Abstract
We present clinical and chest computed tomography (CT) features of 5 cases of pediatric patients with 2019 novel coronavirus. Two patients had fever and dry cough, whereas the rest of 3 patients were asymptomatic. Three patients had unilateral ground glass opacities with or without consolidation in the subpleural region on high-resolution chest CT, 1 patient had bilateral ground glass opacities, and 1 patient was negative for CT. We note that up to 66.7% asymptomatic patients had pulmonary lesions, so the asymptomatic children with Wuhan contact are recommended to do a 2019 novel coronavirus real-time fluorescence polymerase chain reaction screening. Unlike adult patients, only a small amount of patients had multilobes affected, so we speculate that the pediatric patients generally have milder CT findings than adults.
Key Words: coronavirus infections, tomography, x-ray computed, pneumonia, viral, pediatrics
The 2019 novel coronavirus (COVID-19) spread rapidly across China and even other countries, leading to a global panic. Recent studies showed that typical computed tomography (CT) findings included bilateral pulmonary parenchymal ground glass and consolidative pulmonary opacities, with a peripheral lung distribution.1–3 However, the clinical and radiological characteristics of pediatric patients have not been well known. Herein, we demonstrate change in the course of disease over time on high-resolution chest CT scan of 5 pediatric patients. This study was approved by the institutional review board (Certification Number ChiCTR2000029952). Written informed consent was obtained for each patient.
CASE REPORT
Case 1
A 5-year-old boy was admitted to the hospital with fever and dry cough for 3 days and diarrhea for 2 days. On admission, his body temperature was elevated (38.0°C). His blood routine test was normal. Real-time fluorescence polymerase chain reaction (RT-PCR) of the patient's throat swab was positive for COVID-19 nucleic acid. Unenhanced chest high-resolution CT (HRCT) showed subpleural ground glass opacities (GGO) with consolidation in the left lower lobe (Fig. 1A). After 5 days of treatment with ribavirin and interferon, the patient's temperature decreased to normal and repeat chest CT showed healing of the lesion (Fig. 1B). After 13 days after admission, repeat throat swab RT-PCR turned negative, and chest CT showed complete resolution (Fig. 1C).
FIGURE 1.
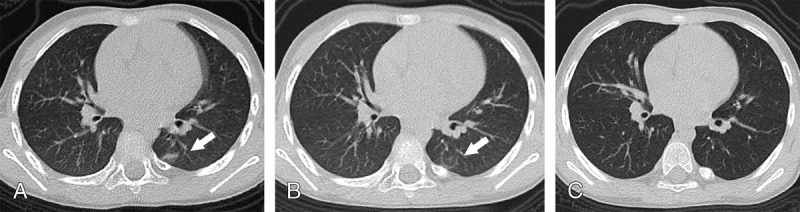
A 5-year-old boy with fever and dry cough for 2 days. High-resolution CT showed subpleural GGO with consolidation in the left lower lobe (A). After 5 days of treatment, repeat chest CT showed healing of the lesion (B). After 13 days after admission, chest CT showed complete resolution (C).
Case 2
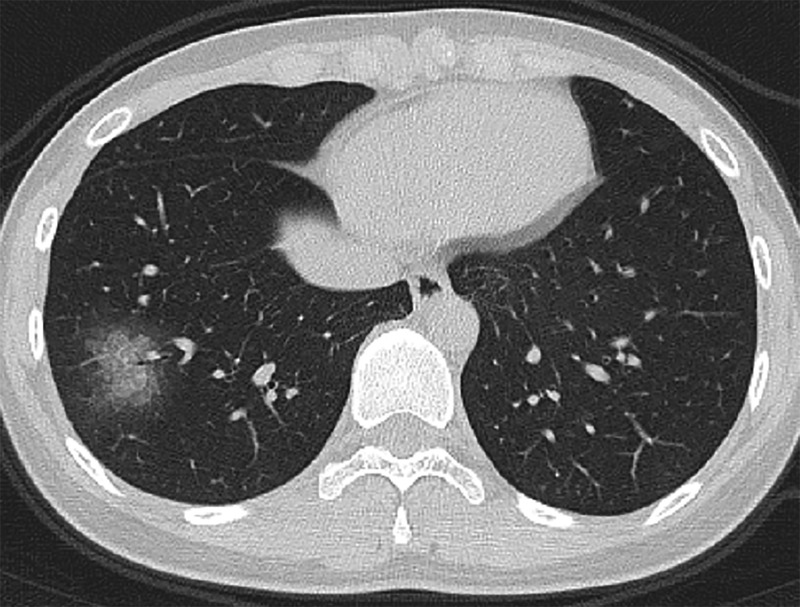
A 2-year-old asymptomatic boy was admitted to the fever clinic of our hospital because his grandpa was confirmed with COVID-19 infection. At admission, he was positive for COVID-19 RT-PCR. The initial HRCT and blood routine test were both normal. However, 6 days after admission, repeat HRCT showed subpleural GGO in bilateral upper lobes (Fig. 2). Repeat COVID-19 nucleic acid was still positive. After 3 days of treatment with ribavirin and interferon, COVID-19 RT-PCR was finally negative, and the follow-up CT scan showed complete resolution.
FIGURE 2.

High-resolution CT of a 2-year-old asymptomatic boy showed subpleural GGO in bilateral upper lobes.
Case 3
A 7-month-old girl was admitted to the hospital with dry cough for 2 days and fever for 1 day. Her mother was diagnosed with COVID-19 6 days ago. Her body temperature was slightly elevated (37.8°C). The initial RT-PCR was negative, but HRCT showed GGO in the upper lobe of the right lung. Repeat RT-PCR was positive on the third day of hospitalization. She was treated with interferon afterward. The GGO was healed 5 days after admission, but RT-PCR was still positive. Thirteen days after admission, throat swab RT-PCR turned negative.
Case 4
A 9-year-old male asymptomatic boy was admitted to the hospital because his father was confirmed with COVID-19 infection. His COVID-19 RT-PCR was positive and HRCT showed GGO in the right lower lobe (Fig. 3). After 7 days of treatment with ribavirin and interferon, both COVID-19 RT-PCR and HRCT turned negative.
FIGURE 3.
High-resolution CT of a 9-year-old asymptomatic boy showed areas of GGO distributed mainly along bronchovascular bundles in right lower lobe.
Case 5
A 13-year-old male asymptomatic boy was admitted to the hospital because his grandma was confirmed with COVID-19 infection. He was positive for initial COVID-19 RT-PCR but negative for HRCT. Three days later, his COVID-19 RT-PCR turned negative.
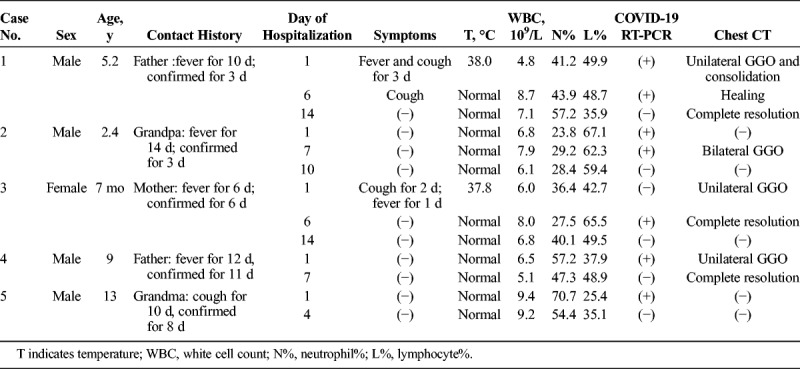
The clinical and HRCT features of all the 5 previously mentioned cases are summarized in Table 1.
TABLE 1.
Clinical and HRCT Characteristics of the Patients Included in the Present Study
DISCUSSION
The 2019 novel coronavirus mainly affects mid-age and elderly people,4 so little is known about the clinical and HRCT characteristics of pediatric patients. To the best of our knowledge, the present study is the first report of the HRCT and clinical features of pediatric patients with COVID-19 in the English literature. Two patients (case 1 and 3) in our study were symptomatic, both of them had fever and dry cough, and one of them had diarrhea in addition. Thus, fever and dry cough are 2 core symptoms of pediatric patients, which is in line with the adults.4 However, up to 60% of the patients (case 2, 4, and 5) in the present study were asymptomatic, so the asymptomatic children with Wuhan contact (lived or traveled to Wuhan or had close contact with any confirmed patients) are recommended to do a COVID-19 RT-PCR screening. Besides, we noted that up to 66.7% asymptomatic patients (case 2 and 4) had pulmonary GGO, so asymptomatic pediatric patients may be positive for HRCT, and thus, HRCT is recommended in the screening of suspected pediatric patients.
We note that there are many differences between the radiological findings of adult and pediatric patients with COVID-19. It is reported that up to 44% adult patients had all 5 lobes affected,1 whereas only 1 patient (case 2) in the present study affected bilaterally, and 3 patients just affected 1 lobe. The HRCT manifestations of adult patients with COVID-19 were reported to be very diverse1–3: most appeared as pure GGO, GGO with consolidation, interlobular septal thickening, bronchiolar wall thickening, and crazy paving pattern, whereas rare manifestations included halo sign, pleural effusion, pericardial effusion, and lymphadenopathy. In our series of pediatric patients, only GGO and consolidative GGO were found. Pan et al5 studied the time course of lung changes of adult COVID-19 patients and concluded that lung lesions would gradually be absorbed in 2 weeks. On the contrary, most lesions in our study were fully resolved in a week. Furthermore, Song et al3 divided the adult patients with COVID-19 to younger (<50 years) and elder group (>50 years) and found that elder group tended to have more areas of lung involvement and more consolidation. Taking their evidence together, we speculate that the pediatric patients generally have milder CT findings than adults.
In conclusion, we demonstrated 5 cases of pediatric patients with COVID-19, and we had the following three findings: (1) fever and dry cough are 2 core symptoms of pediatric patients; besides, asymptomatic children with Wuhan contact are recommended to do a COVID-19 RT-PCR screening; (2) HRCT is of great significance in the screening of suspected pediatric patients; and (3) the pediatric patients generally have milder CT findings than adults. The large sample studies are needed in the future.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020. doi: 10.1007/s00330-020-06731-x. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020;295:202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song F, Shi N, Shan F, et al. Emerging coronavirus 2019-nCoV pneumonia. Radiology. 2020;295:210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;200370. doi: 10.1148/radiol.2020200370200370. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


