IN DECEMBER 2019 a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disease (coronavirus-2019 [COVID-19]) was reported in Wuhan, China, and it rapidly spread across the world.1 On February 21, a 78-year-old man became the first person in Europe to die as a result of COVID-19 in a community hospital in Veneto, a region of about 5,000,000 people located in northeast Italy. Since then, SARS-CoV-2 has become a relentless epidemic in Italy, with a dramatic increase in the number of patients showing COVID-19–related acute respiratory failure and hypoxemia. Considering the epidemiologic data reported from China,2 , 3 it was immediately clear that the number of COVID-19 patients requiring hospital and intensive care unit (ICU) admission would rapidly overwhelm the total ICU capacity, thereby resulting in an unexpected systemic crisis due to the imbalance between increased healthcare demand and potential of supply.4
As soon as the first COVID-19 victim in Italy was recorded, an emergency technical and scientific committee was promptly formed by the local government of Veneto to coordinate the response to the emergency of the SARS-CoV-2 outbreak in the region. The task force included 10 experts on infectious diseases, intensive care, and health management.
The aim of this article is to describe how the region of Veneto dealt with the COVID-19 epidemic crisis and to summarize the urgent measures adopted to prevent the breakdown of the healthcare system.
Local Adopted Measures
From the beginning of the SARS-CoV-2 outbreak, in addition to the progressively adopted national restrictive measures, the Veneto local government immediately acted to limit the spread of the virus throughout the region. In addition, a COVID-19–dedicated coordinating center was promptly set up, aiming to manage and strategically organize medical activity.
Containment Measures
To slow the viral transmission, strict containment measures were adopted immediately. The initial cluster in Vo’, which is near Padua, was isolated through quarantine, and the entire population were administered COVID-19 tests. Both inhabitants and healthcare personnel who came into contact with the first COVID-19 patients without appropriate personal protective equipment (PPE) were isolated until they tested negative for SARS-CoV-2.
Furthermore, a number of policies aimed at curbing in-hospital contagion were introduced, including the following: progressive suspension of ordinary services, with the exception of urgent and oncological cases; mandatory use of surgical masks for anyone within hospital premises; and restricted access to hospital wards for visitors.
Creation of Dedicated Pathways for Patients With COVID-19
In every hospital of the region, a separate access to the emergency department for patients with confirmed or suspected SARS-CoV-2 infection was provided to minimize contact among patients. All patients with respiratory symptoms and fever were considered suspected for COVID-19 and were clinically evaluated and screened in new dedicated triage areas, often located outside the emergency department. They were managed with isolation measures until proven clear of SARS-CoV-2, whereas patients positive for infection were discharged home or admitted to the hospital according to the severity of clinical conditions and laboratory tests. Dedicated COVID-19 medical wards and ICUs were established, and a regional network was created to monitor and manage the distribution of COVID-19 patients.
Healthcare providers working with COVID-19 patients were equipped with maximum PPE, according to the World Health Organization guidelines.5 The type of PPE used when caring for COVID-19 patients varied according to different settings and type of activity, as detailed in the Supplemental Material (Supplemental Table 1). Entry to COVID-19 facilities was restricted to assisting personnel only, and external consulting and patient transfers for examination were strictly limited to essential cases.
Increasing ICU and Medical Ward Capacity
Before the SARS-CoV-2 outbreak, the ICU capacity in Veneto was 438 beds across 36 hospitals, for a total of 1 ICU bed every 11,200 inhabitants.
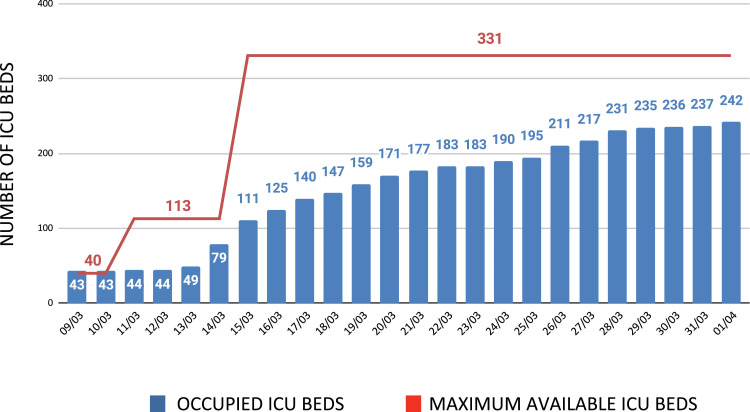
Based on the data arising from the outbreak in China, which reported a 5% ICU admission rate (2.6%-8%), it became clear that the expected number of critically ill COVID-19 patients would not have been manageable in Veneto without increasing ICU capacity.6, 7, 8 As a consequence, 24 additional ICU beds were made available immediately, and over the following 15 days, another 311 ICU beds were created ex novo, accounting for a 71% increase of total ICU beds (Fig 1 ). Such an increase in ICU reception capacity would not have been possible by allocating patients exclusively to hub hospitals. Therefore, several hospitals also were involved to create a regional ICU network. The selected hospitals were required to place COVID-19 patients in dedicated ICUs or in areas separated from the rest of the ICU beds and to report every positive critically ill COVID-19 patient to the regional coordinating center.
Fig. 1.
Number of newly created intensive care unit beds. ICU, intensive care unit.
To meet the appropriate number of healthcare providers (physicians, nurses, and social health operators) required to staff the newly created ICU beds, lower-priority surgical procedures were canceled and operating room personnel were reassigned to the ICUs. Basic training and adequate instructions about safe PPE use were guaranteed for beginner ICU personnel. Moreover, training video tutorials were published online (https://www.youtube.com/channel/UCd2rd2RjAbwkqBVQnweE51Q/playlists).
In parallel, respiratory high-dependency unit capacity was increased by 353%, by both creating new units and adding supplemental beds to the existing ones. The respiratory high-dependency units are areas where patients can be cared for more extensively than on a normal ward but not to the point of intensive care. Respiratory high-dependency units were staffed by pulmonologists already familiar with the treatment of respiratory failure and were dedicated to hypoxemic patients requiring noninvasive respiratory assistance, such as high-flow oxygen therapy and noninvasive ventilation, including continuous positive airway pressure. The patient-to-nurse ratio was less than that of a typical ward but more than that in an ICU. The surge of respiratory high-dependency units aimed to save ICU beds for the most critically ill patients who required invasive mechanical ventilation and multiple organ support therapies. Furthermore, this strong enhancement created an intermediate step between the ordinary medical ward and the ICU, allowing for a more rapid ICU discharge and patient turnover. The number of beds in COVID-19–dedicated medical wards also was increased and the healthcare provision was strengthened by instructing personnel on high-flow oxygen therapy and continuous positive airway pressure use.
Shared Therapeutic Strategies
The regional scientific committee developed specific process flows and protocols for the management of COVID-19 patients and shared them with all affiliated hospitals to standardize the therapeutic strategies between hub and spoke hospitals.
A decisional algorithm with easily available clinical parameters was adopted to help medical ward physicians choose the proper supplementary oxygen therapy and adequate ventilatory support (Supplemental Fig 1). Furthermore, clear indications for the safe tracheal intubation and protective lung ventilation were provided (Supplemental Figs 2 and 3). Extracorporeal membrane oxygenation was considered a rescue therapy for the most critically ill COVID-19 patients for whom lung- protective ventilation and pronation strategies failed.9, 10, 11, 12
Because there were no drugs specifically approved for the treatment of SARS-CoV-2 infection nor widely corroborated guidelines, the regional scientific committee proposed a policy whereby antiviral pharmacologic support would escalate in line with the severity of the infection (Supplemental Table 2).
Epidemiologic Data
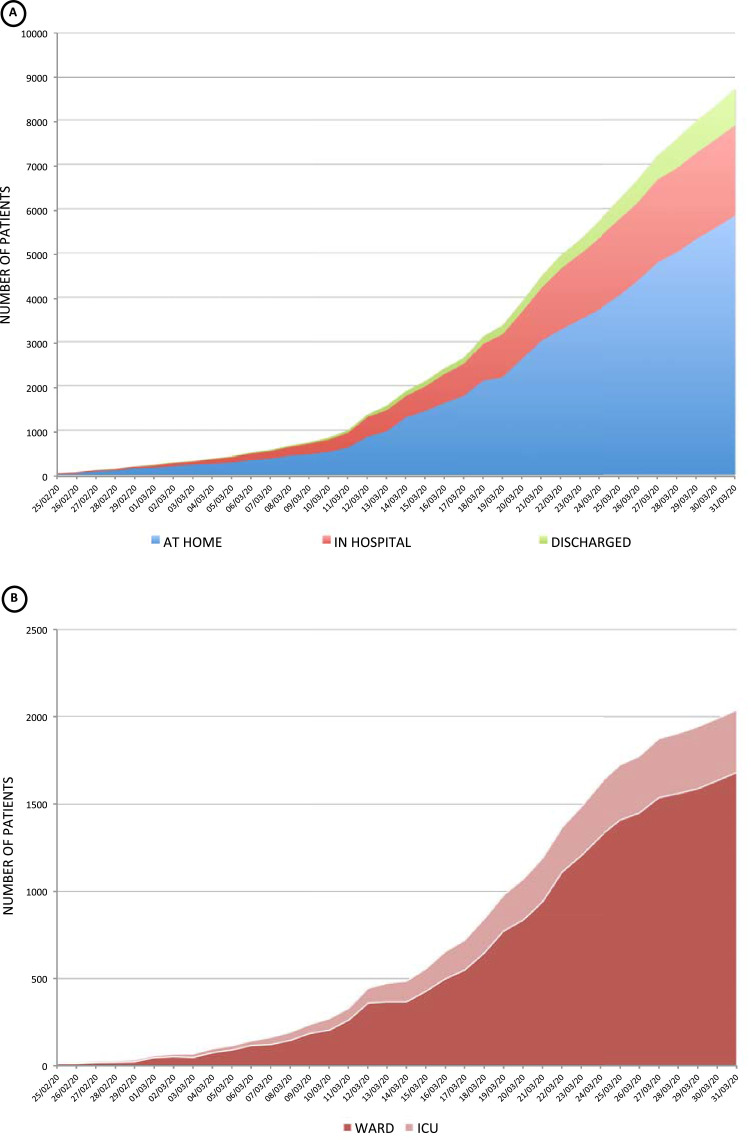
On April 1, 2020, a total of 110,574 official COVID-19 patients were registered in Italy, 9,625 (8.7%) of whom were in the region of Veneto,10 where a total of 112,746 COVID tests were performed. On the same date, 13,155 deaths occurred in Italy, including 488 in Veneto. As the number of infections dramatically increased during 6 weeks, hospital admissions also increased. Fortunately, most patients did not need hospitalization. In fact, only 3,487 (36.2%) required hospital admission, 10% of whom required treatment in the ICU (Fig 2 ). The median age of patients who required hospital admission was 71 (interquartile range [IQR] 58-81) years, and 63% were men. Median hospital stay was 8.0 [IQR 4-12] days, and the median ICU stay was 11 [IQR 6-18] days.
Fig. 2.
(A) Number of coronavirus-2019 patients in Veneto, Italy, from February 25 to March 31, 2020. Blue area, coronavirus-2019 patients managed at home. Red area, coronavirus-2019 patients requiring hospital admission. Green area, coronavirus-2019 patients discharged from hospital. (B) Number of coronavirus-2019 patients in Veneto, Italy, from February 25 to March 31, 2020. Dark red area, coronavirus-2019 patients managed in the medical ward. Light red area, coronavirus-2019 patients requiring intensive care unit admission. ICU, intensive care unit.
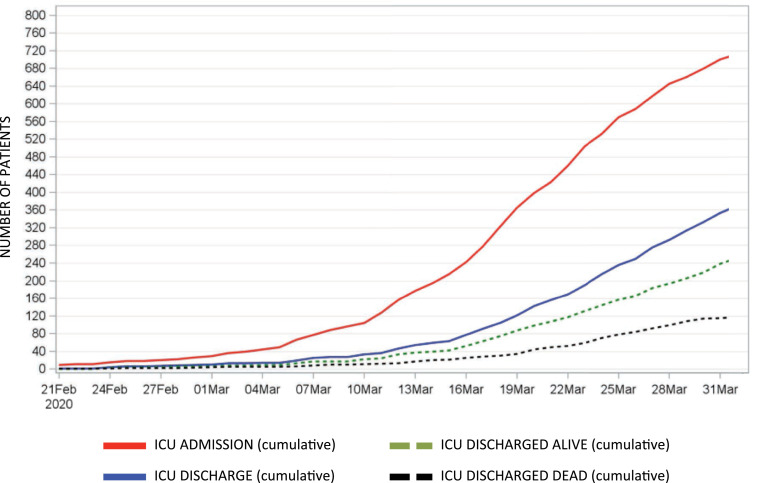
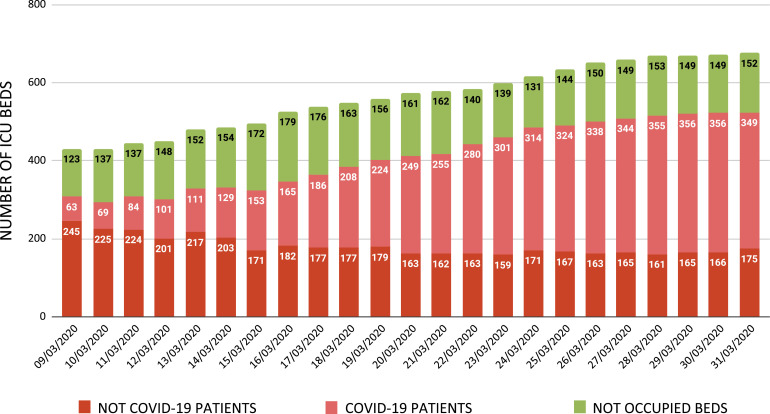
Until the beginning of March, the number of patients requiring ICU admission roughly matched the number of patients discharged or who died in an ICU. In the following weeks, however, the number of patients requiring ICU admission exceeded the number of deaths or discharged patients (Fig 3 ). Nonetheless, the occupancy rate of ICUs in the region remained constant, consequent to the increase of available beds (Fig. 1 and 4 ). The number of ICU beds occupied by non-COVID-19 patients decreased over time (see Fig 4), which likely could be ascribed to the suspension of ordinary surgical activity with planned postoperative ICU monitoring and to the reduction in the number of major traumas as a consequence of the restrictions imposed on everyday life activities. Therefore, the usual triage decision-making for ICU admission did not need to be modified, and all patients requiring advanced life support therapies were allocated easily.
Fig. 3.
Number of patients admitted to the intensive care unit (red line) and discharged from the intensive care unit (blue line) in Veneto, Italy, from February 21 to March 31, 2020. Patients discharged from the intensive care unit alive (dashed green line) are distinct from patients who died in the intensive care unit (dashed black line). ICU, intensive care unit.
Fig. 4.
Number of intensive care unit beds in Veneto, Italy, from March 9 to 31, 2020. Dark red bars, intensive care unit beds occupied by non-coronavirus-2019 patients. Light red bars, intensive care unit beds occupied by coronavirus-2019 patients. Green bars, nonoccupied intensive care unit beds. COVID-19, coronavirus-2019; ICU, intensive care unit.
Among COVID-19 patients admitted to hospital, 488 (14%) died. Among them 311 (63.7%) were men. The mortality rate for patients who recovered in ordinary wards was significantly less than that of patients admitted to the ICU (12% v 32%; p < 0.0001). The median age of patients who died in ordinary wards was significantly greater than that of patients who died in the ICU (84 [IQR 79-89] v 75 [IQR 69-79]; p < 0.05).
Conclusions
Veneto was one of the most affected regions in Italy by the COVID-19 epidemic. The increase of ICU beds associated with the aforementioned measures, aimed at treating milder or hypoxemic respiratory failure cases outside the ICUs, allowed for ICU bed provision for all patients with indication. Overall, the strategies adopted prevented the breakdown of the regional healthcare system.
Conflict of Interest
None.
Footnotes
Supplementary material associated with this article can be found in the online version, at doi:10.1053/j.jvca.2020.05.005.
Appendix. Supplementary materials
References
- 1.Zhu N, Zhang D, Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Guan X, Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA. 2020 Mar 13 doi: 10.1001/jama.2020.4031. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). Available at:https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed February 24, 2020.
- 6.Yang X, Yu Y, Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D, Hu B, Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1601–1609. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie J, Tong Z, Guan X. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020 Mar 2 doi: 10.1007/s00134-020-05979. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ELSO COVID-19 Working Group. Extracorporeal Life Support Organization COVID-19 interim guidelines. A consensus document from an international group of interdisciplinary ECMO providers. Available at: https://www.elso.org/Portals/0/Files/pdf/guidelines%20elso%20covid%20for%20web_Final.pdf. Accessed Feb 24, 2020. [DOI] [PMC free article] [PubMed]
- 10.Hong X, Xiong J, Feng Z. Extracorporeal membrane oxygenation (ECMO): Does it have a role in the treatment of severe COVID-19? Int J Infect Dis. 2020;94:78–80. doi: 10.1016/j.ijid.2020.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): Pooled analysis of early reports. J Crit Care. 2020;58:27–28. doi: 10.1016/j.jcrc.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ñamendys-Silva SA. ECMO for ARDS due to COVID-19. Heart Lung. 2020 Mar 26 doi: 10.1016/j.hrtlng.2020.03.012. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.