Abstract
Background:
Exposure to incarceration is associated with increased risk of mortality, and HIV is cited as a leading cause of death. Yet, few studies have examined the association between incarceration and mortality among people with HIV (PWH), specifically whether and how increasing exposure to incarceration increases risk of mortality. We compared mortality by different incarceration exposures and HIV status.
Methods:
We conducted a prospective cohort study of participants in the Veterans Aging Cohort Study (VACS) from January 2011 to August 2017 (N=5,367). The primary exposure was incarceration by three measures: 1) any (ever/never); 2) frequency; and 3) cumulative duration. Stratifying by HIV status and controlling for age, race, and gender, we used Cox Proportional Hazard models to estimate adjusted hazard ratios (AHRs) and 95% confidence intervals (CIs).
Results:
Incarceration was associated with increased risk of mortality compared with those never incarcerated for PWH (AHR 1.37; 95% CI, 1.13–1.66) and those uninfected (AHR 1.24; 95% CI, 0.99–1.54), but the association was only statistically significant among PWH. Increasing frequency of incarceration was associated with higher risk of mortality in both groups: for PWH, AHRs 1.13, 1.45, and 1.64 for 1, 2–5; 6+ times, respectively; for uninfected, AHRs 0.98, 1.35, and 1.70 for 1, 2–5, and 6+ times, respectively.
Conclusions:
PWH were at increased risk for mortality following incarceration and repeated exposure to incarceration was associated with mortality in both groups in a dose-response fashion. This increased risk for mortality may be mitigated by improving transitional healthcare, especially HIV care, and reducing incarceration.
Keywords: HIV, incarceration, mortality, community reentry
Introduction
Incarceration is associated with an increased risk of mortality following release from correctional facilities.1–3 HIV is a condition of particular interest for three reasons: people with HIV (PWH) are known to experience incarceration at rates at least three times higher than the general population;4 previous studies have shown incarceration and release to be a risk factor for inferior HIV control;5,6 and HIV is a leading cause of excess death among formerly incarcerated individuals.1,3,7 Despite this, few studies have looked at the association between incarceration and mortality risk in those with HIV, especially in the United States.
One recent study compared standardized mortality ratios between PWH released from prison in Connecticut and the general population of the state, and found the exposed group to be at 8.5 greater risk of death.8 The two most common causes of death were HIV/AIDS-related and overdose. However, this study does not isolate the effect of incarceration on mortality among PWH. Additionally, this was a single state study, limiting the generalizability of the current literature. One plausible reason why incarceration may exacerbate risk of death among PWH is that this population experiences greater harm from gaps in care or lapsed health insurance, as is frequently experienced by individuals after release from custody.9 To our knowledge, there are no studies comparing mortality among PWH who have been incarcerated to PWH who have not been incarcerated.
Another gap in knowledge includes how differences in exposure to incarceration, such as duration or frequency of incarceration, may influence an individual’s risk for mortality after release. Prior studies, not specific to PWH, have suggested an increasing mortality risk with increasing duration of incarceration, including an analysis among persons on parole in New York state, which revealed a 15% increase in odds of death for each year spent incarcerated.10 Interestingly, in the study of Connecticut PWH recently released from prison, re-incarceration seemed to exhibit a protective effect, though the authors note this finding is only significant among participants receiving frequent transitional care visits and may be related to increased access to healthcare and medications while incarcerated.8 To our knowledge, no multisite study has explored whether increasing levels of exposure to incarceration is associated with increasing mortality in either PWH or uninfected populations.
To further understand mortality risk among PWH who have been incarcerated, as well as if increasing exposure to incarceration contributes to this risk, we used the Veterans Aging Cohort Study (VACS) to compare mortality by intensity of incarceration exposure among persons with and without HIV. We hypothesized that among both PWH and those uninfected, exposure to incarceration would be associated with increased risk of mortality, and there would be a dose-response relationship between increasing exposure to incarceration and risk of death.
Methods
Data Source
The Veterans Aging Cohort Study is an ongoing national observational cohort study of patients with HIV in the Veterans Health Administration (VHA) and an uninfected group matched two-to-one on age, race and ethnicity, gender, and clinical site. This study identifies patients beginning in 1996 and was designed to examine the role of alcohol and drug use and comorbid medical and psychiatric disease in determining clinical outcomes in HIV infection. A survey study of 3,728 PWH and 3,787 uninfected individuals starting in 2002 is nested within this large observational cohort study and uses survey, administrative, and clinical data from eight nationwide sites (Atlanta, GA; Baltimore, MD; Bronx, NY; New York City, NY; Houston, TX; Los Angeles, CA; Pittsburgh, PA, and Washington, DC); the full methods have been described elsewhere.11 The institutional review boards at all locations approved this study, which includes written consent prior to enrollment.
The analytic sample used for this study included all participants who provided a response to incarceration questions in a VACS follow-up survey between January 2011 to August 2017. If more than one survey was completed, we used the first survey in which the respondent provided a positive response to incarceration.
Exposure
To assess exposure to any incarceration, we used responses to the following questions: “Have you ever spent time in a jail, prison, detention center, or juvenile correctional facility” (yes/no/don’t know); “How many times have you been in a jail, prison, detention center, or juvenile correctional facility?” (once/2–5 times/6–10 times/greater than 10 times/don’t know); “In your entire life, how much total time have you been in a jail, prison, detention center, or juvenile correctional facility?” (“less than a month/less than a year/between 1–5 years/more than 5 years/don’t know). If a participant indicated they had been in jail or prison on any of the three questions about incarceration, we considered them to have been incarcerated. We used the second question to assess a participant’s frequency of exposure to incarceration, and the third to assess a participant’s cumulative duration of exposure to incarceration. Participants with missing information were excluded from the analysis pertaining to the associated question.
Outcome
The primary outcome was mortality. Observation time and mortality were measured beginning with the date of VACS survey used to identify incarceration status and ending with date of death or August 7, 2018, whichever came first. Deaths were comprehensively identified from four sources: 1) the Patient Treatment File, which records hospital deaths in the VHA Healthcare system, 2) the Beneficiary Identification Records Locating System, which tracks VHA death benefits, 3) Medicare Vital Status File, and 4) Social Security National Death Index.
Additional Covariates
We assessed non-modifiable demographic covariates including age (continuous), gender, and race (black, other). We also assessed the following potential mediators: education (less than high school (HS), HS graduate or GED, some college, or college graduation or more), social support, history of homelessness, unhealthy alcohol use, smoking status (never, former, current), past year drug use, diagnosis of mental health condition, hepatitis C (HCV) status (infected versus uninfected). All time-varying covariates were assessed at time of survey. We defined social support as presence of at least one friend or family members who could be called on for help which has been shown to be associated with health outcomes in prior literature.12 We defined unhealthy alcohol use within the past year using the Alcohol Use Disorders Identification Test – Consumption (AUDIT-C), where a score greater than or equal to 3 for women or 4 for men constituted unhealthy alcohol use.13,14 Past year drug use was defined as any self-reported use within the last year of cocaine, stimulants (“amphetamines, uppers, speed, crank, crystal meth, or bam”), heroin, prescription opioids, benzodiazepines, or injection drug use. We defined diagnosis of a mental health condition using the electronic health record and obtained International Classification of Diseases 9th edition administrative diagnoses for schizoaffective disorder, psychosis, schizophrenia, bipolar disorder, major depression, or post-traumatic stress disorder. We ascertained HCV status using the electronic health record; those having a positive HCV viral load, positive antibody test, or clinical diagnosis in the clinical data were defined as having HCV.15 We looked at degree of liver fibrosis using the FIB-4 index, which is a validated index score calculated from platelet count, alanine transaminase, aspartate transaminase, and age16. A FIB-4 score greater than 3.25 is considered consistent with advanced fibrosis. Clinical factors specific to HIV infection were also assessed among the cohort of PWH, including CD4 count (>200 cells/mm3 or ≤200 cells/mm3) and viral load (≤500 copies/mL vs. <500 copies/mL). All laboratory measures were acquired using clinical data for lab values closest to and within one year of the survey date.11
Analyses
We compared baseline characteristics among PWH and uninfected respondents by any prior incarceration. Comparisons were calculated using chi-square tests of independence for categorical variables and t-tests for continuous variables. We then calculated unadjusted mortality rates per 100-person years (pys) by the three incarceration measures. To test the association between prior incarceration and mortality adjusted for demographics, we used Cox Proportional Hazard models controlling for age, gender, race to estimate an adjusted hazard ratio (AHR). We then assessed an AHR for each level of frequency incarcerated, as well as cumulative duration incarcerated. We also tested whether the relationships of level of frequency and cumulative duration incarcerated with mortality were linear. Analyses were stratified by HIV status.
Finally, we conducted a cross-sectional mediation analysis following the Baron and Kenney methodology17 to explore how potential mediators may impact the association between prior incarceration and mortality. A significant association between prior incarceration and mortality was found only in the PWH cohort, thus mediation analysis was limited to this group. We evaluated an association between prior incarceration and the proposed potential mediator (Pathway A), and the potential mediator and mortality (Pathway B). Potential mediators were selected based on statistical significance (p<0.05) in univariate analyses with both incarceration and mortality. We then conducted separate Cox regression models testing for an association between potential mediators which met the above criteria and mortality, adjusting for prior incarceration (Pathway C). We calculated AHRs with 95% confidence intervals and considered an association significant for a p-value <0.05. We conducted all analyses in Stata Version 14.2.
Results
Overall Sample Characteristics
The analytic sample includes 2,717 PWH and 2,650 uninfected participants. The proportion excluded for missing data was low (1.4% for any prior incarceration; 3.3% for frequency incarcerated and 3.4% for time spent incarcerated). The mean observation time was 5.4 years (95% CI, 6.1–7.1) for PWH and 5.3 years (95% CI, 5.5–7.1) among the uninfected. PWH and uninfected participants reported prior incarceration in similar proportions (55% vs. 57%, respectively p=0.10). Overall, 28.9% of the study population had been incarcerated 2–5 times and 11.7% had been incarcerated 6+ times; 14.2% had been incarcerated 1–5 years, and 7.7% had been incarcerated >5 years.
The mean age of participants was 57 years (range 22–90), and 95% were male. Of those who had been incarcerated, the majority (72%) of participants were black (n= 2,173); 14% were white (n=435), 8% were Hispanic (n=244), 5% identified as “other” race (n=157) and 51% reported annual income of less than $12,000 (n=1497). In this group, 41% had HCV infection (n=1,187), 49% currently smoked (n=1,493), 20% had received a diagnosis of a mental health disorder (n=611), and 29% reported past-year drug use (n=876).
Of those who had never been incarcerated, 57% were black (n=1,353), 25% were white (n=593), 12% were Hispanic (n=283), 5% identified as “other” race (n=129) and 32% reported an annual income of less than $12,000 (n=726). In this group, 18% had HCV infection (n=419), 27% currently smoked (n=637), 18% had received a prior diagnosis of mental health disorder (n=430), and 17% reported past year drug use (n=385). The majority of PWH had documented control of their HIV infection, including 86.3% with CD4>200 cells/mm3 (87.3% never incarcerated, 85.5% previously incarcerated p=0.196) and 82.2% with undetectable viral load (84.6% never incarcerated, 80.3% previously incarcerated p=0.004). Additional data on participants stratified by HIV status are available in Table 1.
Table 1.
Demographics of participants by HIV and incarceration status
| PWH (N=2,717) | Uninfected (N=2,650) | |||||
|---|---|---|---|---|---|---|
| Never incarceration | Previous incarceration | p-value | Never incarceration | Previous incarceration | p-value | |
| Total Population | 1224 (45.0%) | 1493 (55.0%) | 1134 (42.8%) | 1516 (57.2%) | ||
| Age (mean, 95% CI) | 55.6 (55.0–56.2) | 56.2 (57.8–56.6) | 0.10 | 58.3 (57.7–59.0) | 56.2 (55.8–56.6) | <0.001 |
| Race | <0.001 | <0.001 | ||||
| White | 314 (25.7%) | 194 (13.0%) | 279 (24.6%) | 241 (15.9%) | ||
| Black | 708 (57.8%) | 1099 (73.6%) | 645 (56.9%) | 1074 (70.8%) | ||
| Hispanic | 136 (11.1%) | 117 (7.8%) | 147 (13.0%) | 127 (8.4%) | ||
| Other | 66 (5.4%) | 83 (5.6%) | 63 (5.6%) | 74 (4.9%) | ||
| Gender | 0.004 | <0.001 | ||||
| Male | 1180 (96.4%) | 1464 (98.2%) | 998 (88.1%) | 1461 (96.6%) | ||
| Female | 44 (3.6%) | 27 (1.8%) | 135 (11.9%) | 52 (3.4%) | ||
| Income | <0.001 | <0.001 | ||||
| <$12,000K | 391 (32.6%) | 739 (51.4%) | 335 (30.9%) | 758 (51.4%) | ||
| $12,000–24,900 | 338 (28.2%) | 357 (24.9%) | 281 (25.9%) | 367 (24.9%) | ||
| >$25,000 | 470 (39.2%) | 340 (23.7%) | 469 (43.2%) | 350 (23.7%) | ||
| Education | <0.001 | <0.001 | ||||
| Less than HS | 44 (3.6%) | 107 (7.3%) | 54 (4.8%%) | 98 (6.6%) | ||
| HS or GED | 313 (25.8%) | 503 (34.1%) | 323 (28.8%) | 578 (38.8%) | ||
| Some College | 535 (44.0%) | 679 (46.0%) | 523 (46.7%) | 663 (44.5%) | ||
| College grad + | 323 (26.6%) | 186 (12.6%) | 220 (19.6%) | 152 (10.2%) | ||
| Employment | <0.001 | <0.001 | ||||
| Not employed for wages | 825 (67.4%) | 1,146 (76.7%) | 764 (67.4%) | 1,175 (77.5%) | ||
| Employed for wages | 399 (32.6%) | 347 (23.2%) | 370 (32.6%) | 340 (22.5%) | ||
| Social Support | 0.001 | 0.21 | ||||
| 0 | 100 (8.2%) | 182 (12.3%) | 92 (8.2%) | 143 (9.6%) | ||
| 1+ | 1116 (91.8%) | 1298 (87.7%) | 1035 (91.8%) | 1350 (90.4%) | ||
| HCV status | <0.001 | <0.001 | ||||
| HCV positive | 269 (22.8%) | 676 (47.2%) | 150 (13.6%) | 511 (35.3%) | ||
| FIB-4 Score | 0.003 | 0.17 | ||||
| Advanced fibrosis | 115 (9.7%) | 195 (13.5%) | 57 (5.3%) | 94 (6.6%) | ||
| Smoking status | <0.001 | <0.001 | ||||
| Never | 496 (40.8%) | 270 (18.2%) | 416 (36.8%) | 254 (16.8%) | ||
| Former | 396 (32.5%) | 509 (34.32%) | 402 (35.6%) | 470 (31.2%) | ||
| Current | 325 (26.7%) | 708 (47.6%) | 312 (27.6%) | 785 (52.0%) | ||
| Past year drug use | 211 (17.2%) | 434 (29.1%) | <0.001 | 174 (15.4%) | 442 (29.2%) | <0.001 |
| Past year unhealthy alcohol use | 278 (22.8%) | 428 (28.7%) | 0.001 | 260 (23.2%) | 490 (32.4%) | <0.001 |
| Ever homeless | 327 (26.9%) | 823 (56.1%) | <0.001 | 361 (32.1%) | 1007 (67.2%) | <0.001 |
| Mental Health Diagnosis | 178 (14.5%) | 299 (20.0%) | <0.001 | 252 (22.2%) | 312 (20.6%) | 0.30 |
PWH = people with HIV
HCV=hepatitis C virus
HS= high school
GED= general education development
Mortality by Incarceration Among PWH
There were 465 deaths in the PWH cohort, including 182 among those never incarcerated (mean follow time 5.5 years) and 283 among those with prior incarceration (mean follow time 5.3 years). Mortality rates were 2.7 per 100 pys for those never incarcerated vs. 3.6 for those ever incarcerated (p= 0.003) (Table 2).
Table 2.
Unadjusted mortality rates and [95% confidence interval] by Incarceration Measures (per 100 Person Years) and HIV status
| Outcome | PWH | Uninfected |
|---|---|---|
| Incarcerated | ||
| Never | 2.7 [2.3–3.1] | 2.5 [2.1–2.9] |
| Ever | 3.6 [3.2–4.0] | 2.5 [2.2–2.9] |
| Frequency Incarcerated | ||
| Never | 2.7 [2.3–3.1] | 2.4 [2.1–2.9] |
| 1 time | 3.1 [2.4–3.9] | 2.2 [1.7–3.0] |
| 2–5 times | 3.6 [3.1–4.2] | 2.6 [2.2–3.2] |
| 6+ times | 4.1 [3.2–5.3] | 2.9 [2.2–3.9] |
| Time Spent Incarcerated | ||
| Never | 2.7 [2.3–3.1] | 2.4 [2.1–2.9] |
| < 1 month | 2.8 [2.3–3.6] | 2.2 [1.7–2.9] |
| 1 month – 1 year | 3.5 [2.8–4.4] | 2.5 [1.9–3.2] |
| 1–5 years | 4.2 [3.4–5.2] | 2.9 [2.2–3.7] |
| > 5 years | 4.2 [3.1–5.8] | 2.6 [1.8–3.8] |
As shown in Table 3, PWH with prior incarceration experienced higher risk of death compared to those with no prior incarceration, after adjustment for age, race, and gender (AHR 1.37, 95% CI 1.13–1.66, p=.001). Increasing number of times incarcerated, with referent group of those never incarcerated, was associated in a dose-response pattern with mortality (AHRs 1.13, 95% CI 0.86–1.49, 1.45, 95% CI 1.16–1.82, and 1.64, 95% CI 1.21–2.21 for 1, 2–5; 6+ times, respectively (Figure 1). Increasing length of time incarcerated, again with the referent group never incarcerated, was also associated with mortality (AHRs 1.11; 95% CI 0.85–1.45, 1.45; 95% CI 1.10–1.92, 1.65; 95% CI 1.26–2.15, and 1.57; 95% CI 1.10–2.24 for <1 month, 1 to 11 months, 1–5 years, and >5 years, respectively (Figure 1)). There was a significant linear trend between both number of times incarcerated and length of time incarcerated with mortality (all p<.001).
Table 3:
Mortality hazard ratios adjusted for age, race and gender among veterans with and without HIV
| Outcome | PWH AHR [95% CI] | Uninfected participants AHR [95% CI] |
|---|---|---|
| Ever incarcerated | 1.37 [1.13–1.66] | 1.24 [0.99–1.54] |
| Age | 1.07 [1.06–1.08] | 1.06 [1.05–1.07] |
| Gender (male=ref) | 0.60 [0.27–1.35] | 0.52 [0.28–0.96] |
| Black race (all other=ref) | 1.29 [1.05–1.58] | 0.99 [0.80–1.25] |
Figure 1.
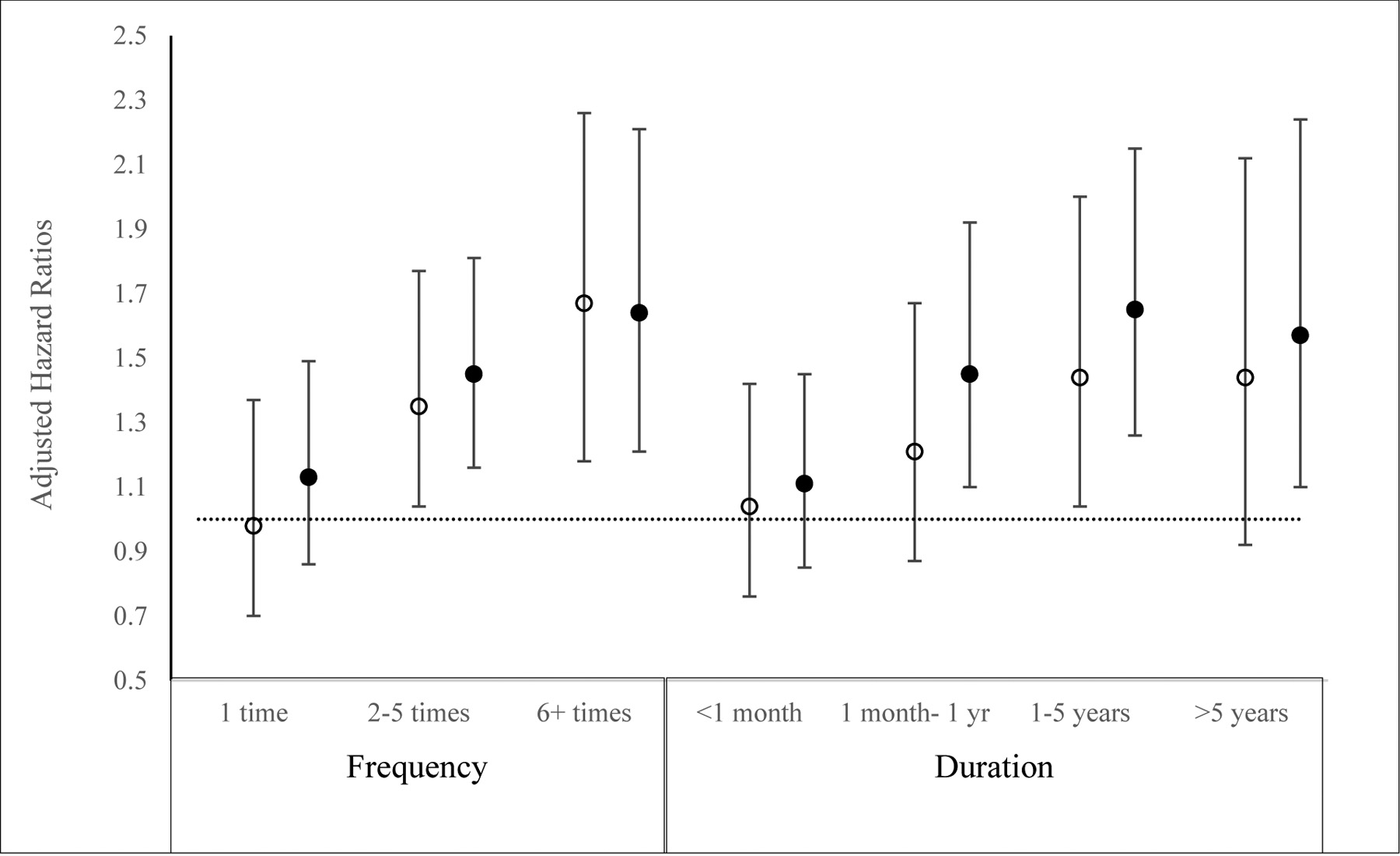
Association between frequency of incarceration and lifetime cumulative duration of incarceration and mortality among participants with and without HIV, adjusted for age, race, and gender
○ Uninfected
● People with HIV
In evaluating Pathway A of the mediation analysis, a univariate analysis found a statistically significant association between incarceration and all potential mediators: education (odds ratio (OR) 0.59; p<0.001), social support (OR 0.64 p=0.001), homelessness (OR 3.37 p<0.001), unhealthy alcohol use (OR 1.64 p<0.001), current smoking (OR 2.49 p<0.001), past year drug use (OR 1.97 p<0.001), mental health disorder (OR 1.73 p<0.001), HCV (OR 2.94 p<0.001), advanced liver fibrosis (OR 1.45 p=0.003), and detectable viral load (OR 1.43 p=0.001). An evaluation of Pathway B found that all potential mediators except unhealthy alcohol use, homelessness, and mental health disorder were associated with mortality. Of the remaining potential mediators, the final mediation analysis (Pathway C) found that HCV was the only complete mediator, meaning it significantly predicted mortality (AHR 1.79 p<0.001) while attenuating the association between incarceration and mortality (AHR 1.14 p=0.19). Education, social support, current smoking, past year drug use, advanced fibrosis, and a detectable viral load were all found to be partial mediators, meaning they significantly predicted mortality while controlling for incarceration, and partially attenuated the association between incarceration and mortality to varying degree (Table 4).
Table 4:
Mediation analysis for potential covariates along the causal pathway between incarceration and mortality among PWH
| Variable | Pathway A* OR, p-value | Pathway B** HR, p-value | Pathway C*** AHR, p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Ever incarcerated | -- | -- | 1.26 p=0.014 | 1.30 p=0.006 | 1.23 p=0.032 | 1.27 p=0.013 | 1.14 p=0.182 | 1.24 p=0.023 |
1.30 p=0.007 |
| Education | 0.59 p<0.001 | 0.68 p<0.001 | 0.70 p<0.001 | -- | -- | -- | -- | -- | -- |
| Social support | 0.64 p=0.001 | 0.68 p=0.003 | -- | 0.70 p=0.005 | -- | -- | -- | -- | -- |
| Homeless | 3.37 p<0.001 | 1.11 p=0.27 | -- | -- | -- | -- | -- | -- | -- |
| Past year unhealthy alcohol use**** | 1.64 p<0.001 | 1.23 p=0.095 | -- | -- | -- | -- | -- | -- | -- |
| Current smoking | 2.49 p<0.001 | 1.43 p<0.001 | -- | -- | 1.37 p=0.001 | -- | -- | -- | -- |
| Past year drug use | 1.97 p<0.001 | 1.37 p=0.002 | -- | -- | -- | 1.32 p=0.009 | -- | -- | -- |
| Mental health disorder | 1.73 p<0.001 | 1.06 p=0.504 | -- | -- | -- | -- | -- | -- | -- |
| HCV status | 2.94 p<0.001 | 1.85 p<0.001 | -- | -- | -- | -- | 1.79 p<0.001 | -- | -- |
| Advanced fibrosis | 1.45 p=0.003 | 3.19 p<0.001 | -- | -- | -- | -- | -- | 3.12 p<0.001 | -- |
| Detectable viral load | 1.43 p=0.001 | 1.34 p=0.016 | -- | -- | -- | -- | -- | 1.30 p=0.029 | |
Pathway A: Univariate association between covariate and incarceration using logistic regression models
Pathway B: Univariate association between covariate and mortality using Cox proportional hazard models
Pathway C: Association of covariate with mortality, adjusting for incarceration, using multivariate Cox proportional hazard models
Referent group participants who reported alcohol use without unhealthy use (ie those reporting no alcohol use not included).
PWH = people with HIV
HCV = hepatitis C virus
Mortality by Incarceration Among Uninfected Participants
There were 356 deaths among uninfected participants, including 157 deaths among those never incarcerated (mean follow time 5.7 years) and 199 deaths among those incarcerated (mean follow time 5.1 years). The unadjusted mortality rate was 2.5 per 100 pys for both those who had and had not been previously incarcerated (p=0.8) (Table 2).
In the uninfected cohort, there was no statistically significant association between incarceration and mortality compared to those never incarcerated after adjustment for age, race, and demographics (AHR 1.24; 95% CI 0.99–1.55; p=0.059). However, in these adjusted models, increasing number of times incarcerated was associated with mortality in a dose-dependent manner (AHRs 0.98; 95% CI 0.70–1.37; 1.35; 95% CI 1.04–1.77, and 1.67; 95% CI 1.18–2.26 for 1, 2–5; 6+ times, respectively; p=0.009 (Figure 1)). Additionally, mortality increased with increasing length of time incarcerated (AHR 1.04; 95% CI 0.76–1.42, 1.21; 95% CI 0.87–1.67. 1.44; 95% CI 1.04–2.00, and 1.44; 95% CI 0.93–2.12 for <1 month (Figure 1), 1 to 11 months, 1–5 years, and >5 years, respectively). There was a significant linear trend between both number of times incarcerated and length of time incarcerated with mortality (all p<.015).
Discussion
In this large multi-cohort site study of veterans, mortality after exposure to incarceration was higher among PWH when compared to never-incarcerated PWH. Moreover, increasing frequency of incarceration and lifetime spent incarcerated were associated with increased risk of mortality. While HIV has been previously established as a leading cause of death among justice-involved individuals, this finding is novel and suggests that incarceration may be associated with mortality among PWH, and that PWH may be particularly impacted by repeated incarceration.
An important finding in this study is the dose-response relationship between incarceration and mortality. Increasing exposure to incarceration (both frequency and total length of time spent incarcerated) was associated with increased mortality for those with and without HIV in models adjusting for demographics. Increased frequency of incarceration may subject criminal justice-involved persons to destabilized social networks and healthcare, while increased time spent incarcerated may increase exposure to the intrinsic harms of incarceration, including solitary confinement, or decreased employment, educational, and social opportunity after release. These findings contribute to the small amount of literature suggesting that increasing exposure to incarceration may increase risk of mortality and that legislation to eliminate frequent reincarceration for minor infractions and mandatory minimum sentencing for drug crimes may produce important health promoting benefits.18
We found that HCV functioned as a complete mediator between incarceration exposure and mortality among PWH. HCV may be a surrogate marker of liver disease and liver cancer, which is consistent with our findings of the partial mediating effect of advanced fibrosis, and have been shown in other studies to be a cause of death among individuals with a history of incarceration,3,19 though it may also be acting in other mechanisms.20–22 Justice-involved individuals experience increased barriers to HCV treatment, which exposes them to higher risk of liver disease.23 This finding is important given the high prevalence of HCV among those with incarceration histories (41% in our study) and the recent improvements in highly effective direct-acting antiviral therapy. Programs to screen for and treat HCV focused in correctional settings may curb the high rates of mortality in this population.
We also found that smoking and drug use also function as partial mediators of mortality among PWH. A high proportion of our sample, especially those with prior incarceration, reported current smoking. Smoking may be disproportionately hazardous to PWH24. While most prisons and jails are smoke-free, return to smoking after release is high25. Correctional system-based interventions to encourage continued cessation after release are sparse, though limited research suggests they may be effective24,25. Expansion of such programs could have an impact on reducing the morbidity and mortality of smoking in this population and more research is necessary. Multiple studies have found an increased risk of overdose death after incarceration; additionally, PWH experience a particularly high risk of overdose compared with uninfected peers.26 Persons who use opioids and are incarcerated should have access to evidence-based treatment with medications for opioid use disorder (e.g., buprenorphine/naloxone, methadone, injectable naltrexone) during incarceration and upon release, along with increased provision of the overdose reversal drug naloxone27–29.
Unsuppressed viral load was associated with higher risk of mortality among PWH, supporting previous findings that interruption of antiretroviral therapy after release from incarceration likely drives worse health outcomes, including mortality.5,30,31 Few interventions have successfully prevented declines in viral suppression after release from incarceration,32 though a recent randomized controlled trial did find that peer navigation following release from jail among PWH successfully prevented declines in viral suppression. Authors speculated that integration of peers into HIV care underpinned success of this intervention.
Unlike previous literature, our results did not show a statistically significant unadjusted increased risk of mortality for those incarcerated who do not have HIV infection. There are several potential explanations for this phenomenon. First, the results may reflect a diminished effect when formerly incarcerated PWH are removed from the population, since HIV has been shown to contribute to excess mortality in multiple studies, as detailed above. Secondly, veterans may experience the health associations of incarceration differently than the general population, especially those engaged in care. One study among veterans in Washington state suggested that having access to veterans benefits may provide a protective effect.33 This association is not fully understood, and further research is indicated.
Limitations
There are several limitations to this study. As with all observational studies, we cannot establish causality to observed associations. It is not possible to know if certain covariates, such as homelessness and mental health conditions, were established prior to or after incarceration. It is likely the vast majority of incarceration events occurred after active duty, because having a prior felony or misdemeanor conviction makes it very difficult to enlist in the military. We did not include marijuana use as the health effects of marijuana are significantly lower than other substances examined34. Receipt of treatment for many covariates, including mental health conditions, may reveal additional modifying effects on the association with incarceration and mortality; these data could not be reliably captured using the data set and therefore were not included in the analyses. Additional incarceration events experienced after the survey, but prior to the end of the study period, will not be captured and so the unexposed group may include some participants with incarceration experience, though this would result in an underestimate of the effects of incarceration. Incarceration exposure relies on self-reported data though prior studies have shown that this is more accurate than state prison or other administrative claims data.35 Cause of death information would be particularly valuable in understanding the mediating influence of HCV and advanced liver fibrosis on mortality, however these data were not captured for this analysis. Future studies examining cause of death would provide valuable information about this vulnerable population. Notwithstanding these limitations, the strengths of this study, with national sampling and robust survey, administrative, and clinical data sources, provide an important contribution to our understanding of incarceration and the associated risk of mortality, especially among those with HIV infection.
Conclusion
In PWH, any incarceration history is associated with increased risk of death, and increasing frequency of incarceration is associated increased risk of mortality in both those with and without HIV. PWH and a history of incarceration are at high risk for death, which may justify application of additional resources to assist this vulnerable population. The role of viral suppression among PWH, smoking and drug use, and HCV as potential modifiable mediators warrants future investigations and may have implications for expansions of treatment in this population. Finally, reconsideration of policies such as crimeless revocation and mandatory minimum sentences could reduce individuals’ exposure to incarceration and therefore may reduce mortality risk.
Acknowledgement
Dr. Hawks received funding support from an Institutional National Research Service Award from T32HP32715, and by the Cambridge Health Alliance. The work reported here was supported by COMpAAAS/Veterans Aging Cohort Study, a CHAART Cooperative Agreement, is supported by the National Institutes of Health: National Institute on Alcohol Abuse and Alcoholism (U24-AA020794 (PI: A Justice), U01-AA020790 (PI: A Justice), U24-AA022001 (PI: A Justice), U10 AA013566-completed (PI: A Justice)) and in kind by the US Department of Veterans Affairs, VHA Public Health Strategic Health Care Group. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Spaulding AC, Seals RM, McCallum VA, Perez SD, Brzozowski AK, Steenland NK. Prisoner survival inside and outside of the institution: implications for health-care planning. Am J Epidemiol. 2011;173(5):479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosen DL, Schoenbach VJ, Wohl DA. All-cause and cause-specific mortality among men released from state prison, 1980–2005. Am J Public Health. 2008;98(12):2278–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maruschak LM. HIV in prisons, 2001–2010. Bureau of Justice Statistics. 2012;20(25.10):1–11. [Google Scholar]
- 5.Wang EA, McGinnis KA, Long JB, et al. Incarceration and health outcomes in HIV-infected patients: the impact of substance use, primary care engagement, and antiretroviral adherence. Am J Addict. 2015;24(2):178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760. [DOI] [PubMed] [Google Scholar]
- 7.Levanon Seligson A, Parvez FM, Lim S, et al. Public Health and Vulnerable Populations: Morbidity and Mortality Among People Ever Incarcerated in New York City Jails, 2001 to 2005. J Correct Health Care. 2017;23(4):421–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loeliger KB, Altice FL, Ciarleglio MM, et al. All-cause mortality among people with HIV released from an integrated system of jails and prisons in Connecticut, USA, 2007–14: a retrospective observational cohort study. Lancet HIV. 2018;5(11):e617–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nasrullah M, Frazier E, Fagan J, Hardnett F, Skarbinski J. The association of recent incarceration and health outcomes among HIV-infected adults receiving care in the United States. Int J Prison Health. 2016;12(3):135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patterson EJ. The dose-response of time served in prison on mortality: New York State, 1989–2003. Am J Public Health. 2013;103(3):523–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Justice AC, Dombrowski E, Conigliaro J, et al. Veterans Aging Cohort Study (VACS): Overview and description. Med Care. 2006;44(8 Suppl 2):S13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS medicine. 2010;7(7):e1000316–e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 14.McGinnis KA, Justice AC, Kraemer KL, Saitz R, Bryant KJ, Fiellin DA. Comparing alcohol screening measures among HIV‐infected and‐uninfected men. Alcohol Clin Exp Res. 2013;37(3):435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tate JP, Justice AC, Hughes MD, et al. An internationally generalizable risk index for mortality after one year of antiretroviral therapy. AIDS (London, England). 2013;27(4):563–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–1325. [DOI] [PubMed] [Google Scholar]
- 17.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. [DOI] [PubMed] [Google Scholar]
- 18.Schiraldi VN. Too big to succeed: The impact of the growth of community corrections and what should be done about it. 2018.
- 19.Spaulding AC, Allen SA, Stone A. Mortality after release from prison. N Engl J Med. 2007;356(17):1785; author reply 1786–1787. [DOI] [PubMed] [Google Scholar]
- 20.Thornton AC, Jose S, Bhagani S, et al. Hepatitis B, hepatitis C, and mortality among HIV-positive individuals. AIDS. 2017;31(18):2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alejos B, Hernando V, Iribarren J, et al. Overall and cause-specific excess mortality in HIV-positive persons compared with the general population: Role of HCV coinfection. Medicine (Baltimore). 2016;95(36). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dold L, Ahlenstiel G, Althausen E, et al. Survival and HLA-B* 57 in HIV/HCV co-infected patients on Highly Active Antiretroviral Therapy (HAART). PLoS One 2015;10(8):e0134158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hochstatter KR, Stockman LJ, Holzmacher R, et al. The continuum of hepatitis C care for criminal justice involved adults in the DAA era: a retrospective cohort study demonstrating limited treatment uptake and inconsistent linkage to community-based care. Health & justice. 2017;5(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Helleberg M, May MT, Ingle SM, et al. Smoking and life expectancy among HIV-infected individuals on antiretroviral therapy in Europe and North America. AIDS. 2015;29(2):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Andrade D, Kinner SA. Systematic review of health and behavioural outcomes of smoking cessation interventions in prisons. Tob Control. 2017;26(5):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Green TC, McGowan SK, Yokell MA, Pouget ER, Rich JD. HIV infection and risk of overdose: a systematic review and meta-analysis. AIDS. 2012;26(4):403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brinkley-Rubinstein L, Cloud DH, Davis C, et al. Addressing excess risk of overdose among recently incarcerated people in the USA: harm reduction interventions in correctional settings. Int J Prison Health 2017;13(1):25–31. [DOI] [PubMed] [Google Scholar]
- 28.Rich JD, McKenzie M, Larney S, et al. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet. 2015;386(9991):350–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Springer SA, Di Paola A, Azar MM, et al. Extended-release naltrexone improves viral suppression among incarcerated persons living with HIV with opioid use disorders transitioning to the community: results of a double-blind, placebo-controlled randomized trial. Jaids Journal of Acquired Immune Deficiency Syndromes. 2018;78(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stephenson BL, Wohl DA, Golin CE, Tien H- C, Stewart P, Kaplan AH. Effect of Release from Prison and Re-Incarceration on the Viral Loads of HIV-Infected Individuals. Public Health Rep 2005;120(1):84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wohl DA, Golin CE, Knight K, et al. A randomized controlled trial of an intervention to maintain suppression of HIV viremia following prison release: The imPACT trial. J AIDS. 2017;75(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wortzel HS, Blatchford P, Conner L, Adler LE, Binswanger IA. Risk of death for veterans on release from prison. J Am Acad Psychiatry Law. 2012;40(3):348–354. [PMC free article] [PubMed] [Google Scholar]
- 34.Hall W, Room R, Bondy S. A comparative appraisal of the health and psychological consequences of alcohol, cannabis, nicotine and opiate use. Addiction Research Foundation; 1994. [Google Scholar]
- 35.Wang EA, Long JB, McGinnis KA, et al. Measuring Exposure to Incarceration Using the Electronic Health Record. Med Care. 2019;57:S157–S163. [DOI] [PMC free article] [PubMed] [Google Scholar]


