Abstract
Since December 2019, the outbreak of novel coronavirus disease 2019 became a major epidemic threat in China and later spread worldwide. During the coronavirus disease 2019 outbreak in mainland China, the Chinese Obstetricians and Gynecologists Association distributed guidelines regarding the care of gynecologic patients. These guidelines were developed by the Department of Obstetrics and Gynecology at the Peking Union Medical College Hospital and represent an effort to integrate infection control strategy and promote professionalism in medical practice. The guidelines represent collaboration with experts from 31 provinces and autonomous regions of mainland China over 2 weeks’ time. With the implementation of these guidelines, no nosocomial infections of coronavirus disease 2019 have been identified at the Peking Union Medical College Hospital. We think these guidelines might be helpful to departments of obstetrics and gynecology internationally during these unprecedented times. In our guidelines, we describe basic infection precaution principles, an epidemiologic screening tool, prioritization of surgical procedures, and operating room requirements. Using these principles, we then review the management of gynecologic patients during the coronavirus disease 2019 epidemic in the outpatient and operative and nonoperative inpatient settings and in clinical trials.
Key words: coronavirus, COVID-19, gynecology, SARS-CoV-2
The impact of the novel coronavirus disease 2019 (COVID-19) pandemic is catastrophic, with the cumulative number of confirmed worldwide cases reaching 1,610,909 by April 11, 2020.1 Despite the necessary reassignment of many healthcare resources to the care of patients with COVID-19, gynecologic patients must still receive a diagnosis and be treated. Therefore, guidelines for the safe management of these patients during the epidemic are needed to protect patients and the healthcare workforce.1 The Chinese Obstetricians and Gynecologists Association (COGA) organized experts from all provinces and autonomous regions in mainland China (Wuhan included) to contribute their experience in the diagnosis and treatment during the epidemic, aiming to distribute guidelines regarding the care of gynecologic patients during the COVID-19 outbreak in mainland China. These guidelines were developed by the Department of Obstetrics and Gynecology at the Peking Union Medical College Hospital (PUMCH)2 and represent an effort to integrate infection control strategy and promote professionalism in medical practice. The guidelines represent collaboration with experts from 31 provinces over 2 weeks' time. With the implementation of these guidelines, no nosocomial infections of COVID-19 have been identified at PUMCH. Given that it is not easy to anticipate when the epidemic will peak and the understanding of COVID-19 is still changing,3 parts of this consensus statement may become obsolete as knowledge about the epidemic evolves.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus behind the COVID-19 pandemic, belongs to the genus Betacoronavirus. Transmission of SARS-CoV-2 virus between individuals can occur through viral shedding, independent of manifestation of symptoms. SARS-CoV-2 is mainly spread through respiratory droplets or direct contact. It may also be transmitted through aerosols with prolonged exposure to high concentrations of aerosol in an enclosed environment. Based on the current epidemiologic understanding, the incubation period of SARS-CoV-2 infections ranges from 1 to 14 days, most often from 3 to 7 days.4 SARS-CoV-2 nucleic acid can be detected in throat swabs, sputum or other lower respiratory tract secretions, blood samples, or stool.5 , 6 The virus is sensitive to ultraviolet radiation and heating. SARS-CoV-2 can be inactivated by heating at 56°C for 30 minutes and by using lipid solvents such as 75% ethanol, chlorine-containing disinfectant, and peroxyacetic acid and chloroform, but not by chlorhexidine.1
Consensus Guidelines
I. Infection precautions for healthcare personnel
Universal precautions and hierarchical precautions, extrapolated from standard aseptic or sterile techniques to the COVID-19 situation, should be followed in clinical work.4 The former refer to a series of measures to minimize the incidence of nosocomial infections based on the principle that patients’ blood, body fluids, secretions (excluding sweat), and incomplete skin and mucous membranes may contain infectious factors. Based on universal precautions, hierarchical precautions refer to contact precautions, spray precautions, airborne precautions, etc. Medical staff should pay attention to their actions during work and avoid close contact with each other in an unprotected state to reduce the possibility that 1 infected worker infects others.7
Gynecologic universal and hierarchical precautions could be taken as follows (based on the principles of universal and hierarchical precautions and local specific measures)8:
-
•
Primary precautions: working in an outpatient gynecology clinic or inpatient ward. Healthcare personnel should wear disposable work caps, medical surgical masks, and work clothes, and disposable latex gloves if necessary.
-
•
Secondary precautions: any caregiver in contact with patients with COVID-19 or persons under investigation. Healthcare personnel should wear disposable work caps, goggles or protective screens, medical protective masks (N95), protective clothing or disposable impermeable isolation clothing and disposable latex gloves, and disposable shoe covers if necessary.
-
•
Tertiary precautions: medical staff in fever clinics and isolation wards and staff performing gynecologic operations, emergency gynecologic treatments, invasive procedures on patients with suspected infection including sputum suction, lower respiratory tract sampling, tracheal intubation and tracheotomy, etc, which may cause splashing of patients’ respiratory secretions and body material. Healthcare personnel should wear disposable work caps, goggles or face shields, medical protective masks (N95), protective clothing, disposable latex gloves, and disposable shoe covers.
II. Infection precautions for operating room
Patients deemed to have a very low risk of COVID-19 infection can be cared for in ordinary operating rooms, and medical staff should follow primary precautions.
Surgery for a patient with suspected COVID-19 infection should be performed in a special operating room with negative air pressure, and the medical staff should follow tertiary precautions (as mentioned previously).
For any surgery in any operating room where there is concern of the patient being infected with COVID-19, the door of the operating room should be kept closed during the operation. Negative pressure with respect to the surrounding facilities should be maintained. The number of people entering and leaving and remaining in the operating room should be minimized. Equipment and supplies should be brought to the operating room door by specific external personnel and retrieved by specific personnel inside the operating room. Internal and external personnel, supplies, and equipment must not be mixed.
Operating rooms should use disposable equipment wherever possible. To prevent the surface of nondisposable and fixed objects in the operating room from being contaminated, disposable plastic films can also be used to cover the surface of diagnostic instruments and other surfaces. After the operation, these films should be treated as special contaminated medical waste. When medical devices or contaminated fabrics need to be sterilized, the operating room should notify disinfection supply centers and laundry rooms that these are COVID-19–contaminated material.
After conducting surgeries involving a patient suspected of having COVID-19, medical staff should take off the contaminated surgical gowns and then gloves and disinfect the hands when leaving the operating room.9 Environment and surface disinfection should follow the principle of cleaning first and then disinfecting. An infected operating room should only be used after cleaning for 30 minutes, terminal disinfection, and air disinfection.
Medical trainees (medical residents and students) who lack specific training and do not already have substantial surgical experience should not participate in surgery on patients with suspected COVID-19. The risk of a serious error by an inexperienced trainee could put many healthcare workers at risk.
III. Epidemiologic screening tool
This tool was developed for use during the COVID-19 pandemic (Figure 1 ).
Figure 1.
Epidemiologic screening tool
COVID-19, coronavirus disease 2019.
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
IV. Classification of surgical procedure priority
During the COVID-19 pandemic, each operation can be classified into 3 types according to urgency, including emergency surgery, “time-limited” surgery, and elective surgery. The details are as follows:
-
•
Emergency surgery: life-threatening circumstances requiring immediate surgical treatment such as trauma, acute abdomen, and massive hemorrhage; diseases specific to gynecology include ectopic pregnancy, ovarian torsion, uncontrollable uterine bleeding from cancer, pelvic mass causing severe symptoms, etc.
-
•
“Time-limited” surgery: this phrase is used to define those procedures needed to extend life; for example, operations on malignant tumors. Although the time of operation can be delayed, it should not be delayed for too long.
-
•
Elective surgery: an elective surgery refers to an operation that is neither emergency nor “time-limited.” This type of procedure is intended to improve the quality of life physically and/or psychologically; for example, excision of pelvic masses without high suspicion of malignancy, hysterectomy for benign diseases, etc.
V. Management of gynecologic patients
All the suggestions below use principles reviewed in I–IV.
1. Outpatient
There should be triage for outpatients. Patients suspected of having COVID-19 should go to the fever clinic for further treatment. In principle, suspected cases, probable cases, or confirmed cases should not be allowed to seek medical advice in the outpatient gynecology clinic. Avoid having people gathering in the waiting area. One doctor or provider should treat 1 patient at a time in the consulting room, and the consulting room should be disinfected immediately after use. During the COVID-19 pandemic, we recommend online or remote consultation by telephone as much as practical, to minimize the risk of disease spread by close contact. Figure 2 presents the outpatient triage protocol.
Figure 2.

Protocol for triage for outpatient clinic
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
2. Operative patient
In emergency surgery with sufficient time available for screening, patients who are clinically stable should be asked the screening questions listed in Figure 1, have their temperature assessed, and be checked for clinical symptoms to eliminate the possibility of COVID-19. If the possibility of a COVID-19 diagnosis cannot be completely ruled out, patients should go to the fever clinic for further screening (Figure 3 ). If the patient is clinically unstable or the patient’s condition is life-threatening, an emergency consultation with infection control experts may be useful. The decision may be made to treat the patient as a suspected case or even confirmed case (Figure 4 ).
Figure 3.
Workflow of preoperative instruction for stable emergency cases
COVID-19, coronavirus disease 2019; OR, operating room.
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
Figure 4.
Workflow of preoperative instruction for unstable cases
COVID-19, coronavirus disease 2019; OR, operating room.
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
For “time-limited” surgery, prehospital screening and education should be done. Inquiry using the screening questions in Figure 1 should be conducted before admission. Once the patient is admitted, the protocol for triage after admission should be followed. (Figure 5 ).
Figure 5.
Protocol for triage for newly admitted patient
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
In principle, it is recommended to reduce elective surgery during the epidemic. If the decision is made to perform elective surgery, the inquiry (screening questions) and triage protocol should be followed as for “time-limited” surgery.
Planning coordination throughout the hospital system, including the various surgical departments, anesthesia, and nursing services, is important in managing surgical services in the setting of a health emergency.10 Furthermore, adequacy of the blood supply must be considered when arranging operations.11 Autologous blood donation, acute normovolemic hemodilution, directed donation, and other methods can be considered as alternatives to allogenic blood transfusion.
3. Nonoperative inpatient
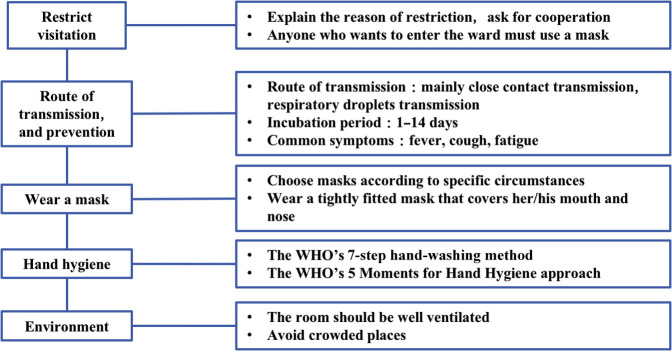
The triage protocol for a newly admitted patient is provided in Figure 5. Recommendations for ward management include the following: First, review the screening questions and take the temperature of patients, visitors, and accompanying persons; any patient with an elective admission or any nonpatient suspected of infection should be refused entry into the hospital. Second, visiting rules can be modified according to local preference. It is recommended to prohibit visiting, and if visitors cannot be avoided, the number of visitors should be no more than 1. Visitors must be screened. Third, if a patient develops fever that cannot be explained by the primary disease (requires judgment by the attending doctor or professor), a consultation with infectious disease specialists is recommended. Fourth, if a patient is identified to have COVID-19, the patient should be transferred to a facility that can provide an airborne infection isolation room. At the same time, everyone who has had close contact with the patient should be isolated (This is a recommendation from our experience in mainland China. If there is a shortage of local medical staff, the strategy can be modified according to the actual situation.). Fifth, rooms should be reserved for emergency use for patients with infections during the outbreak (for emergency operations and for emergency isolations). Sixth, provide education for patients and close contacts (Figure 6 ).
Figure 6.
Outline of education for patients and close contacts
WHO, World Health Organization.
Qiu, Management of gynecology patients during COVID-19 pandemic: Chinese expert consensus. Am J Obstet Gynecol 2020.
VI. Management of gynecologic clinical trials during the epidemic
The core guideline for clinical trials during the outbreak is that the safety of subjects and researchers is the first priority.
“Elective” clinical research that is not time-sensitive should be postponed until the current severe restrictions and precautions are lifted. If the research is time-sensitive, researchers should evaluate whether implementation of the clinical trial program will be significantly affected by the epidemic. If so, the research should be postponed if possible, or the research plan should be amended.
All parties in clinical trials should try to rely on the internet for communication, use information platform technology, and adopt remote collaborative work as much as possible for clinical trial management, to reduce the flow of clinical trial personnel and reduce the risk of disease transmission.
Consensus Statement
This consensus is made by experts in gynecology and obstetrics from 31 provinces and autonomous regions in China, based on their experience in diagnosis and treatment during the COVID-19 epidemic. With the implementation of these guidelines, no nosocomial infections of COVID-19 have been identified at PUMCH. These guidelines might be helpful to departments of obstetrics and gynecology internationally during these unprecedented times. The understanding of COVID-19 is still changing; therefore, parts of this consensus statement may become obsolete as knowledge about the epidemic evolves.
Acknowledgments
The authors acknowledge the thoughtful contributions of the expert team who participated in the consensus building without compensation. Experts from the Chinese Obstetrics and Gynecologists Association (COGA) include Fengxia Xue (Department of Obstetrics and Gynecology of Tianjin Medical University General Hospital), Min Xue (Department of Obstetrics and Gynecology of The Third Xiangya Hospital of Central South University), Yuanguang Meng (Department of Obstetrics and Gynecology of Chinese PLA General Hospital), Zhiqing Liang (Department of Obstetrics and Gynecology of The First Hospital Affiliated to AMU [Southwest Hospital]), Yan Ding (Department of Obstetrics and Gynecology, The First Affiliated Hospital of Xinjiang Medical University), Guonan Zhang (Department of Obstetrics and Gynecology of Sichuan Cancer Hospital), Min Hao (Department of Obstetrics and Gynecology of Second Hospital of ShanXi Medical University), Wenjun Cheng (Department of Obstetrics and Gynecology of Jiangsu Province Hospital), Genhai Zhu (Department of Obstetrics and Gynecology of Hainan General Hospital), Yingfang Zhou (Department of Obstetrics and Gynecology of Peking University First Hospital), Meisong Lu (Department of Obstetrics and Gynecology of The First Affiliated Hospital of Harbin Medical University), Qing Yang (Department of Obstetrics and Gynecology in Shengjing Hospital of China Medical University), Xianghua Huang (Department of Obstetrics and Gynecology in The Second Hospital of Hebei Medical University), Wentong Liang (Department of Obstetrics and Gynecology of Guizhou Provincial People’s Hospital), Yuan Lin (Department of Obstetrics and Gynecology in Fujian Provincial People's Hospital), Manhua Cui (Department of Obstetrics and Gynecology of The Second Hospital of Jilin University), Ruifang An (Department of Obstetrics and Gynecology of First Affiliated Hospital of Xi`an Jiaotong University), Weidong Zhao (Department of Obstetrics and Gynecology, Anhui Provincial Hospital), Mei Ji (Department of Obstetrics and Gynecology of The First Affiliated Hospital of Zhengzhou University), Shuzhong Yao (Department of Obstetrics and Gynecology of The First Affiliated Hospital Sun Yat-sen University), Jiandong Song (Department of Obstetrics and Gynecology of The Affiliated Hospital of Inner Mongolia Medical University), Yongxiu Yang (Department of Obstetrics and Gynecology of The First Hospital of Lanzhou University), Chunfang Ha (Department of Obstetrics and Gynecology of General Hospital of Ningxia Medical University), Jiangqing Zhang (Department of Obstetrics and Gynecology of Qinghai Red Cross Hospital), Ga Zhuo (Department of Obstetrics and Gynecology of Tibet Autonomous Region People`s Hospital), Yun Feng (Department of Obstetrics and Gynecology of The First People`s Hospital of Yunnan Province), Liqun Wang (Department of Obstetrics and Gynecology of Jiangxi Maternal and Child Health Hospital), Keqin Hua (Department of Obstetrics and Gynecology of Obstetrics & Gynecology Hospital of Fudan University), Jun Lin (Department of Obstetrics and Gynecology of Women`s Hospital School of Medicine Zhejiang University), Renfeng Zhao (Department of Obstetrics and Gynecology of The People`s Hospital of Guangxi Zhuang Autonomous Region), and Limin Feng (Department of Obstetrics and Gynecology of Beijing Tiantan Hospital). We also thank the efforts from experts including Yuhua Xie, Peng Yu, Yanfang Sun, Jiong Zhou, Guojie Zhang, and Yang Han from the Peking Union Medical College Hospital (PUMCH).
Footnotes
The authors report no conflict of interest.
This consensus statement was funded by the Chinese Academy of Medical Sciences (CAMS) Initiative for Innovative Medicine (CAMS-I2 M; 2017-I2 M-1-002).
Contributor Information
Experts from the Chinese Obstetricians and Gynecologists Association:
Fengxia Xue, Min Xue, Yuanguang Meng, Zhiqing Liang, Yan Ding, Guonan Zhang, Min Hao, Wenjun Cheng, Genhai Zhu, Yingfang Zhou, Meisong Lu, Qing Yang, Xianghua Huang, Wentong Liang, Yuan Lin, Manhua Cui, Ruifang An, Weidong Zhao, Mei Ji, Shuzhong Yao, Jiandong Song, Yongxiu Yang, Chunfang Ha, Jiangqing Zhang, Ga Zhuo, Yun Feng, Liqun Wang, Keqin Hua, Jun Lin, Renfeng Zhao, and Limin Feng
References
- 1.World Health Organization Coronavirus disease 2019 (COVID-19) situation report – 82. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200411-sitrep-82-covid-19.pdf?sfvrsn=74a5d15_2 Available at: Accessed April 11, 2020.
- 2.Peking Union Medical College Hospital . 2020. Novel coronavirus prevention and control system and standard operating procedures of Peking Union Medical College Hospital. [Google Scholar]
- 3.World Health Organization Novel coronavirus (2019-nCoV) Situation Report - 1. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4 Available at: Accessed January 21, 2020.
- 4.National Health Commission and the State Administration of Traditional Medicine of China Notice regarding the issuance of a new coronavirus pneumonia diagnosis and treatment plan (for trial version 6) http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.shtml?from=timeline Accessed February 19, 2020.
- 5.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peking Union Medical College Hospital . 2020. Compilation of hospital infection management and disease prevention and control work system of Peking Union Medical College Hospital. [Google Scholar]
- 8.National Health Commision of the People’s Republic of China Guidelines for the use of common medical protective products in the prevention and control of novel coronavirus pneumonia (trial) http://www.nhc.gov.cn/yzygj/s7659/202001/e71c5de925a64eafbe1ce790debab5c6.shtml Available at: Accessed January 26, 2020.
- 9.National Health Commission of the People’s Republic of China General principles for disinfection of epidemic sources. http://www.nhc.gov.cn/wjw/s9488/201507/d69be0f22bf24f2880d26974ec0111a7.shtml Available at: Accessed July 31, 2015.
- 10.Weber LeBrun E.E., Moawad N.S., Rosenberg E.I., et al. Coronavirus disease 2019 pandemic: staged management of surgical services for gynecology and obstetrics. Am J Obstet Gynecol. 2020;223:85–90. doi: 10.1016/j.ajog.2020.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chinese College of Emergency Physicians Expert consensus on emergency blood transfusion in special circumstances. Chin J Crit Care Med. 2013;33:481–483. [Google Scholar]