Abstract
Background and Objectives
Falls among older adults is a pressing public health challenge. Considerable research documents that longer tai chi courses can reduce falls and improve balance. However, longer courses can be challenging to implement. Our goal was to evaluate whether a short 6-week modified tai chi course could be effective at reducing falls risk if older adults designed a personal home practice plan to receive a greater tai chi “dose” during the 6 weeks.
Design
A 3-city wait-listed randomized trial was conducted. Habituation Intention and Social Cognitive Theories framed the “coaching” strategy by which participants designed practice plans. RE-AIM and Treatment Fidelity Frameworks were used to evaluate implementation and dissemination issues. Three advisory groups advised the study on intervention planning, implementation, and evaluation. To measure effectiveness, we used Centers for Disease Control and Prevention recommended measures for falls risk including leg strength, balance, and mobility and gait. In addition, we measured balance confidence and executive function.
Results
Program Implementation resulted in large class sizes, strong participant retention, high program fidelity and effectiveness. Participants reported practicing an average of 6 days a week and more than 25 min/day. Leg strength, tandem balance, mobility and gait, balance confidence, and executive function were significantly better for the experimental group than control group.
Conclusion
The tai chi short course resulted in substantial tai chi practice by older adults outside of class as well as better physical and executive function. The course reach, retention, fidelity, and implementation across 3 cities suggest strong potential for implementation and dissemination of the 6-week course.
Keywords: Tai chi, Balance, Home practice, Executive function
Falls among older adults is a pressing public health challenge. Medical costs attributable to falls were estimated to be over $50 billion in the United States (Florence et al., 2018). Every 20 min an older adult dies from a fall and each year 3 million are treated in emergency departments for falls related injuries in the United States according to the Centers for Disease Control and Prevention (CDC)’s Important Facts about Falls (n.d.). Given a rapidly aging population, sustainable health promotion interventions are needed to reduce older adults’ risks of falls (Burns & Kakara, 2018).
Originated around the 13th century, tai chi is a nonimpact exercise that enhances body awareness, postural alignment, coordination, strength, and flexibility while imparting minimal stress on joints (Koh, 1981; Lan, Chen, Lai, & Wong, 2013). Tai chi reduced the overall rate of falls (43%) and injury-related falls (50%) (Lomas-Vega, Obrero-Gaitan, Molina-Ortega, & Del-Pino-Casado, 2017) and affected positively on older adults’ balance, tandem stance, lateral stability and functional reach, leg strength, sensory organization, mobility and gait, and self-efficacy to avoid falls in numerous trials (Del-Pino-Casado, Obrero-Gaitan, & Lomas-Vega, 2016; Hackney & Wolf, 2014; Hu et al., 2016; Huang, Feng, Li, & Lv, 2017; Huston & McFarlane, 2016; Kendrick et al., 2014; Lan et.al., 2013; Li et al., 2005; Lomas-Vega et al., 2017; Tousignant et al., 2012; Zhao & Wang, 2016).
The National Council on Aging suggests a tai chi dose of 50 hr (1-hr class twice per week for 6 months or 3 times per week for 4 months) will reduce the risk/rate of falls (Tai Chi for Falls Prevention, 2016). Current best practice guidelines indicate 3 hr a week of ongoing mid-to-high level balance challenge exercise is needed to reduce the annual rate of falls (Sherrington et al., 2017). Despite these recommendations, two striking questions regarding a needed tai chi dose have been understudied. First, how many course hours per week and across what duration does a course need to be in order to offer a sufficient dose? Tai chi programs of different lengths and intensity have been effective. A systematic review demonstrated wide variation in course length (8–26 weeks) was effective (Wu, MacDonald, & Pescatello, 2016). Second, studies generally under attend to whether and how much individuals practice their tai chi outside of class except in the most general terms (Wu et al., 2016). This is key because dose is composed of both in-class exercise and a person’s out-of-class practice. Nor has research answered what type of intervention could be integrated effectively into a tai chi course to promote practice outside of class. If sustainable daily tai chi practice (both inside and outside class) could be achieved, shorter courses could offer a more easily disseminated and implemented course structure than some of the longer courses found to be effective. The key question is whether a shorter course could achieve a sufficient “dose” if participants practice sufficiently outside of class.
From a dissemination and implementation perspective, a shorter tai chi course would have several advantages. Recruiting and retaining older adults for 6-month community-based exercise programs can be challenging (Farrance, Tsofliou, & Clark, 2016; McPhate, Simek, & Haines, 2013; Mullen et al., 2013; Picorelli, Pereira, Pereira, Felicio, & Sherrington, 2014). Recent research documented substantial participant dropout of a 24-week tai chi course (Coe et al., 2017). Shorter courses also align with needs of community organizations whose class sessions may only last 2 months or less when holidays and winter weather interfere with attendance. Although shorter classes could facilitate attendance however, is it possible to reach Sherrington and colleagues’ (2017) recommended 3-hr dose of mid-to-high level balance challenge exercise per week? If yes, could the short course and home practice together help reduce older adults fall risk indicators within 6 weeks?
Methods
Conceptual Framework
This pragmatic trial evaluates whether an 18-hr Tai Chi Prime (TCP) class, with a unique home practice component, affects older adults’ falls risk indicators. An underlying assumption is that home practice provides a key mechanism of action. To this end, a home practice intervention was devised that drew on two theoretical frameworks used successfully in health programs. Social Cognitive Theory (SCT) was used to increase participants’ self-efficacy to develop realistic practice plans (Bandura, 1997). Participants designed their own plan for weekly tai chi practice, rehearsed practice at home, monitored their practice on logs, returned practice logs to course instructors twice during the course and received support and suggestions throughout the course. Second, the Habituation-Intention Framework informed the approach of embedding practice of four prioritized moves into each person’s habitual daily activities (e.g., while making a morning cup of coffee) (Clemson et al., 2012; Mansukhani, Kieser, Ricci, & Chewning , 2017; Oulette & Wood 1998). The goal was to pair an old habit with a new one as was done with Clemson’s Lifestyle Integrated Functional Exercise approach (Clemson et al., 2012).
Research Design
A pragmatic randomized trial used a wait-list control to satisfy community centers’ desire for all study participants to receive tai chi. Demand was high. A wait list of more than 200 older adults was generated in one city alone. The trial was conducted in fall of 2016 and spring of 2017. Each semester, two TCP courses were offered in each of three Wisconsin cities. The first course in the semester served as the experimental group and the second course served as the control group. Several weeks before the semester started, research staff randomized participants to experimental or wait-list control groups. Twelve courses (four per city) were offered in this design. Measures were collected immediately before and after the TCP courses to allow comparison of the experimental group post-test scores to the control group pretest scores. The University of Wisconsin–Madison Health Sciences Institutional Review Board approved the study protocol.
Stakeholder Engagement
Stakeholder groups regularly informed key study decisions about recruitment strategies and materials, sustainable program implementation, participants’ home practice planners and trackers, data collection, and refinement of course manuals for dissemination. Three separate advisory groups were the following: (a) community site coordinators from each center in the study, (b) older adults representative of study participants, and (c) course instructors. Each advisory group offered unique expertise in a co-learning environment to evaluate and refine the course for feasible community adoption, implementation, and sustainability (Chunharas, 2006).
Study Setting and Sample
Three Aging Units and Aging and Disability Resource Centers in different Wisconsin cities offered the course. Inclusion criteria for course participants were being at least 65 years, dwelling independently in the community, agreeing to be randomized, reporting a fall (to the ground or lower level) in the last year or having a strong fear of falling. Exclusion criteria were using a walker indoors, having a terminal illness, being hospitalized or in a nursing home in the past 2 months, anticipated absence from two tai chi sessions and receiving physical therapy or a community course or balance exercise program for falls prevention in the previous 2 months. Course participants were paid $25 after the post-test and $25 after a 6-week follow-up interview. Participants were given the tai chi course, book, and DVD (Yu, 2015; Yu & Hallisy, 2015).
Tai Chi Fundamentals Overview
TCP was created by adding the home practice intervention to Tai Chi Fundamental (TCF). TCF is a simplified tai chi program for older adults and others with pain or physical limitations (Yu & Johnson, 1999). As a slow, graceful Chinese exercise that enhances relaxation skills, mental focus, and physical alignment, it also builds leg strength, endurance, and postural stability (Hallisy, 2018; Yu & Hallisy 2015). Key features include the following:
Mindfulness—intentional and nonjudgmental attention in the present moment
Postural alignment—upright body creating postures and movements that are biomechanically effective and efficient
Natural (diaphragmatic) breathing—fundamental to all meditative movement therapies (e.g., tai chi yoga, qigong)
Active relaxation—a state of relaxed inner stillness while in motion
Slow movement—slow movement building strength and endurance
Weight separation—enhancing postural control and dynamic balance
Integrated movement—building and coordinating functional movement
TCF was created by a Yang-style lineage certified tai chi master who had taught tai chi for 30 years and noted the difficulty older adults had moving and remembering the complicated movements of traditional tai chi (Yu & Hallisy, 2015). Yu collaborated with physical and occupational therapists to use rehabilitation principles when designing the modified TCF program (Yu & Johnson, 1999). Twenty Basic Moves are taught in a neurodevelopmental sequence offering participants incremental and safe practice. The Basic Moves are in essence “exercises” repeated with verbal, visual and kinesthetic cues from the instructor and act as part-to-whole building blocks allowing the participants to learn tai chi flow and form in a stepwise manner. TCF is based on Yang-style tai chi, which is one of three primary tai chi lineages, or styles, each bearing the family surname of its founder (Chen, Yang, and Wu). The Yang style and its many variations are the most popular and widely practiced tai chi style in the world today.
Tai Chi Program Intervention
TCP is a 6-week twice-weekly simplified tai chi class of 1.5 hr per session with two components: (a) TCF Adapted Program (Yu, 2015; Yu & Hallisy 2015), and (b) home practice coaching.
Each class session followed a similar overall format
Opening—orientation to the day, questions/answers from last session (5–10 min).
Tai chi Warm-ups and Basic Moves instruction (building blocks for learning TCF Short Form) (20–30 min).
Informal teatime (exercise break and time for community building via participant connectedness and socialization time) (10 min).
Group home practice enhancement activities (home practice planning and coaching, use of DVDs, books, home practice planners, and trackers) (20–30 min).
TCF Short Form instruction (simplified flowing sequence of Yang-style tai chi) (10–25 min).
Closing—reminders for home practice, next class preview and Qi Gong closing (5 min).
Traditional Mind Body Skills Training (e.g., centering, breath awareness, relaxation and Everyday Qi Gong) are embedded throughout the classes.
The TCP course directs participants through the stages of motor learning. At first, tai chi movements are highly cognitive, meaning participants must concentrate as they learn. Over time, movements become more associative and learners begin to learn the flow of the system. With practice (in class and home), learners are asked to find ways to automatically use the Fab Four tai chi movements in everyday life. The TCP educational component of the program uses practice planners and trackers to promote autonomous planning on when/where/how to integrate exercise into their day and daily habits.
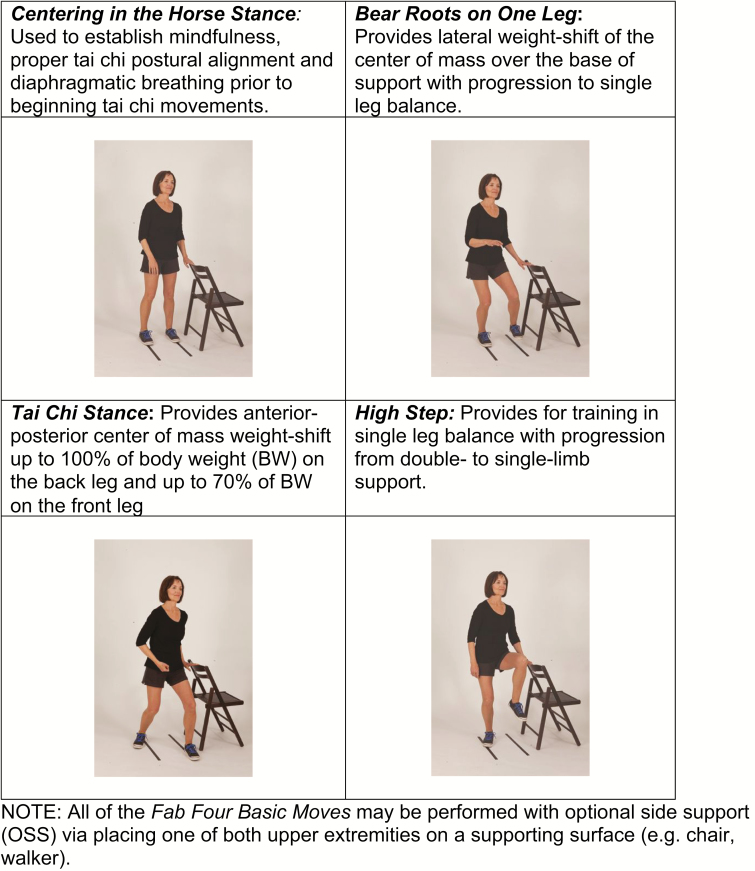
The Fab Four movements were emphasized as they align well with balance principle 1 of Sherrington’s best practice exercise guidelines for falls prevention (Sherrington et al., 2017). They provide mid- to high-level balance challenge by (a) moving the center of mass over the base of support, (b) reducing the base of support from double limb to single limb stance, and (c) decreasing the need for upper limb support in standing (Sherrington et al., 2017). See Figure 1.
Figure 1.
Tai Chi Prime’s Fab Four Basic Moves—used to reinforce daily practice habits. Basic Moves provide mid- to high-level balance challenge by (a) moving the center of mass over the base of support in multiple directions, (b) reducing the base of support from double limb to single limb stance and (c) decreasing the need for upper limb support in standing (Sherrington et al, 2017). All of the Fab Four Basic Moves may be performed with optional side support (OSS) via placing one of both upper extremities on a supporting surface (e.g., chair, walker).
Rapidly the home practice intervention fosters adoption and adherence to home practice. By the second class, participants learned all Fab Four Basic Moves and could plan when and where they could easily embed their daily practice into existing habits (Clemson et al., 2012; Mansukhani et al., 2017; Oulette & Wood 1998; Yu, 2015; Yu & Hallisy, 2015). They also began planning when to practice the TCF Short Form and/or Basic Moves daily in a quiet, flat, safe place at a regular time, either with or without the model DVD. Given that low self-efficacy to overcome exercise barriers is associated with exercise attrition (Bandura, 1997; Farrance et al., 2016; McPhate et al., 2013; Mullen et al., 2013; Oulette & Wood 1998; Picorelli et al., 2014; Tousignant et al., 2012), SCT principles helped to increase self-efficacy to practice the TCF Short Form and Basic Moves at home. Instructors distributed planning forms and tracker logs to participants and shared in class how to plan and rehearse their daily practice of TCF Short Form and/or Basic Moves in a typical day (Bandura 1997; Clemson et al., 2012; McAuley, 1992; Yu & Hallisy 2015). The planner charts were adapted from a pill card developed by the Agency of Healthcare Research and Quality agency to plan patients’ medication schedules (Mansukhani et al., 2017). Participants logged each day how much they practiced for a week and returned their logs to instructors two different weeks during the course. During the class seated time, instructors and peers shared successes and offered support and feedback to overcome practice barriers.
Measures and Data Collection
To measure falls risk, a multimethod data collection assessed physical function indicators, balance confidence, and executive function. Also, demographic information, fidelity of course delivery, course size and attendance, and fidelity of course receipt and enactment in terms of participant tai chi home practice was collected. Trained researchers collected physical, confidence and executive function data at community sites using specific stations for each measure with participants systematically rotating between these stations.
Physical Function
Trained physical therapy teams collected pre- and post-test validated, physical function outcome measures associated with falls risk as recommended by CDC’s Stopping Elderly Accidents, Deaths and Injuries (STEADI) Program (Centers for Disease Control and Prevention [CDC], 2016; Stevens, 2013). Suitable for older adults and sensitive to change, these physical measures were the Timed Up and Go (TUG) test of mobility and gait measured in seconds (Lusardi et al., 2017; Steffen, Hacker, & Mollinger 2002), 30-s Chair Stand test of leg strength measured in number of times stood (Jones, Rikli, & Beam, 1999; Lusardi et al., 2017), and the 4-Stage Balance test measured in seconds (Lusardi et al., 2017; Rossiter-Fornoff, Walf, & Wolfson, 1995). Balance measures were side-by-side, staggered tandem, tandem, and single leg balance positions. Tandem was of greatest interest to this study as the key balance risk indicator. Data collection quality was monitored throughout the study.
Balance Confidence and Executive Function
To explore possible impact on balance confidence (0%–100%), the validated Activities-specific Balance Confidence (ABC) Scale was administered pre- and post-intervention (Huang & Wang, 2009). Trail Making Test (TMT) Part B was administered pre- and post-test to assess the ability to reason and solve novel problems independent of knowledge from the past, reflective of executive function (Salthouse, 2011; Tombaugh, 2004). Participants completed these scales at a station at the same time the physical measures were administered.
Implementation Domains
Several aspects of intervention reach, fidelity, and implementation were collected consistent with the RE-AIM evaluation model (Glasgow, Vogt, & Boles, 1999) as well as the Treatment Fidelity Framework (TFF) from the National Institutes of Health (NIH) Behavior Change Consortium (Borrelli, 2011). Course instructors recorded class attendance for the 6 weeks. Master teachers monitored fidelity of TCP course delivery during four of each instructor’s course sessions using a 40-item dichotomous checklist consisting of General Class Setting, Warm-ups and Basic Moves, Home Practice Activities, Short Form training and Closing according to Tai Chi Health’s certification process (http://taichihealth.com/?page_id=156). Drawing on the RE-AIM evaluation model, we captured two other data related to “reach” as part of implementation quality. Site coordinators documented class sizes, and the participants’ characteristics of race, gender, and age were also collected.
Per the NIH Behavior Change Consortium’s TFF, instructors were trained a minimum of 30 contact hours, did home practice and practice teaching, and completed a written exam and a movement test evaluated by a TCF certification reviewer. All instructors received a detailed course curriculum manual that structured the goals and activities for each class. A second evaluation element of the TFF was how much participants enacted elements of the intervention, which in this case was the TCP home practice (Borrelli, 2011). To measure home practice, participants recorded daily the number of minutes they practiced. The TCP tracker logs were adapted from earlier studies (Mahoney, 2016; Mansukhani et al., 2017). Instructors explained how to complete the trackers when they were distributed in the 4th and 10th classes. Instructors then collected the trackers 1 week later in classes 6 and 12, respectively for analysis.
Data Analysis Plan
All statistics were calculated using Statistical Package for the Social Sciences (SPSS) version 23.0. Statistical tests were performed at the 0.05 level of significance. Student’s t test and chi-square analyses determined whether there were significant differences in participants’ demographics, that is, age, gender, and race. Descriptive analyses were performed. Mean differences were calculated between experimental group post-test scores of each outcome variable and the control group pretest scores. Bivariate correlations between each variable were calculated. To evaluate TCP course effectiveness, controlling for covariate(s), linear regression determined the association of group assignment (experimental or control) with each outcome variable.
Results
Recruitment, Randomization, and Retention
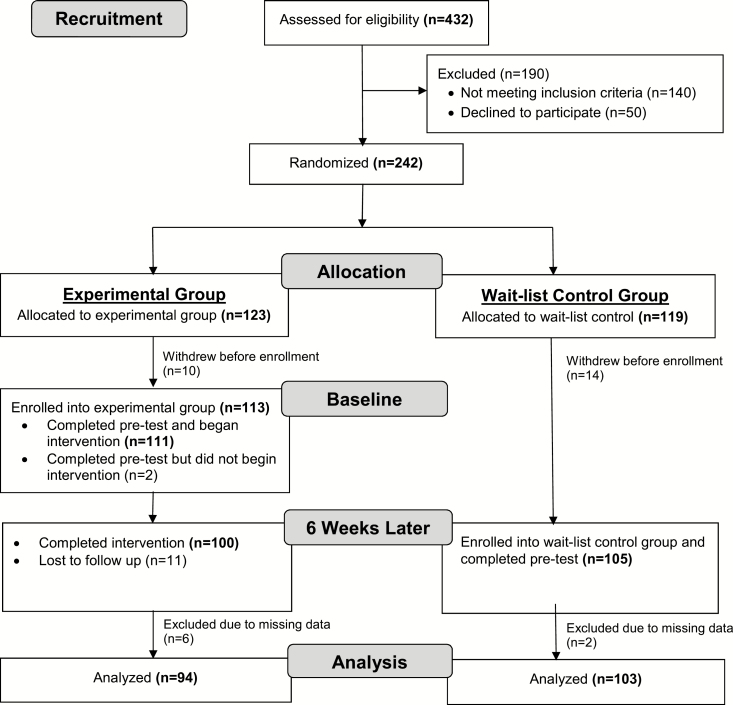
All three sites approached agreed to offer the TCP course. A total of 432 older adults from three Wisconsin cities were screened for eligibility with 32.4% (n = 140) not meeting study eligibility and 11.6% (n = 50) declining to participate. Two hundred forty-two (n = 242, 56%) were enrolled and randomized in the study with 123 randomized to one of two (fall and spring) experimental TCP sessions and 119 to one of two (fall and spring) wait-list control sessions. The total usable sample size was 197 in the final data analysis. See Figure 2.
Figure 2.
Flow Chart of Sample
Baseline Characteristics
Participants were on average 73.9 years old (SD = 7.2), ranging in age from 65 to 94. Most were white (99.5%) and women (83.8%). Potential differences between experimental and control groups’ baseline demographic characteristics are presented in Table 1. Despite randomization, mean age of the control group was younger than the experimental group. Age was also significantly associated with outcomes of interest in bivariate analyses.
Table 1.
Baseline Characteristics of Study Participants (N = 197)
| Characteristic | Intervention (n = 94) | Control (n = 103) | p-value |
|---|---|---|---|
| Age, mean ± SD | 75.0 ± 7.4 | 72.8 ± 7.0 | .032* |
| Age deciles | |||
| 65–69, % | 31.9 | 46.6 | |
| 70–74, % | 22.3 | 20.4 | |
| 75–79, % | 17.0 | 14.6 | |
| 80–84, % | 18.1 | 12.6 | |
| 85–89, % | 7.4 | 2.9 | |
| 90–94, % | 3.2 | 2.9 | |
| Female, % | 80.6 | 87.2 | .206† |
| White, % | 100 | 99.0 |
Note: *Student’s t test.
†Chi-square test.
Physical Function
Analyses tested the a priori hypotheses that exposure to the 6-week TCP course would significantly affect participants’ performance of physical function end points. Age was included as a covariate in linear regression models of group assignment (experimental vs control) predicting the study outcome variables. Leg strength, tandem balance, and mobility and gait are all key determinants of falls risk (Lusardi et al., 2017). Norms for the STEADI scores are provided by the CDC (2017). As predicted, the primary outcome of leg strength (30-s chair stand) for the experimental group was significantly better than the control group scores. See Table 2. Mean and standard deviation for leg strength data for the intervention group (11.5 ± 4.5 repetitions) and control (9.4 ± 3.1 repetitions) groups suggest each had a distribution of risk with some subjects below, at or above the cut score on the Chair Stand Test. Of the four positions in the 4-Stage Balance Test, tandem stance is the key indicator of falls risk. An older adult that cannot stand at least 10 s in the tandem position is at risk for falls. In our sample, both the intervention group (8.5 ± 2.9 s) and the control group (7.76 ± 3.5 s) were at risk. However, as predicted, tandem balance was significantly better in the experimental group. Also consistent with the a priori hypotheses, mobility scores as measured by the TUG were significantly better for the experimental group than the control group. An older adult who takes greater than or equal to 12 s to complete the TUG is at risk for falling. Given the large standard deviations, we can see that both the intervention group (10.6 ± 3.8 s) and the control group (11.9 ± 6.1 s) were fairly high functioning on this test, but the large standard deviation suggests that some subjects were clearly at risk of falling given their TUG scores.
Table 2.
Outcome Measures of Physical Function, Balance Confidence, and Executive Function Scores (N = 197)
| Outcome measure | Intervention (n = 94) | Control (n = 103) | B (SE) | 95% CI | p-value* | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Timed Up and Go, mean ± SD | 10.6 ± 3.8 | 11.9 ± 6.1 | −1.824 (0.717) | −3.238 | −0.409 | .012 |
| 30-s Chair Stand, mean ± SD | 11.5 ± 4.5 | 9.4 ± 3.1 | 2.523 (0.515) | 1.508 | 3.538 | .000 |
| 4-Stage Balance, mean ± SD | ||||||
| Side-by-side | 10.0 ± 0 | 9.97 ± 0.3 | 0.028 (0.035) | −0.041 | 0.097 | .426 |
| Staggered tandem | 9.9 ± 0.9 | 9.6 ± 1.7 | 0.371 (0.195) | −0.014 | 0.756 | .059 |
| Tandem | 8.5 ± 2.9 | 7.6 ± 3.5 | 1.314 (0.435) | 0.455 | 2.172 | .003 |
| Single leg | 6.0 ± 3.7 | 6.2 ± 7.7 | 0.103 (0.872) | −01.617 | 1.823 | .906 |
| Activities-specific balance confidence, mean ± SD | 82.9 ± 12.4 | 76.8 ± 16.5 | 7.216 (2.056) | 3.162 | 11.271 | .001 |
| Trail Making Test Part B, mean ± SD | 84.5 ± 40.4 | 92.3 ± 43.6 | −13.405 (5.488) | −24.229 | −2.580 | .015 |
*Linear regression; reference group is experimental group assignment. All analyses controlled for age.
Balance Confidence and Executive Function
Balance confidence and executive function scores also were consistent with a priori hypotheses. Controlling for age, scores were significantly better for the ABC Scale in the experimental group. See Table 2. TMT Part B is considered a discerning test of executive function with higher scores indicative of greater impairment. On average, older adults take 75 s to complete TMT B, with any time over 273 s indicating significant cognitive impairment. Both experimental (82.9 ± 12.4 s) and control (92.3 ± 43.6) groups were clustered above the mean norm for TMT B (Tombaugh, 2004).
RE-AIM and TFF Evaluation
Program reach
Class sizes exceeded the original planned size. The average class size was 18 participants. One region started with a waiting list of over 200 older adults.
Participants’ class attendance
There were 111 experimental group participants who began at least one TCP class. Ten discontinued the course after 1–5 classes. Reasons for discontinuation included participants’ unanticipated schedule changes, travel, one whose walker dependence was greater than expected, and a hospitalization. The mean number of classes attended by the remaining 101 experimental group participants was 11 (SD = 1.1) of 12 classes.
Course delivery fidelity
To evaluate fidelity of course delivery, TCF Master Teachers observed each instructor for one class in each session. A total of 12 classes were observed and rated. Overall fidelity was high, with 94% of the 40 items evaluated as consistent with the TCP course curriculum. Warm ups and Basic Moves had 92.9% fidelity. Short Form training had a fidelity of 93.1%. Home Practice Promotion Activities had 95.8% fidelity. Other elements had the following fidelity: General Environment (96.9%), Seated Activities (92.9%), and General Instructor (99.1%).
Home practice
A key measure was how much program recipients enacted the practice intervention delivered (Tombaugh, 2004). On the basis of their returned practice logs, the mean number of days practiced during the last week of class was 6.0 days with 57% reporting they practiced all 7 days during week 6. Average reported total minutes per day was 27.8 for the Short Form, Fab Four, and/or other Basic Moves. The return rate of logs was 94% of the 110 participants.
Discussion
Program Outcomes
This is the first randomized controlled trial (RCT) of TCP, a 1.5 hr 6-week twice weekly TCF program offering a novel mechanism to promote daily tai chi practice. This pragmatic trial found positive significant course effects for lower extremity strength, tandem balance, mobility and gait, confidence in balance and executive function (TMT Part B). It is particularly meaningful to have made an impact on the most evidence-supported functional measures to determine individual risk of future falls. The physical indicators as well as confidence in balance are key falls risk indicators (CDC, 2016; Jones et al., 1999; Lusardi et al., 2017; Rossiter-Fornoff et al., 1995; Steffen et al., 2002; Stevens, 2013). The finding on executive function is relevant in that, if validated in future studies, it would help to offer a protective mechanism for moving safely within the environment and staying within one’s postural limits (Fischer et al., 2014; Liu-Ambrose, Ahamed, Graf, Feldman, & Robinovitch, 2008; Zheng et al., 2015). A growing number of studies and systematic reviews have documented positive impact of tai chi on cognitive function (Wayne et al., 2014; Zheng et al., 2015).
The outcomes of our 6-week tai chi course paralleled the balance, leg strength and mobility and gait findings of RCTs of longer community-based tai chi courses. A systematic review by Wu ,MacDonald, and Pescatello (2016) aimed at improving balance of older adults in RCTs, found intervention length varied from 15 weeks to 6 months with an average of 20 weeks. These, along with a more recent study (Li et al., 2018), used the same or similar measures as our RCT for balance (tandem or single leg balance), leg strength (30-s Chair Stand Test), and gait/mobility (TUG). The primary difference of our course was its reduced length and emphasis on home practice to augment class time in our course. Implementation research has documented high course dropout rates for one of the most frequently delivered 24-week courses (Coe et al., 2017). This was not a problem for our study with its low dropout rate.
The focus on daily practice appears to have helped older adults. Participants reported they practiced regularly. Regular practice is necessary to achieve and sustain an effect (Ladawan et al., 2017; Zheng et al., 2015). An underlying assumption of this study was that practice was a key mechanism for course success. Studies document the importance of establishing a “habit” of tai chi practice to sustain the practice effects (Ladawan et al., 2017). According to tracker logs, participants practiced an average of 2.8 hr a week which approaches the best practice guidelines of 3 hr a week for mid-to-high level balance challenge exercise published by Sherrington et al., 2017. At least short term, the course successfully helped older adults develop individual practice plans for TCF Short Form and the Basic Moves (particularly the Fab Four) building both on theory and research. Individualized exercise planning shows promise to support participants’ exercise self-efficacy, self-management, and habit formation—factors strongly linked to program uptake and adherence (Bandura, 1997; Farrance et al., 2016; McAuley, 1992; Nicholls et al., 2016; Oulette & Wood, 1998; Picorelli et al., 2014).
From a dissemination and implementation perspective, several indicators are promising from our study. Using the RE-AIM Framework, the reach of the program was promising. All of the sites approached accepted the invitation to offer the course. Owing to popular demand, the average number of enrolled participants per class was higher than originally planned. The class attendance and retention across the 6-week course was high. Monitoring fidelity of program delivery confirmed good consistency of delivery of course process and content including the home practice component. Site coordinators felt that the 6-week course was feasible. They had collaborated in stakeholder advisory meetings and their recommendations had been incorporated.
Ideally, with more resources future research would investigate falls affect in addition to falls risk indicators for the 6-week course across a year. In addition to effectiveness, implementation at the individual participant and organizational level should be studied. A key question is whether and how participants sustain their practice habit across a longer period of time and what factors influence practice. From an organizational perspective, an exciting option to consider in future studies is the potential of community center and health system partnerships. For example, in a Massachusetts study linking clinical and community interventions, physicians assessed clients’ falls risks, referred clients to one of three programs of their choice, and tracked their enrollment and completion (Coe et al., 2017). Their recommendations for implementing such partnerships could complement implementation domains that were investigated in our study. Finally, there is a need to adapt courses and study their feasibility and effectiveness in more diverse communities with the input of stakeholder groups from the community.
Study Limitations
Although course participants were from three cities in Wisconsin, the sample was homogeneous with white women comprising the large majority. This is consistent with Tai Chi programs across the United States (Jiang, Kong, & Jiang, 2015). Second, a related limitation was that this study did not collect more demographic and health status information to assist interpretation of findings. Third, eligibility criteria for participants included having fallen in the past year or reporting a strong fear of falling. Participants may have exaggerated their fear of falling to gain access. Fourth, a limitation of the self-reported practice data is that it could reflect inaccuracies and social desirability influences. Finally, a limitation of this study is that the program effect on falls could not be measured because of lack of resources for long term follow-up of a large sample.
Conclusion
The short TCP program aligned well with implementation preferences of collaborating community organizations and proved feasible for participants which is promising for future dissemination and implementation. The innovative intervention to promote home practice resulted in the majority of course participants documenting regular home practice of tai chi for nearly 3 hr a week. Consistent with a priori hypotheses, the course proved effective in several other ways. Importantly, although the TCP course was only 6 weeks in length, combined with home practice, it had a significant impact on several falls risk factors (leg strength, tandem balance, and mobility and gait) as well as balance confidence and executive function. Future research is needed to evaluate long term, broader dissemination, and implementation of the TCP course across new states and diverse populations.
Funding
This work was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Acknowledgments
The authors thank the stakeholder advisory group members who contributed to design, implementation, and evaluation of this project; Shannon Meyers from the Community Academic Aging Research Network for facilitating our relationship with the partner community organizations; community site coordinators Gayle Laszewski, Jennifer Lefeber, Jane Jackson; TCP teachers Pat Culotti, Diane Brose, Rachel Sandretto, Sarah Watts; physical therapy data collection teams (Gwyn Straker, Michele Thorman, Georgia Corner, Rachel Thiel, Dan Schumann, Emily Durham, and Samantha Gallo); and students taking Tai Chi Prime. The authors also thank journal reviewers for their careful reading and suggestions for this manuscript.
Conflicts of Interest
Kristine M Hallisy was a co-author on Tai Chi Fundamentals (TCF) Adapted Program with Optional Side Support, Walker Support, and Seated Versions, published by Uncharted Country Publishing in 2015 used in the study, but does not receive royalties for the work. As a TCF certified instructor, Dr. Hallisy does receive honoraria for teaching TCF courses. The other authors have no financial or personal conflicts to report.
Author Contributions
Drs. Chewning, Hallisy, Mahoney led the team on study concept, design, measures selection acquisition of subjects, and data collection. Dale Wilson oversaw data collection and Dr. Gangnon joined Dr. Sangasubana in conducting the data analyses. Drs. Chewning and Hallisy led preparation of the manuscript for publication with Dr. Mahoney as a contributor along with Drs. Sangasubana and Gangnon.
Sponsor’s Role: The funding sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of the paper.
References
- Bandura A. (1997). Self-efficacy: The exercise of control. New York: WH Freeman. [Google Scholar]
- Borrelli B. (2011). The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of Public Health Dentistry, 71, S52–S63. doi:10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns E., & Kakara R (2018). Deaths from falls among persons aged ≥65 years—United States, 2007–2016. MMWR. Morbidity and Mortality Weekly Report, 67, 509–514. doi:10.15585/mmwr.mm6718a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2016). STEADI stopping elderly accidents, deaths, & injuries Retrieved June 7, 2018, from https://www.cdc.gov/steadi/about.html
- Centers for Disease Control and Prevention (CDC) (2017). STEADI materials for health care providers, functional assessments Retrieved June 7, 2018, from https://www.cdc.gov/steadi/materials.html
- Chunharas S. (2006). An interactive integrative approach to translating knowledge and building a “learning organization” in health services management. Bulletin of the World Health Organization, 84, 652–657. doi:10.2471/BLT.05.026922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemson L., Fiatarone Singh M. A., Bundy A., Cumming R. G., Manollaras K., O’Loughlin P., & Black D (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. BMJ, 345, e4547. doi:10.1136/bmj.e4547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe L. J., St John J. A., Hariprasad S., Shankar K. N., MacCulloch P. A., Bettano A. L., & Zotter J (2017). An integrated approach to falls prevention: A model for linking clinical and community interventions through the massachusetts prevention and wellness trust fund. Frontiers in Public Health, 5, 38. doi:10.3389/fpubh.2017.00038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del-Pino-Casado R., Obrero-Gaitán E., & Lomas-Vega R (2016). The effect of tai chi on reducing the risk of falling: A systematic review and meta-analysis. American Journal of Chinese Medicine, 44, 895–906. doi:10.1142/S0192415X1650049X [DOI] [PubMed] [Google Scholar]
- Farrance C., Tsofliou F., & Clark C (2016). Adherence to community based group exercise interventions for older people: A mixed-methods systematic review. Preventive Medicine, 87, 155–166. doi:10.1016/j.ypmed.2016.02.037 [DOI] [PubMed] [Google Scholar]
- Fischer B. L., Gleason C. E., Gangnon R. E., Janczewski J., Shea T., & Mahoney J. E (2014). Declining cognition and falls: Role of risky performance of everyday mobility activities. Physical Therapy, 94, 355–362. doi:10.2522/ptj.20130195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florence C. S., Bergen G., Atherly A., Burns E., Stevens J., & Drake C (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66, 693–698. doi:10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R. E., Vogt T. M., & Boles S. M (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89, 1322–1327. doi:10.2105/AJPH.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackney M. E., & Wolf S. L (2014). Impact of Tai Chi Chu’an practice on balance and mobility in older adults: An integrative review of 20 years of research. Journal of Geriatric Physical Therapy (2001), 37, 127–135. doi:10.1519/JPT.0b013e3182abe784 [DOI] [PubMed] [Google Scholar]
- Hallisy KM. (2018). Health benefits of tai chi: Potential mechanisms of action. International Journal of Family and Community Medicine, 2, 261–264. doi:10.15406/ijfcm.2018.02.00091 [Google Scholar]
- Hu Y. N., Chung Y. J., Yu H. K., Chen Y. C., Tsai C. T., & Hu G. C (2016). Effect of tai chi exercise on fall prevention in older adults: Systematic review and meta-analysis of randomized controlled trials. International Journal of Gerontology, 10, 131–136. doi:10.1016/j.cnre.2015.10.003 [Google Scholar]
- Huang Z. G., Feng Y. H., Li Y. H., & Lv C. S (2017). Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open, 7, e013661. doi:10.1136/bmjopen-2016-013661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang T. T., & Wang W. S (2009). Comparison of three established measures of fear of falling in community-dwelling older adults: Psychometric testing. International Journal of Nursing Studies, 46, 1313–1319. doi:10.1016/j.ijnurstu.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Huston P., & McFarlane B (2016). Health benefits of tai chi: What is the evidence? Canadian Family Physician, 62, 881–890. Retrieved June 7, 2018, from www.cfp.ca/content/cfp/62/11/881.full.pdf [PMC free article] [PubMed] [Google Scholar]
- Important Facts about Falls (n.d). Retrieved June 7, 2018, from Centers for Disease Control and Prevention website, https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- Jiang D., Kong W., & Jiang J.J (2015). Study of tai chi practice in the United States. Annals of Community Medicine and Practice, 1, 1005 Retrieved June 7, 2018, from https://www.jscimedcentral.com/CommunityMedicine/communitymedicine-1-1005.pdf [Google Scholar]
- Jones C. J., Rikli R. E., & Beam W. C (1999). A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport, 70, 113–119. doi:10.1080/02701367.1999.10608028 [DOI] [PubMed] [Google Scholar]
- Kendrick D., Kumar A., Carpenter H., Zijlstra G. A., Skelton D. A., Cook J. R. . . Delbaere K (2014). Exercise for reducing fear of falling in older people living in the community. Cochrane Database Systematic Review, 11, Cd009848. doi:10.1002/14651858.CD009848.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh T. C. (1981). Tai chi chuan. American Journal of Chinese Medicine, 9, 15–22. doi:10.1142/S0192415X81000032 [DOI] [PubMed] [Google Scholar]
- Ladawan S., Klarod K., Philippe M., Menz V., Versen I., Gatterer H., & Burtscher M (2017). Effect of Qigong exercise on cognitive function, blood pressure and cardiorespiratory fitness in healthy middle-aged subjects. Complementary Therapies in Medicine, 33, 39–45. doi:10.1016/j.ctim.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Lan C., Chen S. Y., Lai J. S., & Wong A. M (2013). Tai chi chuan in medicine and health promotion. Evidence-Based Complementary and Alternative Medicine, 2013, 502131. doi:10.1155/2013/502131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Harmer P., Fisher K. J., McAuley E., Chaumeton N., Eckstrom E., & Wilson N. L (2005). Tai chi and fall reductions in older adults: A randomized controlled trial. Journal of Gerontology. Series A, Biological Sciences and Medical Sciences, 60, 187–194. doi:10.1093/gerona/60.2.187 [DOI] [PubMed] [Google Scholar]
- Li F., Harmer P., Fitzgerald K., Eckstrom E., Akers L., Chou L. S., . . . Winters-Stone K (2018). Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Internal Medicine, 178, 1301–1310. doi:10.1001/jamainternmed.2018.3915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu-Ambrose T., Ahamed Y., Graf P., Feldman F., & Robinovitch S. N (2008). Older fallers with poor working memory overestimate their postural limits. Archives of Physical Medicine and Rehabilitation, 89, 1335–1340. doi:10.1016/j.apmr.2007.11.052 [DOI] [PubMed] [Google Scholar]
- Lomas-Vega R., Obrero-Gaitan E., Molina-Ortega F. J., & Del-Pino-Casado R (2017). Tai chi for risk of falls. A meta-analysis. Journal of the American Geriatrics Society, 65, 2037–2043. doi:10.1111/jgs.15008 [DOI] [PubMed] [Google Scholar]
- Lusardi M. M., Fritz S., Middleton A., Allison L., Wingood M., Phillips E., . . . Chui K. K (2017). Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. Journal of Geriatric Physical Therapy (2001), 40, 1–36. doi:10.1519/JPT.0000000000000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney J. E., Gobel V. L., Shea T., Janczewski J., Cech S., & Clemson L (2016). Improving fidelity of translation of the stepping on falls prevention program through root cause analysis. Frontiers in Public Health, 4, 251. doi:10.3389/fpubh.2016.00251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansukhani S. G., Kieser M., Ricci D., & Chewning B (2017). Dose Orchestration and System Enhancement (DOSE): A practice model based on the Habituation-Intention Framework. Research in Social and Administrative Pharmacy: RSAP, 13, 1062–1069. doi:10.1016/j.sapharm.2016.11.001 [DOI] [PubMed] [Google Scholar]
- McAuley E. (1992). The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. Journal of Behavioral Medicine, 15, 65–88. doi:10.1007/bf00848378 [DOI] [PubMed] [Google Scholar]
- McPhate L., Simek E. M., & Haines T. P (2013). Program-related factors are associated with adherence to group exercise interventions for the prevention of falls: a systematic review. Journal of Physiotherapy, 59, 81–92. doi:10.1016/S1836-9553(13)70160-7 [DOI] [PubMed] [Google Scholar]
- Mullen S. P., Wojcicki T. R., Mailey E. L., Szabo A. N., Gothe N. P., Olson E. A. . . . McAuley E (2013). A profile for predicting attrition from exercise in older adults. Preventive Science, 14, 489–496. doi:10.1007/s11121-012-0325-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls D., Sweet L., Muller A., & Hyett J (2016). Teaching psychomotor skills in the twenty-first century: Revisiting and reviewing instructional approaches through the lens of contemporary literature. Medical Teacher, 38, 1056–1063. doi:10.3109/0142159X.2016.1150984 [DOI] [PubMed] [Google Scholar]
- Oulette J.A., & Wood W (1998). Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin, 124, 54–74. doi:10.1037/0033-2909.124.1.54 [Google Scholar]
- Picorelli A. M., Pereira L. S., Pereira D. S., Felício D., & Sherrington C (2014). Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. Journal of Physiotherapy, 60, 151–156. doi:10.1016/j.jphys.2014.06.012 [DOI] [PubMed] [Google Scholar]
- Rossiter-Fornoff J. E., Wolf S. L., Wolfson L. I., & Buchner D. M (1995). A cross-sectional validation study of the FICSIT common data base static balance measures. Journal of Gerontology. Series A, Biological Sciences and Medical Sciences, 50, M291–297. doi:10.1093/gerona/50A.6.M291 [DOI] [PubMed] [Google Scholar]
- Salthouse T. A. (2011). What cognitive abilities are involved in trail-making performance? Intelligence, 39, 222–232. doi:10.1016/j.intell.2011.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C., Michaleff Z. A., Fairhall N., Paul S. S., Tiedemann A., Whitney J., . . . Lord S. R (2017). Exercise to prevent falls in older adults: An updated systematic review and meta-analysis. British Journal of Sports Medicine, 51, 1750–1758. doi:10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- Steffen T. M., Hacker T. A., & Mollinger L (2002). Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Physical Therapy, 82, 128–137. doi:10.1093/ptj/82.2.128 [DOI] [PubMed] [Google Scholar]
- Stevens J. A. (2013). The STEADI tool kit: A fall prevention resource for health care providers. The IHS Primary Care Provider, 39, 162–166. Retrieved June 7, 2018, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4707964/ [PMC free article] [PubMed] [Google Scholar]
- Tai Chi for Falls Prevention (2016). Retrieved June 7, 2018, from National Council on Aging website, https://www.ncoa.org/wp-content/uploads/Tai-Chi-for-Falls-Prevention.pdf
- Tai Chi Fundamentals® Certification Process. (n.d.). Retrieved July 15, 2018, from Tai Chi Health website, http://taichihealth.com/?page_id=156
- Tombaugh T. N. (2004). Trail Making Test A and B: Normative data stratified by age and education. Archives of Clinical Neuropsychology, 19, 203–214. doi:10.1016/s0887-6177(03)00039-8 [DOI] [PubMed] [Google Scholar]
- Tousignant M., Corriveau H., Roy P. M., Desrosiers J., Dubuc N., Hébert R., . . . Beaudoin A. J (2012). The effect of supervised Tai Chi intervention compared to a physiotherapy program on fall-related clinical outcomes: a randomized clinical trial. Disability and Rehabilitation, 34, 196–201. doi:10.3109/09638288.2011.591891 [DOI] [PubMed] [Google Scholar]
- Wayne P. M., Walsh J. N., Taylor-Piliae R. E., Wells R. E., Papp K. V., Donovan N. J., & Yeh G. Y (2014). Effect of tai chi on cognitive performance in older adults: Systematic review and meta-analysis. Journal of the American Geriatrics Society, 62, 25–39. doi:10.1111/jgs.12611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., MacDonald H. V., & Pescatello L. S (2016). Evaluating exercise prescription and instructional methods used in tai chi studies aimed at improving balance in older adults: A systematic review. Journal of the American Geriatrics Society, 64, 2074–2080. doi:10.1111/jgs.14242 [DOI] [PubMed] [Google Scholar]
- Yu T.(Producer & Director). (2015). Tai Chi Fundamentals® adapted program with optional side support version [DVD]. Taos, NM: Uncharted Country Publishing. [Google Scholar]
- Yu T., & Hallisy K (2015). Tai Chi Fundamentals® adapted program with optional side support, walker support, and seated versions. Taos, NM: Uncharted Country Publishing. [Google Scholar]
- Yu T., & Johnson J (1999). Tai Chi Fundamentals® for health professionals and instructors: A simplified approach for mastering tai chi basics. Madison WI: Uncharted Country Publishing. [Google Scholar]
- Zhao Y., & Wang Y (2016). Tai chi as an intervention to reduce falls and improve balance function in the elderly: A meta-analysis of randomized controlled trials. Chinese Nursing Research, 3, 28–33. doi:10.1016/j.cnre.2015.10.003 [Google Scholar]
- Zheng G., Liu F., Li S., Huang M., Tao J., & Chen L (2015). Tai chi and the protection of cognitive ability: A systematic review of prospective studies in healthy adults. American Journal of Preventive Medicine, 49, 89–97. doi:10.1016/j.amepre.2015.01.002 [DOI] [PubMed] [Google Scholar]