Abstract
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality in type 2 diabetes (T2D) patients. Recent cardiovascular outcome trials demonstrated clear cardiovascular benefits of novel classes of glucose-lowering agents. We performed retrospective electronic health record review at two major healthcare systems in the USA to determine the relative frequencies of outpatient encounters (hence prescribing opportunities) that a patient with T2D and CVD had with a cardiologist vs. an endocrinologist over one-year period. Of 109 747 T2D patients, 42.6% had established CVD. The ratio of cardiology-to-endocrinology outpatient encounters was 2.0:1 for all T2D patients, and 4.1:1 for those with T2D and CVD. Because each outpatient encounter provides an opportunity to discuss glucose-lowering medications with cardiovascular benefits, the much greater frequency of cardiology encounters highlights the emerging potential for cardiovascular specialists to influence or even implement evidence-based glucose-lowering therapies, thereby improving cardiovascular outcomes in their T2D patients.
Keywords: cardiologist, cardiovascular disease, endocrinologist, type 2 diabetes
Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality among patients with type 2 diabetes (T2D). Recent cardiovascular outcome trials investigating two novel classes of glucose-lowering agents, the SGLT-2 inhibitors (SGLT-2i) and the GLP-1 receptor agonists (GLP-1RA), have demonstrated compelling cardiovascular benefits. Both classes have been associated with reductions in major adverse cardiovascular events in patients with T2D and established CVD, and SGLT-2i also decreases the risk of heart failure hospitalizations [1–7]. As a result, treatment guidelines from the American Diabetes Association and American College of Cardiology now recommend that SGLT-2i and GLP-1RA be used preferentially in T2D patients with coexisting CVD [8,9]. Nevertheless, the utilization of these diabetes medications in this patient population has, to date, been limited in the USA [10].
One approach to better understand the reason for the slow incorporation of the guidelines recommendations is to look at the prescribing pattern of these glucose-lowering medications in the USA. Currently, endocrinologists (including diabetologists) prescribe them more frequently than cardiologists and primary care providers (PCPs) [11]. However, the number of cardiologists and PCPs far outweighs the number of endocrinologists nationwide [12], raising the question whether greater involvement by these specialties is needed. In fact, there have been calls for cardiologists to take a more active role in using SGLT-2i and GLP-1RA for cardiovascular risk reduction given their frequent encounters with T2D patients [9,13]. In this study, we endeavored to compare prescribing opportunities for glucose-lowering medications with cardiovascular benefits, by assessing the likelihood that a patient with T2D and CVD had outpatient encounters with a cardiologist versus an endocrinologist over a recent one-year period in two large academic healthcare systems in the USA.
Methods
We conducted a retrospective review of electronic health records (EHRs) of patients with T2D who had outpatient encounters within two large USA healthcare systems, one based in New England and one based in the Midwest, during calendar year 2017. We utilized ICD-10 diagnostic codes to select for adult patients (age ≥ 18 years) with T2D. Data extracted included age, sex, race, CVD diagnoses [coronary artery disease (CAD), heart failure (HF), cerebrovascular disease (CeVD), peripheral vascular disease (PVD)] as classified by ICD-10 codes, and the number of cardiology, endocrinology, and primary care encounters. We included the following outpatient encounter types: initial consult, follow-up, appointment, office visit, evaluation, and specifically excluded all procedural visits. Outside the scope of our study were the current glucose-lowering regimens being used by the patients, any prevalent contraindications to specific medications, and the quality of their glycemic control. Because the extracted data did not contain any patient identifying information, the study was exempted from full review by the corresponding institutional review boards. Basic statistical analyses were performed using Microsoft Excel.
Results
A total of 109 747 patients with T2D (mean age 66.6 ± 14.0 years, 51% female, 68% Caucasian) had at least one outpatient encounter. CVD was present in 42.6% of the patients. The most prevalent CVD diagnosis was CAD in 29.5%, followed by heart failure in 15.1%, CeVD in 12.4%, and PVD in 10.2%. Overall, the ratio of cardiology-to-endocrinology outpatient encounters was 2.0:1 (73 909 vs. 37 280 encounters) for all T2D patients (Fig. 1a). For patients with T2D and CVD, the ratio of cardiology-to-endocrinology outpatient encounters was 4.1:1 (63 655 vs. 15 648 encounters). This was comparable to the ratio of PCP-to-endocrinology outpatient encounters (4.0:1, 62 889 vs. 15 648 encounters) (Fig. 1b). Of the four CVD diagnoses, patients with heart failure had the highest cardiology-to-endocrinology encounter ratio at 6.8:1 (34 838 vs. 5100 encounters) (Fig. 2).
Fig. 1.
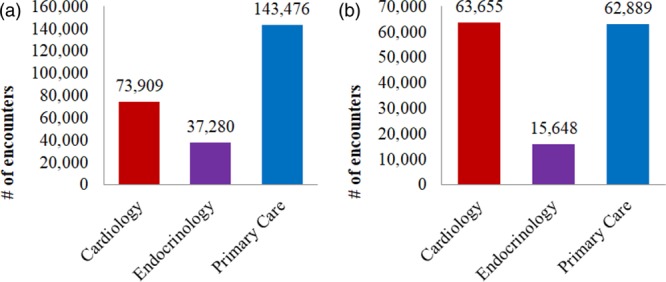
Number of outpatient encounters by specialty in all T2D patients (a) and in patients with T2D and CVD (b). CVD, cardiovascular disease; T2D, type 2 diabetes.
Fig. 2.
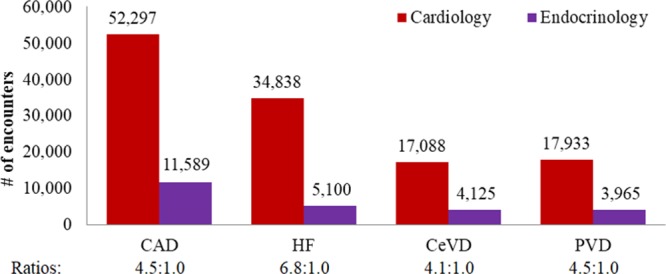
Number of outpatient encounters by specialty and cardiovascular diagnoses in patients with T2D and CVD. CVD, cardiovascular disease; T2D, type 2 diabetes CAD, coronary artery disease, HF, heart failure, CeVD, cerebrovascular disease, PVD, peripheral vascular disease.
Discussion
Over the course of a single year at two large and geographically distinct USA healthcare systems, a T2D patient was twice as likely to have an outpatient encounter with a cardiologist than an endocrinologist. With coexisting CVD, the likelihood doubled to more than four-fold and was highest in patients with heart failure (more thansix-fold). In fact, a patient with T2D and CVD was as likely to have an outpatient encounter with a cardiologist as with a PCP. Of note, each outpatient encounter provides a potential opportunity for initiation of newer evidence-based glucose-lowering medications demonstrated to provide cardiovascular benefits. However, there is a discrepancy, whereby the specialty most familiar with these novel drugs is not the one with the more frequent contact with patients most apt to benefit. One likely explanation for this imbalance is the simple fact that there are more cardiologists than endocrinologists nationwide, and that diabetes, particularly recent-onset disease, is more apt to be handled in the primary care setting. Moreover, once a patient develops CVD, it is not uncommon for frequent office visits to occur with the cardiovascular specialist until the condition is stabilized. Regardless, these data present a current ‘snapshot’ into the relative ‘patient touches’ between these specialties, encounters which may be broadly considered opportunities to at least discuss the use of – if not prescribe – newer and now evidence-based glucose-lowering medications in T2D patients with established CVD. They therefore provide insights into potential opportunities for cardiologists to improve the quality of care provided to their patients with T2D.
Over the past 4 years, seven large cardiovascular outcome trials of two novel classes of glucose-lowering medications (SGLT-2i and GLP-1RA) have demonstrated improved cardiovascular outcomes in high-risk T2D patients (including, in some circumstances, reductions in cardiovascular mortality and lower rates heart failure hospitalizations) [1–7]. Such findings have dramatically changed prevailing paradigms of T2D management, with major professional organizations now advising their preferential use after metformin in those with T2D and CVD [8,9]. Due to clinical inertia, however, uptake of these therapies by primary care providers will likely be very gradual, while endocrinologists have generally been more enthusiastic. Based on the data presented in this report, cardiovascular specialists encouraging the use of these medications (or, if comfortable, actually prescribing these medications) would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them.
Our study had several limitations. By relying on ICD-10 chart diagnostic codes for data collection, our study was susceptible to potential EHR coding inaccuracies. Also, the scope of the study is limited to large academic practices within two regions in the USA. Hence, the findings may not be generalizable to all settings within or outside the USA, where subspecialist availability may vary. However, given the higher prevalence of cardiologists compared with endocrinologists nationwide [12], these observations are at least likely true for the majority of healthcare systems and practice settings in the USA.
In conclusion, American patients with T2D and CVD are at least four times more likely to see a cardiologist than an endocrinologist in the outpatient setting. Greater involvement by cardiologists in optimizing glucose-lowering regimens for cardiovascular protection in patients with established CVD will likely improve their clinical outcomes. One novel way to do this would be to establish a new subspecialty of cardiometabolic medicine as proposed by Eckel et al. [14], which would provide training in preventive cardiology and metabolic endocrinology and serve a medical home for patients with metabolic syndrome, diabetes, and CVD. However, until such an entity can be established, educational efforts directed at cardiologists regarding the emerging recognition of the cardiovascular impact of these novel medications may serve to further augment adherence to the latest national treatment guidelines and improve patient outcomes.
Acknowledgements
Preliminary version of the data, which included data only from Yale, was presented at the ENDO poster session in March 2019.
Conflicts of interest
M.E.N. declares modest speaking honoraria from Abbott. M.K. has served on Clinical Trial Steering/Executive/Publications committees for and/or received honoraria/served on the advisory board as a consultant to AstraZeneca, Boehringer-Ingelheim, Sanofi, Amgen, Novo Nordisk, Merck, Eisai, Janssen, Bayer, Applied Therapeutics, GlaxoSmithKline, Glytec, Intarcia, Novartis, Amarin. He has received research grants from AstraZeneca and Boehringer-Ingelheim, and other research support from AstraZeneca. S.E.I. has served on Clinical Trial Steering/Executive/Publications committees for Boehringer-Ingelheim, AstraZeneca, Novo Nordisk, and Sanofi/Lexicon. He has been a consultant to Zafgen, vTv Therapeutics, Alere, and Merck, and has received lecture honoraria from Merck and Boehringer-Ingelheim. There are no conflicts of interest for the remaining authors.
References
- 1.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. ; EMPA-REG OUTCOME Investigators. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–2128 [DOI] [PubMed] [Google Scholar]
- 2.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. ; SUSTAIN-6 Investigators. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016; 375:1834–1844 [DOI] [PubMed] [Google Scholar]
- 3.Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. ; LEADER Steering Committee; LEADER Trial Investigators. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016; 375:311–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. ; CANVAS Program Collaborative Group. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–657 [DOI] [PubMed] [Google Scholar]
- 5.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. ; DECLARE–TIMI 58 Investigators. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–357 [DOI] [PubMed] [Google Scholar]
- 6.Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019; 394 [DOI] [PubMed] [Google Scholar]
- 7.Hernandez AF, Green JB, Janmohamed S, D’Agostino RB, Sr, Granger CB, Jones NP, et al. ; Harmony Outcomes committees and investigators. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (harmony outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018; 392:1519–1529 [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019; 42Suppl. 1S90–S102 [DOI] [PubMed] [Google Scholar]
- 9.Das SR, Everett BM, Birtcher KK, Brown JM, Cefalu WT, Januzzi JL, Jr, et al. 2018 ACC expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a report of the american college of cardiology task force on expert consensus decision pathways. J Am Coll Cardiol. 2018; 72:3200–3223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnold SV, Inzucchi SE, Tang F, McGuire DK, Mehta SN, Maddox TM, et al. Real-world use and modeled impact of glucose-lowering therapies evaluated in recent cardiovascular outcomes trials: an NCDR® research to practice project. Eur J Prev Cardiol. 2017; 24:1637–1645 [DOI] [PubMed] [Google Scholar]
- 11.Vaduganathan M, Sathiyakumar V, Singh A, McCarthy CP, Qamar A, Januzzi JL, Jr, et al. Prescriber patterns of SGLT2I after expansions of U.S. Food and drug administration labeling. J Am Coll Cardiol. 2018; 72:3370–3372 [DOI] [PubMed] [Google Scholar]
- 12.Association of American Medical Colleges. active physicians in the largest specialties. 2017. https://www.aamc.org/data/workforce/reports/492556/1-1-chart.html. [Accessed 13 July 2019]
- 13.Nassif ME, Kosiborod M. Are we ready to bell the cat? A call for cardiologists to embrace glucose-lowering therapies proven to improve cardiovascular outcomes. Circulation. 2018; 138:4–6 [DOI] [PubMed] [Google Scholar]
- 14.Eckel RH, Blaha MJ. Cardiometabolic medicine: a call for a new subspeciality training track in internal medicine. Am J Med. 2019; 132:788–790 [DOI] [PubMed] [Google Scholar]


