we don’t move them. One of us, or any of us working, when we get on the phone and call the family . . . and we call 911. We call [management] to let them know. If the persons on hospice, we don’t call 911 unless there’s a broken bone. We call the hospice nurse and they tell us what to do.
State regulations require documentation of accidents or sudden adverse changes and their response. Hospice regulations had specific protocols, with hospice personnel determining the final response. When Gerald fell and broke his hip, the hospice nurse was notified first and took no further action. However, when his daughter visited later, she determined Gerald was in significant pain and sent him to the hospital, where his hip was repaired.
Informing, consulting, or collaborating
As the aforementioned examples show, the processes of identifying, assessing, and responding to health changes often interrelate and include communication in the form of informing, consulting, and collaborating. We observed multiple communication modes, with in-person and phone being most common, however, E-mail, letter- and note-writing, texting, and video-chatting also were used, typically among formal and informal care partners. In some informal convoys, communication was rare except during health crises.
Residents frequently alerted care staff or called informal caregivers, often depending on the type or severity of the problem and residents’ communication ability. For example, when Doris broke a tooth, she called her son who arranged for dental care. However, cognitive or physical impairment frequently impeded residents’ communication roles, as illustrated by Rachel, a resident with dementia who experienced a choking episode during lunch, described in fieldnote data:
One of the care staff from memory care ran in calling out to Sheila to come and help. She said she thought someone must have fallen but when she got there she saw Rachel struggling to breathe and turning colors so she immediately did the Heimlich. . .
After staff intervention, 911 and Rachel’s daughter were called. According to her daughter, “The staff at the Riverview literally saved her life. . . . She choked, quit breathing, and went unconscious. Fortunately, they were able to dislodge the food and the paramedics took it from there.”
Communication, and thus response, about change was not always immediate, as with Roger, a Garden House resident with congestive heart failure. He hesitated to divulge changes when his daughter was out of town, including when he failed to tell her and staff “the whole story” about how he was feeling. He noted, “I should have done it sooner, but they [staff] came in and we decided it was 911.”
The four largest communities had emergency call systems, where residents wore pendants with a button to push for assistance, including in emergencies. Wallace at Riverview reported using his “when I passed out or came close to it,” yet residents often forgot to wear or use them, including Garden House resident Doris, whose daughter routinely reminded, “You are supposed to have your alert button with you all the time.”
When AL care workers were the identifiers, they often communicated with the resident to further assess the change before involving other convoy members, usually AL management and family members, and, in acute situations, emergency or other external health care professionals. In the case of Jane’s UTI, the AL care worker first informed Jane’s daughter and the med tech on duty, who then consulted with Jane’s hospice nurse, who arranged for a urine test and subsequent antibiotic treatment. Irrespective of the identifier, informing, consulting, and collaborating among convoy members often were central to both assessing significance and determining whether and how to respond.
Informing and consulting did not always generate consensus on the nature of change or the best response, including in generally cohesive convoys. For instance, we observed lack of agreement in Roberta’s otherwise cohesive convoy when a rash surfaced on her leg. Fieldnote data explain:
Sally [local daughter] took a photo of it and sent it to Barbara [out-of-state daughter] who began “yelling” at Sally “via text” telling her “Take mom to the hospital immediately.” Sally said, “Barbara’s not here. She doesn’t know. I’ve now learned not to take pictures. Barbara overreacted and got on the phone to her daughter who’s a physician’s assistant and she called Daddy and told him to get her to a hospital. Daddy was hopping mad. . . . Neither one of us thought it was a good idea to take her to the hospital. Anyway, I’ve learned my lesson. No more photos.”
Roberta’s doctor prescribed a topical medication and the rash disappeared without a hospital visit. How, what, to whom, and when one communicates all are potentially consequential as a care partners interpret and negotiate a response to residents’ health change.
In emergency situations, residents’ advance directives were not always communicated and followed, as with Beatrice’s cardiac arrest, when despite her “do not resuscitate” (DNR) order, emergency medical technicians were summoned and she was taken to the ED and intubated before her family could be notified. Another situation was reported by Cassie, a care manager:
Eight-thirty that night I get a call from the staff about Josie [who], they sent out [but] weren’t supposed to send out because she has a DNR. I’m chasing the ambulance to get her from the hospital . . . we [didn’t] actually have the signed paperwork. . . . The [informal caregiver] who had that was out of town. . . . I called the resident’s nurse practitioner, [who] said, “Go get her. I can vouch for this. Go get her.” I did, but [calling 911] was really a difference of opinion between staff. . . . Josie passed out and fell and then immediately was back at it. The med tech didn’t wanna send her. The med tech had me on the phone while the other person already called 911. . . . Once they got out here the staff were back and forth. I had already said don’t send her. The paramedic was like, “Better safe than sorry. I’m taking her.”
When Cassie arrived at the hospital, Josie had been admitted and further explained that hospital staff “weren’t even gonna see her because during all the chaos staff didn’t send the paperwork that gave permission for her to be in the hospital without another person present and because she had dementia they can’t do anything unless they have someone present.” In this instance, confusion, differing opinions, and a lack of documentation and communication led to the unnecessary transportation of a frail resident to the ED and a brief hospital admission, both potentially frightening and disorienting.
In many instances, convoy member communication and collaboration during health status changes were successful. Fieldnote data show collaboration among multiple care partners with positive outcomes for Doris, who had an injury in her room:
She fell asleep and her book fell off of her lap and somehow the cover created a paper cut on her leg. She said it bled a lot and Melanie [administrator] and Sally [LPN] both came to attend to her. They called her son Ross, who stopped by after work. Sally told me she thought it should have stitches but Ross did not think so and since he is a doctor she deferred to him . . . Sally said that he had put a dressing on her leg . . . Doris’s doctor had come by and ordered home health to come out and change the dressing.
Communication among care partners shaped responses to health changes, affecting the timing and appropriateness of care, both influential for residents’ health experiences and outcomes and care partners’ involvement in the care process.
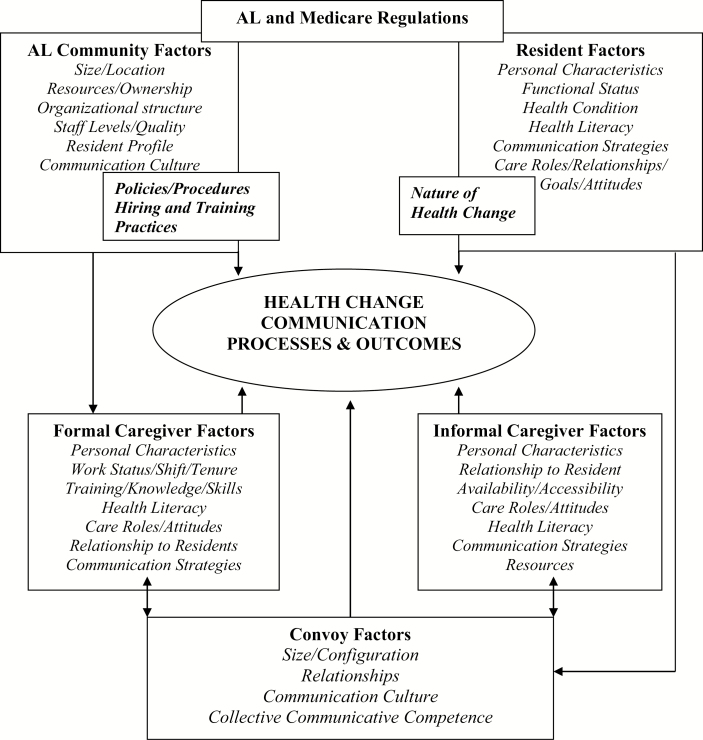
Influential Factors
Illustrated in Figure 2, our analysis identified multiple interrelated multilevel factors that affect the four processes surrounding change and the outcomes and pertained to individuals, namely residents and their care partners, care convoys, AL homes, and the wider community. The nature of the health change exerts fundamental influence. Other resident factors include: personal characteristics, such as age, gender, race, class, culture, education, religion; health condition; physical and cognitive function and health knowledge; and relationship quality; and care roles, goals, and attitudes. Informal and formal caregiver factors relate to: availability and accessibility; care roles and attitudes; health knowledge and skills; relationship with resident. Important convoy factors include: the number, configuration, and relationships of convoy members; as well as communication modes and strategies; and collective communicative competencies, which varied according convoy type with cohesive convoys demonstrating greater competence, than fragmented or discordant convoys (see Kemp et al., 2018).
Figure 2.
Communicative competence.
Among key factors at the AL home level were size and physical design; resident profile; staff quality, quantity, and consistency; policies and procedures; communication culture and resources; organizational structure; and use of external health care providers. At the community level, AL regulations have important influences, including on resident and staff profiles, physical environments, care policies and procedures, and communication strategies. Medicare regulations, which govern and fund hospice and other health care use in AL, also shape processes and outcomes related to residents’ health changes.
Discussion
Our analysis of the processes surrounding AL residents’ health status changes in the context of communication identified four basic and interrelated processes that comprise our model of communicative competence: identifying change; assessing the significance of change; responding to change; and communication, consisting of informing, consulting, and collaborating regarding change (see Figure 2). Although all four processes generally happened when change occurred, situations varied in their presence, nature, and sequencing. Communicative competence of residents and their care partners was variable, influenced by multiple and interrelated factors, and critical to whether and how health transitions were handled and in care outcomes.
Our findings provide further evidence of the fragility of AL residents’ health and the frequency of health status changes, adding to our earlier work (Kemp et al., 2019) and corroborating data from AL residents nationally (Khatutsky et al., 2016). Almost all resident participants experienced health changes, many multiple times, across a range of health dimensions and situations. The instability and complicated nature of AL residents’ health status reinforces the importance of the health literacy of residents and their care convoy members in identifying, understanding the significance of, and responding to health changes. Our data provide numerous examples of how knowledge, or lack thereof, related to health conditions and changes affected response to health changes and health outcomes.
These findings highlight the need for basic and ongoing education and training to enhance the health literacy of all care convoy members. AL administrators should develop educational opportunities for residents, staff, and informal caregivers that are tailored to the needs, abilities, and cultures of their unique communities. Education should address topics germane to health changes, including clinical information about health conditions and common indicators of change and strategies for appropriate actions surrounding the four identified processes associated with change. Specialized training may be needed for identifying changes among residents living with dementia or those who are unable to communicate.
Health education could be integrated into a home’s engagement programming, continuing staff education, and family events, and use a variety of educators from its own community, including experienced care staff, licensed nurses, professionals from external organizations providing care in the home, such as hospice and home health agencies and medical practices, and even health professionals among AL residents and their family members or those from the surrounding community. Innovative dissemination strategies could be developed, involving, for example, role playing, peer mentoring, videos, and webinars, building educational content around real-life scenarios where health changes have been handled appropriately and inappropriately. However, attention must be paid to retaining an emphasis on a social model of care whereby monitoring resident health takes place in the context of day-to-day life, care activities, and social encounters and relationships.
Past research, our own and others, illuminates the important role direct care workers play in detecting and responding to residents’ health transitions. Relative to other care partners, care staff typically spend the most time with residents and are most likely to be present when health changes occur. Thus, their ongoing education and training and communicative competence are especially crucial. Resident care directors or other AL personnel who oversee resident care should incorporate opportunities for regular communication (at intervals dictated by situations) with care staff to review residents’ health conditions and any observed or anticipated changes. Such interactions could occur one-on-one or in groups, and in-person or through alternative communication modes (e.g., telephone, written log).
Familiarity with residents and identifying and assessing change in the context of what is typical and atypical is essential for good care outcomes, emphasizing the need for care continuity. Thus, findings have implications for staffing patterns and retention strategies. Mismatched ratios between care needs and capacity to meet those needs, high workloads, and inconsistent assignment can affect care workers’ overall effectiveness, including communicative competence, and should be evaluated and addressed. Theirs are physically and emotionally demanding jobs with increasing responsibility and accompanying pressure, yet U.S. AL care workers earn among the lowest wages, their access to health and other benefits is limited, and many have multiple additional demands in their lives (Kelly et al., 2018). Providing opportunities for additional health training and developing “health specialists” positions, with increased pay, might be possible avenues for enhancing job satisfaction and retention and enhancing resident care.
Having engaged informal care partners and cohesive, as opposed to fragmented or discordant, convoys typically led to timely and appropriate care. Informal care partners were pivotal in monitoring residents and facilitating familiarity between residents and formal care partners, especially AL staff. These findings resonate with those from a small qualitative study involving 14 family members of nursing home residents in the United Kingdom that characterizes their care roles as important in timely detection of resident health changes by noticing change and informing and educating care staff about change (Powell et al., 2018).
Residents’ inability or unwillingness to communicate health transitions that were invisible to, or undetected by, others were especially challenging for care partners and underscore the importance of ongoing monitoring and the identification and assessment of even the subtlest change. Convoy members should collaborate to educate residents about the importance of communicating health changes and encourage them to take action.
Our findings emphasize need for ongoing oversight of residents in order to identify health changes, admittedly a challenge for the available resources of many AL communities. Using technology, such as video monitoring or other tools might alleviate some of the staffing pressures and improve outcomes related to health changes. Some experts recommend that AL communities employ registered nurses with gerontological training to assist with resident assessment and care and to supervise care staff (Maas & Buckwalter, 2006). This model would be effective in certain settings, including larger communities and those with greater resources, but may not be universally possible or necessary.
Our work reinforces the need for AL care managers and potentially external health care providers to assess and understand the potential strengths and weaknesses of residents’ care networks and how those might affect communication processes during health transitions. In some instances, the communicative competence of one convoy member affected the competence of the whole, influencing care outcomes. Yet, the quality of communicative competence frequently depended on the relationships and interactions among care partners and evolved, along with care convoys, over time. AL communities should work to facilitate positive relationships and open communication among all care partners.
We find that the concept of communication space (Coiera, 2006) has relevance for the AL care environment, which has become increasingly complex with expansion of the range and number of health care professionals providing care to residents, in and out of the home (Kemp et al., 2019), in addition to the AL staff and informal care partners who populate residents’ care convoys (Kemp et al., 2018). Our earlier work examining AL residents’ care convoys (Kemp et al., 2018) found that convoys varied in size, configuration, and function and changed over time in response to a multiplicity of factors, compounding the complexity of AL care arrangements. The sheer numbers and types of individuals potentially involved render communicative competence increasingly challenging regarding knowing whom to notify, when and how, and what information to provide.
Findings reinforce the need for AL communities to have communication systems that include well-defined policies and procedures regarding the handling of residents’ health changes, including appropriate communications means and channels. Although regulatory systems exterior to an individual AL setting, including state AL and Medicare and Medicaid home health and hospice entities and the Health Insurance Portability and Accountability Act, exert influence, AL homes should have in-house systems specific to their environments. Up to date, key information, including whom to contact and how, should be kept in residents’ own rooms or in a dedicated book accessible to staff, for example, in the resident care director’s office.
Our data also reinforce the need for having documented advanced health care directives outlining preferred responses to health changes, particularly regarding life-threatening conditions, easily accessible to appropriate individual(s) when needed, including during fast-paced emergency situations that can introduce new care partners and settings. Failure to do so can lead to costly, unwanted, unnecessary, and potentially harmful ambulance rides and hospital visits.
Our research has limitations. First, data were collected in a small number of care settings in and around one area in a single state, and derive from only one regulatory model. Next, although we endeavored to include as many convoy members as possible, first responders and ED and hospital staff were not part of our sample. Their inclusion would further enhance understanding of communicative competence. Third, the research lacks the potential breadth derived from quantitative or mixed-methods approaches. Finally, beyond learning about residents’ dementia diagnoses, researchers did not conduct cognitive assessments. However, our observational data provide insight into the influence of cognitive ability on communicative competence.
A major strength of this work is the use of an in-depth, longitudinal, and comprehensive view of the processes surrounding AL residents’ health status changes in a diverse group of AL communities and residents that are similar to those found in many other states. We identified general processes through in-depth and prolonged examination of entire care convoys—an approach that few, if any, others have taken to understand communication processes surrounding older adults’ health changes. Although derived through our AL research, our communicative competence model can be tested and modified in other locations and complex care environments where multiple care network members are involved. Identifying ways to create and maintain communicative competence within care convoys across populations and settings is challenging, especially while retaining a social care model, but is critical for quality of care and quality of life.
Acknowledgments
The authors thank all those who participated, shared their experiences, and gave generously of their time. We are very grateful to co-investigators, Elisabeth O. Burgess, Jennifer Craft Morgan, and Molly M. Perkins and to Carole Hollingsworth and Patrick Doyle for their valuable contributions. Thank you also to Elizabeth Avent, Natasha Belton, Christina Barmon, Victoria Helmly, Richelle King, Lokyee Lee, Emily Maggio, Yolanda Mendoza-Miller, Alejandro Torres-Pomales, Russell Spornberger, and Deborah Yoder for assisting with data collection and analysis activities.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (R01AG044368 to C. L. Kemp). The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
We have no conflict of interest to declare.
References
- Ball M. M., Kemp C. L., Hollingsworth C., & Perkins M. M (2014). “This is our last stop”: Negotiating end-of-life transitions in assisted living. Journal of Aging studies, 30, 1–13. doi:10.1016/j.jaging.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball M. M., & Whittington F. J (1995). Surviving dependence: Voices of African American elders. New York: Routledge. [Google Scholar]
- Beeber A. S., Zimmerman S., Reed D., Mitchell C. M., Sloane P. D., Harris-Wallace B., . . . Schumacher J. G (2014). Licensed nurse staffing and health service availability in residential care and assisted living. Journal of the American Geriatrics Society, 62, 805–811. doi:10.1111/jgs.12786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belim C., & De Almeida C. V (2018). Communication competencies are the key! A model of communication for the health professional to optimize the health literacy—assertiveness, clear language and positivity. J Healthcare Communication, 3, 31. doi:10.4172/2472-1654.100141 [Google Scholar]
- Caffrey C., Sengupta M., Park-Lee E., Moss A., Rosenoff E., & Harris-Kojetin L (2012). Residents living in residential care facilities: United States, 2010. NCHS Data Brief, 91, 1–8. Retrieved March 24, 2019, from https://www.cdc.gov/nchs/products/databriefs/db78.htm [PubMed] [Google Scholar]
- Carder P., O’Keeffe J., & O’Keeffe C (2015). Compendium of residential care and assisted living regulation and policy: 2015 edition. Washington, DC: U.S. Department of Health & Human Services, Office of the Assistant Secretary for Planning and Evaluation; Retrieved March 24, 2019, from https://aspe.hhs.gov/basic-report/compendium-residential-care-and-assisted-living-regulations-and-policy-2015-edition [Google Scholar]
- Coiera E. (2006). Communication systems in healthcare. Clinical Biochemist Reviews, 27, 89–98. [PMC free article] [PubMed] [Google Scholar]
- Corbin J., & Strauss A (2015). Basics of qualitative research: Techniques and procedures for developing grounded theory. 4th ed. Thousand Oaks, CA: Sage. [Google Scholar]
- Georgia Department of Community Health. (2013). Rules and Regulations for Personal Care Homes Act. O.C.G.A. § 31-8-131 et seq. [Google Scholar]
- Gordon J. E., Deland E., & Kelly R. E (2015). Let’s talk about improving communication in healthcare. Columbia Medical Review, 1, 23–27. doi:10.7916/D8RF5T5D [Google Scholar]
- Harris-Kojetin L., Sengupta M., Park-Lee E., Valverde R., Caffrey C., Rome V., & Lendon J (2016). Long-term care providers and services users in the United States: Data from the national study of long-term care providers, 2013–2014. Vital and Health Statistics, 3, 1–105. [PubMed] [Google Scholar]
- Hymes D. (1966). Two types of linguistic relativity. In Bright W. (Ed.), Sociolinguistics (pp. 114–158). The Hague: Mouton. [Google Scholar]
- Institute of Medicine (2013). Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academic Press. [PubMed] [Google Scholar]
- Kelly C. M., Morgan J. C., Kemp C. L., & Deichert J. A (2018). A profile of the assisted living direct care workforce in the United States. Journal of Applied Gerontology. 1, 1–26. doi: 10.1177/0733464818757000 [DOI] [PubMed] [Google Scholar]
- Kemp C. L., Ball M. M., Morgan J. C., Doyle P. J., Burgess E. O., Dillard J. A., . . . Perkins M. M (2017). Exposing the backstage: Critical reflections on a longitudinal qualitative study of residents’ care networks in assisted living. Qualitative Health Research, 27, 1190–1202. doi:10.1177/1049732316668817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp C. L., Ball M. M., Morgan J. C., Doyle P. J., Burgess E. O., & Perkins M. M (2018). Maneuvering together, apart, and at odds: Residents’ care convoys in assisted living. Journal of Gerontology: Series B, Psychological Sciences and Social Sciences, 73, e13–e23. doi:10.1093/geronb/gbx184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp C. L., Ball M. M., & Perkins M. M (2013). Convoys of care: Theorizing intersections of formal and informal care. Journal of Aging Studies, 27, 15–29. doi:10.1016/j.jaging.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp C. L., Ball M. M., & Perkins M. M (2019). Individualization and the health care mosaic in assisted living. The Gerontologist, 59:644–654. doi: 10.1093/geront/gny065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatutsky G., Ormond C., Wiener J. M., Greene A. M., Johnson R., Jessup E. A., & Harris-Kojetin L (2016). Residential care communities and their residents in 2010: A national portrait. (DHHS Publication No. 2016-1041). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Kistler C. E., Zimmerman S., Ward K. T., Reed D., Golin C., & Lewis C. L (2017). Health of older adults in assisted living and implications for preventive care. The Gerontologist, 57, 949–954. doi:10.1093/geront/gnw053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas M. L., & Buckwalter K. C (2006). Providing quality care in assisted living facilities: Recommendations for enhanced staffing and staff training. Journal of Gerontological Nursing, 32, 14–22. [DOI] [PubMed] [Google Scholar]
- Nussbaum J. F., Baringer O., & Kundrat A (2003). Health, communication, and aging: Cancer and older adults. Health Communication, 15, 185–192. doi:10.1207/S15327027HC1502_6 [DOI] [PubMed] [Google Scholar]
- Patton M. Q. (2015). Qualitative methods and evaluation methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Powell C., Blighe A., Froggatt K., McCormack B., Woodward-Carlton B., Young J., . . . Downs M (2018). Family involvement in timely detection of changes in health of nursing homes residents: A qualitative exploratory study. Journal of Clinical Nursing, 27, 317–327. doi:10.1111/jocn.13906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenberg A. E., Ball M. M., Kemp C. L., Doyle P. J., Fritz M., Halpin S., . . . Perkins M. M (2018). Contours of “here”: Phenomenology of space for assisted living residents approaching end of life. Journal of Aging Studies, 47, 72–83. doi:10.1016/j.jaging.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeir P., Vandijck D., Degroote S., Peleman R., Verhaeghe R., Mortier E., . . . Vogelaers D (2015). Communication in healthcare: A narrative review of the literature and practical recommendations. International Journal of Clinical Practice, 69, 1257–1267. doi:10.1111/ijcp.12686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman S., Sloane P. D., & Reed D (2014). Dementia prevalence and care in assisted living. Health affairs (Project Hope), 33, 658–666. doi:10.1377/hlthaff.2013.1255 [DOI] [PubMed] [Google Scholar]