Abstract
OBJECTIVE | Treatment of gestational diabetes mellitus and type 2 diabetes during pregnancy can improve maternal and neonatal outcomes; yet, self-care burdens for pregnant women with diabetes are high, particularly for low-income and minority women. Although prior studies have investigated patient-perceived barriers and facilitators to diabetes self-management during pregnancy, little work investigates the perspectives of health care providers (HCPs) on these factors. The objective of this study was to investigate HCPs’ perspectives on patient barriers and facilitators to diabetes care during pregnancy.
METHODS | In this qualitative investigation, focus groups were conducted using a semistructured interview guide designed to elicit HCPs’ perceptions of patient barriers and facilitators to successful diabetes-related self-care. HCPs included physicians, nurses, health educators, and other personnel who care for low-income pregnant women with diabetes. Interviews were transcribed verbatim. Transcripts were analyzed using the constant comparative technique to identify themes and subthemes, using the Social Ecological Model as a theoretical framework.
RESULTS | Participants (n = 29) identified barriers and facilitators to women’s achievement of optimal diabetes self-care according to six levels (environment, access, institution, interpersonal, knowledge, and individual). Example subthemes included inflexible work schedule, poor access to medication and supplies, overburdened clinic, perceived patient “policing,” and low health literacy. Individual factors included self-efficacy, motivation, and engagement. HCPs identified barriers, but not facilitators, for each theme.
CONCLUSION | HCPs described facilitators and barriers to diabetes care at all levels of the Social Ecological Model. These data can inform interventions to dismantle barriers patients face and thus create meaningful health care interventions to improve outcomes for low-income pregnant women with diabetes.
Gestational diabetes mellitus (GDM) is the most common metabolic disorder of pregnancy, and its prevalence is increasing worldwide, with conservative estimates that ∼16% of pregnancies are affected globally (1,2). This increased incidence, fueled by older maternal age and the obesity epidemic, disproportionately affects low-income and racial and ethnic minority women and perpetuates a cycle of health disparities among minority women (1,2). Similarly, the prevalence of women entering pregnancy with type 2 diabetes has also risen and demonstrates similar disparities (3,4).
GDM and type 2 diabetes during pregnancy can be managed with diet and medication, interventions that decrease risk of some adverse maternal and neonatal outcomes. Yet, achievement of adequate glycemic control poses a significant burden for pregnant women. The diagnosis of diabetes mandates self-management action, substantial treatment adherence, and engagement in health care, which can be a greater challenge for women from socially disadvantaged backgrounds.
Prior work has asserted that several social, psychological, behavioral, and economic factors influence a woman’s glycemic control. Factors such as inadequate food security, psychosocial deprivation, and chaotic lifestyle are all thought to influence blood glucose control (5–7). Moreover, women with diabetes experience added logistical, educational, and knowledge-based burdens that can influence pregnancy outcomes. Prior qualitative work with low-income pregnant women with diabetes by our group indicated that additional barriers include anxiety, lack of social support, and inadequate understanding of diabetes and its associated risks (8,9).
Although prior research has elucidated barriers experienced firsthand by pregnant women with diabetes, little work has investigated the unique viewpoint of health care providers (HCPs) regarding their experiences and what they perceive to be the greatest barriers to self-management for patients. Such perspectives are crucial to developing a holistic picture of individuals with diabetes and dismantling barriers and creating meaningful interventions to improve not only patient engagement but also health outcomes during and after pregnancy. Additionally, an understanding of HCPs’ perspectives is necessary to optimally train and support HCPs in providing the best possible care to women in this population. Thus, we aimed to explore HCPs’ perspectives on barriers and facilitators of diabetes care experienced by low-income pregnant women.
Research Design and Methods
This was a qualitative study designed to assess HCPs’ perceptions regarding the experiences of their low-income patients with diabetes during pregnancy and their own experiences in caring for this population. This study was a planned secondary analysis of data from participants who were interviewed during evaluation of a novel mobile health technology for pregnant women with diabetes; however, the present analysis focuses only on HCPs’ views of the experiences of this population. This study was approved by the Northwestern University Institutional Review Board.
Participants were recruited from Northwestern Memorial Hospital in Chicago, IL, from December 2018 to March 2019. This site is a large academic tertiary care center that serves a large and diverse population of pregnant women with all forms of diabetes and additionally serves as a referral site for women requiring maternal-fetal medicine care. In this multidisciplinary practice, maternal-fetal medicine fellows and an advanced practice nurse (APN) have continuity with patients throughout prenatal care via a specialized diabetes in pregnancy program for low-income patients. Faculty maternal-fetal medicine subspecialists and resident obstetrician/gynecologists function as a group practice alongside the maternal-fetal medicine fellows, who organize the collaborative diabetes care. In addition to receiving specialty care from the obstetrical team and endocrinologists as needed, patients also receive onsite counseling from certified health education specialists (CHESs) (personnel certified to provide health information, including diabetes-related education, to patients) and registered dietitians (RDs). Any clinician or HCP who had experience treating or educating pregnant women with GDM or type 2 diabetes was eligible for participation in focus groups. Trainee physicians (residents and fellows) were included to capture the most diverse range of HCP perspectives, including those with less career experience caring for this population. To identify eligible participants, a review of the institution’s clinical personnel records was performed, and potential participants were contacted via e-mail. Interested individuals were organized into focus groups of three to seven individuals at a mutually agreeable time. Focus groups contained HCPs of multiple disciplines; for example, groups did not contain all physicians or all nurses, but rather intentionally included HCPs of multiple professional viewpoints when possible. Participants who were unable to attend groups were interviewed individually.
Focus groups and interviews were conducted in English by a trained research assistant using a semistructured guide, facilitating an open-ended conversation regarding HCP-perceived patient barriers to care and self-management, as well as HCP challenges in providing care for low-income pregnant women with diabetes (Table 1). Although all HCPs had experience caring for women of all income strata at this tertiary care center, they were asked to focus their comments on their experiences caring for women at greater social disadvantage, particularly those with low income or receiving publicly funded prenatal care. Similarly, given the overlap in care strategies and requirements for women with GDM and those with type 2 diabetes, HCPs were able to comment on their experiences in caring for women with either diagnosis. Focus groups lasted for 60–90 minutes and were recorded using a digital audio recorder. All participants provided written informed consent and were compensated with a meal and a gift card.
TABLE 1.
Semi-Structured Interview Guide Topics
| • Role in clinic or at institution with pregnant women with diabetes |
| • Greatest perceived challenges for diabetes patients and management |
| • Perceived facilitators for diabetes patients and management |
| • Greatest challenges in providing care for diabetes patients |
| • Recommended resources for patients to use outside of clinic |
| • Any perceived insufficiency of resources for patients |
Interviews were professionally transcribed verbatim and uploaded to Dedoose (www.dedoose.com), a secure, Web-based platform for organizing qualitative data. Interview transcripts were analyzed using the constant comparative method, a modified version of the grounded theory approach (10,11). In the constant comparative approach, transcripts are read line by line, and recurring concepts are coded by independent analysts. These recurring concepts, called subthemes, are collapsed into overarching themes during iterative readings of the transcripts. Team members met on a weekly basis to reprocess, negate, and organize themes. Themes were further refined and organized in an iterative process throughout the interview and analysis process. Recruitment of new HCPs ceased after reaching saturation—the point at which captured responses reflect the full range of experiences and obtaining more samples likely would not yield novel results.
Analysis was driven by the Social Ecological Model as a theoretical framework (12,13). The defining characteristic of the Social Ecological Model is its emphasis on individuals’ interactions with the environment and vice-versa and how these interactions influence individuals’ health behaviors. The model states that external factors that influence individuals’ actions are composed of public policy, community, institutional, and interpersonal components. Nested centrally within these variables are the intrapersonal factors that affect the external ones. Using this model, themes and subthemes are described below with exemplary quotations.
Results
During this study period, 29 HCPs were interviewed, including 14 physicians, 6 nurses (including 1 APN), 2 medical assistants, 1 RD, 1 licensed clinical social worker, 1 lactation peer counselor, and 4 CHESs. Physician participants included 5 maternal-fetal medicine faculty physicians, 3 maternal-fetal medicine fellows, and 6 obstetrics and gynecology resident physicians. All participants had experience with treating or educating pregnant women with diabetes and worked with both privately and publicly insured women. Providers ranged in years of experience from 1 (first-year resident in obstetrics and gynecology) to >20 (experienced perinatal diabetes-focused APN). Five of 29 providers were unable to attend focus groups and were interviewed individually by trained research personnel; all remaining HCPs participated in focus groups.
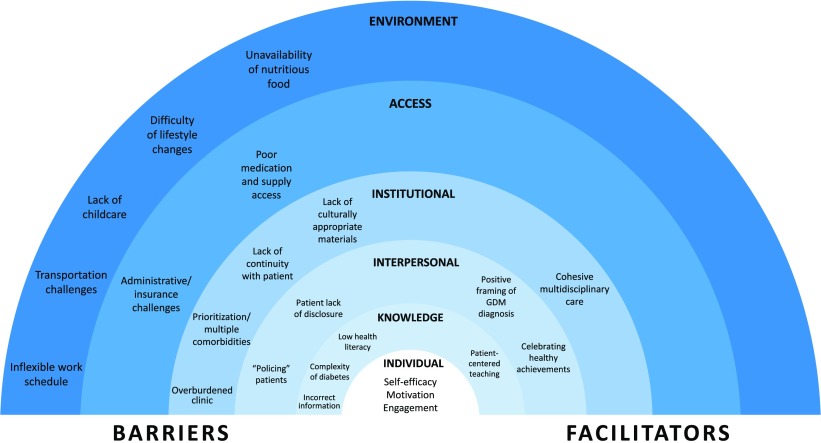
Overarching themes were organized using a modified Social Ecological Model, as described above, yielding primary themes organized around the following factors: environmental, access-related, institutional, interpersonal, knowledge-based, and individual (Figure 1). Each theme encapsulated several subthemes, which were classified as either facilitators or barriers to obtaining care, although not all levels of the Social Ecological Model were identified as having facilitators.
FIGURE 1.
Social Ecological Model of HCP-reported patient facilitators and barriers to diabetes care and self-management during pregnancy.
Environmental Factors
Environmental factors that influenced individuals’ ability to receive care were defined as those that were related to the broader social environment—such as people and institutions—that individuals interacted with or experienced outside of the health care facility. Such interactions may have included their job, family, childcare situation, or other factors. Most facets of patients’ environments were cited as barriers to receiving care (Table 2). HCPs said patients commonly had inflexible work schedules, making it difficult for them to attend prenatal care appointments or conduct diabetes self-care tasks. Many patients also had a lack of transportation in tandem with a strict work schedule, making it difficult for them to arrive at the office in a timely and affordable manner for the frequent appointments required for pregnant women with diabetes. One maternal-fetal medicine fellow stated, “. . . a lot of our patients come from very, very far away, and it’s such a pain, particularly on the south and west sides, to be able to get to the [clinic] with any sense of urgency.” Further, participants frequently cited their patients’ difficulties in finding available and affordable childcare during their frequent clinic appointments in conjunction with their difficulties with transportation.
TABLE 2.
HCP-Identified Patient Barriers to Diabetes Care and Self-Management During Pregnancy
| Theme | Subtheme | Exemplary Quotation |
|---|---|---|
| Environment | Inflexible work schedule | “People who work and their work schedule doesn’t coincide with when they need to eat and check their sugars and take insulin, [or] care for other children and family members, which can make it hard for them to take care of their diabetes. Definitely things like not sleeping, eating, [or] working on a specific schedule.” |
| Transportation challenges | “Like getting here and getting to the appointment and parking . . . is what they’re like focused on, and they get here, and I respect that.” | |
| Lack of childcare | “I also would just say trying to identify with the patient what their barriers are to getting here, whether it be child care or transportation or just their own, you know, personal belief in that, ‘Well, it’s okay if I don’t come for that week.’” | |
| Difficulty of lifestyle changes | “When I was doing counseling for prenatal patients, their diet changes were so hard for them. I’ve done fewer nutritional assessments here, but I feel like behavior or change around diet is such a big one.” | |
| Unavailability of nutritious food | “We had a patient come this week . . . she just looked off. I made a comment, saying, ‘Oh, you don’t look right, what’s wrong?’ And she said that she felt very dizzy. So [a nurse] asked her, ‘When was the last time you ate or drank something?’ And she said, ‘Yesterday.’ And this was afternoon clinic, too, and so right there, I said, ‘Are you having a hard time having food in your house?’ She said, ‘Yes.’” | |
| Access | Administrative/insurance challenges | “We do have a few moms we see [who] are lower income with gestational diabetes, type 1, type 2, and the moms who have the challenge they might have insurance, but it doesn’t cover their urine dipstick or it doesn’t cover . . . their meds. So, it’s a bit of a challenge for the providers. It’s kind of like trial and error.” |
| Poor prescription and supply access | “They don’t have enough glucose test strips, and there’s no way for them to actually test their glucose three, four times a day because they have to stretch out the small supply that they have.” | |
| Institutional | Overburdened clinic | “. . . It’s hard for me in that limited time slot to brainstorm with them ways that they can incorporate taking care of themselves in the greater matrix of everything that’s going on.” |
| Prioritization/multiple comorbidities | “When they come in with multiple comorbidities or other complications in pregnancy [such as] fetal anomalies or what have you, . . . there’s a hierarchical need, and at some points, especially if the fetal side of things is complicated or if there are other comorbid medical conditions [that] are so severe . . . it sort of overshadows the diabetic side of things.” | |
| Lack of continuity with patient | “They usually show up for their first visit, and then . . . sometimes it can be spotty. They want to come for their 20-week ultrasound, so they’ll show up for that visit.” | |
| Lack of culturally appropriate materials | “I think it’s resources that are geared toward this population, like how do you meet these goals given your circumstances and also [be] culturally sensitive and [have] culturally sensitive materials? What are the actual food items that make sense that . . . they’re actually [going to] eat?—not [that] you’ve given them a list of foods that are not typical of [their] diet.” | |
| Interpersonal | “Policing” patients | “You come in with this empty report card. I don’t even have to say anything. I just walk in the room, and I just put it down, and automatically patients will say something or try to explain it. You know, it makes me feel like the police. . . . like the assumption [is] that around our management of this disease, we expect you to be this disciplined person in an environment and in a world that is inherently undisciplined. How do you begin to do that? And I think it’s really hard because it breaks apart that alliance, and it breaks apart the ability to adequately come up with a game plan . . . . I think sometimes it’s hard to communicate to patients without feeling like you’re receiving all of your power as a physician, or you are becoming strictly paternalistic in overriding what they want to do.” |
| Patient lack of disclosure | “I feel like people are sheepish. ‘Oh, I have to tell my doctor that I walked three times this week, so I should probably go out and walk,’ or people will just lie if it really makes them feel bad. . . . You don’t want people to feel bad about not accomplishing their goal.” | |
| Knowledge | Incorrect information | “One of the biggest barriers that I notice with my patients in terms of their diet and managing diabetes in pregnancy also relates to cultural barriers, and that’s [that] they get different information from their clinicians and their providers and different information from their family members, who might tell them to eat for two or, ‘You should eat more,’ or ‘Why aren’t you eating? You need to eat more to have a healthy baby’ as opposed to the clinicians, who might be prescribing [a] more restricted diet, and they’re not sure who to believe or who to follow. . . . And then, I also think that it’s just difficult in general to follow a specific diet when it comes to managing diabetes in pregnancy, especially due to food security issues.” |
| Complexity of diabetes | “You have to remember a lot for diabetes. . . . Like, first of all, it’s confusing. I find it confusing, and I’m extremely health literate compared to someone who didn’t go through all this training, and it’s hard. . . . It’s just overwhelming for people.” | |
| Low health literacy | “A lot of the times, our gestational diabetes patients have a hard time or just their health literacy of gestational diabetes tends to be very low, and they need a lot of education.” |
Individual characteristics presented in Table 4.
Another common environmental barrier was the trouble many women had in changing their diet and activity regimens, likely because of the scope and intensity of recommended changes. Additionally, participants recognized that their patients of diverse backgrounds often had problems finding a culturally congruent meal plan that included their food preferences. A dietitian said, “. . . A lot of women we see are of Hispanic culture or . . . of African descent, and they eat very different food. . . . And trying to understand that and figure out where they’re getting their food from to better help them as well [is difficult].”
One formidable patient struggle HCPs recognized was that of unavailability of nutritious foods, usually because of food deserts or food insecurity. Commonly, recommended foods were seldom affordable options for patients, and, as one clinic nurse stated, “Cheaper food is food that is not going to manage [a patient’s] diabetes.” Many HCPs acknowledged that these food-related barriers often prevented women from being able to adequately control their diabetes, despite their best intentions to do so and their access to food assistance programs. One registered nurse described a scenario that many women face:
“[Patients] are getting the medical plan, but they’re not getting food stamps, right? I’ve had patients saying, ‘I would like to buy more fruits and vegetables, but I make X amount of money, and I [have to] pay bills,’ so it’s . . . going to be whatever they sell at McDonalds for $1 value, because they’re trying to stretch their money.”
No environment-level facilitators of care were identified. Although environmental-level facilitators such as city-based resources for fresh food or pregnancy support groups exist, these were sparingly mentioned by participants.
Access-Related Factors
Access factors were those related to patients’ ability to obtain high-quality, affordable health care in a timely manner. In many cases, access factors were directly correlated to patients’ insurance status (Table 2). HCPs stated that their patients were often inconsistently insured; sometimes, patients were uninsured or their insurance providers changed, leaving them with gaps in coverage, particularly for women whose public insurance ended 42 days after delivery. Other women were only able to enroll in public insurance after becoming pregnant and thus had not been able to obtain adequate health care before conception.
Even for patients who were insured and had access to HCPs, participants stated that one of the most obstructive barriers to diabetes care was suboptimal access to self-care supplies and prescription drugs, usually because of insurance restrictions (Table 2). For example, one nurse stated that the hospital where she had worked previously did not have glucose meters. “I do remember a couple people at [another hospital] saying that they needed a new glucometer, and we weren’t able to prescribe it through the hospital,” she said. “It’s not something that the pharmacy had.” Additionally, patients were sometimes unable to obtain supplies and medications because they were unable to afford them, despite being insured.
No access-level facilitators of care were identified by these participants.
Institutional Factors
Institutional factors were those that HCPs felt were embedded into the process of providing care itself. Institutional factors were largely identified as barriers, with four subthemes identified (Table 2). First, providers described an overburdened clinic, at which patients were only scheduled for 15-minute follow-up visits even if multiple providers needed to see them. Even the slightest deviation from such tight scheduling resulted in major delays. Almost all participating physicians felt that they were not allotted enough time to fully explain diabetes, diabetes care, self-management recommendations, and potential consequences of the disease. In addition to the practice-based barrier of high clinic volume, HCPs also reported an institutional barrier related to treating complicated patients in this practice; if patients had multiple comorbidities, even less time could be allotted to each concern. Many HCPs expressed a desire for additional time to more comprehensively counsel and educate their patients about each comorbidity and its short- and long-term management and consequences. As one HCP said,
“When they come in with multiple comorbidities or other complications, . . . there’s a hierarchical need, and at some point, especially if the fetal side of things is complicated or if there are other comorbid medical conditions [that] are so severe, it sort of overshadows the diabetic side of things. Many times, we’re playing sort of like ‘What can we deal with today? What can we deal with next time?’ because we have such limited time.”
In many cases, HCPs reported that patients with comorbidities were scheduled to see several specialists to treat different conditions. One fellow who provided primary perinatal diabetes care felt that specialist appointments were not “optimized” and found that much of his time was “devoted to other things rather than necessarily primary diabetic management” because he had to explain several other aspects of patients’ conditions to them.
Another identified institutional barrier was a lack of continuity. One participant said, “Some of the challenge is actually getting [the patients] to show up for the visit,” and another described patients’ appointment attendance as “spotty.” This lack of continuity made it difficult for HCPs to provide consistent diabetes care. Additionally, because of the nature of a teaching practice, some physicians noted a particular lack of constancy with their patients.
A final institutional barrier was related to the lack of multilingual patient education materials. Participating Health Learning Center personnel explained that, although the institution had materials available in Spanish, sometimes it lacked written or audio materials in other languages. Participants acknowledged that this barrier could make it exceedingly difficult for patients to understand their diagnoses and treatment plans. Additionally, as noted with environmental barriers, HCPs expressed a lack of cultural sensitivity and awareness of patients’ cultural preferences with regard to dietary counseling and available educational materials. Specifically, much of the counseling and hospital-approved patient education materials did not contain information about foods from different cultures, nor did they address patients’ individual food preferences. As one resident said,
“I think it’s resources that are geared toward this population, like how do you meet these goals given your circumstances and also [be] culturally sensitive and [have] culturally sensitive materials? What are the actual food items that make sense that . . . they’re actually [going to] eat?—not [that] you’ve given them a list of foods that are not typical of [their] diet.”
The one identified institutional facilitator was the presence of cohesive multidisciplinary care at the institution (Table 3). One registered nurse said,
TABLE 3.
Provider-Identified Patient Facilitators to Diabetes Care and Self-Management During Pregnancy
| Theme | Subtheme | Exemplary Quotation |
|---|---|---|
| Environment & Access | No facilitators identified | |
| Institutional | Cohesive multidisciplinary care | “My clinic is a great clinic for diabetes care because it’s great for our moms because they not only see the [maternal-fetal medicine specialist], they see [the APN] and/or the endocrinologist. [T]he providers . . . can step out of the room and chat with each other about the patient’s care, and it’s right there. So, our patients . . . don’t have to wait, ya know? Because they have the answer. . . .” |
| Interpersonal | Positive framing of diabetes diagnosis | “That’s where [the APN] comes in, which is a big attribute to our department, I must say, because she can alleviate a lot of fears . . . because there’s a lot of fear with it. Will I end up on insulin? . . . What’s going to happen to my baby? Is my baby gonna be too big to deliver? [T]hose are all things that create a fear for the patient, and if we can alleviate those fears by them having contact, quick contact that’s easy for the provider [and] easy for the patient, I think it’ll be a really positive outlook for pregnancy for them.” |
| Celebrating achievable milestones | “Our patients are really motivated by the ultrasounds and by the [non-stress tests]. When a patient is a type 2 diabetic on insulin or gestational diabetic on insulin, we do more fetal testing, so I find my experience that the patients who earlier in the pregnancy I was sort of every week reminding them to do certain mundane tasks and tests . . . were really excited to get the test done. That I think is very motivating; the baby becomes real; the pregnancy becomes more real. They’re looking at the fetal growth at 32 and 36 weeks . . . [and] patients, I think, are very motivated for that. | |
| Knowledge | Patient-centered teaching | “It’s a team approach. . . .[If the endocrinologist] steps out and says, ‘You know what? I really think [the APN] should see this patient,’ [the APN] puts her on her schedule, she sees them, and they’re counseled. So, they get an extensive education piece with [the APN]. It’s really, really good. And [it's] available for moms who have [the] low-income clinic, too.” |
Individual characteristics presented in Table 4.
“. . . The patient may share to the dietitian something different than she will share to the APN than she will share to the resident . . . and I think the benefit in a clinic like [this institution] is that these people are intertwined, and they have the ability to speak with each other. I think in a lot of other clinics . . . you have an endocrinologist that doesn’t necessarily always speak with the physician, that doesn’t speak with the dietitian, and I think that can make for disjointed care and mixed messages for patients.”
Additionally, one licensed practical nurse explained the importance of the availability of an APN in clinical settings ranging from “[private] clinic to [resident] clinic to labor and delivery to antepartum.” The nurse explained that, should a physician feel that a patient needed to be counseled by the APN, visits were easy to coordinate given the interdisciplinary nature of the clinic and the ease of communication among disciplines.
Interpersonal Factors
This theme focused specifically on factors that influenced relationships between patients and HCPs. Two interpersonal barriers (Table 2) and two facilitators (Table 3) were identified. One of the most commonly referenced drawbacks to patient-provider relationships was rooted in the nature of diabetes management itself. Many HCPs reported feeling like they “policed” their patients when they uploaded blood glucose readings from their glucose meters and reviewed the results. One fellow stated,
“Because they give you their meter, [and you] go and physically upload it yourself, and you come back with a sheet, a report card, on how they did, and, like, it’s empty, it’s a sign they didn’t check their sugars. If they’re really high, it’s a sign, it’s often the diet. So, you are kind of checking up on them in a really basic way every week or every other week.”
Another fellow similarly stated that he felt that he was checking his patients’ “empty report card”; without even having to say anything, patients would often explain themselves and attempt to justify their blank glucose logs.
Another related barrier to providing high-quality and effective diabetes care was the HCPs’ sense of a lack of patient disclosure regarding health information. A dietitian said,
“. . . [T]hey’re afraid to tell me what they’re truly eating, so it’s very difficult to actually help them clinically if they won’t tell us what’s actually going on at home and if they’re not bringing in their meters, we also can’t really understand what’s going on at home and how the foods they’re eating are impacting their blood sugar . . . Even when they do tell me what they eat, sometimes they’re not as truthful as they could be.”
Despite the challenges present in the patient-provider relationship, HCPs reported that facilitators of care included positive interpersonal factors (Table 3). They reported feeling able to exert a positive influence on their interactions with patients to facilitate better health outcomes. One fellow cited the importance of framing a diabetes diagnosis as something manageable and conquerable because this approach generally increased patients’ sense of self-efficacy and improved their engagement with health care. This fellow said,
“I think framing the disease in a way that is not, like, life-threatening . . . . These are otherwise healthy women who then all of the sudden have GDM, and then they’re like, ‘Oh, this is a huge complication, this is a huge setback, something bad is gonna happen,’ and when you contextualize it, yes, there are adverse outcomes, but in the grand scheme of things, this is a treatable disease. You may have a high risk of developing type 2 in the future, but for now, if we monitor it and we initiate therapy . . . this is very well managed.”
Similarly, several participants stated the importance of acknowledging healthy achievements. For example, some HCPs noted that undergoing an ultrasound and receiving a healthy result, a common obstetric milestone, was an extremely motivating event for patients. Several nurses agreed that most patients made sure to attend the ultrasound and non–stress test appointments, and encouraging this engagement was seen as a facilitator. Similarly, other achievements included achieving successful glycemic control. One APN illustrated her approach to affirming patients’ successes, saying,
“I do ‘jelly bean dances’ every time I see a woman coming in. No really, [if a patient is] 300 pounds and has not gained a pound, . . . [I say], ‘Get off your seat and dance with me. This is great!’ . . . I think everybody needs to celebrate those achievements a little bit more.”
Knowledge-Based Factors
Knowledge-based facilitators and barriers related to patients’ factual knowledge regarding diabetes during pregnancy, including the meaning of the diagnosis, treatment, plan of care, and risks to the fetus. One identified knowledge-based barrier involved patients acquiring inaccurate information (Table 2), usually from the Internet or well-meaning family members. Patients often searched for information online. One nurse stated,
“. . . [P]atients will come in and . . . they have not been eating any carbs because they read on the Internet that they should have zero carbs, or they have cut out all fruit because they heard that fruit is really bad . . . or they’ll have a gestational diabetes blog they’re reading where they heard that intermittent fasting worked, or X, Y, Z diet trend worked . . . ”
Family members also communicated misinformation. Providers reported that family members of patients with diabetes would tell them to “eat for two” and question why a pregnant woman was eating less than expected, leading to confusion and challenges following nutritional therapy. For example, one provider stated,
“Sometimes [family members] can be a good resource, and sometimes they can be a not-so-great resource. . . . [T]hey may have a family history . . . of diabetes. So, then their aunt tells them, ‘You’ve got to avoid all of these foods,’ and they scare them, and they feel like, ‘ I can’t eat anything.’”
In some cases, these conflicting messages from family members could stem from cultural beliefs about appropriate weight gain during pregnancy.
HCPs also identified complexity of knowledge requirements as an additional knowledge-based barrier. Participants repeatedly referenced the complexity of managing diabetes and explained that understanding this information and the way it was presented could be cognitively taxing for many patients, regardless of their education or socioeconomic status. One nurse explained this problem:
“When you look at a. . . first-time mom who is coming into pregnancy itself with all of its challenges and educational needs and questions and fears, and then you add the diagnosis of gestational diabetes on top of it . . . I think it compounds the educational feeling of being overwhelmed with things they don’t know and that might frighten them.”
This problem of being educationally overwhelmed was often described as complicated by the fact that many patients seen by this cohort of HCPs had very low health literacy and struggled to understand their diagnoses and treatment plans.
In contrast, one knowledge-based facilitator that many HCPs cited was the commitment to patient-centered teaching (Table 3). Patient-centered teaching focused on taking the necessary time and effort to explain information to patients in an understandable manner. Although office visit time limitations compete with this facilitator, physicians acknowledged that health information could be overwhelming for patients and said that having a commitment to high-quality patient teaching could support better care and outcomes. One physician explained her approach to teaching patients about diabetes:
“I think the [American College of Obstetricians and Gynecologists] patient [flyers] are probably the most easy to digest, but . . . to be honest, it’s like just handing them packets of words that are never gonna get read . . . . I end up just drawing a lot of stuff out for people. . . . I feel like I engage them more when they’re learning right in front of them, and I’m putting it in a picture instead of writing words that they’ve probably never heard of.”
Individual Factors
The innermost semicircle in the model shown in Figure 1 includes three individual traits that influence the encircling facilitators and barriers. Individuals’ level of self-efficacy, engagement, and motivation were perceived to be crucial influencers of outcomes (Table 4). One maternal-fetal medicine fellow explained how crucial a woman’s self-efficacy was in managing diabetes, saying,
TABLE 4.
Individual Characteristics Influencing Diabetes and Self-Management During Pregnancy
| Theme | Subtheme | Exemplary Quotation |
|---|---|---|
| Individual | Self-efficacy/control | “The other thing that I think is a little bit of a self-fulfilling cycle . . . that’s special to our clinic or unique maybe to the patients that we see that are lower socioeconomic status is that their self-efficacy is very different than that that I’ve experienced with patients who are of higher socioeconomic status or higher educational brackets. . . . Oftentimes, their life has been chaotic. They haven’t had control over things in the past, outside of pregnancy, outside of diabetes, things have kind of just happened to them as opposed to them feeling, like, control over the different aspects of their life. . . . I think that that plays into their diabetes, too. They don’t necessarily exhibit or portray that they have self-efficacy over the situation, that they have the ability to control it. It’s kind of more something that they resign to . . . ‘Things haven’t gone right for my life in the past. They’re not gonna go right now. Why would this be any different?’ Like it’s just kind of something that’s happening to them that’s out of their control almost.” |
| Motivation | “Sometimes this is a really high time to capture people because, if they are really concerned about their health or their baby’s health, it can be a really big motivating factor. Like, ‘Okay . . . maybe before I wasn’t taking care of myself, but now I really have to make sure this baby is okay. So, yes, I’m going to listen to everything you say, even if it’s just for the weeks that I’m pregnant, because I really want to make an impact.’ So sometimes that is the case, so that’s helpful.” | |
| Engagement | “The level of engagement to a provider or to a system for [lower-income] women is different than [for] those women who have high expectations from the system.” |
“The other thing that I think is a little bit of a self-fulfilling cycle . . . that’s special to our clinic or unique maybe to the patients that we see that are lower socioeconomic status is that their self-efficacy is very different than that that I’ve experienced with patients who are of higher socioeconomic status or higher educational brackets. . . . Oftentimes, their life has been chaotic. They haven’t had control over things in the past, outside of pregnancy. . . . I think that that plays into their diabetes, too. . . . It’s kind of more something that they resign to . . . ‘Things haven’t gone right for my life in the past . . . . Why would this be any different?’”
According to participants, another important influencer of health behavior was a woman’s level of motivation. Many women were motivated to adhere to their treatment plans because of their desire for healthy outcomes for their fetus. As one resident stated, “A lot of our moms are very motivated, which is a good thing. They care a lot about their fetuses, and that makes this an even better time in their life to make a lifestyle change because they have the emotional energy to do so.” In contrast, reduced motivation in conjunction with other barriers may further challenge a woman’s ability to succeed.
As a combined result of individual self-efficacy and motivation, women were reported as having varying levels of engagement. Several HCPs cited low patient engagement in health care with various underlying reasons. Sometimes, they said, patients did not think the treatment they were receiving was strictly necessary, a circumstance also known as failure of outcome expectation. One HCP said that, “[Some women have a] personal belief in that, “Well, it’s okay if I don’t come for that week. I’ll just wait a couple more weeks. I know I’ll be okay.” In other cases, participants believed their patients simply were unable to engage in health care because of their busy lives.
Discussion
Diabetes management during pregnancy is often burdensome and complex, particularly for low-income and minority women. Prior data have identified patient-perceived facilitators and barriers to diabetes care; however, to develop effective interventions and optimize provider training to improve health outcomes, it is necessary to understand HCP-identified facilitators and barriers.
HCPs in this study identified factors that affect diabetes care and self-management that fell into the broad categories of environment, access, institution, interpersonal, knowledge, and individual factors. Environmental barriers included patients’ inflexible work schedules, transportation challenges, and lack of childcare, all of which contributed to patients’ difficulties in attending frequent appointments. Additionally, patients struggled with making lifestyle changes and with the unavailability of nutritious food. Access-level barriers were related to insurance challenges. Institutional barriers included a high-volume clinic, comorbidities, lack of continuity, and minimal or unavailable multicultural educational materials. Cohesive multidisciplinary care was identified as the sole institutional facilitator. Interpersonal barriers included HCPs’ perceptions that they were “policing” their patients and that their patients were not being fully truthful. Interpersonal facilitators included positively framing a diabetes diagnosis and celebrating healthy achievements. Knowledge barriers encompassed patient acquisition of inaccurate information, as well as the complexity of diabetes management, compounded by low health literacy, whereas patient-centered teaching was a facilitator. Finally, varying levels of patient self-efficacy and motivation led to different levels of engagement with health care and was perceived to affect outcomes.
Limited information exists regarding HCPs’ perspectives on patient experiences in the context of diabetes during pregnancy. One study, performed with a group of 10 HCPs to investigate their perceptions of barriers to care for adolescents with type 1 diabetes, identified family conflict as a common barrier (14). Although this report explored a different population, themes common to our study included difficulties with insurance and financial constraints. Another study investigated HCPs’ perceived barriers to type 2 diabetes care in remote Aboriginal settings (15); however, because of the differences in location and patient population, these results are of limited relevance to low-income pregnant women with diabetes in the United States. One qualitative meta-synthesis study compared factors that both patients and HCPs found to be facilitators of or barriers to medication adherence (16). This study found that increased positive emotion experienced by patients increased their sense of self-efficacy, which underscores the importance of the facilitator of positively framing a diabetes diagnosis that was identified in this study (16). The meta-synthesis also noted barriers congruent with those identified in our study—namely, the complexity of diabetes, logistical/environmental barriers of transportation and childcare, and access-related cost barriers (16). Finally, one study recently investigated the perspectives of patients and HCPs regarding barriers to postpartum follow-up for women with gestational or type 2 diabetes (17). HCPs cited barriers such as patients being overwhelmed with a diabetes diagnosis, which highlights the importance of framing gestational diabetes as a conquerable pregnancy complication (17). Importantly, HCPs also cited difficulties in coordinating care with physician subspecialists, nutritionists, and diabetes educators, which emphasizes the facilitator of cohesive multidisciplinary care identified in our study.
The findings from our work largely mirror prior research investigating patient-perceived barriers to and facilitators of diabetes care. In a prior study done by our group (8,9), several barriers identified by pregnant women aligned with those identified by providers herein, including difficulties with transportation and childcare; inability to afford nutritious foods, medications, and supplies; and low self-efficacy. Our prior work also emphasized the burden of disease management, which aligned with HCP-identified difficulties with the complexity of diabetes knowledge. Data from another study also align with our HCP-identified barriers, including time constraints during office visits, a dearth of more culturally and linguistically relevant information, and limited access to affordable, nutritious food (16).
Strengths of this study include participation of a diverse group of HCPs, who were involved in a broad range of patient care activities. Inclusion of such a diverse group allowed for the examination of facilitators and barriers at various systemic and interpersonal levels. Additionally, this study is one of the first to investigate HCPs’ perspectives on facilitators of and barriers to diabetes care during pregnancy. However, this study was limited to a single academic hospital, and results are not fully generalizable; the perspectives of HCPs from other institutions, medical specialties, and health care settings could yield different and new facilitators of and barriers to patient care within those populations. Additionally, if HCPs did not mention a facilitator or barrier of their own accord, they were not prompted to comment on facilitators and barriers described in prior literature so as not to bias responses. Thus, participant responses may not have captured the full range of existing facilitators and barriers. For example, issues of patient mistrust or racial congruence between patients and providers were not emphasized by our participants but are important areas for future exploration.
Low-income and minority women are more likely to experience diabetes during pregnancy as well as barriers to successful diabetes self-management. Therefore, it is important to consider both HCP- and patient-identified barriers to enrich effective interventions to subsequently enhance favorable patient outcomes. Environmental and access-related barriers are exceedingly difficult to change; however, much opportunity lies at the institutional, interpersonal, and knowledge-based levels. At the institutional level, promoting continuity of care with non-physician personnel, particularly nurse practitioners and diabetes educators, could improve patient engagement and education. Addressing institutional barriers that limit sufficient time for multidisciplinary clinic visits would also contribute to improving the quality of care. Additionally, availability of culturally relevant, literacy-matched, and responsive patient information in various languages could increase patients’ understanding of and ability to engage with treatment plans. Furthermore, positively framing diabetes diagnoses and providing targeted, patient-centered education could increase patients’ self-efficacy and belief in their ability to conquer diabetes, as well as dispel myths or incorrect information regarding diabetes. Clearly, understanding HCP experiences remains crucial to improving diabetes care and outcomes for all.
Article Information
Funding
L.M.Y. was supported by National Institute of Child Health and Human Development (NICHD) grant K12 HD050121-11 at the time of the study. Additionally, this work was supported by the NICHD grant 1R21 HD094271-01.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
All authors contributed equally to this work. L.M.Y. conceived of and supervised the project, wrote the grant that funded the project, and wrote the manuscript. K.L. collected and analyzed data and wrote the manuscript. J.J. collected and analyzed data and reviewed/edited the manuscript. C.M.N. reviewed/edited the manuscript and contributed to the discussion. M.A.S. supported the writing of the grant, reviewed/edited the manuscript, and contributed to the discussion. L.M.Y. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
This abstract was presented at the Society for Maternal-Fetal Medicine 40th Annual Pregnancy Meeting in Grapevine, TX, 3–8 February 2020.
References
- 1.Yuen L, Wong VW, Simmons D. Ethnic disparities in gestational diabetes. Curr Diab Rep 2018;18:68. [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists Committee on Practice Bulletins ACOG Practice Bulletin No. 190: gestational diabetes mellitus. Obstet Gynecol 2018;131:e49–e64 [DOI] [PubMed] [Google Scholar]
- 3.Britton LE, Hussey JM, Crandell JL, Berry DC, Brooks JL, Bryant AG. Racial/ethnic disparities in diabetes diagnosis and glycemic control among women of reproductive age. J Womens Health (Larchmt) 2018;27:1271–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peng TY, Ehrlich SF, Crites Y, et al. Trends and racial and ethnic disparities in the prevalence of pregestational type 1 and type 2 diabetes in Northern California: 1996–2014. Am J Obstet Gynecol 2017;216:177.e1–177.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahr MK, Suter MA, Ballas J, et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am J Obstet Gynecol 2016;214:110.e1–110.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colicchia LC, Parviainen K, Chang JC. Social contributors to glycemic control in gestational diabetes mellitus. Obstet Gynecol 2016;128:1333–1339 [DOI] [PubMed] [Google Scholar]
- 7.Cosson E, Bihan H, Reach G, Vittaz L, Carbillon L, Valensi P. Psychosocial deprivation in women with gestational diabetes mellitus is associated with poor fetomaternal prognoses: an observational study. BMJ Open 2015;5:e007120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yee LM, McGuire JM, Taylor SM, Niznik CM, Simon MA. “I was tired of all the sticking and poking”: identifying barriers to diabetes self-care among low-income pregnant women. J Health Care Poor Underserved 2015;26:926–940 [DOI] [PubMed] [Google Scholar]
- 9.Yee LM, McGuire JM, Taylor SM, Niznik CM, Simon MA. Social and environmental barriers to nutrition therapy for diabetes management among underserved pregnant women: a qualitative analysis. J Nutr Educ Behav 2016;48:170–180.e1 [DOI] [PubMed] [Google Scholar]
- 10.Hallberg L-M. The “core category” of grounded theory: making constant comparisons. Int J Qual Stud Health Well-being 2006;1:141–148 [Google Scholar]
- 11.Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL, Aldine Publishing Company, 1967 [Google Scholar]
- 12.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351–377 [DOI] [PubMed] [Google Scholar]
- 13.Glanz K, Rimer B, Viswanath K. Health Behavior: Theory, Research, and Practice. 5th ed. San Francisco, CA, Jossey-Bass, 2015 [Google Scholar]
- 14.Redondo MJ, Callender CS, Gonynor C, et al. Diabetes care provider perceptions on family challenges of pediatric type 1 diabetes. Diabetes Res Clin Pract 2017;129:203–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhattacharyya OK, Estey EA, Rasooly IR, Harris S, Zwarenstein M, Barnsley J. Providers’ perceptions of barriers to the management of type 2 diabetes in remote Aboriginal settings. Int J Circumpolar Health 2011;70:552–563 [DOI] [PubMed] [Google Scholar]
- 16.Brundisini F, Vanstone M, Hulan D, DeJean D, Giacomini M. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: a qualitative meta-synthesis. BMC Health Serv Res 2015;15:516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCloskey L, Sherman ML, St John M, et al. Navigating a ‘perfect storm’ on the path to prevention of type 2 diabetes mellitus after gestational diabetes: lessons from patient and provider narratives. Matern Child Health J 2019;23:603–612 [DOI] [PubMed] [Google Scholar]