Abstract
This comment discusses the contribution of population movement to the spread of COVID-19, with a reference to the spread of SARS 17 years ago. We argue that the changing geography of migration, the diversification of jobs taken by migrants, the rapid growth of tourism and business trips, and the longer distance taken by people for family reunion are what make the spread of COVID-19 so differently from that of SARS. These changes in population movement are expected to continue. Hence, new strategies in disease prevention and control should be taken accordingly, which are also proposed in the comment.
Keywords: COVID-19, SARS, Population movement, Spread, China
The initial outbreak of 2019 novel coronavirus disease (COVID-19) quickly became a far greater global health concern than severe acute respiratory syndrome (SARS) was in 2003 (Wang et al., 2020). Despite being closely related, COVID-19 has infected far more people, over a larger geographical area, and within a shorter time, than SARS (Chan et al., 2020; Heymann & Shindo, 2020; Lu et al., 2020).
The different spread of COVID-19 from SARS has been attributed most often to their differences in disease dynamics (Heymann and Shindo, 2020; Wilder-Smith et al., 2020). For example, asymptomatic and pre-symptomatic patients, who are often missed and not isolated, can transmit COVID-19 but cannot spread SARS (Wilder-Smith et al., 2020). The basic reproductive number (R0) of COVID-19, albeit still emerging, is now estimated to have a mean of 3.28 and a median of 2.79, both higher than the equivalent figures of SARS (Liu et al., 2020).
Regardless of their differences in disease dynamics, both COVID-19 and SARS are introduced from animals to human populations, transmitted by human-to-human contact, and spread widely first in China. Hence, if we want to know why the coronavirus spreads so differently to SARS, limiting our attention to the virus per se is not enough. We should also consider how the patterns of population movement in China have changed so much in the most recent 17 years.
First, unlike SARS, COVID-19 has achieved nationwide and global spread without the help of urban super-stars. In China, the epicentre of COVID-19 is still in Wuhan, a city previously largely unheard of by most people outside China. In contrast, although SARS emerged in Foshan, it was not nationally spread until the epicentre moved to China's capital, Beijing.
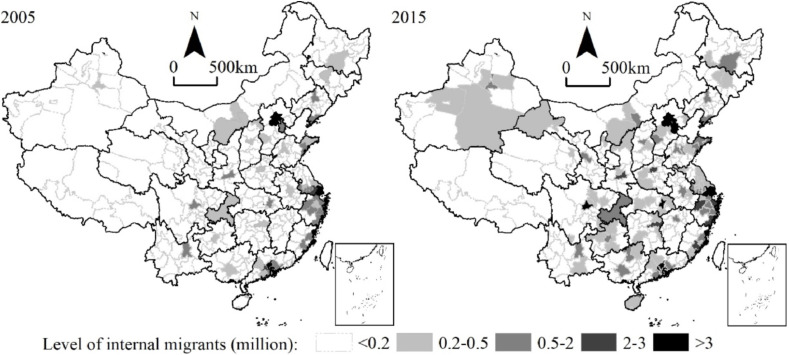
China's migration landscape is radically different from 17 years ago. (Fig. 1) In the 2002–2003 SARS outbreak, there were 2.87 million migrants in Beijing with a population share of 20.15 per cent. These proportions in cities like Foshan and Wuhan were less than half that in Beijing. 17 years later, Wuhan is now the home to 2.24 million internal Chinese migrants, and their population share has risen to 20.25 per cent; higher than the equivalent figure of Beijing in 2003 (National Bureau of Statistics of China, 2020; Statistical Bureau of Wuhan, 2020).
Fig. 1.
Geographical distribution of internal migrants in China (2005, 2015). Source: 1% Population Census in China (2005, 2015).
During the inter-epidemic period, internal migrants in China have become much less concentrated in a few coastal cities, and more evenly distributed across the whole country (Liu et al., 2015). This change is closely related to China's transformation from an export-oriented economy toward a consumption-based one (Lardy, 2016). The closing economic gap between the coast and inland under China's strong commitment to regional balanced development has also made a contribution (Démurger and Xu, 2011). Moreover, the continued strictness of getting household registration (hukou) in first-tier cities and the recent lift of restrictions elsewhere have facilitated a geographically more even distribution of internal migrants in China (Liu and Shi, 2019). A future nationwide epidemic is now possible to be triggered from almost any large city; its control in future will be even harder again.
Ordinary cities outside the heart of the outbreak have been hit harder by COVID-19 than they were by SARS. In Wenzhou, a city outside Hubei province, 504 COVID-19 cases were confirmed by February 19th (Health Commission of Wenzhou, 2020). This already surpasses the highest number of confirmed SARS cases outside the epicentre, which was found in Taiyuan, the capital city of Shanxi province, to be 325 in 2003 (Tan et al., 2005).
Of migrant workers returning to Wenzhou in 2020, more people are classified as entrepreneurs than rural-urban job-seekers. Compared to job-seekers, entrepreneurs are more socially integrated in both origin and destination, so more easily become infected, and are also more likely to spread the disease. These highly active migrants have expanded with the structural upgrading and spatial integration of the Chinese economy. Surveys from the National Health Commission in China show a 1.7 percentage-point rise in the share of entrepreneurs among migrants between 2010 and 2017.
Apart from entrepreneur-migrants, internal student-migrants have also increased. According to the latest population census, their number in Wuhan reached 1.25 million in 2015, over one third of which were inter-provincial student-migrants. In spreading COVID-19, however, their contribution should be limited (Zhang, 2020). Most student-migrants had already returned home long before the escalation of the outbreak, as the 2019 autumn term ended around January 10th. They were unlikely to carry the virus then because they spent almost all of their term time in self-sufficient gated campuses and had extremely low contact with the outside world. But this fact also means that if a future virus emerges on campus, it will spread quickly among students who come from all over the country and can carry the virus home. Even more ordinary cities that are seemingly insignificant in the current landscapes of migration are expected to be hit severely by future epidemics.
Changing migration and hence movement patterns within China mean that COVID-19 travels further and quicker than SARS. SARS never reached Hainan province, a holiday island in China. But many COVID-19 cases were found there even before the Chinese Spring Festival, and reached 168 by February 20th (Health Commission of Hainan, 2020).
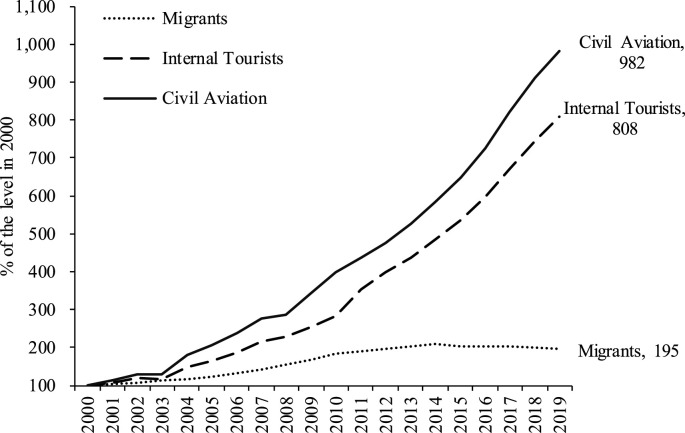
Tourism and business travel have boomed in China and contributed to the nationwide spread of COVID-19. (Fig. 2 ) The seaside resort Sanya has the highest number of confirmed cases in Hainan province, although its population is less than one third of that in the capital city Haikou (Health Commission of Hainan, 2020). Tourists move much more frequently than migrants both between and within places; their movement is free and sporadic, and their potential to spread the disease is both stronger and not restricted by time. Internal tourist numbers have more than tripled since 2002, and their numbers continue to rise (National Bureau of Statistics of China, 2020). A future nationwide endemic could occur at any time and spread even wider and more quickly than in 2020.
Fig. 2.
Trends in migration, internal tourism, and civil aviation in China (2000–2019). Source: China Statistical Yearbook 2019; Statistical Communiqué of the People's Republic of China (2019).
Changes in patterns of population movement may also partly explain why COVID-19 has a higher share of cluster cases occurring within family and social circles than did SARS. Until February 11th, 83 per cent of the cluster outbreaks of COVID-19 were reported to occur among family members (Xinhua, 2020). In contrast, the famous cluster outbreaks of SARS mostly occurred due to mixing in public places, such as the Metropole Hotel in Hong Kong (Heymann and Shindo, 2020).
The COVID-19 outbreak was escalated because of its synchronisation with the Chinese New Year, a time in China for reunion (Shi and Liu, 2020). Returning to hometown in this period is not limited to internal-migrants; it is also practiced by people having settled down in new places. Returnees not only reunite with extended family members, but also with local friends. This practice of reunion is an old tradition. But now people travel longer distances to achieve reunion and have a larger social circle to reunite than before. This timing led to a rhetoric that the virus had arrived at a bad time, when both travel and flu seasons were in full swing (Chan et al., 2020). The Spring Festival will continue being a bad time for controlling endemics in China; but it is more important to understand how rapidly the patterns and frequency of general population movement in China have changed in recent years, rather than to blame the ancient Spring Festival.
The draconian measures taken by China to contain the COVID-19 outbreak have resulted in a sharp and steady drop of new confirmed cases since February 3rd. But they have also brought huge societal and economic costs to China and its people (Hui et al., 2020). Reflections on how we can now better prepare are required, especially now we know that future epidemics can be so quickly and widely spread from almost anywhere in China, at any time. First, health resources should be more evenly distributed and more equally accessible. Second, local authorities should be empowered and required to raise the capability needed for dealing with public health events. Third, real-time data and new technologies should be better used and shared in epidemiological surveillance and for disease control. Fourth, the national stockpile of medical equipment such as ventilators, masks and gowns should be taken more seriously. Last, as the increased movement of people becomes a norm, the epidemic should motivate us to understand that increasingly, either internally or internationally we are all migrants.
Funding
This work is supported by the National Natural Science Foundation of China (41801146), COVID-19 Special Fund of Peking University and the PEAK Urban programme funded by UKRI's Global Challenge Research Fund (ES/P011055/1).
Declaration of competing interest
None.
References
- Chan J.F., Yuan S., Kok K., To K.K., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Démurger S., Xu H. Return migrants: the rise of new entrepreneurs in rural China. World Dev. 2011;39(10):1847–1861. doi: 10.1016/j.worlddev.2011.04.027. [DOI] [Google Scholar]
- Health Commission of Hainan . 2020. Update on Pneumonia Caused by the New Coronavirus Infections 20/02/2020; p. 2020.http://wst.hainan.gov.cn/yqfk/ [Google Scholar]
- Health Commission of Wenzhou . 2020. Update on Pneumonia Caused by the New Coronavirus Infections 20/02/2020; p. 2020.http://wjw.wenzhou.gov.cn/art/2020/2/20/art_1209919_41953307.html [Google Scholar]
- Heymann D.L., Shindo N. COVID-19: what is next for public health? Lancet. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., I Azhar E., Madani T.A., Ntoumi F., Kock R., Dar O. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health — the latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lardy N.R. China: toward a consumption-driven growth path. In: Zhou Y., editor. Seeking Changes: the Economic Development in Contemporary China (85-111): World Scientific. 2016. (Reprinted. [Google Scholar]
- Liu T., Qi Y., Cao G., Liu H. Spatial patterns, driving forces, and urbanization effects of China's internal migration: county-level analysis based on the 2000 and 2010 censuses. J. Geogr. Sci. 2015;25(2):236–256. doi: 10.1007/s11442-015-1165-z. [DOI] [Google Scholar]
- Liu T., Shi Q. Acquiring a Beijing hukou: who is eligible and who is successful? China Q. 2019:1–14. doi: 10.1017/S0305741019001541. [DOI] [Google Scholar]
- Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Trav. Med. 2020;27(2) doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics of China . 2020. Annual Data 20/02/2020; p. 2020.http://www.stats.gov.cn/english/Statisticaldata/AnnualData/ [Google Scholar]
- Shi Q., Liu T. Should internal migrants be held accountable for spreading COVID-19? Environ. Plann.: Econ. Space. 2020:308518X–2091676X. doi: 10.1177/0308518X20916764. [DOI] [Google Scholar]
- Statistical Bureau of Wuhan . 2020. Statistical Communiqué of Wuhan on National Economic and Social Development 20/02/2020; p. 2020.http://tjj.wuhan.gov.cn/newslist.aspx?id=2012111010452022 [Google Scholar]
- Tan J., Mu L., Huang J., Yu S., Chen B. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59(3):186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xinhua . 2020. More than 80 Pct of Cluster Coronavirus Cases Occur in Families: Expert 20/02/2020; p. 2020.http://www.xinhuanet.com/english/2020-02/11/c_138774791.htm [Google Scholar]
- Zhang Y. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]