Abstract
Objective:
Substantial research has accrued in support of a key role for social processes in Substance Use Disorders (SUD). Researchers have developed a range of interventions that capitalize on these social processes to bolster treatment outcomes by involving significant-others (e.g. romantic partners, family, friends) in SUD treatment. Yet dissemination of these treatments to many contexts has been slow, and information on their broad efficacy is lacking. This meta-analysis aims to quantify the effect of significant-other involvement in SUD treatments above and beyond individually-based therapies.
Method:
A total of 4,901 records were screened for randomized controlled trials examining the effect of significant-other involved treatments (SOIT) vs. individually-based active comparator treatments. Our search yielded 77 effect sizes based on data from 2,115 individuals enrolled in 16 independent trials.
Results:
Findings indicated a significant effect of SOIT above and beyond individually-based active comparator treatments for reducing substance use and substance-related problems, d=0.242, 95%CI=0.148–0.336, I2=10.596, Q(15)=16.778. This effect was consistent across SOIT treatment types and endured 12–18 months after the end of treatment. Analyses of raw mean differences indicated that this effect translates to a 5.7% reduction in substance use frequency—the equivalent of approximately 3 fewer weeks a year of drinking/drug use.
Conclusion:
Findings indicate a significant advantage for SOIT in SUD treatment, and hold interesting conceptual implications for theories of SUD maintenance.
Keywords: intervention, substance use disorder, addiction, couples, family
In 1974, in his second special report on alcohol and health to congress, National Institute on Alcohol Abuse and Alcoholism’s inaugural director Morris Chafitz referred to couples and family approaches as among the most notable current advances in psychotherapy (p. 116, Chafez, 1974). In the decades since this report was made, substantial empirical research has accrued to support a key role for social processes in the development and maintenance of Substance Use Disorders (SUD; Epstein & McCrady, 1998; Fairbairn & Sayette, 2014; Leonard & Eiden, 2007), and clinical trials have examined the impact of incorporating romantic partners, family members, and other close ones into SUD treatment, adopting a range of modalities spanning those based in Behavioral Couples Therapy to those taking a family systems approach (McCrady, Epstein, Cook, Jensen, & Hildebrandt, 2009; O’Farrell & Clements, 2012). In light of the considerable body of work that has accrued and the compelling potential conceptual implications of this research, it is critical to assess the broad efficacy of integrating significant-others into SUD treatment—an endeavor that can lead to challenges at the level of both patient and institute/provider. The current meta-analysis seeks to aggregate and organize this body of work, quantifying the effect of significant-other involvement (vs. individually-based active comparator treatments) on SUD outcomes in addiction treatment programs.
Basic Close Relationship Processes and Significant-Other Involved SUD Treatments
Both within and outside the sphere of scientific research, the possibility of conceptual connections between processes underlying addiction and those supporting close relationships has long captured the collective imagination. In popular culture, songs comparing addiction to romantic relationships abound, with longing for interpersonal connection being compared to craving for the next drink so often as to enter the realm of cliché (Peele, 2012). Within scientific communities, researchers have reflected on similar patterns of affective, behavioral, and neurobiological responding to addictive substances as to attachment figures (e.g., caregivers, romantic partners, and other close ones) speculating that, in light of potentially overlapping substrates underlying addiction and attachment, the rewards and stressors associated with close relationships may provide a unique context for understanding both the exacerbation of, and also recovery from, SUD (Burkett & Young, 2012; Fairbairn et al., 2018; Kassel, Wardle, & Roberts, 2007).
While the notion of common underlying substrates for addiction and attachment processes still exist firmly in the realm of speculation, the strong and reciprocal connection between close relationship functioning and substance use is well established. Humans are social beings, and thus human behavior—substance using and otherwise—exists in social context (Baumeister & Leary, 1995). Consistent with this premise, research suggests that close relationship factors predict both the initial onset and the eventual maintenance of substance use (Fairbairn & Sayette, 2014; Leonard & Eiden, 2007). In research with both adult and adolescent populations, insecure attachment relationships with family and romantic partners longitudinally predict substance use (Fairbairn et al., 2018), and the belief that alcohol enhances social interactions emerges as a robust predictor of later alcohol problems (Jones, Corbin, & Fromme, 2002). Among treatment seeking populations, a range of social factors emerge as strong predictors of relapse, including offers to use substances from friends and family (Eddie & Kelly, 2017; Stout, Kelly, Magill, & Pagano, 2012) as well as social stressors and relationship conflict (Knight & Simpson, 1996; Leach & Kranzler, 2013). Indeed, longitudinal research with populations of substance users suggests that, above and beyond the substance users’ own behaviors, social behaviors of their close others longitudinally predict relapse at follow-up (Fairbairn & Cranford, 2016; O’Farrell, Murphy, Neavins, & Van Hutton, 2000).
In tandem with the burgeoning body of basic correlational research pointing to a key role for close relationships in SUD, a growing body of randomized clinical trials has accumulated examining the causal impact of integrating significant-others into SUD treatment. Grounded in research indicating that most individuals with SUD do maintain regular contact with family and other close ones (Stanton & Shadish, 1997), these interventions, which we will refer to here collectively as significant-other involved treatments, feature therapy administered to not only the individual with SUD but also close others. These interventions have diverged along several dimensions: significant-others integrated into treatment have ranged from parents to romantic partners to other family/friends (Dennis et al., 2004; O’Farrell, Murphy, Alter, & Fals-Stewart, 2010), patients targeted have ranged from adolescents to adults (Rigter et al., 2013; Vedel, Emmelkamp, & Schippers, 2008), and treatments have drawn on therapeutic modalities varying from Cognitive Behavioral Therapy (CBT) to family systems-based approaches (Liddle, Rodriguez, Dakof, Kanzki, & Marvel, 2005; McCrady et al., 2016). While varying in certain elements, significant-other involved treatments are also highly similar along a number of domains, including a common focus on improving relationship quality and also leveraging social systems to reduce substance use.
Although significant-other involved SUD treatments have taken a variety of forms, to date the most widely researched intervention types are couples-based approaches, family therapy approaches, and therapies based in the Community Reinforcement Approach. Couples-based approaches for addiction draw on techniques from Behavioral Couples Therapy to simultaneously reduce substance use while also working to enhance relationship quality within intimate partnerships (McCrady et al., 2016; O’Farrell & Clements, 2012). Within such approaches, patients are taught behavioral techniques aimed at reducing substance use and maintaining abstinence goals as well as engaging in relationship-building practices with their partners to improve relationship quality and functioning (McCrady et al., 2016). Similar to couples approaches, family-focused treatments also aim to reduce substance use by altering elements of the family dynamic that directly or indirectly support substance use while simultaneously improving the quality of family relationships. While the majority of these family interventions have been designed to be implemented with adolescent populations (e.g. Boustani, Henderson, & Liddle, 2016), other variants of family interventions specifically target adult populations and recruit parents, siblings, or other close family members into treatment to provide social and structural support for sobriety (O’Farrell et al., 2010). Finally, the Community Reinforcement Approach differs from couples and family-based approaches in that some iterations of this intervention may be implemented without the direct involvement of significant-others (Miller, Meyers, & Hiller-Sturmhofel, 1999). However, significant-other involvement is viewed as an element that enhances treatment and, in applications of the Community Reinforcement Approach that do involve significant-others, treatment focuses on increasing positive interactions, decreasing aversive interactions, and enlisting the significant-other’s support to alter contingencies surrounding substance use (Miller et al., 1999).
Impact and Dissemination of Significant-Other Involved SUD Treatments
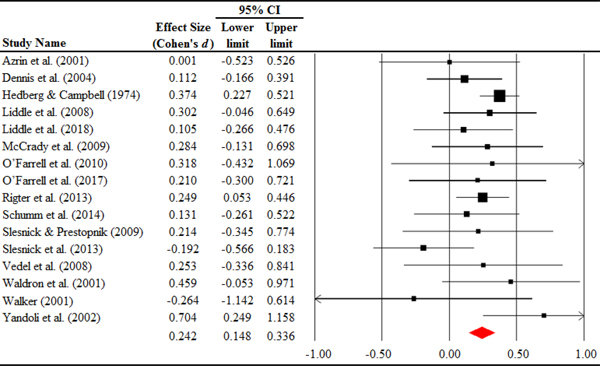
While interest in significant-other involved SUD treatments has been apparent for some time now (Chafez, 1974), attention to these interventions has increased in recent years. This growing interest has been evident within the addiction research community, as well as within some applied clinical settings. For example, the Veteran’s Health Administration recently recognized addictions couples therapy as an empirically based practice, taking important strides towards disseminating couples-based addictions interventions to veterans nationally (O’Farrell et al., 2015). Meanwhile, family therapy approaches, including Multidimensional Family Therapy, have been recognized as empirically supported interventions and disseminated across multiple cites internationally (Rowe et al., 2013; Volkow, 2011). Within the realm of research, there appears to have been a dramatic surge of interest in significant-other involved SUD treatments since the start of the 21st century, with almost double the number of studies published from 2001 to 2018 referencing significant-other involved SUD treatments compared to all of the five proceeding decades (See Figure 1). It’s also worth noting that, in light of potentially intriguing conceptual implications for addiction theory, interest in significant-other involved SUD treatment research has extended well beyond the applied realm. Specifically, in the context of a basic literature that has been constrained to correlational methods for examining links between social factors and addiction (e.g., Fairbairn et al., 2018; Leonard & Eiden, 2007), randomized controlled trials of significant-other involved SUD treatments featuring individual therapy intervention comparison groups are prized in that they offer a rare glimpse of potential causal links.
Figure 1.
Number of studies referencing significant-other involved SUD interventions displayed according to year of publication.
Note. Database search terms used to produce the above results are outlined within the “search strategy” portion of the methods section.
Despite growing interest in significant-other involved SUD treatments, and recent implementation of these therapies in some contexts, the widespread dissemination of these treatments has been markedly slow (McGovern, Fox, Xie, & Drake, 2004). Numerous scientists have remarked that the pace of dissemination for significant-other involved SUD treatments has not kept pace with empirical research, and have called for the increased dissemination of these treatments to applied settings (Copello, Templeton, & Velleman, 2006; Klostermann, Kelley, Mignone, Pusateri, & Wills, 2011; Rowe, 2012). Of note, the implementation of these treatments into the community is not free of obstacles, and such approaches may involve burden for not only therapists but also patients and their significant-others (Clark, 2002). For example, regarding therapists, conducting sessions with SUD patients and significant-others simultaneously can present providers with new challenges—especially given the level of close relationship distress commonly associated with SUD—and preparing to deliver such treatments effectively may require months of didactics and supervision (Liddle et al., 2006). These interventions may also present challenges for patients, including those associated with scheduling appointments at mutually convenient times and, in couples/families involving small children, identifying reliable childcare (Kazdin, Holland, & Crowley, 1997; Mensinger, Diamond, Kaminer, & Wintersteen, 2006). Lastly, research indicates that some women may be more likely to opt into individual treatment over couples therapy due to various factors, including personal preferences and concern over partner support (McCrady, Epstein, Cook, Jensen, & Ladd, 2011).
In light of widespread interest in significant-other involved SUD treatments, as well as the potential challenges associated with such approaches, it becomes especially important to gain a more precise sense of the efficacy of these interventions. In particular, an exact quantification of the effect for significant-other involved SUD treatment—above and beyond individually-based treatments—could help providers and also patients make informed decisions about the incremental utility of implementing such interventions across individual contexts and cases. In addition, such comparisons, conducted within the context of randomized trials, can also carry intriguing (albeit broad) conceptual implications for understanding the general role of close relationship processes in the maintenance of SUD, and thus might ultimately inform addiction theory.
Reviewing Significant-Other Involved SUD Treatments
Over two decades ago, Stanton and Shadish (1997) conducted a meta-analysis examining the efficacy of significant-other involved SUD treatments, spanning across modalities ranging from couples treatment approaches to various family-based therapies. This review included an analysis of effects from 6 randomized trials comparing the efficacy of significant-other involved treatments to individually-based treatment as usual. Importantly, however, since the time of this review’s publication, multiple large-scale trials have been published comparing significant-other involved SUD treatments with “strong” active comparator treatments, increasing the size of this literature by a factor of several fold (Dennis et al., 2004; McCrady et al., 2009; Rigter et al., 2013). Also over the course of the past two decades, serious questions have been raised about the research of scientist William Fals-Stewart1—a prolific author whose work was not only represented within Stanton and Shadish’s original meta-analysis, but has also been included in more recent reviews targeting specific sub-domains of significant-other involved treatments (e.g., Fals-Stewart’s work represented approximately 50% of studies included in Powers, Vedel, & Emmelkamp, 2008 meta-analysis of Behavioral Couples Therapy). In sum, in light of the burgeoning size of the empirical literature, along with grave questions raised about some prior research, it is high time for an updated meta-analysis that quantifies the broad efficacy of significant-other involved SUD treatments.
In addition to its utility in providing an overall quantification of effect sizes across samples, an updated meta-analysis might have utility for exploring the consistency vs. variability of effects across various characteristics of study populations and treatment approaches (i.e., moderators of treatment efficacy). In particular, while there are commonalities in mechanisms targeted across family therapies, community reinforcement approaches, and couples-based treatments, there are also different change processes engaged in some of these treatments that may yield differential outcomes (Rowe, 2012). Furthermore, given the strain that heavy substance use can put on close relationships, researchers have called for studies examining whether substance use severity at baseline is likely to differentially affect treatment outcomes (McCrady et al., 2016). Other factors of potential interest as moderators of treatment efficacy include type of substance used (e.g., alcohol vs. drugs), relationship to significant-other integrated in treatment (e.g., parent vs. romantic partner), and age group of population targeted (Kraemer, Frank, & Kupfer, 2006).
The Current Review
In sum, within both clinical and research communities, there has been substantial enthusiasm for SUD treatments that involve significant-others. At the same time researchers have noted challenges that can accompany the implementation of these approaches. A review quantifying the broad efficacy of these approaches would help establish the extent to which they produce meaningful changes in substance use and thereby potentially clarify the utility of these approaches and facilitate dissemination. Here we present a meta-analysis of the effect of significant-other involved treatments for individuals with SUD. Note that, in the current review, we chose to target studies comparing significant-other involved treatments with individually-based active comparator treatments. For the purposes of this review, individually-based active comparator treatments are operationalized broadly as active therapy (e.g., evidence-based therapies, treatment as usual/usual care) delivered primarily in a one-on-one setting. This comparison condition was selected as that most likely to be useful to providers seeking to make informed decisions surrounding implementation (i.e., the incremental utility of significant-other involved approaches above and beyond a form of intervention commonly implemented across SUD treatment settings). We also chose this contrast, which permits the isolation of the effect of significant-other involvement, as one with potentially interesting conceptual implications for addiction theory seeking to elucidate the broad role of social factors in the maintenance of SUD.
The primary aim of this review is to quantify the overall effect of significant-other involved treatments for individuals with SUD, examining whether there exists a statistically significant effect of these treatments above and beyond individually-focused usual care. A secondary aim is to examine various potential moderators of this effect, including type of SUD treatment, baseline substance use severity, age and gender of the target population, relationship to significant-other involved, type of substance used, and type of substance use outcome measured.
Methods
Search Strategy
The following strategies were used to search for relevant studies: a) The following database keywords were entered: (“couple* therap*” OR “couple* intervention*” OR “couple* treatment*” OR “conjoint therap*” OR “conjoint intervention*” OR “conjoint treatment*” OR “marital therap*” OR “marital intervention*” OR “marital treatment*” OR “family therap*” OR “family intervention*” OR “family treatment*” OR “community reinforcement”) AND (“alcohol” OR “drinking” OR “substance*” OR “addiction” OR “drug*” OR “marijuana” OR “cannabi*” OR “smoking” OR “tobacco” OR “nicotine” OR “cocaine” OR “opioid*” OR “opiate*” OR “heroin” OR “illicit” OR “amphetamine*” OR “benzodiazepine*” OR “prescription drug*” OR “hallucinogen*”). The database searched was PsycINFO. An asterisk (*) was added next to the search terms to capture all variations in the ending of the words (for instance therapy or therapies). Search terms were allowed to appear anywhere in the abstract, all subject and indexing, document title, or publication title; b) once a study was identified as meeting inclusion criteria, the reference lists of each eligible study was scanned for other potential candidate studies; c) the reference sections of nine reviews published in the literature on the topic of significant-other involved SUD treatments were scanned for eligible studies (Baldwin, Christian, Berkeljon, & Shadish, 2012; Boustani et al., 2016; Filges, Andersen, & Jørgensen, 2015; O’Farrell & Clements, 2012; O’Farrell & Fals-Stewart, 2003; Powers et al., 2008; Rowe, 2012; Stanton & Shadish, 1997; Tanner-Smith, Wilson, & Lipsey, 2013). The search included studies published prior to January 2019. Together, these search methods yielded a total of 4,901 abstracts, all of which were scanned for potential inclusion in this review.
Inclusion Criteria
Study characteristics.
Our search aimed to target studies that compared significant-other involved SUD treatments (SOIT) with individually-based active comparator treatments. Studies were required to include at least one behavioral treatment that integrated significant-others (defined as partners, caregivers, or other significant-others such as siblings, or close friends) and at least one individually-based active treatment comparison condition. Random assignment to treatment conditions was required. Therapies had to have a clear face-to-face therapy format to be considered eligible (e.g., text or phone-based treatments were excluded). Studies that recruited adolescents where parents were only peripherally involved in the individually-based active comparator treatments (e.g. took part in the assessment or in one psycho-education session) were considered eligible. Comparator treatments were not required to be time-matched for inclusion in this review (note that any discrepancies in treatment length between SOIT and comparator treatments were documented—see below section on data extraction). In order to isolate the effect of social processes associated with close social relationships/attachment relationships, and avoid confounds, we excluded studies featuring group-based (i.e., not individual) treatments, since social processes (e.g., the formation of new social bonds) may emerge in the context of group therapy (Weiss, Jaffee, de Menil, & Cogley, 2004).2 We also excluded treatment modalities where significant-others individually sought treatment with the aim of engaging and motivating the diagnosed individual to start treatment, but the patient him/herself was not involved (e.g. Community Reinforcement and Family Therapy). Lastly, due to serious questions raised about the work of William Fals-Stewart (see above), studies that listed Fals-Stewart as a lead author or a grant receiver on the project were also excluded.
Participant characteristics.
Studies were required to recruit individuals with SUD, defined as individuals identified as meeting specific criteria for use disorders as outlined by the Diagnostic and Statistical Manual of Mental Disorders (DSM; e.g., American Psychiatric Association, 2013) and/or as being identified by study authors as individuals seeking treatment for alcohol or other substance use. Studies were excluded if they recruited non-clinical samples (e.g., heavy drinkers, social drinkers, juvenile offenders not identified as having SUD). Further, studies were excluded if they exclusively recruited a substance using population that presented with co-morbid psychotic disorders (i.e., schizophrenia-related disorders), since the focus of treatment in these studies was often not on SUD. No age or gender restrictions were placed on participants.
Outcome characteristics.
Studies were required to include at least one measure of substance use (e.g., quantity, frequency, abstinence) or substance-related problems measured at post-treatment (at the end of treatment) and/or follow-up (N months after the end of treatment).
Data Extraction
All study characteristics and effect sizes were coded by both the first author as well as a research assistant. The following characteristics of studies were coded: (a) sample size; (b) average age of participants at study initiation; (c) gender composition of participants; (d) type of substance used (alcohol, drug, or combined alcohol and drug use); (e) type of SOIT—categories included couple-focused treatments (e.g. Behavioral Couples Therapy), family-focused treatments (e.g. Multidimensional Family Therapy, Functional Family Therapy, Ecologically Based Family Therapy, or other-SOIT approaches) and Community Reinforcement Approach; (f) individually-based active comparator treatment type (e.g., CBT, MET, 12-Step, and “other” individual treatment approaches)3; (g) type of substance use outcome measure assessed (abstinence, use frequency, use quantity, substance-related problems, and “other use measure”)4; (h) drinking severity at baseline (evaluated as the average percent days spent using and/or drinking); (i) relationship to significant-other involved (e.g. partner, caregiver, or “other” which capture studies that involve a mix of individuals such as parents, siblings, children, and/or partners); (j) treatment length difference (computed as the total number of sessions required for SOIT subtracted from the total number of sessions for individually-based active comparator). Effect sizes were coded as Cohen’s d coefficients by both the first author and a research assistant. All effect sizes were coded such that positive effect sizes indicate that the findings favor SOIT over individually-based active comparator treatments, whereas negative effect sizes indicate that the findings favor individually-based active comparator treatments over SOIT. If a report did not include sufficient information for the calculation of treatment effect sizes for at least one substance use outcome, authors were contacted directly. Nine different authors were contacted, three of whom communicated the requested information (Dennis et al., 2004; Liddle, Dakof, Turner, Henderson, & Greenbaum, 2008; Slesnick, Erdem, Bartle-Haring, & Brigham, 2013), two authors mentioned that they no longer have access to the original data (Kalman, Longabaugh, Clifford, Beattie, & Maisto, 2000; McCrady et al., 1986; McCrady, Stout, Noel, Abrams, & Nelson, 1991). In the case of one study, the author did not respond to our request and we had insufficient data to calculate an effect size (Nattala, Leung, Nagarajaiah, & Murthy, 2010).
The study and effect size calculations of the two coders were compared, and any discrepancies were resolved through discussion until agreement was reached. The average intraclass correlation (ICC) between the coders was 1.00 for both variables coded on a continuous scale (age, gender proportion) as well as for the effect size calculations. Cohen’s kappa between the two coders was κ=0.97 for categorical variables.
Study Quality Assessment
We used the “Risk of Bias Assessment Tool” developed by the Cochrane Collaboration to assess the quality of the eligible studies (Higgins et al., 2011). Five domains were evaluated by two research assistants to determine the risk of bias for each eligible study: “random sequence generation,” “allocation concealment,” “incomplete outcome data,” “blinding on outcome assessment,” and “selective outcome reporting” (see Higgins et al., 2011 for details of the assessment). Of note, we did not include an assessment of the domain of “blinding of participants and personnel” in the current risk of bias assessment. This is because blinding clients and treatment providers to the kind of intervention delivered is not possible in psychotherapeutic treatments (Munder & Barth, 2018). The risk of bias for each domain was rated as either low, unclear, or high based on the criteria specified in the assessment tool. Subsequently, the overall level of risk of bias for each study was determined based on the following ratings of the five domains: a) low risk of bias if all five domains were assessed as having low risk of bias; b) unclear risk of bias if at least one of the five domains was assessed as having an unclear risk of bias and none presented with a high risk of bias; and c) high risk of bias if at least one domain was assessed as having a high risk of bias (see Table 1 for overall level of risk of bias assessment for each study). The overall interrater agreement was κ=0.48, which is comparable to agreement achieved in past studies (Bilandzic, Fitzpatrick, Rosella, & Henry, 2016; Couto, Pike, Torkilseng, & Klemp, 2015). Differences in ratings were discussed in group until unanimous agreement was reached.
Table 1.
Study Characteristics
| Study (Year) | Size Sample | Age | % Male | Substance Type | Type of SOIT | Type of individual tx | Tx length difference | Substance use measure | Time-point | RoB | Relationship to significant-other involved |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Azrin et al. (2001) | 56 | 15.40 | 82.14 | CMD | Family (Other-SOIT) | CBT | 0 | Freq | PT FU (6 mo.) | Unclear | Caregiver |
| Dennis et al. (2004) | 300 | N/R | 81.33 | CMD | Family (MDFT) CRA | MET | 9.5 | Abs | FU (9 mo.) | Unclear | Caregiver |
| Hedberg & Campbell (1974) | 49 | 38.20 | 91.84 | AUD | Family (Other-SOIT) | OIACT | 0 | Other | PT | High | Partner |
| Liddle et al. (2008) | 224 | 15.40 | 81.25 | CMD | Family (MDFT) | CBT | 0 | Freq Prob | PT FU (12 mo.) | Unclear | Caregiver |
| Liddle et al. (2018) | 113 | 15.36 | 75.00 | CMD | Family (MDFT) | MET | 0 | Freq Prob | FU (12 mo.) | Unclear | Caregiver |
| McCrady et al. (2009) | 102 | 45.05 | 0.00 | AUD | Couple (BCT) | CBT | 0 | Abs Other | PT FU (12 mo.) | Low | Partner |
| O’Farrell et al. (2010) | 29 | 29.09 | 55.17 | CMD | Family (Other-SOIT) | CBT | 0 | Abs Freq Prob | PT FU (6 mo.) | Unclear | Other |
| O’Farrell et al. (2017) | 61 | 38.70 | 0.00 | CMD | Couple (BCT) | 12-step | 0 | Abs Freq Prob | PT FU (12 mo.) | Low | Partner |
| Rigter et al. (2013) | 450 | 16.30 | 85.00 | CMD | Family (MDFT) | CBT | N/R | Freq | PT FU (6 mo.) | Unclear | Caregiver |
| Schumm et al. (2014) | 105 | 44.40 | 0.00 | CMD | Couple (BCT) | 12-step | 0 | Abs Prob | PT FU (12 mo.) | Unclear | Partner |
| Slesnick & Prestopnik (2009) | 119 | 15.13 | 45.38 | CMD | Family (FFT) Family (EBFT) | OIACT | N/R | Freq Quant Prob | PT FU (12 mo.) | Unclear | Caregiver |
| Slesnick et al. (2013) | 179 | 15.40 | 47.49 | CMD | Family (EBFT) | OIACT | 5 | Freq | PT FU (18 mo.) | Unclear | Caregiver |
| Vedel et al. (2008) | 64 | 45.50 | 85.94 | AUD | Couple (BCT) | CBT | 0 | Quant | PT FU (6 mo.) | Unclear | Partner |
| Waldron et al. (2001) | 120 | 15.61 | 80.00 | DUD (marijuana) | Family (FFT) Family (Joint FFT/CBT) | MET | 6 | Freq | PT FU (3 mo.) | Unclear | Caregiver |
| Walker (2001) | 25 | 34.00 | 54.64 | DUD (stimulants) | CRA | OIACT | 0 | Abs | PT FU (3 mo.) | Low | Other |
| Yandoli et al. (2002) | 119 | 28.20 | 63.00 | DUD (opiates) | Family (Other-SOIT) | OIACT | N/R | Other | PT | High | Other |
Note. SOIT= Significant-Other Involved Treatment; AUD= Alcohol Use Disorder; CMD= Combined alcohol and drug use disorder, with specific drug-type varying within sample; DUD= Drug Use Disorder; CRA= Community Reinforcement Approach; BCT= Behavioral Couple Therapy; EBFT= Ecologically Based Family Therapy; FFT= Functional Family Therapy; MDFT= Multidimensional Family Therapy; Other-SOIT= Other Significant-Other Involved Treatment; CBT= Cognitive Behavioral Therapy; MET= Motivational Enhancement Treatment; 12-step= 12-step focused individual treatment; OIACT= Other Individual Active Comparator Treatment; Freq= Frequency; Quant= Quantity; Prob= Problems; Abs= Abstinence; PT= Post -Treatment; FU= Follow-up; mo.= month; Tx= Treatment; N/R: information Not/Reported; RoB= Risk of Bias. Of note, the treatment length difference was computed as the total number of sessions required for SOIT subtracted from the total number of sessions for individually-based active comparator treatments.
Data Analysis
Comprehensive Meta-Analysis 2.0 software was used to aggregate effect sizes across studies (Borenstein, Hedges, Higgins, & Rothstein, 2005). We used a random-effects statistical model rather than a fixed-effects model because the studies included in this analysis are not functionally identical (Hedges & Vevea, 1998).
The results for this meta-analysis are presented in stages. First, we computed an aggregate effect size for all substance use outcomes across both post-treatment and follow-up time-points. We then broke down this effect by examining it across specific types of substance use outcome (e.g., frequency, abstinence, problems, quantity, and other). Next, the overall effect size was parsed according to time-point –post-treatment vs. follow-up time-points, as well as short-term (less than 12 months) vs. long-term (12 months or more) follow-up. Lastly, we computed overall effects subdivided by specific types of SOIT (e.g., Multidimensional Family Therapy, Behavioral Couples Therapy) across all use measures and all time-points.
In cases where studies reported more than one follow-up point, the last follow-up time-point was used to compute effect sizes. In cases where more than one time point or substance use outcome was reported, CMA software was employed to compute the mean value of the relevant outcomes. This approach accounts for clustering within studies by creating an overall average effect size for each study. Effect sizes were interpreted following guidelines proposed by Cohen (1988), with 0.20 indicating a “small” effect size, 0.50 indicating “medium,” and 0.80 and above indicating a “large” effect. A 95% confidence interval (CI) was calculated for each effect size (Lipsey & Wilson, 2001).
Heterogeneity was assessed by examining both Cochran’s Q-statistic and its associated p-value, as well as the I2 statistic (Cochran, 1954). Cochran’s heterogeneity Q-statistic is a commonly used indicator of variation across studies. A significant Q-statistic indicates that heterogeneity is present and that there may be differences between study characteristics. Similarly, the I2 index is another index of heterogeneity which can be interpreted as the percentage of total variability due to between study variation, with 25%, 50%, and 75% representing low, medium, and high heterogeneity respectively (Higgins, Thompson, Deeks, & Altman, 2003).
We then followed-up our analysis with random effects meta-regression models to identify study characteristics that may influence the intervention treatment effect size. In carrying out these moderator analyses, we conducted univariate meta-regression models to examine the bivariate relationships between the various explanatory variables and the substance use outcome variables. Effects that reached significance in bivariate regression models were then entered into multivariate models in order to account for possible covariation across predictors that could account for significant effects. Specifically, we examined the effect of treatment length, type of SOIT, individually-based active comparator treatment type, type of substance used, age, gender, relationship to significant-other involved, baseline use severity, and the type of substance use outcome measure assessed as moderators of the effect of SOIT (see section on data extraction). For the purposes of these analyses, effect sizes were aggregated across post-treatment and follow-up time-points as well as across the substance use outcomes. The Q-statistic was used to test the overall significance of moderating effects for categorical variables whereas the standardized meta-regression coefficients and their corresponding p-values were examined for continuous data.
Lastly, we conducted analyses aimed at gaining a better understanding of the clinical utility of integrating significant-others into treatment. To this end, we examined raw mean differences in the substance use frequency outcome comparing SOIT to individually-based active comparator treatments, aggregated across studies.
Results
Study Selection
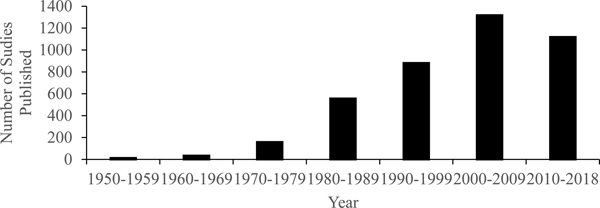
Of 4,901 articles reviewed 4,556 were excluded on the basis of titles and abstracts. The remaining 345 full-text articles were further assessed for eligibility. Among the 345 papers, 98 were excluded because the treatments in these studies did not compare SOIT treatments to individually-based active comparator treatments. Fifty-six studies were excluded for not reporting any substance use related outcomes at post-treatment or follow-up time-points. Thirty were excluded because the participants who engaged in the studies were non-SUD samples. One hundred and four studies were excluded because treatment groups were not randomly assigned. Fourteen studies were excluded because therapy was not conducted in an individual format (i.e., included group-based therapy format—4 involving group therapy in both individual and SOIT conditions). Thirteen studies listed Fals-Stewart as a lead author on a study or a grant receiver on the study project. Five studies recruited a substance-using population that presented with co-morbid schizophrenia and/or schizophrenia-related disorders. Four studies examined treatment modalities where significant-others alone sought treatment, in the absence of the patient him/herself. Lastly, four studies were excluded because sufficient information was not available for effect size calculation: some authors indicated that they no longer had access to the original dataset, and one author did not respond to queries. As a result, a total of 17 reports, derived from 16 independent samples, were included in the current analyses.5 The study selection process is illustrated in Figure 2.
Figure 2.
PRISMA flow diagram illustrating the process of identifying eligible studies.
Note. Studies meeting “other exclusion criteria”: Fourteen studies did not have an experimental and/or comparison treatment group that had at least one clear face-to-face therapy session component. Four studies included treatment modalities where significant-others sought treatment with the aim of engaging and motivating the diagnosed individual to start treatment. Five studies recruited substance using populations that presented with co-morbid severe mental illnesses. Thirteen studies listed Fals-Stewart as a lead author on a study or a grant receiver on the project.
Descriptive Statistics
In total, 77 effect sizes calculated based on data from 2,115 individuals enrolled in 16 independent clinical trials were covered by this review. On average, across all studies, participants were 65.20% male, with an average age of 22.7 (SD= 13.47, Median= 28.2) at study initiation. Eight studies in the current review integrated primary caregivers (e.g. parents), five integrated romantic partners, and three studies integrated a mix of individuals (e.g. parents, siblings, children, and/or partners). Four of the studies had a couples therapy focus, eleven studies had a family therapy focus, and two employed the Community Reinforcement Approach. Nine studies reported a measure of frequency of use or drinking, six studies reported a measure of abstinence, six studies reported a measure of alcohol or drug related problems, two studies reported a measure of quantity of alcohol or drug use, and three studies reported substance use outcomes that fall in the “other” category (e.g., percentage of individuals who have met their treatment goal). Two studies had a 12-step focused individual treatment approach, six studies had a CBT-focused individual treatment approach, three studies had an MET-focused individual treatment approach and lastly, five treatments fell under the “other” treatment category. Fourteen studies reported substance use outcomes at post-treatment, and fourteen studies reported substance use outcomes at follow-up time-points. The average length of follow-up was 9.21 months with follow-ups ranging from 3 months to 18 months. See Table 1 for a full report of study characteristics.
Publication Bias
We used three different strategies to assess for publication bias. First, Rosenthal’s fail-safe N was calculated to determine whether publication bias might have influenced the size of the effect of addiction treatments on emotion outcomes (Rosenthal, 1979). Results indicated that 78 unpublished null results would be required to offset the significant finding, a figure that is beneath Rosenthal’s criteria of 5*k+10 (5*16+10=90). Second, we visually inspected funnel plots of the data. Funnel plots depict the effect size for each sample against its standard error. When there is no publication bias, funnel plots approximate the shape of a funnel, with larger samples clustered around the average effect size at the top of the graph, and smaller samples being more spread out along the bottom of the graph. When publication bias is present, the bottom of the plot appears asymmetrical (Sutton, 2009). Visual inspection of the funnel plot indicated that effects were reasonably evenly distributed around the mean (Figure 3). Lastly, we used Egger’s test of the intercept to calculate for the possibility of asymmetry (Egger, Davey, Schneider, & Minder, 1997). Egger’s test of the intercept yielded a non-significant result, β0=−0.709, t(14)=1.278, p=0.222. This non-significant finding indicates that bias is unlikely. Taken together, these tests of publication bias indicate that, although some minor publication bias may have been present, this bias was unlikely to have had a major influence on results.
Figure 3.
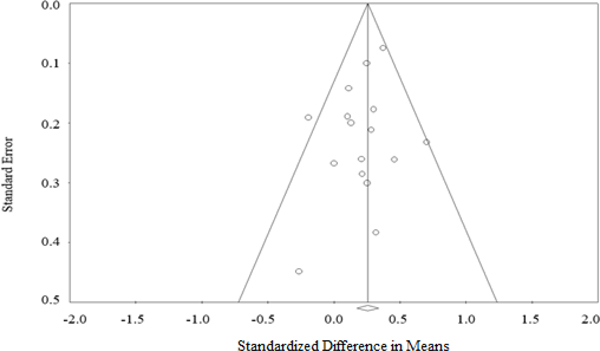
Funnel plot of studies included in the meta-analysis.
Effect of Significant-Other Involvement in SUD Treatment
Overall effect size.
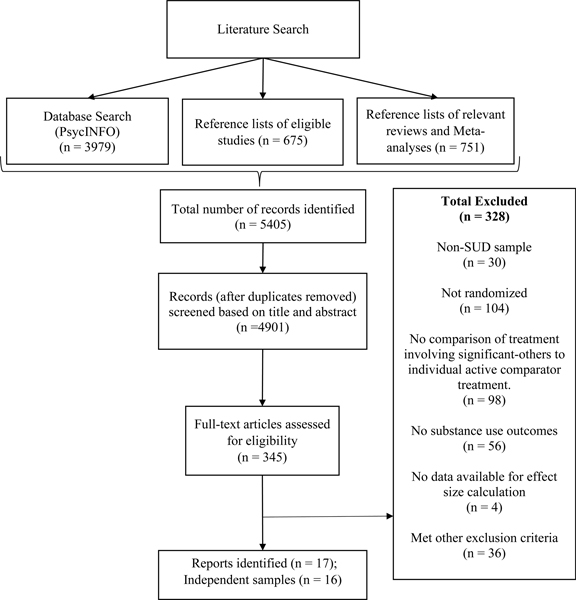
We first aimed to quantify the overall effect of SOIT relative to individually-based active comparator treatments. This effect was examined by aggregating all substance outcomes (frequency, quantity, abstinence, problems, and “other use measure”) across all time-points (post-treatment and follow up time-points examined together). Results indicated a significant effect of SOIT above and beyond individually-based active comparator treatments that was small in magnitude, d=0.242, 95%CI=0.148 to 0.336, k=16 (See Figure 4). Heterogeneity metrics indicated relatively little variation in the size of these effects at the level of the study, indicating that the magnitude of effects tended to be consistent across samples, I2=10.596, Q(15)=16.778, p=0.332, k=16. These findings suggest that across studies, participants enrolled in SOIT demonstrated significantly reduced substance use and substance-related problems compared with those enrolled in individually-based active comparator treatments.
Figure 4.
Effect size table with forest plot.
Note. Cohen’s d values reported above represent the average of all effects that could be derived from the sample, averaged across all time points (post-treatment and follow-up) and substance use outcomes (frequency, problems, abstience, quantity, and “other use measure”). Effects subdivided by time point and outcome are presented in the main text.
Type of substance use outcome.
Next, we ran follow-up analyses breaking down this effect by specific substance use outcome. Results indicated that effect sizes were generally consistent across frequency, d=0.172, 95%CI=0.048 to 0.296, k=9, abstinence, d=0.173, 95%CI=0.004 to 0.349, k=6, problems, d=0.185, 95%CI=0.005 to 0.365, k=6, and were somewhat higher for quantity, d=0.358, 95%CI=−0.048 to 0.763, k=2, as well as “other use measure,” d=0.396, 95%CI=0.256 to 0.537, k=3. Of note, relatively few studies incorporated “quantity” and “other” use measures, and so effect size estimations might be interpreted with these small study samples in mind.
Follow-up time-points.
We then conducted additional analyses separating post-treatment from follow-up time-points. There was a significant main effect of SOIT on overall substance use outcomes at post-treatment that was small in magnitude, d=0.265, 95%CI=0.154 to 0.376 (I2=18.262, Q(13)=15.904, p=0.254, k=14). In the analysis looking at follow-up time-points only, there was also a small and significant effect of SOIT, d=0.171, 95%CI=0.068 to 0.274 (I2=0.000, Q(13)=10.459, p=0.656, k=14). Lastly, a further subdivision of follow-up time-points into short-term (0–12 months) and long-term follow-up (12 month follow-up and beyond) revealed a consistent significant small effect in favor of SOIT at both short-term, d=0.174, 95%CI=0.036 to 0.313 (I2=0.000, Q(6)=4.938, p=0.552, k=7), and also long-term follow-up, d=0.167, 95%CI=0.013 to 0.321 (I2=0.000, Q(6)=5.516, p=0.480, k=7). Taken together, these analyses indicate that SOIT led to significantly reduced substance use and substance use problems at post-treatment, above and beyond individually-based active comparator treatments, and further that effects of SOIT endured 12–18 months past the end of treatment.
Treatment Length Difference.
It is useful to consider these effects within the context of the relative number of sessions required to administer SOIT vs. individually-based active comparator treatments. In the current review, the modal difference in treatment length between SOIT and individually-based active comparator SUD treatments was 0—with SOIT and individual SUD treatments requiring exactly equal numbers of sessions in most studies. However, some studies covered in this review did implement SOIT in a manner that required more sessions (ranging up to 10 sessions), with the average difference in number of sessions being 1.58. We therefore ran a univariate meta-regression examining the bivariate association between difference in treatment length and the magnitude of the effect size produced by the study. The impact of treatment length difference (SOIT vs. individually-based active comparator treatments) was nonsignificant, β=−0.022, p=0.140. This result suggests that treatment length differences did not relate to the overall effect size of the study, and increased duration of SOIT vs individually-based active comparator treatments in some studies did not account for significant effects for SOIT.
Type of SOIT treatment.
Finally, we also examined the overall effects subdivided across specific types of treatment. Of note, the samples of studies were quite low for several subcategories of treatment, and thus the effects did not always reach statistical significance. Nonetheless, effects tended to be relatively consistent in their magnitude across Multidimensional Family Therapy, Functional Family Therapy, Behavioral Couples Therapy, Community Reinforcement Approach, and other approaches, with a small overall effect across each subset of trials with the exception of Ecologically Based Family Therapy. Specifically, Behavioral Couples Therapy had an overall effect of, d=0.212, 95%CI=−0.017 to 0.441, k=4; Multidimensional Family Therapy had an overall effect of, d=0.195, 95%CI=0.059 to 0.330, k=4; Functional Family Therapy had an overall effect of d=0.369, 95%CI=−0.006 to 0.744, k=2; Community Reinforcement Approach treatment had an overall effect of, d=0.120, 95%CI=−0.146 to 0.385, k=2; other-SOIT approaches had an overall effect of, d=0.376, 95%CI=0.161 to 0.5891, k=4; and Ecologically Based Family Therapy had an overall effect of, d=−0.081, 95%CI=−0.403 to 0.241, k=2. Of note, the (small) negative effect in the case of Ecologically Based Family Therapy should be interpreted in light of the relatively small number of studies contributing to its estimation.
Moderator Analysis
We next conducted meta-regression models examining associations between moderators and effect sizes across studies. Of note, the results of heterogeneity analyses reported above indicated low variation across studies and thus we did not anticipate identifying significant moderators. However, moderator analyses were conducted as a conservative measure and in light of recommendations that such analyses may sometimes have utility even given non-significant study-level heterogeneity (Higgins et al., 2003).
The univariate analyses revealed that effects were consistent across most of the moderators examined, with no significant effects for type of SOIT implemented, Q(2)=1.50, p=0.471; individually-based active comparator treatment type, Q(3)=0.63, p=0.890; age of participants, β=0.005, p=0.240; gender of participants, β=0.002, p=0.295; relationship to significant-other involved, Q(2)=4.58, p=0.102; use severity at baseline, β=0.006, p=0.189; and type of substance use outcome measure assessed, Q(3)=3.94, p=0.2696. Two moderators did reach significance in univariate models: level of risk of bias, Q(2)=6.77, p=0.034,7 and type of substance used, Q(2)=7.16, p=0.028 (See Table 2). However, these effects did not reach or approach significance in multivariate models: level of risk of bias, Q(2)=1.29, p=0.525, and type of substance used, Q(2)=1.68, p=0.432. Taken together, results indicate that effects of SOITs tend to be consistent across treatment, study, and population characteristics.
Table 2.
Results of Univariate Meta-Regression Analyses Examining Study-Level Moderators of SOIT vs. Individual Therapy Effect Sizes
| Moderators | Coefficient | p-value | Q-statistics |
|---|---|---|---|
| Treatment length | |||
| Treatment length | −0.022 | 0.140 | |
| Risk of bias | |||
| High | 0.233 | 0.010* | |
| Low | 0.020 | 0.900 | Q=6.77, df=2, p=0.034* |
| Type of significant-other involved treatment implemented | |||
| Couple | 0.476 | 0.311 | |
| Family | 0.535 | 0.242 | Q=1.50, df=2, p=0.471 |
| Individually-based active comparator treatment type | |||
| CBT | −0.031 | 0.809 | |
| 12-step | −0.113 | 0.564 | |
| MET | −0.100 | 0.509 | Q=0.63, df=3, p=0.890 |
| Age of subjects | |||
| Age | 0.005 | 0.240 | |
| Gender of participant | |||
| Percent male | 0.002 | 0.295 | |
| Relationship to significant-other involved | |||
| Caregiver | −0.289 | 0.131 | |
| Partner | −0.132 | 0.493 | Q=4.58, df=2, p=0.102 |
| Use severity at baseline | |||
| Severity at baseline | 0.006 | 0.190 | |
| Type of substance use outcome | |||
| Abstinence | −0.419 | 0.090 | |
| Frequency | −0.332 | 0.089 | |
| Quantity | −0.215 | 0.564 | Q=3.94, df=3 p=0.269 |
| Type of substance used | |||
| Alcohol use disorder | 0.200 | 0.025* | |
| Drug use disorder | 0.326 | 0.057 | Q=7.16, df=2, p=0.028* |
p < 0.05
Note. The Q-statistic offers an omnibus test of overall significance when categorical moderators involve more than two groupings. The reference for the type of SOIT implemented was “community reinforcement approach”. The reference group for risk of bias was set as “unclear risk”. The reference group for individually-based active comparator treatment type, relationship to significant-other involved, and type of substance use outcome were all set as “other”. Lastly, the reference for type of substance used was “Combined alcohol and drug use disorder”.
Clinical Implications: Analysis of Raw Mean Differences
An enduring challenge for intervention research, particularly for systematic reviews, is the interpretation of effect sizes in terms of their tangible implications for the world of clinical practice (Cuijpers, Turner, Koole, Van Dijke, & Smit, 2014; Jacobson & Truax, 1991). A large effect size might reflect large variation between groups, small variation within groups, or some combination of these two (Blanton & Jaccard, 2006). Even when sufficient numbers of studies employ the same outcome variable such that an analysis of raw mean differences is feasible, it is sometimes difficult to translate these numbers into metrics that would be meaningful to a clinician attempting to make decisions to enhance the welfare of his/her client (e.g., what are the precise implications of a 2-point reduction on a negative mood scale for the welfare of a depressed patient?). Although the interpretation of effect sizes represents a challenge across domains of clinical psychology, substance use intervention research is somewhat unique in that some specific commonly-reported substance outcomes (e.g., frequency of use, etc.) are readily interpretable across studies and patient populations. Of note, in the current meta-analysis, the majority of studies (9 of 16) reported treatment effects in relation to a frequency of alcohol or drug use metric (i.e., number of days of recent alcohol/drug use)—a measure that not only carries intrinsic meaning but also reflects the most common outcome assessed in our sample of studies. As these frequency metrics sometimes differed in the time interval covered (e.g., #days/6 months, #days/year), we converted frequency metrics into percentages for the purposes of raw mean difference analysis. Results examining raw mean differences across these studies revealed that SOIT, compared with individually-based active comparator treatments, yielded an overall 5.69% decrease in number of days of drug and/or alcohol use, 95%CI=1.558 to 9.828. When considered in terms of monthly intake, these results translate to approximately 2 fewer days of substance use per month or, in terms of yearly intake, 21 fewer days (about 3 weeks) of substance use a year. Follow-up analyses indicated that effect sizes for studies incorporating a frequency metric, d=0.187, 95%CI=0.063 to 0.312 (k=9), are generally comparable to effect sizes for studies that do not include such a metric, d=0.287, 95%CI=0.134 to 0.441 (k=7)—although effect sizes for studies assessing frequency are slightly lower, suggesting that our estimate of 5.69% may be a conservative one.
Discussion
Over two decades have passed since the publication of the most recent integrative quantitative review of significant-other involved SUD treatments (Stanton & Shadish, 1997), during which time the number of clinical trials assessing the efficacy of these interventions has grown by a factor of several fold. Aggregating effects across trials that together recruited over two thousand participants, the current meta-analysis integrated results from studies that have compared the effects of significant-other involved SUD treatments to “strong” individually-focused active comparator therapies. Significant-other involved treatments examined in this meta-analysis ranged from couples therapy to family therapy to Community Reinforcement Approaches, and individually-focused comparison conditions encompassed a variety of empirically-supported treatments including CBT, MET, and 12-step approaches. Results indicated that, above and beyond the effects of individually-based active comparator treatments, significant-other integration into SUD treatment led to an increased reduction in substance use and substance use problems. Importantly, improved outcomes for significant-other involved treatments extended beyond the end of treatment, enduring as long as 12 to 18 months post-treatment. When examined as raw frequency metrics, the effect of significant-other involvement equates to an approximate 6% reduction in substance use frequency beyond individually-focused treatments—translating to approximately 2 fewer days a month or 3 fewer weeks a year of drinking/drug use. The magnitude of this effect was consistent across treatment types, including couples approaches, Community Reinforcement Approaches, and various family therapy approaches. Effects for significant-other involvement also emerged as consistent across a range of population and treatment characteristics including treatment type, participant age, participant gender, type of substance used, substance use severity at baseline, and relationship to significant-other involved in treatment.
Substance use disorders have been characterized as chronic disorders with pervasive and sometimes grave negative consequences for the user (American Psychiatric Association, 2013; Volkow & Li, 2004). These disorders can be somewhat notoriously difficult to treat, with very high rates of relapse (Brownell, Marlatt, Lichtenstein, & Wilson, 1986). Among individuals whose substance use has progressed into more severe forms, even a single episode of use can lead to major legal, interpersonal, and/or medical problems (e.g., incarceration, hospitalization, family disillusionment). Thus, given the potential severity of the disorder, any treatment that offers the possibility for a few additional substance-free days may be valuable. As noted earlier, numerous researchers have called for the more widespread dissemination of significant-other involved SUD treatments as a useful addition to our arsenal of techniques for treating these challenging disorders (Copello et al., 2006; Karlin & Cross, 2014; Klostermann et al., 2011). But dissemination of these treatments has been markedly slow (McGovern et al., 2004). By providing a precise quantification of effect sizes for significant-other involvement in SUD treatment, this review aims to help practitioners make informed decisions about the usefulness of such treatments and so potentially facilitate their dissemination.
The extent to which significant-other involvement represents a useful addition to treatment will naturally vary depending on the individual case. Personal preferences such as how willing a client is to accept support, levels of perceived support from significant-others, or a desire to work on personal issues may represent barriers to the successful integration of significant-others and family members into treatment (De Civita, Dobkin, & Robertson, 2000; McCrady et al., 2011). Furthermore, although efforts have been made to expand these treatments such that they allow for the possibility of involving a range of significant-others and relationship types (Copello et al., 2002), the majority of such approaches still work specifically with family or romantic partners, making them less relevant for those without strong family/romantic ties. Finally, among individuals with milder forms of substance use disorder, negative consequences of use may be less extreme. In such cases, a 6% reduction in use frequency may carry less significance and so the benefits of significant-other involvement may not outweigh potential barriers (e.g., identifying childcare). Nonetheless, results of the review indicate that integrating significant-others into treatment can lead to reductions in substance use that endure beyond post-treatment and, in many cases, will be meaningful. Further, although some studies included in our sample did require more sessions for significant-other involved treatments, in most cases significant-other involved treatments required equal time commitments as individual therapy and, importantly, there was no association between effect size and differential session frequency.
In addition to implications for clinical practice, results of this review might also have conceptual implications for theory seeking to understand factors contributing to the progression of SUD. The basic literature examining links between close relationship processes and substance use has been characterized nearly exclusively by correlational studies (e.g., Leonard & Eiden, 2007). Thus, although robust associations have been found between various dimensions of close relationships and substance use (Epstein & McCrady, 1998), and in some cases temporal precedence has been established (Fairbairn et al., 2018), no causal relationships can be captured. In this regard, the randomized trials included in this review offer an invaluable resource for addiction theory seeking to understand factors contributing to addiction maintenance/recovery. Note that it is important not to overstate the specificity of inferences that might be derived from these studies— many significant-other involved treatments incorporated diverse change processes including support for drink refusal, modules targeting structural elements and SUD contingencies, daily trust/commitment discussions, as well as exercises intended to enhance the quality of close relationships. Thus, “close relationship processes,” as they are captured within the comparisons provided within studies reviewed here, must be conceptualized extremely broadly. Nonetheless, results of these randomized trials, indicating a positive effect of significant-other integration beyond individual care, move towards providing converging evidence for a causal connection between broad close relationship processes and substance use recovery.
Limitations and future directions should be noted. Similar to most meta-analytic reviews, here we were limited to examining moderators at the level of the sample. Although such sample-level comparisons are appropriate in some cases, and our meta-analysis was reasonably well powered to address some of these sample-level moderators (e.g., gender), they can nonetheless obscure effects and, in some cases, may be especially likely to lead to confounds. For these and other reasons, researchers are increasingly advocating for reviews that account for within study nesting and incorporate participant-level data. Of note, such participant-level analyses may become increasingly more feasible in the future due to data sharing initiatives, such as that recently introduced by the National Institutes of Health. Future reviews with access to participant-level data might usefully re-examine some of the moderators identified here. Second, in the current study, we chose to focus on studies that have incorporated individually-based active comparator treatments. We chose to focus on individually-based comparator conditions to avoid confounds across experimental and control conditions (with a few exceptions, significant-other involved treatments are not administered in groups) and also because other social processes can develop in groups (e.g., the formation of new social bonds) that we believed might complicate interpretations of our findings as they relate to addiction theory. Nonetheless, group-based therapy represents a common form of usual care, and future reviews might consider examining significant-other involved treatments in comparison to group-based active comparator conditions. Third, although our sample of studies was sufficiently large to examine many of the effects of interest here, in the case of some moderator analyses, sub-samples of studies became quite small (e.g., our comparison of effects across specific subtypes of significant-other involved treatments). More research will need to accrue before such moderators can be productively examined in meta-analysis. Fourth, relatively few studies in this literature directly examine mechanisms of change and, where results of mechanistic analyses were reported, measures of mechanism were not consistent across studies. As a result, we were not able to isolate the specific element of close relationship processes (e.g. relationship quality, structural support for sobriety) responsible for effects. Thus, as noted above, the question of the precise close relationship process that is responsible for effects of significant-other involved treatments is left for future research to address. Finally, while reports of quantity of use can carry useful information, we did not include a raw mean difference analysis of quantity. Clinical trials included in this meta-analysis focus on multiple substances aside from alcohol, and so quantity metrics could potentially vary across studies and substances (e.g., a dollar amount for cocaine, number of drinks for alcohol). Further, given the limited number of studies that reported a quantity measure, an analysis of raw mean differences across studies for quantity measures was not feasible.
In sum, the current meta-analysis provides a long overdue update to our understanding of the efficacy of significant-other involved SUD treatments. Results carry interesting conceptual implications for theory seeking to understand factors contributing to the maintenance of addiction, as well as practical implications for clinicians. Findings highlight that capitalizing on the power of close social bonds to drive behavior can yield useful tools within the context of SUD treatment, especially if the diagnosed individual is able and willing to involve close ones.
Public Health Significance Statement:
We synthesize studies that compare addiction treatments involving significant-others with individual addiction interventions. Results indicate a significant edge for treatments that involve significant others in reducing substance use—an effect that endures beyond 1 year after the end of treatment and translates to a reduction of approximately 3 weeks per year in substance use frequency.
Acknowledgments
This research was supported by National Institutes of Health Grant R01AA025969 to Catharine E. Fairbairn. Our thanks to Walter J. Venerable and Dahyeon Kang for their help in the preparation of this manuscript. Our thanks also to Barbara McCrady for helpful feedback at an earlier stage of this project.
Appendix
No article has previously been published based on this meta-analytic dataset, nor are there any articles in press or under review.
Footnotes
The veracity of findings published by William Fals-Stewart is unclear. Thus, and erring on the side of caution, this meta-analysis excludes the work of this researcher.
Although individually-based therapy remains a common treatment format across many contexts, we wish to acknowledge that group-based therapy may be a more common form of usual care in some of these settings. Importantly, the vast majority of studies excluded for this reason included group-based therapy only in the control comparison and not in the significant-other involved treatment condition—thus introducing a confound. Only 4 of the excluded samples included group-based intervention across both treatment and control conditions.
Two studies (Hedberg & Campbell, 1974; Slesnick, Erdem, Bartle-Haring, & Brigham, 2013) involved more than one individual active comparator, and so effects were aggregated into a single comparator categorized as “other.”
Alcohol and substance use related outcomes were coded into four broad categories: Abstinence, frequency, quantity, problems, and “other use”. The abstinence category captures variables that code for the number of days that the individual was abstinent. The frequency of use category captures the number of days spent using and/or drinking. The quantity category captures the amount of alcohol or drugs consumed in a given day or week. The problems category included variables such as consequences of drinking and/or use behaviors as well as alcohol and/or drug related problems. Lastly, the “other” category captures studies that reported proportions of individuals that met their treatment goals and measures of heavy drinking days.
Two studies in this review reported on overlapping samples (Hendriks, van der Schee, & Blanken, 2011; Rigter et al., 2013). Thus, the number of independent samples is slightly lower than the number of reports.
An alternative analysis was carried out in which we examined a larger grouping for the active comparator treatment type. Specifically, this variable was dichotomized into evidence-based treatments or usual care individual treatment. Analysis of this alternative active comparator variable also yielded a non-significant effect, β=−0.275, p=0.143. Similarly, we examined larger groupings for the relationship to significant-other variable in which we combined the “caregiver” and the “other” groupings, and this moderator analysis also yielded non-significant effects, β=0.123, p=0.171.
In univariate models including all studies, those categorized as high risk of bias produced significantly larger effect sizes vs. studies categorized as unclear risk for bias, β=0.233, p=0.010. However, there was no significant difference between either low vs. high, β=0.212, p=0.212, or unclear vs. low β=0.020, p=0.900.
Contributor Information
Talia Ariss, Department of Psychology, University of Illinois— Urbana-Champaign
Catharine E. Fairbairn, Department of Psychology, University of Illinois— Urbana-Champaign
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, & DeCato LA (2001). A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. Journal of Child & Adolescent Substance Abuse, 11(1), 1–43. 10.1300/J029v11n01_01 [DOI] [Google Scholar]
- Baldwin SA, Christian S, Berkeljon A, & Shadish WR (2012). The effects of family therapies for adolescent delinquency and substance abuse: A meta-analysis. Journal of Marital and Family Therapy, 38(1), 281–304. 10.1111/j.1752-0606.2011.00248.x [DOI] [PubMed] [Google Scholar]
- Baumeister RF, & Leary MR (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin, 117(3), 497–529. 10.1037/0033-2909.117.3.497 [DOI] [PubMed] [Google Scholar]
- Bilandzic A, Fitzpatrick T, Rosella L, & Henry D (2016). Risk of bias in systematic reviews of non-randomized studies of adverse cardiovascular effects of thiazolidinediones and cyclooxygenase-2 inhibitors: Application of a new Cochrane risk of bias tool. PLoS Medicine, 13(4), 1–20. 10.1371/journal.pmed.1001987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanton H, & Jaccard J (2006). Arbitrary metrics in psychology. American Psychologist, 61(1), 27–41. 10.1037/0003-066X.61.1.27 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, & Rothstein H (2005). Comprehensive meta-analysis 2.0. Englewood, NJ: Biostat. [Google Scholar]
- Boustani M, Henderson CE, & Liddle HA (2016). Family-based treatments for adolescent substance abuse: How scientific advances yield new developmental challenges. In Zucker RA & Brown SA (Eds.), The Oxford Handbook of Adolescent Substance Abuse; Retrieved from https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199735662.001.0001/oxfordhb-9780199735662-e-032?print=pdf [Google Scholar]
- Brownell KD, Marlatt GA, Lichtenstein E, & Wilson GT (1986). Understanding and preventing relapse. American Psychologist, 41(7), 765–782. https://psycnet.apa.org/doi/10.1037/0003-066X.41.7.765 [DOI] [PubMed] [Google Scholar]
- Burkett JP, & Young LJ (2012). The behavioral, anatomical and pharmacological parallels between social attachment, love and addiction. Psychopharmacology, 224(1), 1–26. 10.1007/s00213-012-2794-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chafez ME (1974). Trends in treatment of alcoholism In Keller M (Ed.), Second special report to the U.S. Congress on alcohol and health: New knowledge (Vol. 2, pp. 111–127). Washington, DC: Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Clark HW (2002). Bridging the gap between substance abuse practice and research: The national treatment plan initiative. Journal of Drug Issues, 32(3), 757–767. 10.1177/002204260203200302 [DOI] [Google Scholar]
- Cochran WG (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101 10.2307/3001666 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed). Hillsdale, N.J: L. Erlbaum Associates. [Google Scholar]
- Copello A, Orford J, Hodgson R, Tober G, Barrett C, & UKATT Research Team. (2002). Social behaviour and network therapy: Basic principles and early experiences. Addictive Behaviors, 27(3), 345–366. 10.1016/S0306-4603(01)00176-9 [DOI] [PubMed] [Google Scholar]
- Copello A, Templeton L, & Velleman R (2006). Family interventions for drug and alcohol misuse: Is there a best practice? Current Opinion in Psychiatry, 19(3), 271–276. 10.1097/01.yco.0000218597.31184.41 [DOI] [PubMed] [Google Scholar]
- Couto E, Pike E, Torkilseng E, & Klemp M (2015). Inter-rater reliability of the Risk of Bias Assessment Tool: For Non-Randomized Studies of Interventions (ACROBAT-NRSI). Cochrane Colloquium. [Google Scholar]
- Cuijpers P, Turner EH, Koole SL, Van Dijke A, & Smit F (2014). What is the threshold for a clinically relevant effect? The case of major depressive disorders. Depression and Anxiety, 31(5), 374–378. 10.1002/da.22249 [DOI] [PubMed] [Google Scholar]
- De Civita M, Dobkin PL, & Robertson E (2000). A study of barriers to the engagement of significant others in adult addiction treatment. Journal of Substance Abuse Treatment, 19(2), 135–144. 10.1016/S0740-5472(00)00095-7 [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, … Funk R (2004). The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment, 27(3), 197–213. 10.1016/j.jsat.2003.09.005 [DOI] [PubMed] [Google Scholar]
- Eddie D, & Kelly JF (2017). How many or how much? Testing the relative influence of the number of social network risks versus the amount of time exposed to social network risks on post-treatment substance use. Drug and Alcohol Dependence, 175, 246–253. 10.1016/j.drugalcdep.2017.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey SG, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. https://doi.org/DOI: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, & McCrady BS (1998). Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clinical Psychology Review, 18(6), 689–711. 10.1016/S0272-7358(98)00025-7 [DOI] [PubMed] [Google Scholar]
- Fairbairn CE, Briley DA, Kang D, Fraley RC, Hankin BL, & Ariss T (2018). A meta-analysis of attachment security and substance use. Psychological Bulletin, 144(5), 532–555. 10.1037/bul0000141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbairn CE, & Cranford JA (2016). A multimethod examination of negative behaviors during couples interactions and problem drinking trajectories. Journal of Abnormal Psychology, 125(6), 805–810. 10.1037/abn0000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbairn CE, & Sayette MA (2014). A social-attributional analysis of alcohol response. Psychological Bulletin, 140(5), 1361–1382. 10.1037/a0037563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filges T, Andersen D, & Jørgensen AK (2015). Effects of Multidimensional Family Therapy (MDFT) on nonopioid drug abuse: A systematic review and meta-analysis. Research on Social Work Practice, 28(1), 68–83. https://doi.org/10.1177%2F1049731515608241 [Google Scholar]
- Hedberg AG, & Campbell L (1974). A comparison of four behavioral treatments of alcoholism. Journal of Behavior Therapy and Experimental Psychiatry, 5(3–4), 251–256. 10.1016/0005-7916(74)90072-X [DOI] [Google Scholar]
- Hedges LV, & Vevea JL (1998). Fixed-and random-effects models in meta-analysis. Psychological Methods, 3(4), 486–504. [Google Scholar]
- Hendriks V, van der Schee E, & Blanken P (2011). Treatment of adolescents with a cannabis use disorder: Main findings of a randomized controlled trial comparing multidimensional family therapy and cognitive behavioral therapy in The Netherlands. Drug and Alcohol Dependence, 119(1–2), 64–71. 10.1016/j.drugalcdep.2011.05.021 [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, … Sterne JAC (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, 1–9. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- Jones BT, Corbin W, & Fromme K (2002). A review of expectancy theory and alcohol consumption. Addiction, 96(1), 57–72. 10.1046/j.1360-0443.2001.961575.x [DOI] [PubMed] [Google Scholar]
- Kalman D, Longabaugh R, Clifford PR, Beattie M, & Maisto SA (2000). Matching alcoholics to treatment: Failure to replicate finding of an earlier study. Journal of Substance Abuse Treatment, 19(2), 183–187. 10.1016/S07405472(00)00096-9 [DOI] [PubMed] [Google Scholar]
- Karlin BE, & Cross G (2014). From the laboratory to the therapy room: National dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. American Psychologist, 69(1), 19–33. 10.1037/a0033888 [DOI] [PubMed] [Google Scholar]
- Kassel JD, Wardle M, & Roberts JE (2007). Adult attachment security and college student substance use. Addictive Behaviors, 32(6), 1164–1176. 10.1016/j.addbeh.2006.08.005 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, & Crowley M (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65(3), 453–463. 10.1037/0022-006X.65.3.453 [DOI] [PubMed] [Google Scholar]
- Klostermann K, Kelley ML, Mignone T, Pusateri L, & Wills K (2011). Behavioral couples therapy for substance abusers: Where do we go from here? Substance Use & Misuse, 46(12), 1502–1509. 10.3109/10826084.2011.576447 [DOI] [PubMed] [Google Scholar]
- Knight DK, & Simpson DD (1996). Influences of family and friends on client progress during drug abuse treatment. Journal of Substance Abuse, 8(4), 417–429. 10.1016/S0899-3289(96)90003-6 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Frank E, & Kupfer DJ (2006). Moderators of treatment outcomes: Clinical, research, and policy importance. JAMA, 296(10), 1286–1289. https://doi.org/doi: 10.1001/jama.296.10.1286 [DOI] [PubMed] [Google Scholar]
- Leach D, & Kranzler HR (2013). An interpersonal model of addiction relapse. Addictive Disorders & Their Treatment, 12(4), 183–192. 10.1097/ADT.0b013e31826ac408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KE, & Eiden RD (2007). Marital and family processes in the context of alcohol use and alcohol disorders. Annual Review of Clinical Psychology, 3, 285–310. 10.1146/annurev.clinpsy.3.022806.091424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Rowe CL, Henderson C, Greenbaum P, Wang W, & Alberga L (2018). Multidimensional Family Therapy as a community-based alternative to residential treatment for adolescents with substance use and co-occurring mental health disorders. Journal of Substance Abuse Treatment, 90, 47–56. 10.1016/j.jsat.2018.04.011 [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Turner RM, Henderson CE, & Greenbaum PE (2008). Treating adolescent drug abuse: A randomized trial comparing multidimensional family therapy and cognitive behavior therapy. Addiction, 103(10), 1660–1670. 10.1111/j.1360-0443.2008.02274.x [DOI] [PubMed] [Google Scholar]
- Liddle HA, Rodriguez RA, Dakof GA, Kanzki E, & Marvel FA (2005). Multidimensional Family Therapy: A science-based treatment for adolescent drug abuse In Lebow J (Ed.), Handbook of clinical family therapy (pp. 128–163). New York: John Wiley and Sons. [Google Scholar]
- Liddle HA, Rowe CL, Gonzalez A, Henderson CE, Dakof GA, & Greenbaum PE (2006). Changing provider practices, program environment, and improving outcomes by transporting multidimensional family therapy to an adolescent drug treatment setting. American Journal on Addictions, 15, 102–112. 10.1080/10550490601003698 [DOI] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. Thousand Oaks, Calif: Sage Publications. [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, & Hildebrandt T (2009). A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology, 77(2), 243–256. 10.1037/a0014686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, & Ladd BO (2011). What do women want? Alcohol treatment choices, treatment entry and retention. Psychology of Addictive Behaviors, 25(3), 521–529. 10.1037/a0024037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Noel NE, Abrams DB, Stout RL, Nelson HF, & Hay WM (1986). Comparative effectiveness of three types of spouse involvement in outpatient behavioral alcoholism treatment. Journal of Studies on Alcohol, 47(6), 459–467. 10.15288/jsa.1986.47.459 [DOI] [PubMed] [Google Scholar]
- McCrady BS, Stout R, Noel N, Abrams D, & Nelson HF (1991). Effectiveness of three types of spouse-involved behavioral alcoholism treatment. British Journal of Addiction, 86(11), 1415–1424. 10.1111/j.1360-0443.1991.tb01727.x [DOI] [PubMed] [Google Scholar]
- McCrady BS, Wilson AD, Muñoz RE, Fink BC, Fokas K, & Borders A (2016). Alcohol-focused behavioral couple therapy. Family Process, 55(3), 443–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Fox TS, Xie H, & Drake RE (2004). A survey of clinical practices and readiness to adopt evidence-based practices: Dissemination research in an addiction treatment system. Journal of Substance Abuse Treatment, 26(4), 305–312. https://doi.org/DOI: 10.1016/j.jsat.2004.03.003 [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Diamond GS, Kaminer Y, & Wintersteen MB (2006). Adolescent and therapist perception of barriers to outpatient substance abuse treatment. American Journal on Addictions, 15(Suppl 1), 16–25. https://doi.org/DOI: 10.1080/10550490601003631 [DOI] [PubMed] [Google Scholar]
- Miller WR, Meyers RJ, & Hiller-Sturmhofel S (1999). The community-reinforcement approach. Alcohol Research and Health, 23(2), 116–121. [PMC free article] [PubMed] [Google Scholar]
- Munder T, & Barth J (2018). Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychotherapy Research, 28(3), 347–355. https://doi.org/doi: 10.1080/10503307.2017.1411628 [DOI] [PubMed] [Google Scholar]
- Nattala P, Leung K, Nagarajaiah J, & Murthy P (2010). Family member involvement in relapse prevention improves alcohol dependence outcomes: A prospective study at an addiction treatment facility in India. Journal of Studies on Alcohol and Drugs, 71(4), 581–587. 10.15288/jsad.2010.71.581 [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, & Clements K (2012). Review of outcome research on marital and family therapy in treatment for alcoholism. Journal of Marital and Family Therapy, 38(1), 122–144. https://doi.org/doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, & Fals-Stewart W (2003). Alcohol abuse. Journal of Marital and Family Therapy, 29(1), 121–146. 10.1111/j.1752-0606.2003.tb00387.x [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM, Neavins TM, & Van Hutton V (2000). Verbal aggression among male alcoholic patients and their wives in the year before and two years after alcoholism treatment. Journal of Family Violence, 15(4), 295–310. [Google Scholar]
- O’Farrell TJ, Murphy M, Alter J, & Fals-Stewart W (2010). Behavioral family counseling for substance abuse: A treatment development pilot study. Addictive Behaviors, 35(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Schumm JA, Kar H, Gnys M, Glynn S, & Klostermann K (2015, November). Dissemination of Behavioral Couple Therapy for Substance Use Disorders. Presented at the Annual Association for Behavioral and Cognitive Therapies Convention, Chicago, IL. [Google Scholar]
- O’Farrell TJ, Schumm JA, Murphy MM, & Muchowski PM (2017). A randomized clinical trial of behavioral couples therapy versus individually-based treatment for drug-abusing women. Journal of Consulting and Clinical Psychology, 85(4), 309–322. 10.1037/ccp0000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peele S (2012). The greatest love addiction songs of all time: Leonard and Lucinda have captured addiction better than the NIDA. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/addiction-in-society/201202/the-greatest-love-addiction-songs-all-time [Google Scholar]
- Powers MB, Vedel E, & Emmelkamp PMG (2008). Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review, 28(6), 952–962. 10.1016/j.cpr.2008.02.002 [DOI] [PubMed] [Google Scholar]
- Rigter H, Henderson CE, Pelc I, Tossmann P, Phan O, Hendriks V, … Rowe CL (2013). Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: A randomised controlled trial in Western European outpatient settings. Drug and Alcohol Dependence, 130(1–3), 85–93. https://doi.org/doi: 10.1016/j.drugalcdep.2012.10.013. [DOI] [PubMed] [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Rowe CL (2012). Family therapy for drug abuse: Review and updates 2003–2010. Journal of Marital and Family Therapy, 38(1), 59–81. https://doi.org/doi: 10.1111/j.1752-0606.2011.00280.x. [DOI] [PubMed] [Google Scholar]
- Rowe CL, Rigter H, Henderson C, Gantner A, Mos K, Nielsen P, & Phan O (2013). Implementation fidelity of Multidimensional Family Therapy in an international trial. Journal of Substance Abuse Treatment, 44(4), 391–399. https://doi.org/doi: 10.1016/j.jsat.2012.08.225 [DOI] [PubMed] [Google Scholar]
- Schumm JA, O’Farrell TJ, Kahler CW, Murphy MM, & Muchowski P (2014). A randomized clinical trial of behavioral couples therapy versus individually based treatment for women with alcohol dependence. Journal of Consulting and Clinical Psychology, 82(6), 993–1004. 10.1037/a0037497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Erdem G, Bartle-Haring S, & Brigham GS (2013). Intervention with substance-abusing runaway adolescents and their families: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 81(4), 600–614. 10.1037/a0033463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, & Prestopnik JL (2009). Comparison of family therapy outcome with alcohol-abusing, runaway adolescents. Journal of Marital and Family Therapy, 35(3), 255–277. 10.1111/j.1752-0606.2009.00121.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton MD, & Shadish WR (1997). Outcome, attrition, and family-couples treatment for drug abuse: A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin, 122(2), 170–191. [DOI] [PubMed] [Google Scholar]
- Stout RL, Kelly JF, Magill M, & Pagano ME (2012). Association between social influences and drinking outcomes across three years. Journal of Studies on Alcohol and Drugs, 73(3), 489–497. 10.15288/jsad.2012.73.489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton AJ (2009). Publication bias In Cooper H, Hedges LV, & Valentine JC (Eds.), The handbook of research synthesis and meta-analysis (Vol. 2, pp. 435–452). New York, NY: Russell Sage Foundation. [Google Scholar]
- Tanner-Smith EE, Wilson SJ, & Lipsey MW (2013). The comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. Journal of Substance Abuse Treatment, 44(2), 145–158. 10.1016/j.jsat.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vedel E, Emmelkamp PMG, & Schippers GM (2008). Individual cognitive-behavioral therapy and behavioral couples therapy in alcohol use disorder: A comparative evaluation in community-based addiction treatment centers. Psychotherapy and Psychosomatics, 77(5), 280–288. 10.1159/000140087 [DOI] [PubMed] [Google Scholar]
- Volkow ND (2011). Principles of drug addiction treatment: A research-based guide. DIANE Publishing. [Google Scholar]
- Volkow ND, & Li T (2004). Drug addiction: The neurobiology of behaviour gone awry. Nature Reviews Neuroscience, 5, 963–970. 10.1038/nrn1539 [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, & Peterson TR (2001). Treatment outcomes for adolescent substance abuse at 4-and 7-month assessments. Journal of Consulting and Clinical Psychology, 69(5), 802–813. 10.1037/0022-006X.69.5.802 [DOI] [PubMed] [Google Scholar]
- Walker DD (2001). The influence of significant others in the treatment of cocaine and stimulant disorders (Doctoral Dissertation). Retrieved from https://search.proquest.com/psycinfo/docview/619719524/abstract/8F127D479F348C2PQ/2
- Weiss RD, Jaffee WB, de Menil VP, & Cogley CB (2004). Group therapy for substance use disorders: What do we know? Harvard Review of Psychiatry, 12(6), 339–350. https://doi.org/DOI: 10.1080/10673220490905723 [DOI] [PubMed] [Google Scholar]
- Yandoli D, Eisler I, Robbins C, Mulleady G, & Dare C (2002). A comparative study of family therapy in the treatment of opiate users in a London drug clinic. Journal of Family Therapy, 24(4), 402–422. 10.1111/1467-6427.00227 [DOI] [Google Scholar]