As of April 15, 2020, the number of confirmed coronavirus disease-2019 (COVID-19) cases in New York City (NYC) was >110,000, thus making it the global epicenter of the pandemic (1). This rapid surge in the number of cases imposed a major burden on all hospitals in NYC, as well as causing significant stress in emergency departments (EDs). In addition, public health messages promoting social distancing and news reports focusing on the death toll associated with COVID-19 have created a sense of generalized anxiety in society. Changes in the observed incidence of acute cardiovascular conditions have been anecdotally reported, including the occurrence of ST-segment elevation myocardial infarctions (2). Incidentally, the number of at-home deaths in NYC has reached an 8- to 10-fold increase compared with the same time period in 2019, thereby raising concerns about the impact of the pandemic on non–COVID-related health conditions.
Acute type A aortic dissection is a life-threatening condition for which the only effective treatment requires surgical intervention, and the portal to initial diagnosis is invariably the ED. In the absence of emergency surgical intervention, 30-day mortality after acute type A aortic dissection ranges from 50% to 60% (2). The COVID-19 crisis has created additional challenges in EDs, such as more layers of screening through pre-ED triage and registration, reduced individual patient attention, rationing of timely computed tomography scanning, and confusion of atypical symptoms of type A aortic dissection with common COVID-19 presentations.
To investigate the impact of the COVID-19 pandemic on the incidence of acute type A aortic dissections, we compiled data from all hospitals and health systems providing cardiac surgery in NYC (N = 11). This approach allowed us to capture all cases of surgical repair of acute type A aortic dissections from January 1, 2018 to April 15, 2020. No change in the management of acute type A aortic dissection was reported by any of the centers. All patients with acute type A aortic dissection in NYC underwent emergency open repair. Univariable linear regression was used to calculate the estimated decrease in monthly procedural volumes between the before–COVID-19 and after–COVID-19 periods. The cutoff between before and after COVID-19 was March 1, 2020, corresponding to the first reported case in NYC. Because this study includes no protected health information, Columbia University’s Institutional Review Board advised that this study was exempt from Institutional Review Board submission.
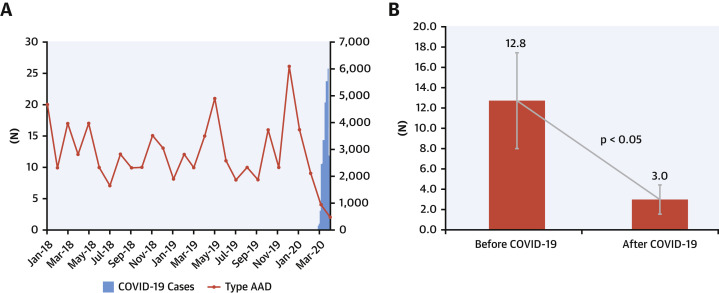
There was a significant and precipitous drop in the monthly surgical case volume of acute type A aortic dissection from 12.8 ± 4.6 cases/month before COVID-19 to 3.0 ±1.0 cases/month after COVID-19; this change represented a 76.5% decrease in volume (Figures 1A and 1B ). This decline was statistically significant by regression analysis (9.8; 95% confidence interval: 2.95 to 16.67; p = 0.007). Low volumes in 2 consecutive months (March and April 2020) further confirmed the unusual nature of the observation. Given the known seasonal effect with a higher incidence of aortic dissections during the winter months (3), analysis of the volumes in the 4 months (January to April) of the last 3 years further confirmed the unusually low volumes after COVID-19.
Figure 1.
Trend of Type A Repair Volume
(A) Variation in monthly volumes of surgically treated acute type A aortic dissections (AAD) (red line, left vertical axis) and coronavirus disease-2019 (COVID-19) cases (blue bar, right vertical axis) in New York City from January 1, 2018 to April 15, 2020. (B) Decrease in average monthly volumes before and after COVID-19 (p < 0.05).
Although no causal relationship can be firmly established among the drop in type A aortic dissections, the COVID-19 outbreak in NYC, and the increase in at-home deaths since the last week of March 2020, this gives pause for thought. Several hypotheses may explain this observation, including patient fear of contracting COVID-19 if presenting to the ED, overstretched first responders causing undue delays, or overburdened EDs causing delayed or missed diagnoses. Importantly, this finding raises important public health concerns about the unintended consequences of the COVID-19 pandemic. It is critical, as we adjust to the pandemic, to balance the public health imperative of social distancing with the individual need to consult in the presence of sudden severe symptoms. Furthermore, additional resources, ranging from telemedicine to numbers of first responders, should be greatly increased. This serves as a word of caution for cities yet to experience a surge in COVID-19 cases, as well as for future similar events.
Footnotes
Please note: Dr. Brinster has served on the Speakers Bureau of Terumo Aortic and Cook Medical. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. Christoph A. Nienaber, MD, PhD, served as Guest Associate Editor for this paper. P.K. Shah, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.New York City Department of Health COVID-19 Data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Available at:
- 2.Hagan P.G., Nienaber C.A., Isselbacher E.M. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903. doi: 10.1001/jama.283.7.897. [DOI] [PubMed] [Google Scholar]
- 3.Mehta R.H., Manfredini R., Hassan F. Chronobiological patterns of acute aortic dissection. Circulation. 2002;106:1110–1115. doi: 10.1161/01.cir.0000027568.39540.4b. [DOI] [PubMed] [Google Scholar]