Abstract
OBJECTIVE | Type 2 diabetes represents a major health disparity for many American Indian/Alaska Native (AIAN) communities, in which prevalence rates are more than double that of the general U.S. population. Diabetes is a major indicator for other comorbidities, including the leading cause of death for AIANs (i.e., cardiovascular disease). This study investigated associations between protective factors (social support and cultural factors) and self-reported empowerment to manage illness.
DESIGN AND METHODS | Participants were drawn from a random sample of tribal clinic records. Data included results from computer-assisted personal interviews with 192 American Indian adults with a diagnosis of type 2 diabetes living on or near a reservation. Community Research Councils, developed at each of the five partnering Anishinaabe reservations, oversaw protocols and procedures in this community-based participatory research collaboration.
RESULTS | Multiple ordinary least squares regression models determined that general social support and diabetes-specific social support are positively related to diabetes empowerment. These associations persisted when both social support measures were added to the model, indicating independent effects of different types of social support. Cultural identity and cultural practices were positively related to diabetes empowerment in bivariate analyses; however, both measures dropped from statistical significance after accounting for all other covariates. An interaction term revealed a moderation effect through which cultural identity amplified the positive relationship between social support and diabetes empowerment.
CONCLUSION | Results moderately support policy and risk-reduction efforts aiming at expanding social support networks into multiple domains and reinforcing cultural identity and cultural practices.
Type 2 diabetes represents a modern epidemic and major health inequity in many American Indian/Alaskan Native (AIAN) communities, where rates of diabetes overall are more than double that seen in the general U.S. population (1). Furthermore, diabetes is a major contributor to cardiovascular disease, the leading cause of death for AIAN people (2) and other comorbidities affecting these communities (3–5). Thus, determining protective factors that improve quality of life for AIAN people living with diabetes is an important empirical initiative to improve individual and community health and well-being.
Social Support and Health
For AIAN people and indigenous populations throughout the world, family and community support are imperative in improving health and decreasing barriers to healthy behaviors, especially with regard to diabetes management. Among indigenous adults in Canada, social support (i.e., positive interaction, emotional support, and tangible support) was associated with thriving health, and emotional support specifically increased the odds of thriving health by almost twofold (6). Furthermore, important diabetes-specific health outcomes have been shown to result from social support. Epple et al. (7) found that AI individuals reporting family support in healthy eating had better outcomes for triglyceride, cholesterol, and A1C levels. Most important to all metabolic outcomes was having another person cook most of the meals. The authors deduced that having support in meal preparation creates broader family ownership of the disease such that the burdens of diabetes care are shared. In addition, Dill et al. (8) found that an increase in positive family support improved the outcomes of an educational curriculum focused on weight loss for AIAN people with diabetes. Encouragement and shared ownership of disease management leads to better health outcomes among AIAN adults living with diabetes.
Among AIAN people, disconnection and lack of support from family and community are crucial barriers to disease management. In one intervention study, family criticism or family negativity toward diabetes-related behaviors was associated with higher baseline weight and less weight loss after the intervention (8). Taylor et al. (9) identified barriers to engaging in diabetes-related health behaviors, including conflicting family and community responsibilities. If family roles and position in the community were disrupted because of diabetes care behaviors, family and community responsibilities often took precedence.
Although disconnection from family and community and competing social responsibilities may deter positive health outcomes, it is often family support that resolves the dilemma that the individual might have in balancing family needs with individual needs (7). Thus, empirical evidence suggests that family and community play important roles in supporting improved health behaviors and better health outcomes for indigenous people living with diabetes.
Cultural Factors and Health
There are two major gaps in research related to understanding how indigenous cultures are associated with health: 1) investigations into multiple dimensions of culture and 2) efforts to broaden the study of health outcomes that might relate to cultural domains. Currently, much of the literature supporting ideas of “culture as treatment” focuses on substance abuse and mental health (10,11). Yet, there is evidence of broader protective effects that cultural identity and cultural engagement may provide to AIAN communities by improving wellness and healthy behaviors (12,13), encouraging positive strategies for coping with stress (14), and building youth resilience (15,16).
Indigenous cultural factors are associated with diabetes-related behaviors and outcomes as well, although these relationships are empirically underexplored. Greater rates of indigenous language knowledge were found to significantly predict lower prevalence rates of diabetes among 31 First Nations communities in Canada (17). In a study of participants in an AIAN diabetes project, Dill et al. (8) found a significant and positive relationship between indigenous spirituality and weight loss in a sample of AIAN respondents living with diabetes. Qualitative research has also reported the importance of spirituality, traditional practices, and identity in coping with stress while living with diabetes (18) and with diabetes care management (19) among AIAN and First Nations people. These studies have revealed important relationships between indigenous cultural factors and diabetes-related health, thus warranting additional research.
Interrelatedness of Social Support and Cultural Factors
There is a multifaceted relationship between social support and indigenous cultures. Indigenous people often consider social support and culture as interrelated (and possibly interdependent) concepts. As one author noted, “. . .[F]amily and traditions such as valuing heritage and respecting kinship helped the participants persevere in the world with diabetes . . . [T]ensions within tribal traditions included loss of family support and not being well enough to participate in cultural practices. . . .” (20). Furthermore, exploring why and how diabetes affects Aborigines in Australia, Thompson and Gifford (21) reported that being connected to family and community actually protects people from the disease; it is only when people are disconnected from their families that they are “open to illness . . . from the outside world.” In this conceptualization of health, connection to family and community instills standards toward living a traditional lifestyle, including traditional diet and traditional labor activities. In other studies, protective family and peer influences have been positively and significantly related to cultural identity (22), and social support from family and friends has been related to enculturation (16). Family, community, and culture are often spoken about simultaneously in indigenous contexts; thus, disentangling their independent or interactive effects may be difficult.
On the other hand, there are aspects of indigenous cultures that are unrelated to social support, which leads us to believe that culture can amplify the impact of social support on health and wellness. Wexler (23) offers a few cultural mechanisms that may lead to positive health outcomes. Culture provides a sense of pride, a moral compass, and an outlook on life that may encourage a higher standard for self-care when managing chronic disease. Coping with historical trauma, the feelings of loss that are often heightened when one is more enculturated (24), is thought to lead to a “fierce willpower” (23) that could provide determination to deal with other hardships, including chronic illness. Cultural identity may mean one participates in more traditional cultural activities, which has been shown to be associated with better mental health outcomes (25). Furthermore, researchers who study resilience among AI youth have associated cultural identity with better self-esteem and subjective well-being (15,16), which might indicate better behaviors for the sake of healthy living. Thus, there is impetus to identify the interactive associations among culture, social support, and health.
Diabetes Empowerment and Health
Diabetes empowerment is another mechanism likely to influence health behaviors and therefore health. Diabetes empowerment is an important construct for improving the health of individuals living with diabetes given evidence that empowerment, or self-efficacy to manage diabetes-related health, positively affects self-management behaviors such as monitoring blood glucose, following a diabetes meal plan, performing foot checks (26), taking medications, and gaining diabetes knowledge (27,28). Researchers posit that more important than gaining knowledge about one’s chronic condition is having the ability to set goals, organize resources, and implement problem-solving strategies, as well as knowing the actions that are necessary for disease self-management (29). Intervention strategies geared toward increasing empowerment focus on self-management experiences, problem-solving, and behavioral goal-setting (30,31), which are important predeterminants of behavior change.
This study is based on the premise that social support and indigenous cultural factors lead to better health outcomes for AIAN people while recognizing that the relationship among social support, cultural factors, and health remains unclear. This study specifically focuses on Anishinaabe people. (“Chippewa” has been the legal term used by the federal government in major legal and treaty negotiations and is included in the names of multiple tribes [32,33], but many members of this group prefer the terms “Anishinaabe” or “Ojibwe.”)
Social support is a key indicator of health and well-being when it comes to chronic disease, including type 2 diabetes (34,35), and among AIAN communities (7,8). In addition, “culture as treatment” (10,36) is a concept innately understood in indigenous communities and is emerging as the foundation for indigenous health research and practice. With this emergence, it is important to explore multiple domains of culture as a multidimensional concept. Investigating various components of cultural engagement, values, and beliefs in research can better support community-based efforts to promote health. Furthermore, social support and social integration are intertwined in cultural practices and cultural socialization (16,22).
With regard to the evidence presented, our analyses are based on a sociocultural conceptual model (Figure 1). We investigated associations among individual and interactive effects of cultural factors and social support for diabetes-related empowerment among Anishinaabe people living with type 2 diabetes by testing three hypotheses:
Hypothesis 1 (H1): Social support (diabetes specific and general) will be positively associated with diabetes empowerment.
Hypothesis 2 (H2): Indigenous cultural factors (identity and practice) will be positively associated with diabetes empowerment.
Hypothesis 3 (H3): Cultural factors will moderate the relationship between social support and diabetes empowerment.
FIGURE 1.
The sociocultural conceptual model on which this research was based.
Research Design and Methods
The Maawaji’ idi-oog Mino-ayaawin (Gathering for Health) study is a community-based participatory research collaboration between researchers and five Anishinaabe communities in the Upper Midwest region of the United States. Community research councils (CRCs) composed of tribal members and health providers at each site are active research partners and participate in all aspects of study planning, protocol development, and implementation to ensure cultural and local acceptability of study procedures. For example, CRC members generated ideas for and reviewed and adapted all measures included in the survey, made hiring decisions for community-based interviewers, presented project updates to tribal governments alongside university project members, and continue to strategize with the analysis team regarding important manuscripts or research questions to explore with the data. CRC members and interviewers also attend and present data from the project at academic conferences. They are local experts on the cultural and community contextual factors important for interpretation of results and leaders for our team overall. The project is supported by resolutions from each tribal government, and all study procedures were reviewed and approved by the University of Minnesota and the National Indian Health Service institutional review boards.
Sample
Staff at the partnering tribal clinics generated simple random probability samples from medical records to form a recruitment list for the study. Patients who were ≥18 years of age, had a diagnosis of type 2 diabetes, lived on or near one of the five partnering reservations (i.e., within a 1-hour drive), and self-identified as AIAN were eligible for inclusion. Selected patients were mailed a study invitation letter with mail and call-in refusal options.
A total of 194 participants enrolled in the study, representing a baseline response rate of 67%. Data for this article include responses from the 192 participants for which we have baseline computer-assisted personal interviews (CAPIs) completed between November 2013 and November 2015. Participants received $50 and a traditional gift of wild rice for taking the survey.
Measures
Diabetes Empowerment
The dependent variable diabetes empowerment was measured using an adapted version of the Diabetes Empowerment Scale–Short Form (DES-SF) (37). The DES-SF is an eight-item self-reported measure to assess the self-efficacy of people with diabetes in managing the psychosocial aspects of diabetes, dissatisfaction and readiness to change, and ability to set and achieve goals related to diabetes. Item scores ranged from 1 (strongly agree) to 4 (strongly disagree). Items were inversely scored and summed to create a final diabetes empowerment variable with higher values indicating greater diabetes empowerment.
Social Support
The independent variables included two social support measures: diabetes support and general social support.
Diabetes support was measured using an adapted version of the Diabetes Care Profile (DCP)–Support Received Scale (38,39). Respondents were asked about support they receive from their families and friends as it relates to handling diabetes-related behaviors and moods. Item scores ranged from 1 (strongly agree) to 4 (strongly disagree). The final diabetes support variable was inversely scored, and a sum score was created, with a possible range of 0–15, with higher values indicating more support.
General social support was measured using the “received support” components of the adapted 2-Way Social Support Scale, designed to measure instrumental and emotional support (40). Respondents were asked to rate whether they had someone to provide them emotional and instrumental support. Response options included “not at all true,” “sometimes true,” “often true,” and “always true.” General support was a mean score of all items, with a possible range of 0–3, with higher scores indicating higher levels of received support.
Anishinaabe Culture
Independent variables also included two cultural measures—Anishinaabe cultural identity and Anishinaabe cultural practice.
Anishinaabe cultural identity was measured using an adapted version of the In-Group Identification Measure (41). We asked respondents to rate the degree to which they agree or disagree with questions regarding their bond with native people, commitment to native people, and feelings toward being native. The mean score of each item formed the final variable, with possible ranges of 0–3, with higher scores indicating greater cultural identity.
The second cultural measure signified whether the respondents felt they lived by Anishinaabe ways. We chose this measure to indicate the level of practicing Anishinaabe cultural ways. Anishinaabe cultural practice was measured using one self-reported question: How much do you live by or follow Anishinaabe ways? Response options included “none,” “not much,” “some,” and “a lot,” which were coded as 0–3, respectively.
Demographics
Four additional measures were included as control variables. Sex was coded as either 0 = male or 1 = female. Age was calculated by self-reported age in years at the respondent’s last birthday. Income was divided by the number of people in the household and then divided by 1,000 to assess per-capita income. Currently living on a reservation was measured with a self-reported yes-or-no question (on reservation = 1, off = 0).
Statistical Analysis
We used SPSS, version 24, for data analysis (42). Multiple ordinary least squares (OLS) regression models were used to examine the associations among social support, cultural factors, and diabetes empowerment, controlling for sex, age, income, and currently living on the reservation. Descriptive and bivariate analyses were generated to examine variable distributions and focal relationships among key study variables. OLS regression models (including mean-centering independent variables for calculating interaction terms) were used for multivariate modeling.
Results
Descriptive information and bivariate correlations for all study variables are presented in Table 1. More than half of the study population (55.7%) was female. The average age of respondents was 46 years, and the majority (almost 79%) reported living on a reservation. The average per-capita income was <$10,000.
TABLE 1.
Descriptive Statistics and Bivariate Correlations for All Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sex (female = 1) | 1 | ||||||||
| 2 | Age | 0.03 | 1 | |||||||
| 3 | Income | 0.04 | 0.24** | 1 | ||||||
| 4 | Currently live on reservation | 0.02 | −0.13 | −0.22** | 1 | |||||
| 5 | Diabetes care support | −0.16* | 0.01 | 0.16* | 0.02 | 1 | ||||
| 6 | Social support | 0.08 | 0.00 | 0.19** | −0.03 | 0.32** | 1 | |||
| 7 | Cultural identity | 0.07 | 0.16* | 0.13 | 0.02 | 0.28** | 0.30** | 1 | ||
| 8 | Follows Anishinaabe ways | 0.03 | −0.02 | 0.03 | 0.03 | 0.24** | 0.19** | 0.42** | 1 | |
| 9 | Diabetes empowerment | 0.01 | 0.02 | 0.18* | 0.05 | 0.33** | 0.37** | 0.30** | 0.23** | 1 |
| Mean or % (SD) | 55.7% | 46.3 (12.2) years | $9,767 per capita | 78.7% | 8.67 (3.1) score | 2.24 (0.7) score | 2.4 (0.5) score | 1.6 (0.9) score | 16.02 (2.9) score | |
Boldface indicates statistical significance (two-tailed tests).
P <0.05.
P< 0.01.
Turning first to demographic control variables, being female was negatively associated with diabetes support, and age was positively associated with Anishinaabe cultural identity. Income was positively related to diabetes care support, general social support, Anishinaabe cultural identity, and diabetes empowerment. Both measures of social support (general social support and diabetes support) were significantly and positively correlated with diabetes empowerment, thus supporting H1. The two cultural measures (cultural identity and cultural practices) were significantly and positively associated with each other, and both were positively associated with receiving social support and diabetes empowerment, thus supporting H2.
Results of OLS regression analyses are shown in Table 2. Model 1 displays results when diabetes empowerment is regressed on four demographic control variables. Holding sex, age, and reservation residency constant, income was positively associated with diabetes empowerment (b = 0.22, P< 0.01).
TABLE 2.
Multiple Regression for All Study Variables and Interaction Term
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | B | B | B | B | B | |||||||
| Variable | (b/SE) | β | (b/SE) | β | (b/SE) | β | (b/SE) | β | (b/SE) | β | (b/SE) | β |
| Sex (Female = 1) | 0.14 | 0.03 | 0.39 | 0.07 | 0.19 | 0.03 | 0.13 | 0.02 | 0.11 | 0.02 | 0.14 | 0.02 |
| (0.42) | (0.41) | (0.40) | (0.40) | (0.40) | (0.39) | |||||||
| Age | −0.01 | −0.02 | 0.00 | −0.01 | 0.00 | 0.01 | 0.00 | −0.02 | 0.00 | −0.01 | 0.00 | 0.00 |
| (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | |||||||
| Income | 0.06 | 0.19 | 0.04*** | 0.14 | 0.03 | 0.10 | 0.03 | 0.10 | 0.03 | 0.10 | 0.03 | 0.10 |
| (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | (0.02) | |||||||
| Currently live on the reservation | 0.62(0.53) | 0.09 | 0.51(0.51) | 0.07 | 0.52(0.49) | 0.08 | 0.47(0.49) | 0.07 | 0.47(0.49) | 0.07 | 0.41(0.48) | 0.06 |
| Diabetes care support | 0.28††(0.07) | 0.30 | 0.20†(0.07) | 0.22 | 0.17***(0.07) | 0.19 | 0.16***(0.07) | 0.18 | 0.14**(0.07) | 0.15 | ||
| Social support | 1.11†† | 0.26 | 0.99*** | 0.23 | 0.97† | 0.23 | 0.92† | 0.22 | ||||
| (0.31) | (0.32) | (0.32) | (0.32) | |||||||||
| Cultural identity | 0.83** | 0.14 | 0.62 | 0.11 | 0.77 | 0.13 | ||||||
| (0.43) | (0.46) | (0.47) | ||||||||||
| Follows Anishinaabe ways | 0.28(0.23) | 0.09 | 0.33(0.23) | 0.11 | ||||||||
| Diabetes care support × identity | 0.23*(0.13) | 0.13 | ||||||||||
| Constant | 15.09 | 12.68 | 10.83 | 9.75 | 9.85 | 9.63 | ||||||
| (1.01) | (1.13) | (1.21) | (1.32) | (1.32) | (1.32) | |||||||
Boldface indicates statistical significance (two-tailed tests).
P <0.10.
P <0.065.
P <0.05.
P <0.01.
P <0.001.
Next, we added two social support variables to the model. Model 2 illustrates a positive relationship between diabetes support and diabetes empowerment (b = 0.27, P <0.001) after controlling for demographic variables. When including both social support variables in Model 3, both diabetes support (b = 0.21, P< 0.01) and general social support (b = 1.07, P<0.001) were positively related to diabetes empowerment. The statistical significance of these social support variables persisted in all remaining models even when cultural variables were added (Models 4 and 5).
Models 4 and 5 show relationships between cultural factors and diabetes empowerment after accounting for social support factors and demographic controls. As illustrated in Model 4, cultural identity was significantly and positively related to diabetes empowerment. When both cultural variables are added to the model (Model 5), neither was significantly related to diabetes empowerment.
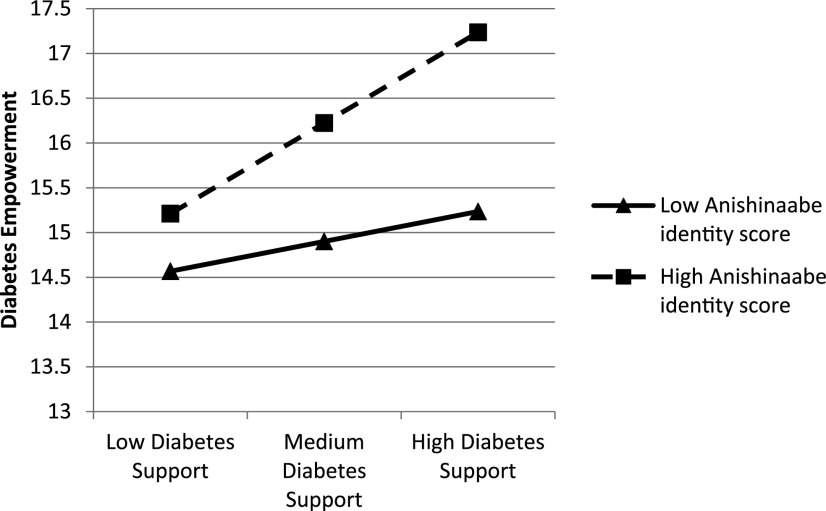
To test for the potential modifying effects of culture and social support factors for diabetes empowerment, we created interaction terms between our two measures of culture and two measures of social support (four interaction terms total). Only one of the multiplicative interactions (diabetes support × identity) was significant (P <0.10 level) and is shown in Model 6. As can be seen in a visual display of the interaction effect in Figure 2, increasing levels of diabetes support are related to more diabetes empowerment for all participants (those with low or high identity scores); however, this relationship is much more pronounced for those who report a stronger Anishinaabe cultural identity. For respondents with high Anishinaabe cultural identity scores, levels of diabetes empowerment increase at a much higher rate in response to increasing diabetes support in comparison with respondents with low Anishinaabe cultural identity scores. The highest diabetes empowerment was seen in respondents with the highest levels of Anishinaabe cultural identity and the highest levels of diabetes support. In short, the interaction illustrates that a strong cultural identity strengthens the positive relationship between diabetes support and diabetes empowerment.
FIGURE 2.
Levels of diabetes empowerment by Anishinaabe cultural identity and diabetes care support.
Discussion
The purpose of this study was to examine the relationships among social support, culture, and diabetes empowerment in Anishinaabe adults living with type 2 diabetes. We hypothesized that social support would be positively related to diabetes empowerment (H1), that cultural factors would be positively related to diabetes empowerment (H2), and that cultural factors would moderate the relationship between social support and empowerment (H3). Our results highlight the importance of social support, disease-specific support, and cultural factors for promoting diabetes empowerment among AIAN patients with type 2 diabetes.
We documented bivariate associations between social support and diabetes empowerment that persisted in multivariate models after controlling for relevant demographic variables, thus supporting H1. This is consistent with prior literature showing empowerment, or self-efficacy to manage diabetes-related health, may also mediate the effect of family and friend support on diabetes-related behaviors such as following a meal plan and checking feet (26). A particularly important and novel finding was that general social support and disease-specific support had independent effects for diabetes empowerment in our multivariate models. This suggests that efforts to amplify social support in multiple domains may be beneficial for patients with diabetes and builds on the findings of prior studies that emphasize links between social support and health among AIAN and First Nations people living with type 2 diabetes (43,44).
In bivariate results, cultural identity and cultural practices were each positively related to general social support, disease-specific social support, and diabetes empowerment. These results align with prior research documenting a positive relationship between AIAN cultural identity and social support (22) and between AIAN cultural behaviors/practices and well-being (16). Age was also positively associated with cultural identity. This finding is consistent with developmental theories in which cultural identity unfolds over the life course (23,45). At the same time, fostering cultural identity in young people is crucial for building resiliency into adulthood (16,46), and our finding suggests that older participants may have stronger ethnic identities and lessons to share with younger generations.
The bivariate relationship between cultural factors and diabetes empowerment provides support for H2 and offers new evidence of potentially protective effects of culture on diabetes-related outcomes. Further, in multivariate analysis, cultural identity remained significantly related to diabetes empowerment even after accounting for social support and demographic factors (Model 4). That both social support constructs retained statistical significance in this model suggests that cultural identity, social support, and diabetes support offer independent contributions to diabetes empowerment, making each vital to the reduction or delay of diabetes. These independent effects are especially compelling given that prior research has cited social support as a possible mechanism of culturally driven health promotion. For example, others have argued that cultural embeddedness or belonging to a social group (23) provides social support and that social support shapes identity (47). However, our results indicate that culture may improve diabetes empowerment even when accounting for social support (with additional modifying effects, discussed below). Both of the cultural variables dropped from statistical significance, however, when each was added to our final multivariate model, including controls, social support, and a multiplicative interaction term. This result may be because of shared variance among the cultural measures and a relatively small sample size.
Beyond the direct associations discussed above, we found that cultural identity modified the relationship between diabetes support and empowerment, lending partial support to H3. This finding signifies that culture may also strengthen the relationship between social support and well-being; that is, those with a greater degree of positive cultural identity were most likely to benefit from possible impacts of social support on diabetes empowerment.
Limitations
Although this study resulted in novel conclusions regarding the role of social support and indigenous cultural factors on disease-specific empowerment, there are limitations to our approach. The cross-sectional nature of these data prohibits conclusions about causal ordering. In addition, the conceptual framework that theorizes culture as a modifier of social support cannot be clearly determined by these data. One measurement challenge was the assessment of cultural factors. Our two cultural measurements (cultural identity and cultural practices) are correlated and may overlap in terms of predicting variance in multivariate models. Health researchers are committed to investigating the role of cultural factors in indigenous health; however, the way in which we measure culture remains unclear. Not only do constructs of indigenous culture evolve, but also, culture’s dynamic nature is difficult to elucidate in terms of measures. There may exist other mechanisms of culture that better predict social support and diabetes empowerment. In addition, indigenous culture is confounded by cultural-related stress (i.e., discrimination and historical trauma), which negatively affects health outcomes and blurs the relationship between indigenous culture and health (48).
Conclusion
Our study demonstrates that general support and diabetes-specific support are independently related to diabetes empowerment among AI adults. This finding expands our view of social support for diabetes patients by assessing multiple domains of social support. In addition, cultural identity and social support were associated with diabetes empowerment independent of the effects of each other, thus implying independent potential protective aspects of culture and social support for AIAN people.
These results inform our understanding of the complexity of culture and the mechanisms by which culture promotes healthy behaviors and outcomes (49). The results also suggest that cultural identity may strengthen the relationship between diabetes support and diabetes empowerment. Because of the cross-sectional nature of the study, further research to determine causal relationships among social support, cultural factors, and diabetes empowerment would strengthen our findings. These findings are also on par with prior literature (35), thus bolstering the relevance of social support for intervention programming. Finally, this work supports community calls for culturally relevant programming and is therefore applicable to AIAN peoples.
Article Information
Acknowledgments
Community Research Council (CRC) members, interviewers, and clinical staff contributed to the design of the study, the collection of data, and the interpretation of results, and the CRC members reviewed the manuscript. CRC members, interviewers, and clinical staff included the following: Sidnee Kellar, Rose Barber, Robert Miller, Tweed Shuman, Lorraine Smith, Sandy Zeznanski, Patty Subera, Tracy Martin, Geraldine Whiteman, Lisa Perry, Trisha Prentice, Alexis Mason, Charity Prentice-Pemberton, Kathy Dudley, Romona Nelson, Eileen Miller, Geraldine Brun, Murphy Thomas, Mary Sikora-Petersen, Tina Handeland, GayeAnn Allen, Frances Whitfield, Phillip Chapman Sr., Sonya Psuik, Hope Williams, Betty Jo Graveen, Daniel Chapman Jr., Doris Isham, Stan Day, Jane Villebrun, Beverly Steel, Muriel Deegan, Peggy Connor, Michael Connor, Ray E. Villebrun Sr., Pam Hughes, Cindy McDougall, Melanie McMichael, Robert Thompson, and Sandra Kier.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
M.B.G. wrote the manuscript. K.A.H. contributed to writing the manuscript and reviewed/edited the manuscript. M.L.W. researched the data and reviewed/edited the manuscript. M.B.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Centers for Disease Control and Prevention Estimates of diabetes and its burden in the United States. Available from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 2 October 2019
- 2.Heron M. Deaths: leading causes for 2017. National Vital Statistics Report #68. Available from https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf. Accessed 12 May 2019 [PubMed]
- 3.Centers for Disease Control and Prevention National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 4.Goins R, Spencer S, Roubideaux Y, Manson S. Differences in functional disability of rural American Indian and White older adults with comorbid diabetes. Res Aging 2005;27:643–658 [Google Scholar]
- 5.Walls ML, Aronson BD, Soper GV, Johnson-Jennings MD. The prevalence and correlates of mental and emotional health among American Indian adults with type 2 diabetes. Diabetes Educ 2014;40:319–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richmond CAM, Ross NA, Egeland GM. Social support and thriving health: a new approach to understanding the health of indigenous Canadians. Am J Public Health 2007;97:1827–1833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epple C, Wright AL, Joish VN, Bauer M. The role of active family nutritional support in Navajos’ type 2 diabetes metabolic control. Diabetes Care 2003;26:2829–2834 [DOI] [PubMed] [Google Scholar]
- 8.Dill EJ, Manson SM, Jiang L, et al. ; Special Diabetes Program for Indians Diabetes Prevention Demonstration Project . Psychosocial predictors of weight loss among American Indian and Alaska Native participants in a diabetes prevention translational project. J Diabetes Res 2016;2016:1546939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor C, Keim KS, Sparrer A, Van Delinder J, Parker S. Social and cultural barriers to diabetes prevention in Oklahoma American Indian women. Prev Chronic Dis 2004;1:A06. [PMC free article] [PubMed] [Google Scholar]
- 10.Gone JP, Looking PE. American Indian culture as substance abuse treatment: pursuing evidence for a local intervention. J Psychoactive Drugs 2011;43:291–296 [DOI] [PubMed] [Google Scholar]
- 11.Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska natives: incorporating culture in an “indigenist” stress-coping paradigm. Public Health Rep 2002;117(Suppl. 1):S104–S117 [PMC free article] [PubMed] [Google Scholar]
- 12.Hodge FS, Nandy K. Predictors of wellness and American Indians. J Health Care Poor Underserved 2011;22:791–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Priest N, Mackean T, Davis E, Briggs L, Waters E. Aboriginal perspectives of child health and wellbeing in an urban setting: developing a conceptual framework. Health Sociol Rev 2012;21:180–195 [Google Scholar]
- 14.Wolsko C, Lardon C, Mohatt GV, Orr E. Stress, coping, and well-being among the Yup’ik of the Yukon-Kuskokwim Delta: the role of enculturation and acculturation. Int J Circumpolar Health 2007;66:51–61 [DOI] [PubMed] [Google Scholar]
- 15.LaFromboise TD, Hoyt DR, Oliver L, Whitbeck LB. Family, community, and school influences on resilience among American Indian adolescents in the Upper Midwest. J Community Psychol 2006;34:193–209 [Google Scholar]
- 16.Stumblingbear-Riddle G, Romans JS. Resilience among urban American Indian adolescents: exploration into the role of culture, self-esteem, subjective well-being, and social support. Am Indian Alsk Native Ment Health Res 2012;19:1–19 [DOI] [PubMed] [Google Scholar]
- 17.Oster RT, Grier A, Lightning R, Mayan MJ, Toth EL. Cultural continuity, traditional indigenous language, and diabetes in Alberta First Nations: a mixed methods study. Int J Equity Health 2014;13:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwasaki Y, Bartlett J, O’Neil J. Coping with stress among Aboriginal women and men with diabetes in Winnipeg, Canada. Soc Sci Med 2005;60:977–988 [DOI] [PubMed] [Google Scholar]
- 19.Shaw JL, Brown J, Khan B, Mau MK, Dillard D. Resources, roadblocks and turning points: a qualitative study of American Indian/Alaska Native adults with type 2 diabetes. J Community Health 2013;38:86–94 [DOI] [PubMed] [Google Scholar]
- 20.Tiedt JA. Living with diabetes in the 4-fold World of the Coeur d’ Alene tribe. Fam Community Health 2013;36:324–337 [DOI] [PubMed] [Google Scholar]
- 21.Thompson SJ, Gifford SM. Trying to keep a balance: the meaning of health and diabetes in an urban aboriginal community. Soc Sci Med 2000;51:1457–1472 [DOI] [PubMed] [Google Scholar]
- 22.Baldwin JA, Brown BG, Wayment HA, Nez RA, Brelsford KM. Culture and context: buffering the relationship between stressful life events and risky behaviors in American Indian youth. Subst Use Misuse 2011;46:1380–1394 [DOI] [PubMed] [Google Scholar]
- 23.Wexler L. Looking across three generations of Alaska Natives to explore how culture fosters indigenous resilience. Transcult Psychiatry 2014;51:73–92 [DOI] [PubMed] [Google Scholar]
- 24.Les Whitbeck B, Chen X, Hoyt DR, Adams GW. Discrimination, historical loss and enculturation: culturally specific risk and resiliency factors for alcohol abuse among American Indians. J Stud Alcohol 2004;65:409–418 [DOI] [PubMed] [Google Scholar]
- 25.Kading ML, Hautala DS, Palombi LC, Aronson BD, Smith RC, Walls ML. Flourishing: American Indian positive mental health. Soc Ment Health 2015;5:203–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosland AM, Kieffer E, Israel B, et al. . When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. J Gen Intern Med 2008;23:1992–1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hernandez-Tejada MA, Campbell JA, Walker RJ, Smalls BL, Davis KS, Egede LE. Diabetes empowerment, medication adherence and self-care behaviors in adults with type 2 diabetes. Diabetes Technol Ther 2012;14:630–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ratner NL, Davis EB, Lhotka LL, Wille SM, Walls ML. Patient-centered care, diabetes empowerment, and type 2 diabetes medication adherence among American Indian patients. Clin Diabetes 2017;35:281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults: a review and questions for research. J Aging Health 1991;3:3–27 [Google Scholar]
- 30.Anderson RM, Funnell MM, Aikens JE, et al. . Evaluating the efficacy of an empowerment-based self-management consultant intervention: results of a two-year randomized controlled trial. Ther Patient Educ 2009;1:3–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang TS, Gillard ML, Funnell MM, et al. . Developing a new generation of ongoing diabetes self-management support interventions: a preliminary report. Diabetes Educ 2005;31:91–97 [DOI] [PubMed] [Google Scholar]
- 32.Satz RM. Chippewa treaty rights: the reserved rights of Wisconsin’s Chippewa Indians in historical perspective. Transactions of the Wisconsin Academy of Sciences, Arts and Letters 1991;79:1–251 [Google Scholar]
- 33.Treuer A. Ojibwe in Minnesota. St. Paul, MN, Minnesota Historical Society, 2010 [Google Scholar]
- 34.Stopford R, Winkley K, Ismail K. Social support and glycemic control in type 2 diabetes: a systematic review of observational studies. Patient Educ Couns 2013;93:549–558 [DOI] [PubMed] [Google Scholar]
- 35.van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HFJM, van den Borne BHW. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns 2005;59:1–12 [DOI] [PubMed] [Google Scholar]
- 36.Gone JP. Redressing First Nations historical trauma: theorizing mechanisms for indigenous culture as mental health treatment. Transcult Psychiatry 2013;50:683–706 [DOI] [PubMed] [Google Scholar]
- 37.Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS. The Diabetes Empowerment Scale-Short Form (DES-SF). Diabetes Care 2003;26:1641–1642 [DOI] [PubMed] [Google Scholar]
- 38.Michigan Diabetes Research and Training Center Diabetes Care Profile (survey). Available from https://diabetesresearch.med.umich.edu/peripherals/profs/documents/svi/dcp.pdf. Accessed 3 May 2019
- 39.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof 1996;19:208–230 [DOI] [PubMed] [Google Scholar]
- 40.Shakespeare-Finch J, Obst PL. The development of the 2-Way Social Support Scale: a measure of giving and receiving emotional and instrumental support. J Pers Assess 2011;93:483–490 [DOI] [PubMed] [Google Scholar]
- 41.Leach CW, van Zomeren M, Zebel S, et al. . Group-level self-definition and self-investment: a hierarchical (multicomponent) model of in-group identification. J Pers Soc Psychol 2008;95:144–165 [DOI] [PubMed] [Google Scholar]
- 42.IBM Corp IBM SPSS Statistics for Windows, v. 24.0. Armonk, NY, IBM Corp., 2016 [Google Scholar]
- 43.Goins RT, Noonan C, Gonzales K, Winchester B, Bradley VL. Association of depressive symptomology and psychological trauma with diabetes control among older American Indian women: does social support matter? J Diabetes Complications 2017;31:669–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mendenhall TJ, Seal KL, Greencrow BA, Littlewalker KN, Brownowl SA. The Family Education Diabetes Series: improving health in an urban-dwelling American Indian community. Qual Health Res 2012;22:1524–1534 [DOI] [PubMed] [Google Scholar]
- 45.Brown RA, Dickerson DL, D’Amico EJ. Cultural identity among urban American Indian/Alaska Native youth: implications for alcohol and drug use. Prev Sci 2016;17:852–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whitesell NR, Mitchell CM, Spicer P. A longitudinal study of self-esteem, cultural identity, and academic success among American Indian adolescents. Cultur Divers Ethnic Minor Psychol 2009;15:38–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stryker S. Symbolic Interactionism: A Social Structural Version. Menlo Park, CA, Benjamin/Cummings, 1980 [Google Scholar]
- 48.Walls ML, Whitbeck L, Armenta B. A cautionary tale: examining the interplay of culturally specific risk and resilience factors in indigenous communities. Clin Psychol Sci 2016;4:732–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kagawa-Singer M, Dressler WW, George SM, Elwood WN. The Cultural Framework for Health: An Integrative Approach for Research and Program Design and Evaluation. Bethesda, MD, National Institutes of Health, Office of Behavioral and Social Science Research, 2014 [Google Scholar]