Abstract
Objective
IgG4-related disease (IgG4-RD) is an immune-mediated multi-organ, chronic and progressive disease. Therefore, we conducted a study to investigate the susceptibility of COVID-19 in IgG4-RD patients in Hubei province, and to characterize the clinical manifestation of COVID-19 in IgG4-RD patients.
Methods
A follow-up system that includes over 200 IgG4-RD patients across the country during the past ten years. A total of ninety-one patients with IgG4-RD who live in Hubei, China were identified and responded to our survey. Medical history, clinical symptoms, laboratory tests, CT imaging, and treatment were obtained through a standardized data collection form, and then independently reviewed by two investigators.
Results
2 of 91 cases were infected with COVID-19. Both of them were classified as moderate type. The symptoms such as fever and cough and radiologic features were similar to other COVID-19 patients. Neither of them episode recurrent of IgG4-RD nor progressed to severe or critical condition of COVID-19 under the condition of continuous oral low-dose of glucocorticoids. Besides, patient 2 took a long time for SARS-CoV-2 nucleic acid to turn negative.
Conclusion
IgG4-RD patients may belongs to the susceptible population of COVID-19 infection, and thus need more careful personal protection. Early identification and properly treatment are very important to prevent IgG4-RD patients with COVID-19 from progression to severe condition.
Keywords: IgG4-related disease, COVID-19, Risk of infection
Introduction
Coronavirus disease 2019 (COVID-19), first recognized in December 2019 [1], rapidly spread to over 200 countries and territories. The causative agent was soon identified as a new strain of coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on February 11, 2020. According to the early transmission dynamics, the mean incubation period was 5.2 days (95% confidence interval [CI], 4.1 to 7.0), with a 95th percentile of the distribution at 12.5 days [2]. Common symptoms are fever, fatigue, myalgia, dry cough, shortness of breath and diarrhea [3]. Laboratory examination usually shows lymphopenia, elevated C-reactive protein and serum ferritin level, prolonged prothrombin time, and elevated lactate dehydrogenase (LDH) [3]. Typical chest computed tomographic (CT) findings include bilateral ground-glass opacity and multifocal patchy consolidation [4]. Advanced age (>60), male sex, and underlying comorbidities (high blood pressure, diabetes, coronary heart disease, etc.) are risk factors for severe disease and death from SARS-Cov-2 infection [5, 6].
IgG4-related disease (IgG4-RD), first identified in 2003, is an immune-mediated multi-organ, chronic and progressive disease characterized by elevated serum IgG4 levels, tumefactive lesions, and characteristic histopathological findings [7]. It occurs most frequently in middle-aged and elderly men. Lesions and persistent inflammation often lead to fibrosis and can cause irreversible damage to surrounding tissues, resulting in IgG4-related autoimmune pancreatitis, sclerosing cholangitis, retroperitoneal fibrosis, kidney disease, and other serious visceral injury and dysfunctions [7, 8]. Glucocorticoids are the first-line agent for all patients with active, untreated IgG4-RD unless contraindications to such treatment are present, and the combination of glucocorticoids and a steroid-sparing immunosuppressive agent is needed for some patients [8]. Rituximab may be considered for failure of conventional therapy, recurrence during steroid reduction, steroid resistance or intolerance, rituximab may be considered [9, 10]. Long-term use of these medications may increase the risk of infection [11].
As one of the major centers of IgG4-RD in China, we have built a follow-up system that includes over 200 IgG4-RD patients across the country during the past ten years. Since IgG4-RD patients may be susceptible to infections due to the immune-related disease itself and the medications they take, we conducted a study to investigate COVID-19 infection rate in Hubei IgG4-RD patients during the recent outbreak in Hubei province, and to characterize the clinical manifestation of COVID-19 in IgG4-RD patients.
Methods
Study design and patients enrolled
The study protocol was approved by the institutional review board (IRB) of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All the IgG4-RD patients were diagnosed according to 2011 comprehensive diagnostic criteria for IgG4-RD [12] and the consensus statement on IgG4-RD pathology [13] or the New Classification Criteria for IgG4-RD released by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) [14]. We excluded patients who were not living in Hubei during the outbreak or lost follow-up from our IgG4-RD follow-up system, and a total of ninety-one patients with IgG4-RD who live in Hubei, China were identified and responded to our survey. Among them, two cases of COVID-19 infection were confirmed according to the Guidance for Corona Virus Disease 2019 (6th edition) released by the National Health Commission of China (http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf).
Data collection
Medical history, clinical symptoms, laboratory tests, CT imaging, and treatment were obtained through a standardized data collection form, and then independently reviewed by two investigators. In our follow-up system, all the patients with active IgG4-RD or other special situation such as infection were followed up at an one month interval. Patients who were at stable remission condition were followed up every three months.
Statistical analysis
Data were analyzed using IBM SPSS, version 21 (SPSS Inc, Chicago, IL) and GraphPad Prism version 7.00 (GraphPad Software, La Jolla). All statistical data were expressed as mean ±SEM.
Results
Basic information of patients with IgG4-RD in Hubei, China
A total of 91 patients(mean age 56±1.321 years; 73.63% male) diagnosed with IgG4-RD in Hubei province were enrolled in the study(Suppl Table 1 ), majority of whom had at least one chronic medical condition. Three patients had fever between January 1st and March 31st, 2020, and two were eventually diagnosed as COVID-19 infection. None of the patients' family members were infected with COVID-19. Compared with the first visit, the IgG4-RD RI score measured on the last on-site follow-up in 2019 decreased dramatically. Most of patients were in stable condition for the latest three months, while three had a flare of IgG4-RD and one patient was hospitalized because of sepsis. During the outbreak, 45 patients (49.45%) are stilling taking low-dose oral glucocorticoids, with an average dose of 6.278±0.582 mg/d and a maximum of 25 mg/d, while 22 patients (24.2%) are taking immunosuppressive agent, such as cyclosporine, tacrolimus, mycophenolate, and methotrexate. 34 patients (37.4%) are not taking any medication for IgG4-RD.
Table 1.
Characteristics of two IgG4-RD patients with COVID-19.
| Basic information | Patient 1 | Patient 2 | The last follow-up | Patient 1 | Patient 2 |
|---|---|---|---|---|---|
| Age (y) | 58 | 45 | IgG4 (g/L) | 11.4 | 4.19 |
| Gender | Male | Male | T-IgE (<100) | 477.9 | 14.65 |
| History of IgG4-RD (y) | 2 | 1.5 | CD3+CD19-(955-2860) | 985 | 966 |
| IgG4-RD RI (the first follow up) | 18 | 15 | CD3+CD8+(320-1250) | 209 | 271 |
| IgG4-RD RI (the last follow up) | 1 | 6 | CD3+CD4+ (550-1440) | 744 | 634 |
| Biological agents | No | No | CD3-CD19+ (90-560) | 127 | 149 |
| Prednisone (mg/d) | 5 | 5 | NK (150-1100) | 1473 | 1423 |
| Symptoms | Comorbidities | ||||
| Fever | Yes | Yes | Hypertension | No | No |
| Cough | Yes | Yes | Cardiovascular disease | No | No |
| Fatigue | Yes | Yes | Diabetes | Yes | No |
| Diarrhea | No | No | Tumor | No | No |
| Lab findings | Complications | ||||
| PT, s (10-16) | 13.5 | 15.4 | ARDS | No | No |
| D-dimer, mg/L (0-0.5) | 0.58 | 0.16 | Shock | No | No |
| Albumin, g/L (40-55) | 33.1 | 42.3 | Acute cardiac injure | No | No |
| ALT, U/L (9-50) | 118 | 77 | Acute liver injure | Yes | Yes |
| AST, U/L (15-40) | 36 | 36 | Acute kidney injure | No | No |
| LDH, U/L (120-250) | 330 | 66.1 | Electrolyte disorder | Yes | Yes |
Abbreviations: PT, prothrombin time, ALT, alanine aminotransferase, LDH, lactic dehydrogenase, AST, aspartate transaminase, ARDS, acute respiratory distress syndrome, IgG4-RD, IgG4 related disease.
Clinical characteristics of IgG4-RD patients infected with COVID-19
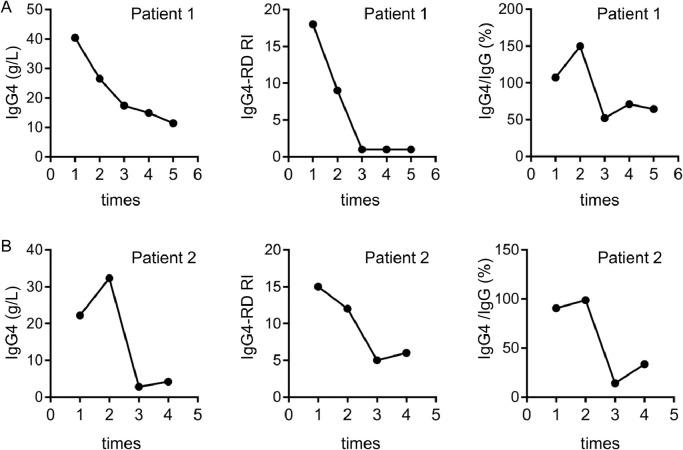
The clinical manifestations of the primary disease and disease condition on the last on-site visit of the two IgG4-RD patients infected with COVID-19 were as follows: Patient 1 is a fifty-eight years old male, diagnosed with IgG4-RD two years ago. The involved organs include gallbladder, biliary tract, kidney and ureter. The IgG4-RD RI score was 18 at the time of diagnosis. Patient 2 is a forty-five years old male, diagnosed with IgG4-RD one and a half years ago. The involved organs include sinuses, lacrimal, submandibular gland and retroperitoneal lymph nodes, with an IgG4-RD RI score of 15 at the first visit. On the last on-site visit, both patients showed a significant remission of symptoms, with the IgG4-RD RI scores dropped to 1 and 6, respectively. The levels of serum IgG4 and total IgE in patient 1 were still higher than the normal upper limit, but the percentages and absolute numbers of circulating T lymphocyte, B cell, and NK cell are within normal range in both patients (Table 1). Up to now, patient 1 and patient 2 have completed 5 and 4 follow-up visits respectively. Compared with the first visit, their IgG4-RD RI score, serum IgG4 concentration, and the ratio of IgG4/IgG decreased dramatically, especially after the third visit (Fig. 1 ). Both patients have been taking 5mg prednisone daily for more than 6 months before the infection of COVID-19 (Table 1).
Fig. 1.
The clinical characteristic of IgG4-RD patients with COVID at each on site follow up. A. The serum concentration of IgG4, IgG4-RD RI and IgG4/IgG% of patient 1; B. The serum concentration of IgG4, IgG4-RD RI and IgG4/IgG of patient 2.
Both patients have residential history of Wuhan, Hubei and a history of fever, dry cough, and fatigue before admission. Patient 1 presented as transient intermittent low-grade fever (Tmax 37.5℃) for 3 days, while patient 2 as fever(Tmax 38.5℃) for 5 days. Neither of them had running nose, diarrhea, myalgia or dyspnea. For laboratory inspection, the number and percentages of white blood cell (WBC) and lymphocytes of Patient 1 were in the normal range while they were slightly reduced in patient 2 (Fig. 2 ). Both patients had significant elevated C-reactive protein (CRP) and slightly elevated alanine aminotransferase (ALT), while their procalcitonin were normal. Besides, patient 1 showed a decreased serum albumin level and elevated levels of LDH. Imaging examination of Chest CT scan showed a mixed pattern of ground glass opacities and multiple patchy high density shadows in both lungs of these two patients (Fig. 2). Their diagnosis of COVID-19 were soon confirmed by positive SARS-CoV RNA test. According to the Guidance for Corona Virus Disease 2019 (6th edition), both of the IgG4-RD patients were classified as having moderate type of COVID-19.
Fig. 2.
Timeline of two IgG4-RD patients with COVID. A. Timeline of laboratory findings (including the number of white blood cells and lymphocytes, CRP, SARS-CoV-2 nucleic acid test) and chest CT imaging changes in IgG4-RD patient 1 with COVID; B. Timeline of laboratory findings (including the number of white blood cells and lymphocytes, CRP, SARS-CoV-2 nucleic acid test) and chest CT imaging changes in IgG4-RD patient 2 with COVID.
During hospitalization, they were both treated with antivirus agent (oseltamivir 75mg bid po for patient 1; ganciclovir 0.5g qd ivdrip, oseltamivir 75mg bid po and recombinant human interferon a-2b 5 million U qd IM for patient 2), antibiotics (moxifloxacin 0.4g qd ivdrip), and Chinese medicinal formulae. Patient 1 was also given intravenous transfusion of albumin(10g/d for 4 days) and immunoglobulin (10g/d for 10 days). Their symptoms were gradually relieved within two weeks after treatment. The inflammation lesions in the lungs of patient 1 peaked at day 4 after admission and then gradually absorbed, while lung lesions in patient 2 continuously improved since admission (Fig. 2). Patient 1 was discharged after 17 days of hospital stay after two consecutive negative results of SARS-CoV-2 nucleic acid test. Patient 2 had twice weak positive of SARS-CoV-2 nucleic acid intermittently after the symptoms disappeared, and was discharged after 36 days of hospital stay (Fig. 2). Both patients were positive for SARS-CoV-2 nucleic acid antibodies IgG while negative for IgM one month later. Both patients continued at the stable dose of 5mg prednisone daily after discharge, and none of them had recurrent of IgG4-RD.
Discussion
To the best of our knowledge, our study is the first to report the susceptibility of COVID-19 in IgG4-RD patients, although a newly initial data from the COVID-19 Global Rheumatology Alliance provider registries analyzed 110 individuals with rheumatic disease who have been diagnosed with COVID-19 showed that patients with rheumatoid arthritis(RA), psoriatic arthritis(PsA) and systemic lupus erythematosus(SLE) were the main infected population, while 17 of 110 cases were listed as having other rheumatic disease [15]. We followed up 91 IgG4-RD patients in Hubei province, the epicenter of COVID-19 outbreak in China, and found two case of IgG4-RD patients had infected with COVID-19. Consistent with the reports, most of IgG4-RD patients were middle-aged to elderly men [7, 16]. In addition, the majority of the patients in our study had at least one chronic medical condition, such as hypertension and diabetes. The available data at present suggested that advanced age, male sex and chronic comorbidities are risk factors of mortality in patients with SARS-Cov-2 infection [17], [18], [19]. Therefore, theoretically IgG4-RD patients have a high risk of progressing to severe/critical COVID-19 once infected and thus need to be identified and properly treated as early as possible.
Our study is also the first to describe the clinical characteristics of COVID-19 in IgG4-RD patients. The symptoms such as fever and cough and radiologic features were similar to other COVID-19 patients. However, the decline in white blood cells and lymphocytes in IgG4-RD patients may not be as typical and significant as other COVID-19 patients. The disease activity of IgG4-RD may also affect the recovery process of COVID-19. On the last on-site visit, patient 1 had a much lower IgG4-RD RI score than patient 2. Although patient 2 was younger, it took a longer time for him to recover from COVID-19. It is worth noting that neither of them developed primary disease relapse nor progressed to severe or critical condition of COVID-19 under the condition of continuous oral low-dose of glucocorticoids. This may be in part due to their prompt hospitalization, and it might also indicate that long-term oral low-dose of glucocorticoid may not be the risk factor for accelerating disease progression of COVID-19.
The use of glucocorticoids remains controversial in patients infected with COVID-19. There are many studies supporting the use of corticosteroids in patients with coronavirus infection [3, 20, 21]. However, high-dose corticosteroids may be associated with increased risks of secondary infections, long-term complications, and prolonged virus shedding in COVID-19 patients [22]. In fact, it has been reported that the duration of viral RNA clearance as detected in oropharyngeal swabs and fecal samples was longer in glucocorticoid treatment group than that in non-glucocorticoid treatment group [23]. In our study, patient 2 took a long time for SARS-Cov-2 nucleic acid to turn negative, which may implicated that the viral load in such patients may need to be monitored for a longer time after discharge. Besides, the clearance of viral RNA in patients' stools may take a longer time compared to that in oropharyngeal swabs [23], it is better to test the viral RNA in stools or in combination with oropharyngeal swabs.
In summary, we describe the infection status and clinical characteristics of COVID-19 among IgG4-RD patients under the pandemic situation in this study. IgG4-RD patients may belong to the susceptible population of COVID-19 infection, and thus need more careful personal protection. Early identification and properly treatment are very important to prevent IgG4-RD patients with COVID-19 from progression to severe condition. As COVID-19 has become a global health threat, our study could help rheumatologists to better manage IgG4-RD patients under the pandemic situation.
Fundings
This work was supported by grants from the National Natural Science Foundation of China (no. 81771754 and no. 81901651) and the Tongji Hospital Clinical Research Flagship Program (no. 2019CR206).
Declaration of Competing Interest
The authors have declared no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.semarthrit.2020.04.015.
Appendix. Supplementary materials
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R. A Novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K., Lau E., Wong J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., Ma K., Xu D., Yu H., Wang H. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamisawa T., Zen Y., Pillai S., Stone J.H. IgG4-related disease. Lancet. 2015;385:1460–1471. doi: 10.1016/S0140-6736(14)60720-0. [DOI] [PubMed] [Google Scholar]
- 8.Khosroshahi A., Wallace Z.S., Crowe J.L., Akamizu T., Azumi A., Carruthers M.N., Chari S.T., Della-Torre E., Frulloni L., Goto H. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015;67:1688–1699. doi: 10.1002/art.39132. [DOI] [PubMed] [Google Scholar]
- 9.Khosroshahi A., Bloch D.B., Deshpande V., Stone J.H. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. 2010;62:1755–1762. doi: 10.1002/art.27435. [DOI] [PubMed] [Google Scholar]
- 10.Carruthers M.N., Topazian M.D., Khosroshahi A., Witzig T.E., Wallace Z.S., Hart P.A., Deshpande V, Smyrk T.C., Chari S., Stone J.H. Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis. 2015;74:1171–1177. doi: 10.1136/annrheumdis-2014-206605. [DOI] [PubMed] [Google Scholar]
- 11.Vandewalle J., Luypaert A., De Bosscher K., Libert C. Therapeutic mechanisms of glucocorticoids. Trends Endocrinol Metab. 2018;29:42–54. doi: 10.1016/j.tem.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Umehara H., Okazaki K., Masaki Y., Kawano M., Yamamoto M., Saeki T., Matsui S., Yoshino T., Nakamura S., Kawa S. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22:21–30. doi: 10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 13.Deshpande V., Zen Y., Chan J.K., Yi E.E., Sato Y., Yoshino T., Kloppel G., Heathcote J.G., Khosroshahi A., Ferry J.A. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181–1192. doi: 10.1038/modpathol.2012.72. [DOI] [PubMed] [Google Scholar]
- 14.Wallace Z.S., Naden R.P., Chari S., Choi H.K., Della-Torre E., Dicaire J.F., Hart P.A., Inoue D., Kawano M., Khosroshahi A. The 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-related disease. Ann Rheum Dis. 2020;79:77–87. doi: 10.1136/annrheumdis-2019-216561. [DOI] [PubMed] [Google Scholar]
- 15.Gianfrancesco M.A., Hyrich K.L., Gossec L., Strangfeld A., Carmona L., Mateus E.F., Sufka P., Grainger R., Wallace Z., Bhana S. Rheumatic disease and COVID-19: initial data from the COVID-19 Global Rheumatology Alliance provider registries. Lancet Rheumatol. 2020;2:250–253. doi: 10.1016/S2665-9913(20)30095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang L., Zhang P., Zhang X., Lin W., Tang H., Li J., Wang M., Liu X., Fei Y., Chen H. Sex disparities in clinical characteristics and prognosis of immunoglobulin G4-related disease: a prospective study of 403 patients. Rheumatology. 2019;58:820–830. doi: 10.1093/rheumatology/key397. [DOI] [PubMed] [Google Scholar]
- 17.Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P., Wang X., Hu C., Ping R., Hu P. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan K.W., Wong V.T., Tang S. COVID-19: an update on the epidemiological, clinical, preventive and therapeutic evidence and guidelines of integrative Chinese-western medicine for the management of 2019 novel coronavirus disease. Am J Chin Med. 2020;48:1–26. doi: 10.1142/S0192415X20500378. [DOI] [PubMed] [Google Scholar]
- 19.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen R.C., Tang X.P., Tan S.Y., Liang B.L., Wan Z.Y., Fang J.Q., Zhong N. Treatment of severe acute respiratory syndrome with glucosteroids: the Guangzhou experience. Chest. 2006;129:1441–1452. doi: 10.1378/chest.129.6.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shang L., Zhao J., Hu Y., Du R., Cao B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet. 2020;395:683–684. doi: 10.1016/S0140-6736(20)30361-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ling Y., Xu S.B., Lin Y.X., Tian D., Zhu Z.Q., Dai F.H., Wu F., Song Z.G., Huang W., Chen J. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J. 2020;133:1039–1043. doi: 10.1097/CM9.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.