Highlights
-
•
A compartmental model was used to simulate social distancing scenarios.
-
•
Magnitude and duration of social distancing needed to control pandemic are modeled.
-
•
Social distancing can be reduced if people exercise personal caution.
-
•
The most effective way to reduce social distancing is a stepping-down approach.
Keywords: COVID-19, Mathematical modeling, Compartmental model, Intervention strategies, Pandemic
Abstract
Objectives
To model the effects of continuous, intermittent, and stepping-down social distancing (SD) strategies and personal protection measures on COVID-19 transmission dynamics.
Methods
Constant, intermittent, and stepping-down SD strategies were modeled at 4 mean magnitudes (5%, 10 %, 15 % and 20 %), 2 time windows (40-days, 80-days), and 2 levels of personal caution (30 % and 50 %).
Results
The stepping-down strategy was the best long-term SD strategy to minimize the peak number of active COVID-19 cases and associated deaths. The stepping-down strategy also resulted in a reduction in total time required to SD over a two-year period by 6.5 % compared to an intermittent or constant SD strategy. An 80-day SD time-window was statistically more effective in maintaining control over the COVID-19 pandemic than a 40-day window. However, the results were dependent upon 50 % of people being cautious (engaging in personal protection measures).
Conclusion
If people exercise caution while in public by protecting themselves (e.g., wearing a facemask, proper hand hygiene and avoid agglomeration) the magnitude and duration of SD necessary to maintain control over the pandemic can be reduced. Our models suggest that the most effective way to reduce SD over a two-year period is a stepping-down approach every 80 days. According to our model, this method would prevent a second peak and the number of intensive care units needed per day would be within the threshold of those currently available.
1. Introduction
In an effort to contain the spread of COVID-19, the United States (US), like much of the world, implemented social distancing (SD) regulations. Updated models show a major decline in the number of predicted cases and deaths [1], indicating that SD is working. However, SD regulations cannot be sustained indefinitely. Therefore, in the absence of a vaccine or pharmaceutical treatment, it is important to understand long-term consequences of various SD strategies (i.e., type, duration, intensity, magnitude) on COVID-19 transmission dynamics.
Recently, Kissler and colleagues (2020) used a mathematical model to estimate the duration and intensity of SD to maintain control of COVID-19 over a 5-year period. The result indicated that the best-case scenario involved intermittent SD until 2022 [2]. Intermittent SD involves an on-again, off-again approach to SD. For example, the SD scenario modeled by Kissler et al. (2020) used a 60 % SD on – 60 % SD off approach. Note, that recently released location data to index SD compliance indicates mean levels closer to 40 % [3]. However, intermittent strategy is not the only alternative type of SD and other scenarios should be explored.
In addition, personal protection measures (PPM) such as wearing facemasks, frequently washing hands, and avoiding agglomerations may play a crucial role in preventing the spread of COVID-19 [4] and the Kissler model did not consider such factors. The purpose of the current investigation was to model the consequences of continuous, intermittent, and stepping-down SD strategies along with PPM on the transmission dynamics of COVID-19.
2. Methodology
2.1. The SUEIHCDR model
We extended a generalized Susceptible-Exposed-Infected-Recovered (SEIR) compartmental model using factors specific to COVID-19 [5,6] to investigate the COVID-19 pandemic in the US. It is composed of eight compartments: Susceptible, Unsusceptible, Exposed, Infected, Hospitalized, Critical, Dead, and Recovered (SUEIHCDR) (Fig. 1 ).
Fig. 1.
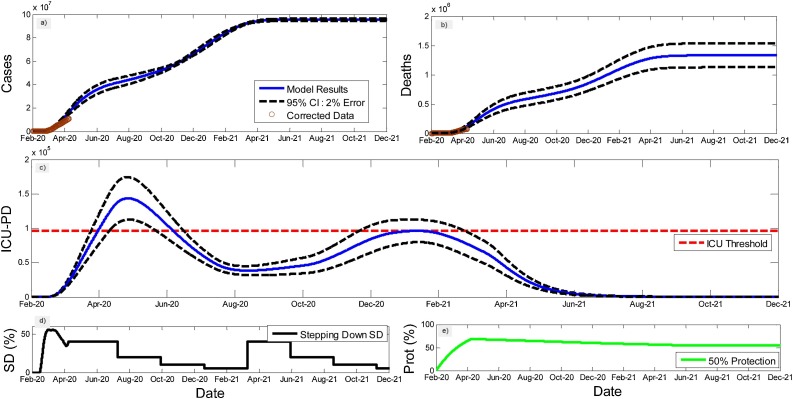
Fitting results for accumulated cases (a) and deaths (b) for US. And an illustration of the 95 % confidence interval estimated for the ICU beds used per day ICU-PD (c) for one example of scenarios illustrating a “stepping-down” SD strategy (d) with a minimum protection percentage of 50 % (e).
The SUEIHCDR model assumes that as time progresses, a susceptible person out of the population (Npop) (Eq. 1) can either become unsusceptible (Eq. 2) considering a protection rate (α; Eq. 9; [23]) or exposed (Eq. 3) to the virus considering social distancing (SD) and an infection rate (β). This protection rate was introduced to account for possible decreases in the number of susceptible people to the virus caused by factors other than social distancing such as the use of facemasks, hand washing, maintaining at least 5 feet to other people and avoiding agglomerations. Exposed people become infectious after an incubation time of 1/γ (Eq. 4). Infected people stay infected for a period of 1/δ and can recover with no medical attention (m) or can be hospitalized (1-m). Hospitalized people (Eq. 5) stay hospitalized for 1/ζ days and can either recover (1-c) or become critical (c) needing to go to an Intensive care unit (ICU). A person stays on average 1/ ε in the ICU (Eq. 6) and can either go back to the hospital (1-f) or die (f; Eq. 7). Recovered people (Eq. 8) can come from infection (m) or from the hospital (1-c).
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
| (7) |
| (8) |
| (9) |
where is the maximum or minimum possible value for a window of time and is the final time of the window. Alpha was optimized considering the window of time from the beginning of the pandemic until present day, and it was manipulated afterwards in different windows of time to project possible future scenarios. Changes in α causes changes in the number of people that are unsusceptible to the disease at a given time; we exhibit alpha manipulations as the percentage ratio of the unsusceptible or protected people over the country’s population (i.e. Protection (%)). Note, that insusceptibility in our model accounts for a time-dependent state of an individual that because of his/her behavior can change from susceptibility to insusceptibility or the other way around.
Furthermore, social distancing until present day was determined from mobility data trends from Apple Maps [3]. Data were low-pass filter filtered at 0.09 Hz (Butterworth 4th order), and minimum values from baseline were considered. From present day forward SD was manipulated in different windows of time to project possible future scenarios.
2.2. Solving and testing the model
We used the fourth order Runge-Kutta numerical method to solve our system of ordinary differential equation in MATLAB (MathWorks Inc.R14a).
2.3. Optimization
We used both accumulated cases and deaths time series to fit the model, both corrected by a factor (Table 01). Cases sub-test factor was calculated as the ratio between the death rate in Iceland (country with the greatest percentage of test per inhabitant [7]), corrected by age stratification (older adults (60+): 6.4 %; senior older adults (80+): 13.4 % [8]). Death sub-factor was determined using recent reports [9,10].
Fitting analysis was done with a custom build MATLAB global optimization algorithm using Monte Carlo iterations and multiple local minima searches. The algorithm was tested for the best solution considering all inputs varying within ranges obtained from the WHO [10] and several publications [[11], [12], [13]] (Table 1 ). Infected initial values (I0) were determined from corrected accumulated cases as well as initial death values (D0). Other initial values were set proportional to I0 considering model parameters (m, c, f); all initial parameters could vary during optimization as well (Table 1). Data under 500 active cases were discarded.
Table 1.
Optimized coefficients for US on May 04, 2020, respective ranges and correcting factors for accumulated cases (Factor C) and deaths (Factor D).
| Coeffs | Fit | Lower B. | Upper B. |
|---|---|---|---|
| α | 0.026 | 0.01 | 0.12 |
| β | 0.60756 | 0.5 | 1.2 |
| γ | 1.90320 | 0.5 | 5 |
| δ | 0.10013 | 0.07 | 0.5 |
| ζ | 0.21124 | 0.2 | 0.33 |
| ε | 0.08669 | 0.05 | 0.14 |
| m | 0.93330 | 0.65 | 0.99 |
| c | 0.34732 | E0/2 | 2.00E+00 |
| f | 0.49915 | I0/2 | 2I0 |
| E0 | 813 | H0/2 | 2H0 |
| I0 | 531 | C0/2 | 2C0 |
| H0 | 457 | Re0/2 | 2Re0 |
| C0 | 9 | D0/2 | 2.00E+00 |
| Re0 | 0 | ||
| D0 | 0 | ||
| R0 | 4.28 | ||
| FactorC | 8.94 | ||
| FactorD | 1.07 | ||
| Latent | 0.5 | ||
| Infectious | 10.0 | ||
| Hospitalized | 4.7 | ||
| Critical | 11.5 |
2.4. Future projections
After the fitting, the coefficients were used to model 48 possible future scenarios considering 3 strategies of mitigation: 1) a stepping- down strategy (starting at a specific SD, it is divided by half for the next 3 time windows, on the fifth time window SD is back to its initial value, and the process is repeated); 2) a standard intermittent SD strategy (a specific SD value alternates with periods of no SD); and 3) a constant SD strategy (SD is kept constant at as specific value). For the stepping-down strategy and for the intermittent strategy we used 4 different maximum SD values: 40 %, 30 %, 20 % and 10 %. Constant SD strategy was simulated with 20 %, 15 %, 10 % and 5% values. SD values were chosen so that different strategies had similar average SD across time; note however, that average SD values across time tends to be 6.25 % smaller for the stepping-down strategy compared to the other two (intermittent using same maximum value and constant using half of the maximum value). Times windows were either 40 or 80 days. Every scenario was simulated with protection percentage decreasing with time and eventually plateauing at either 50 % or 30 %. We had 48 scenarios: 3 strategies x 4 SD values x 2 time-windows x 2 protection endpoints.
A Confidence Interval of 95 % was estimated using Monte Carlo for a 2% error for all coefficients to measure the confidence in the model results, to test if future projected scenarios were statistically different at a 5% level, and to compare model results to actual ICU numbers (Fig. 1). Confidence interval projected lines were not included in all the figures for clarity. Model results were based on an average of 5000 runs. Peak ICU estimations were compared to data obtained from DATAUSA coronavirus database [14].
3. Results
Our model was able to accurately fit the corrected accumulated cases and deaths data for the US (Fig. 1). On the day of the analysis (May 4, 2020), SD was 40 % and protection was 68 %. All optimized coefficients, as well as the latent period, infectious period, hospitalized period, ICU period and reproductive number (R0) estimated from the model can be found in Table 1.
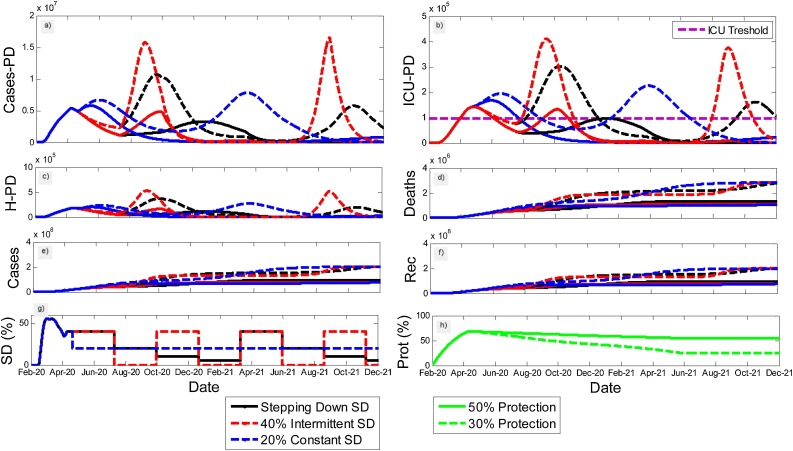
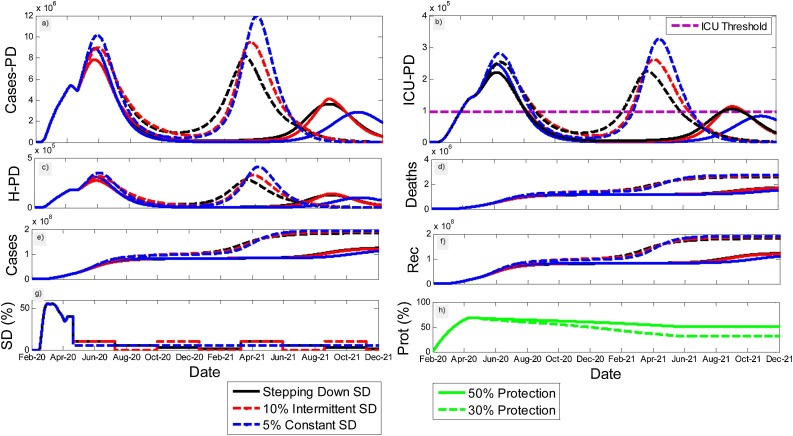
Our results suggest 40 % SD until mid-July can significantly help decrease the current peak of the pandemic in the US (Fig. 1). No strategy was able to safely contain the pandemic with values of protection dropping to 30 % (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6 ). Considering the 50 % protection scenario, a 40 % intermittent strategy (20 % average SD) produced a second peak in active cases by the end October (Fig. 2a) that caused the number of ICU beds used per day to pass the ICU threshold (Fig. 2b). The stepping-down strategy pushed the peak in cases to January 2021 (Fig. 2a) with peak in ICU matching statistically ICU threshold (Fig. 2b).
Fig. 2.
Model results for active cases per day (a), total ICU beds per day (b), hospitalizations per day (c), accumulative deaths (d), accumulative cases (e), accumulative recuperated cases (f), as well as SD strategies (g), and protection percentage (h) in USA. Initial stepping down SD starts at 40 %, then it is divided by half for the next 3 windows, and the pattern repeats itself from the start (80 days/window); intermittent SD alternate 40 % and 0; constant strategy keeps SD at 20 % for the total duration of the pandemic. Protection percentage drops from current estimated values of 68 % to either 50 % or 30 %.
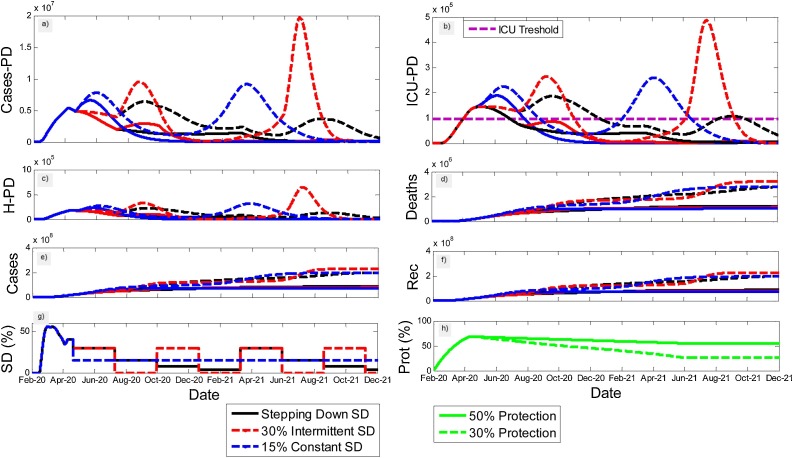
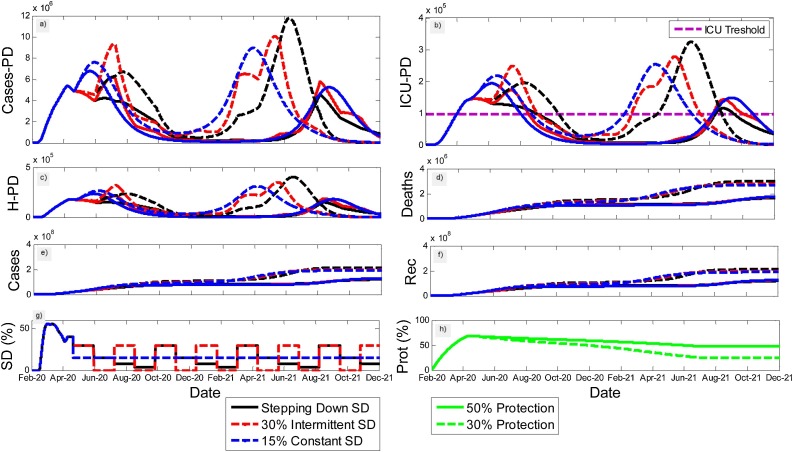
Fig. 3.
Model results for active cases per day (a), total ICU beds per day (b), hospitalizations per day (c), accumulative deaths (d), accumulative cases (e), accumulative recuperated cases (f), as well as social distancing (SD) strategies (g), and protection percentage (h) in US. Initial stepping-down SD starts at 30 %, then it is divided by half for the next 3 windows, and the pattern repeats itself from the start (80 days/window); intermittent SD alternate 30 % and 0; constant strategy keeps SD at 15 % for the total duration of the pandemic. Protection percentage drops from current estimated values of 68 % to either 50 % or 30 %.
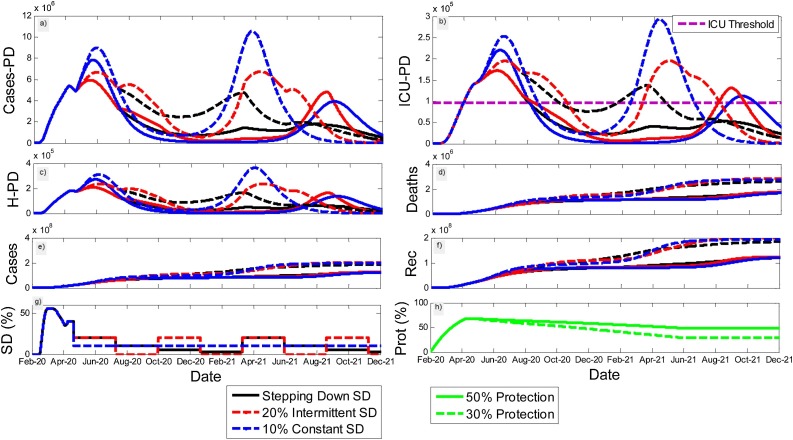
Fig. 4.
Model results for active cases per day (a), ICU beds per day (b), hospitalizations per day (c), accumulative deaths (d), accumulative cases (e), accumulative recuperated cases (f), as well as social distancing (SD) strategies (g), and protection percentage (h) in US. Initial stepping-down SD starts at 20 %, then it is divided by half for the next 3 windows, and the pattern repeats itself from the start (80 days/window); intermittent SD alternate 20 % and 0; constant strategy keeps SD at 10 % for the total duration of the pandemic. Protection percentage drops from current estimated values of 68 % to either 50 % or 30 %.
Fig. 5.
Model results for active cases per day (a), total ICU beds per day (b), hospitalizations per day (c), accumulative deaths (d), accumulative cases (e), accumulative recuperated cases (f), as well as social distancing (SD) strategies (g), and protection percentage (h) in US. Initial stepping-down SD starts at 10 %, then it is divided by half for the next 3 windows, and the pattern repeats itself from the start (80 days/window); intermittent SD alternate 10 % and 0; constant strategy keeps SD at 5% for the total duration of the pandemic. Protection percentage drops from current estimated values of 68 % to either 50 % or 30 %.
Fig. 6.
Model results for active cases per day (a), total ICU beds per day (b), hospitalizations per day (c), accumulative deaths (d), accumulative cases (e), accumulative recuperated cases (f), as well as social distancing (SD) strategies (g), and protection percentage (h) in US. Initial-stepping down SD starts at 30 %, then it is divided by half for the next 3 windows, and the pattern repeats itself from the start (40 days/window); intermittent SD alternate 30 % and 0; constant strategy keeps SD at 15 % for the total duration of the pandemic. Protection percentage drops from current estimated values of 68 % to either 50 % or 30 %.
Additionally, the results indicate that a 15–20 % constant SD starting May 15 cause a slight increase in the current peak (Figs. 2a and 3 a) but contained the pandemic until the end of 2021 (Fig. 2, Fig. 3). Alternatively, a steady 10 % SD caused a significant increase in the current peak and led to a drop in active cases to lower than 100, 000 after the peak. However, because of the drop, the number of remaining susceptible people was great enough to lead to a second peak (Fig. 4a).
Moreover, no intermittent strategy scenario was efficient in containing the pandemic (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6), but the best intermittent scenario was with 80 days on and off windows and with SD of 30 % (Fig. 3) when on, not 40 % (Fig. 2). At this scenario, containment of the first peak was better than in the 15 % constant SD, but a second peak that matched the ICU threshold would happen in October 2020 (Fig. 3b). A similar scenario, with 20 % SD pushed the second peak to September 2021 passing the ICU threshold (Fig. 4b).
The best strategy studied considering the containment of the first peak, controlling the pandemic to avoid a second peak, and smaller mean social distance across the pandemic period was the stepping-down strategy (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6). Notably, when minimum protection was 50 % and 80-day windows were used, both stepping down from 30 % and 20 % SD effectively controlled the second peak in active cases (Figs. 3a and 4 a). In both scenarios peak ICU per day were kept under the threshold after the first peak. Regarding the first peak, however, only stepping down from 30 % could significantly stop the growth of the first peak in active cases (Fig. 3a).
Finally, no strategies using SD percentages of 10 % could attenuate the course of the pandemic (Fig. 5) and for every matching scenario analyzed an 80-days window yielded better results than a 40-days window (Fig. 6).
4. Discussion
We used a SUEIHCDR compartmental model to project 48 scenarios for the transmission dynamics of COVID-19 through the next two years based upon three different SD strategies (continuous, intermittent, and stepping-down) at 4 different mean values (5%, 10 %,15 %), 2 time windows (40 days, 80 days), and 2 minimum levels of protection (30 %, 50 %).
4.1. Personal protection measures
Our model highlighted the importance of PPM in maintaining control of the pandemic. More specifically, our simulations suggest that a minimum protection of 50 % is necessary to avoid another spike in COVID-19 cases and associated deaths. A protection percentage of 50 % indicates that half of all people are actively engaged in behavior that will minimize the likelihood of contracting the virus (e.g. wearing facemasks, frequently washing hands, using hand sanitizer, maintaining at least 5 feet to other people and avoiding agglomerations) [[15], [16], [17]]. This finding is consistent with research indicating that wearing facemasks regardless of symptoms is crucial for mitigating the spread of COVID-19 [15] and recommendations by the CDC [18]. In fact, the Manhattan Project for COVID- 19 recommend that the US require all citizens to use facemasks in public [19]. Public use of facemasks are common in China and other nations in Asia. However, many US citizens report that facemasks are uncomfortable and inconvenient with some refusing to comply with the recommendations [20]. As such, policy mandates may be needed to increase public adherence to using personal protection equipment.
4.2. Social distancing
With the economic burden of SD increasing and people growing weary of restrictions there is major concern with how a decline in SD will affect COVID-19 infections and associated deaths. At the peak of the pandemic in the US, our analysis of location data [3] indicated that the magnitude of SD was at 60 %, just a few weeks later, current levels are at 40 % SD. According to our projections, some level of SD needs to continue over the next two years. If the US stops practicing social distancing (SD = 0) or maintains levels lower than 10 % our simulations indicate the pandemic will quickly worsen and deplete available health resources. This result is consistent with models indicating that SD may be in place for an extended period [2]. Interestingly, however, our models indicate the more critical factor in the best-case scenarios was the level of personal caution (engaging in PPM). If personal caution levels were maintained at 50 %, SD could be reduced to 15 % average across time without crossing the threshold for available ICU beds. Increasing SD to an average of 20 % was not more beneficial. Although 20 % average SD was effective at maintaining control of the first peak, the second peak was in fact much larger. This result is consistent with the notion that a one-time SD may result in a catastrophic second peak, if the virus reoccurred and not enough people have immunity [2,21]. Alternatively, intermittent strategies may allow for periods of transmission resulting in herd immunity without overwhelming hospital resources [2,22]. Indeed, the Kissler model [2] indicated that intermittent SD was the best-case scenario to maintain control over the pandemic. Note, however, that previous COVID-19 projection models have not explored scenarios associated with stepping-down strategies.
4.3. Stepping-down strategies
Our model indicates that the most effective way to reduce SD over a two-year period is a stepping-down approach. Such an approach involves gradual stair-step declines in SD. The approach we modeled was multiplying SD values of 40 %, 30 % and 20 % by 1, then 1/2, then 1/4, then 1/8 and then back to 1 and repeat. Similar, to the argument made for intermittent SD a stepping-down strategy may allow for periods of transmission without burdening hospital resources. Our modal indicated that the stepping-down was more effective at maintaining control over the pandemic than intermittent SD. In addition, the modeled stepping-down strategy resulted in a reduction in total time required to SD over a two-year period by 6.5 % compared to the best intermittent and constant strategies. A 6.5 % reduction in the time required to SD may have significant economic and psychological benefits. The best-case scenario indicated by our model was a stepping-down strategy with an 80-day window. That is, an 80-day period in between each SD level. According to our model, this scenario prevented a second peak while the number of ICUs needed per day was within the threshold of those currently available.
5. Conclusion
Our model highlighted the importance of personal protection measures such as wearing facemasks and proper hand-washing hygiene in maintaining control over the COVID-19 pandemic. In addition, the results indicate the most effective way to reduce SD over a two-year period is a stepping-down approach every 80 days. According to our model, this method would prevent a second peak and the number of ICUs needed per day would be within the threshold of those currently available.
Funding source
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors
Informed consent and patient details
Patients did not participate in this study.
Data sharing statement
All data used in the study are included in the references.
CRediT authorship contribution statement
Deanna M. Kennedy: Conceptualization, Data curation, Writing - original draft. Gustavo José Zambrano: Methodology. Yiyu Wang: Data curation, Writing - original draft. Osmar Pinto Neto: Conceptualization, Formal analysis, Methodology, Supervision, Writing - original draft.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank Apple, CDC, IHME, and journals that have made data and information relative to COVID-19 publicly available. We would also like to thank José Clark Reis, Ana Carolina Brisola Brizzi, Joabe Marcos de Souza, Wellington Amorim Pedroso, Rodrigo Cunha de Mello Pedreiro, Bruno de Matos Brizzi and Ellysson Oliveira Abinader for helping us during this research project and all the frontline workers risking their lives to help others during the COVID-19 pandemic.
References
- 1.Institute for Health Metrics and Evaluation (IHME) 2020. COVID-19 Projections.https://covid19.healthdata.org/united-states-of-america Available at: [Google Scholar]
- 2.Kissler S.M., Tedijanto C., Goldstein E. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020 doi: 10.1126/science.abb5793. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Apple . 2020. Mobility Trends Reports.https://www.apple.com/covid19/mobility Available from: [Google Scholar]
- 4.Hillier M.D. Using effective hand hygiene practice to prevent and control infection. Nurs Stand. 2020;35(5):45–50. doi: 10.7748/ns.2020.e11552. [DOI] [PubMed] [Google Scholar]
- 5.APMonitor Optimization Suite . 2020. COVID-19 Optimal Control Response.https://apmonitor.com/do/index.php/Main/COVID-19Response Available: [Google Scholar]
- 6.Covid-19- scenarios. ©2020. Available in: https://covid19-scenarios.org/about.
- 7.Gudbjartsson D.F., Helgason A., Jonsson A.H. Early spread of SARS-Cov-2 in the icelandic population. N. Engl. J. Med. 2020:1–34. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verity R., Dorigatti I., Winskill P. Estimates of the severity of coronavirus deases 2019: a model-based analysis. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.County Miami-Dade. Second Round of COVID-19 Community Testing Completed; Miami-dade County and the University of Miami Miller School of Medicine Announce Initial Findings. https://www.miamidade.gov/releases/2020-04-24-sample-testing-results.asp Available at:
- 10.World Health Organization (WHO); 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 Available at: [Google Scholar]
- 11.Ranjan R. Estimating the final epidemics size for COVID-19. medRxiv. 2020;1:1–15. doi: 10.1101/2020.04.12.20061002. [DOI] [Google Scholar]
- 12.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y., Gayle A.A., Wilder-Smith A. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020;27(2):1–4. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Data U.S.A. COVID-19 in the United States. https://dataU.S.A.io/coronavirus Available at:
- 15.Lee J.K., Jeong H.W. Wearing facemasks regardless of symptoms is crucial for preventing spread of COVID-19 in hospitals. Infect. Control Hosp. Epidemiol. 2020 doi: 10.1017/ice.2020.202. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin Y.H., Liu C.H., Chiu Y.C. Google searches for the keywords of "wash hands" predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.020. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kratz A., Todt D., V’kovski P. Inactivation of severe acute respiratory syndrome coronavirus 2 by WHO-Recommended hand rub formulations and alcohols. Emerg Infect Dis. 2020 doi: 10.3201/eid2607.200915. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Center for Disease Control and Prevention (CDC) 2020. Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-based Transmissions.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face Available: [Google Scholar]
- 19.Cahill . 2020. Scientist to Stop COVID-19. The Manhatten COVID-19 Project.https://s.wsj.net/public/resources/documents/Scientists_to_Stop_COVID19_2020_04_23_FINAL.pdf Available: [Google Scholar]
- 20.9News . 2020. We Asked Our Medical Expert to Respon to the Reasons Why People Don’t Wear Facemasks.https://www.9news.com/article/news/health/coronavirus/doctor-responds-to-reasons-for-not-wearing-masks/73-d2c5c731-da4a-4fc0-b8d7-b0195e9abf50 Available at: [Google Scholar]
- 21.Kwok K.O., Wei W.I., Wong S.Y.S. Herd immunity - estimating the level required to halt the COVID-19 epidemics in affected countries. J Infec. 2020 doi: 10.1016/j.jinf.2020.03.027. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valdez L.D., Macri P.A., Braunstein L.A. Intermittent social distancing strategy for epidemic control. Phys. Rev. E Stat. Nonlin. Soft Matter Phys. 2012;85(3 PT 2) doi: 10.1103/PhysRevE.85.036108. [DOI] [PubMed] [Google Scholar]