Abstract
Background
Gliomas are the most common primary malignant brain tumor. Diffuse low-grade and intermediate-grade gliomas, which together compose the lower-grade gliomas (LGGs; World Health Organization [WHO] grades II and III), present a therapeutic challenge to physicians due to the heterogeneity of their clinical behavior. Nomograms are useful tools for individualized estimation of survival. This study aimed to develop and independently validate a survival nomogram for patients with newly diagnosed LGG.
Methods
Data were obtained for newly diagnosed LGG patients from The Cancer Genome Atlas (TCGA) and the Ohio Brain Tumor Study (OBTS) with the following variables: tumor grade (II or III), age at diagnosis, sex, Karnofsky performance status (KPS), and molecular subtype (IDH mutant with 1p/19q codeletion [IDHmut-codel], IDH mutant without 1p/19q codeletion, and IDH wild-type). Survival was assessed using Cox proportional hazards regression, random survival forests, and recursive partitioning analysis, with adjustment for known prognostic factors. The models were developed using TCGA data and independently validated using the OBTS data. Models were internally validated using 10-fold cross-validation and externally validated with calibration curves.
Results
A final nomogram was validated for newly diagnosed LGG. Factors that increased the probability of survival included grade II tumor, younger age at diagnosis, having a high KPS, and the IDHmut-codel molecular subtype.
Conclusions
A nomogram that calculates individualized survival probabilities for patients with newly diagnosed LGG could be useful to health care providers for counseling patients regarding treatment decisions and optimizing therapeutic approaches. Free online software for implementing this nomogram is provided: https://hgittleman.shinyapps.io/LGG_Nomogram_H_Gittleman/.
Key Points
1. A survival nomogram for lower-grade glioma patients has been developed and externally validated.
2. Free online software for implementing this nomogram is provided allowing for ease of use by practicing health care providers.
Keywords: lower grade glioma, survival, nomogram, glioma, TCGA
Importance of the Study.
Gliomas are the most common primary malignant brain tumor. Diffuse low-grade and intermediate-grade gliomas, which together make up LGGs (WHO grades II and III), cause considerable morbidity and present a therapeutic challenge to physicians due to the heterogeneity of their clinical behavior. The nomogram provides an individualized estimate of survival rather than a group estimate. This tool can be useful to patients and health care providers for counseling patients and their families regarding treatment decisions, follow-up, and prognosis. Here we describe a survival nomogram for patients with LGG which has been developed and independently validated. To facilitate clinical use of this nomogram, free online software for its implementation is provided (https://hgittleman.shinyapps.io/LGG_Nomogram_H_Gittleman/).
Gliomas are the most common primary malignant brain and other central nervous system tumor, accounting for approximately 80% of malignant brain tumors, with 15 000–17 000 new cases annually in the United States.1–4 Although diffuse low-grade and intermediate-grade gliomas, which together compose the lower-grade gliomas (LGGs; World Health Organization [WHO] grades II and III),5 are rarer than grade IV gliomas, glioblastoma (GBM); cause considerable morbidity; and present a therapeutic challenge to physicians due to the heterogeneity of their clinical behavior.1,2,5–9 Prognosis is variable, and survival ranges widely.1 Traditionally, grade II gliomas were thought to have a better prognosis than grade III gliomas, but since the 2016 WHO reclassification of gliomas, it is thought that the molecular alterations (which can be determined objectively) are significantly more important than the grade (which is somewhat subjective and sample dependent).5
Diagnosis and current treatment varies depending on patient prognostic factors, including histology, tumor grade, age at diagnosis, Karnofsky performance status (KPS), first presenting symptom, extent of resection, tumor size and location, and neurologic deficits, as well as certain molecular markers.5–8,10 These molecular markers include codeletion of chromosome arms 1p and 19q and isocitrate dehydrogenase enzyme 1/2 (IDH) mutation.1–4,7,10 Codeletion of 1p/19q is the most common genetic characteristic of oligodendroglioma, with up to 70% of adult oligodendrogliomas having this codeletion.3 In general, this codeletion significantly predicts positive response to chemotherapy and radiation.1,5,7,9,10IDH mutations characterize the majority of LGGs in adults and are considered hallmarks of these neoplasms.1,3–5,10 Patients with IDH mutations have improved prognosis compared with IDH wild-type patients.1–4 In 2016, the WHO revised the definition of oligodendrogliomas, which are classified by 1p/19q codeletion and IDH mutation status, and of astrocytomas, which are classified by IDH mutation status.1,11 Current literature suggests classifying LGG into IDH wild-type (IDHwt) cases, IDH mutants additionally carrying 1p/19q codeletion (IDHmut-codel), and IDH mutants with euploid 1p/19q (IDHmut-non-codel).2 Previous analyses by The Cancer Genome Atlas (TCGA) showed that IDHmut-non-codel glioma patients had shorter overall survival than IDHmut-codel patients, yet both of these subgroups had significantly longer overall survival than patients with IDHwt gliomas.5
Nomograms are useful and accessible tools for physicians to use for predicting survival, planning for individualized treatment, and deciding the interval for follow-up and/or imaging.12 Nomograms have been previously developed for gliomas, including 2 nomograms for GBM,12,13 1 for both high- and low-grade glioma,14 and 3 specifically for LGG.15–17 Of the 3 LGG nomograms, however, 1 was for prediction of IDH/1p/19q molecular subtype and not survival,15 and the other 2 nomograms lacked important prognostic factors such as performance status and 1p/19q codeletion.16,17 Therefore, the purpose of this study was to develop and independently validate a nomogram for estimation of individualized survival probabilities for newly diagnosed LGG that would include 1p/19q codeletion and IDH mutation status as well as additional important prognostic factors. The final nomogram was developed using data from TCGA and externally validated using data from the Ohio Brain Tumor Study (OBTS). In addition, an easy to use online calculator is provided.
Materials and Methods
Data Collection and Study Population
This study was approved by the University Hospitals institutional review board. The training data consisted of the data from TCGA from its hallmark paper (diagnosis years 1994–2013) “Comprehensive, Integrative Genomic Analysis of Diffuse Lower-Grade Gliomas,” 5 merged with data for the same patients from the more recent paper “An Integrated TCGA Pan-Cancer Clinical Data Resource to Drive High-Quality Survival Outcome Analytics,” 18 in order to obtain more current patient outcomes (follow-up/survival time and survival status). For the validation dataset, data were obtained from the OBTS for the diagnosis years 2007–2018 on adult patients with newly diagnosed LGG. LGG is defined as diffuse low-grade and intermediate-grade glioma (WHO grades II and III).5 Both datasets were defined using International Classification of Diseases for Oncology, third edition (ICD-O-3) codes 9382/3 (oligoastrocyoma), 9400/3 (diffuse astrocytoma), 9401/3 (anaplastic astrocytoma), 9450/3 (oligodendroglioma), and 9451/3 (anaplastic oligodendroglioma). These ICD-O-3 codes predated molecular marker diagnosis and were used for selection of patients for study only.
TCGA data initially included 289 patients with LGG that was newly diagnosed in 1994–2013. Because some LGG patients in TCGA were also in the OBTS set, the OBTS patients were dropped from the dataset of TCGA (n = 18 patients). Patients with mismatched histology groups with their ICD-O-3 codes (ie, an oligodendroglioma patient with a 9382/3 ICD-O-3 code) were excluded (n = 13 patients). Other exclusion criteria included patients with a prior cancer diagnosis (n = 7), patients with a survival time of 0 days (n = 2 patients), patients with a known inherited genetic syndrome (n = 1 patient), and patients with an unknown molecular subtype (TCGA set only; n = 10 patients). The final TCGA dataset had a total of 238 patients. The OBTS dataset contained 98 total patients diagnosed in 2007–2018.
The following variables were obtained for each patient: tumor grade (grade II or III), year of diagnosis (1994–2018), age at diagnosis (continuous), sex, race (white, black, American Indian or Alaska Native), KPS (40–100 in tens) recorded postsurgery, first presenting symptom (seizures or other), molecular subtype (IDHmut-codel, IDHmut-non-codel, IDHwt), survival/follow-up time in months (continuous), and survival status (alive or dead). Due to the high amount of missing KPS values (55.0% missing in TCGA and 40.8% missing in OBTS), KPS was imputed using multivariate imputation by chained equations using the R package ‘mice’.19 In addition, 33 of the 98 patients in OBTS (33.7%) had missing molecular subtype, so these values were imputed as well. The raw, unimputed values versus their imputed values for both datasets are displayed in Supplementary Table 1.
All gliomas were histologically confirmed. For TCGA, clinical information, histology, and molecular classifications (including IDH and 1p/19q-based molecular subtypes) were obtained from the supplementary material from the 2016 pan-glioma paper, where this information was generated as described previously.5,20 For OBTS, IDH testing was conducted via immunohistochemistry. Fluorescence in situ hybridization analysis was used to detect deletion of chromosome arms 1p and 19q. Both IDH mutation status and 1p/19q codeletion status were reviewed at each participating center by an expert neuropathologist.
Statistical Analyses
Descriptive statistics were used to assess any differences in patient characteristics and prognostic factors between the 2 datasets using chi-square tests for categorical variables, a t-test for age at diagnosis, and a Wilcoxon rank-sum test for follow-up time, in the unimputed and imputed datasets. Using the ‘survival’ package in R,21 overall survival rates by molecular subtype were calculated for each of the 2 datasets using the Kaplan–Meier method, and differences were assessed using the log-rank test. Overall survival by study was also evaluated for any differences between TCGA and OBTS, unadjusted and adjusted for molecular subtype. Overall survival was assessed using Cox proportional hazards (CPH) regression (‘survival’ package)21 in univariable and multivariable models. Nonsignificant variables (P > 0.05) were dropped unless they held appreciable clinical significance. After these variables were dropped, overall survival was evaluated using CPH regression, random survival forests (RSFs) (‘randomForestSRC’ package),22 and recursive partitioning analysis (RPA) (‘rpart’ package).23 In CPH, the proportional hazards assumption was verified using the methodology of Grambsch and Therneau.24 RSF is an ensemble tree method for analyzing right-censored survival data. Trees are grown by randomly drawing bootstrap samples of the data, and at each node of the tree a subset of the covariates are selected randomly as candidate variables for splitting.25 One thousand trees were generated, and all possible split points for each variable were evaluated to find the optimal split solution. In RPA, a full recursive classification tree was generated and the least important splits were removed recursively to obtain the final subclassification tree with the minimal model deviance.
The models were trained using TCGA data and then independently externally validated using the OBTS data. Models were also internally validated using 10-fold cross-validation, and individual predicted 60-, 90-, and 120-month survival probabilities were generated to measure predictive accuracy compared with the observed survival as “ground truth.” The predictive accuracies for overall survival of the 3 statistical approaches (CPH, RSF, and RPA) were calculated using the concordance index, which ranges from 0.5 (completely random prediction) to 1 (perfect prediction) and is equivalent to the area under the receiver operating characteristic curve for censored data.26 A final nomogram was developed using the method with the greatest predictive accuracy for individualized estimation of survival. Calibration of the final model was visually examined by assigning all patients into quintiles of the nomogram-predicted 60-month survival probabilities and plotting the mean nomogram predicted 60-month survival probability against the Kaplan–Meier estimated 60-month survival for each quintile using the ‘rms’ R package.27 Finally, a sensitivity analysis was conducted using a subset of the OBTS patients with complete (unimputed) molecular markers as the validation set in order to assess any differences in calibration when molecular subtype was not imputed. All analyses were performed using R version 3.5.2.28P-values less than 0.05 were considered to be statistically significant.
Results
Patient Characteristics
Demographics for TCGA patients (N = 238) and the OBTS patients (N = 98) are presented in Table 1. Overall, there were more males (TCGA: 55.5%, OBTS: 56.1%) than females (TCGA: 44.5%, OBTS: 43.9%), almost all the patients were white (TCGA: 95.7%, OBTS: 91.8%), the most common first presenting symptom was seizures (TCGA: 53.2%, OBTS: 61.2%), and most patients were alive (TCGA: 74.8%, OBTS: 54.1%) at their last follow-up. There were several differences between the training (TCGA) and validation (OBTS) datasets. Diagnoses in patients in TCGA were at earlier ages (mean age at diagnosis = 42.46 y) than in patients in OBTS (mean age at diagnosis = 47.69 y) (P = 0.002). The imputed KPS values were distributed differently between TCGA and OBTS, with TCGA patients having higher KPS values (95.0% had KPS ≥70) than OBTS patients (78.6% had KPS ≥70) (P < 0.001). The majority of TCGA patients had the IDHmut-non-codel molecular subtype (52.5%), whereas the majority of OBTS patients had IDHwt (39.8%) (P < 0.001). OBTS patients had significantly longer follow-up (median follow-up = 43.29 mo) compared with TCGA patients (median follow-up = 20.70 mo) (P < 0.001). Not surprisingly, more patients were alive at their last follow-up in TCGA (74.8%) compared with the OBTS set (54.1%) (P < 0.001).
Table 1.
Newly diagnosed primary LGG patient characteristics, imputed data (TCGA 1994–2013, OBTS 2007–2018)
| TCGA (N = 238) | OBTS (N = 98) | P-value | |
|---|---|---|---|
| Tumor grade,* N (%) | 0.190 | ||
| Grade II | 118 (49.6) | 57 (58.2) | |
| Grade III | 120 (50.4) | 41 (41.8) | |
| Year of diagnosis,* N (%) | <0.001 | ||
| 1994 | 2 (0.8) | 0 (0.0) | |
| 1995 | 3 (1.3) | 0 (0.0) | |
| 1996 | 1 (0.4) | 0 (0.0) | |
| 1997 | 3 (1.3) | 0 (0.0) | |
| 1998 | 9 (3.8) | 0 (0.0) | |
| 1999 | 3 (1.3) | 0 (0.0) | |
| 2000 | 4 (1.7) | 0 (0.0) | |
| 2001 | 5 (2.1) | 0 (0.0) | |
| 2002 | 0 (0.0) | 0 (0.0) | |
| 2003 | 2 (0.8) | 0 (0.0) | |
| 2004 | 1 (0.4) | 0 (0.0) | |
| 2005 | 7 (2.9) | 0 (0.0) | |
| 2006 | 14 (5.9) | 0 (0.0) | |
| 2007 | 13 (5.5) | 4 (4.1) | |
| 2008 | 20 (8.4) | 9 (9.2) | |
| 2009 | 23 (9.7) | 12 (12.2) | |
| 2010 | 28 (11.8) | 5 (5.1) | |
| 2011 | 50 (21.0) | 18 (18.4) | |
| 2012 | 44 (18.5) | 8 (8.2) | |
| 2013 | 6 (2.5) | 14 (14.3) | |
| 2014 | 0 (0.0) | 10 (10.2) | |
| 2015 | 0 (0.0) | 9 (9.2) | |
| 2016 | 0 (0.0) | 5 (5.1) | |
| 2017 | 0 (0.0) | 2 (2.0) | |
| 2018 | 0 (0.0) | 2 (2.0) | |
| Age at diagnosis,^ y, mean (SD) | 42.46 (13.27) | 47.69 (16.58) | 0.002 |
| Sex,* N (%) | 1.000 | ||
| Male | 132 (55.5) | 55 (56.1) | |
| Female | 106 (44.5) | 43 (43.9) | |
| Race,* N (%) | (MIissing = 4; 1.7) | 0.107 | |
| White | 224 (95.7) | 90 (91.8) | |
| Black | 9 (3.8) | 6 (6.1) | |
| American Indian/Alaska Native | 1 (0.4) | 0 (0.0) | |
| Asia/Pacific Islander | 0 (0.0) | 2 (2.0) | |
| KPS* (imputed),* N (%) | <0.001 | ||
| 40 | 1 (0.4) | 2 (2.0) | |
| 50 | 4 (1.7) | 10 (10.2) | |
| 60 | 7 (2.9) | 9 (9.2) | |
| 70 | 21 (8.8) | 14 (14.3) | |
| 80 | 41 (17.2) | 14 (14.3) | |
| 90 | 106 (44.5) | 36 (36.7) | |
| 100 | 58 (24.4) | 13 (13.3) | |
| First presenting symptom,* N (%) | (Missing = 20; 8.4) | 0.229 | |
| Seizures | 116 (53.2) | 60 (61.2) | |
| Other | 102 (46.8) | 38 (38.8) | |
| Molecular subtype,* N (%) | <0.001 | ||
| IDHmut-codel | 65 (27.3) | 30 (30.6) | |
| IDHmut-non-codel | 125 (52.5) | 29 (29.6) | |
| IDHwt | 48 (20.2) | 39 (39.8) | |
| Follow-up months,# median [interquartile range] | 20.70 [7.18, 40.93] |
43.29 [16.73, 82.92] |
<0.001 |
| Survival status,* N (%) | <0.001 | ||
| Alive | 178 (74.8) | 53 (54.1) | |
| Dead | 60 (25.2) | 45 (45.9) |
*P-value calculated by chi-square test.
^P-value calculated by t-test.
#P-value calculated by Wilcoxon rank-sum test.
Survival by the Kaplan–Meier Method and Cox Proportional Hazards
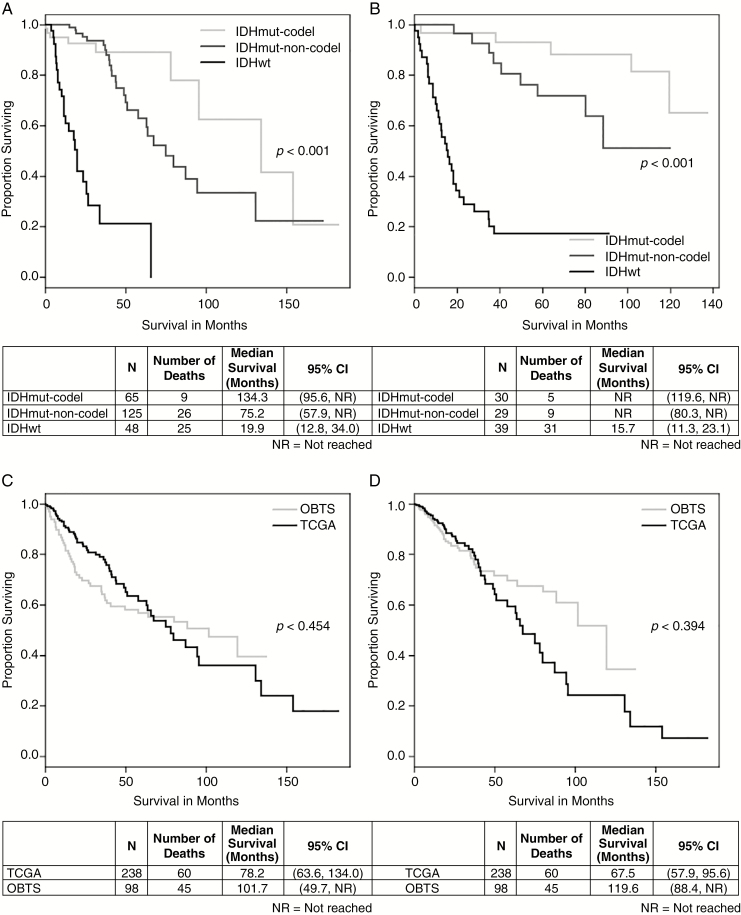
Stratifying by molecular subtype, the Kaplan–Meier curve (Fig. 1A) for TCGA showed a significant difference (P < 0.001), with the IDHmut-codel subtype having the best survival (median survival = 134.3 mo; 95% CI: 95.6–median survival not reached [NR] mo), followed by the IDHmut-non-codel subtype (median survival = 75.2 mo; 95% CI: 57.9–NR mo), and the IDHwt subtype having the worst survival (median survival = 19.9 mo; 95% CI: 12.8–34.0 mo). Similarly for OBTS (Fig. 1B) when stratifying by molecular subtype (P < 0.001), the IDHmut-codel subtype had the best survival (median survival = NR mo; 95% CI: 119.6–NR mo), followed by the IDHmut-non-codel subtype (median survival = NR mo; 95% CI: 80.3–NR mo), and the IDHwt subtype had the worst survival (median survival = 15.7 mo; 95% CI: 11.3–23.1 mo). Without adjusting for any covariates, overall survival did not differ between TCGA (median survival = 78.2 mo; 95% CI: 63.6–134.0 mo) and OBTS (median survival = 101.7 mo; 95% CI: 49.7–NR mo) (P = 0.454) (Fig.1C). After adjusting for molecular subtype, there was still no difference in overall survival between TCGA (median survival = 67.5 mo; 95% CI: 57.9–95.6 mo) and OBTS (median survival = 119.6 mo; 95% CI: 88.4-NR mo) (P = 0.394) (Fig. 1D).
Fig. 1.
Kaplan–Meier survival curves for newly diagnosed LGG patients by (A) molecular subtype from TCGA patients, (B) molecular subtype from OBTS patients, (C) study (unadjusted), and (D) study adjusted for molecular subtype; P-values from log-rank tests.
Univariable and multivariable CPH regression results are displayed in Supplementary Table 2 and Table 2, respectively, for both the training set (TCGA) and the validation set (OBTS) separately. Because patient race and first presenting symptom were not found to be statistically significant in univariate analyses, these variables were dropped from the models. Sex was also not found to be statistically significant, but this variable was kept in the multivariable models due to clinical importance. In the multivariable analyses, younger age at diagnosis, having the IDHmut-codel molecular subtype compared with the IDHwt molecular subtype, and having the IDHmut-non-codel subtype compared with the IDHwt molecular subtype were significantly associated with better survival outcomes (all P ≤ 0.005) in both datasets. The data did not violate the proportional hazards assumption of the CPH model (TCGA: P = 0.676, OBTS: P = 0.921).
Table 2.
Multivariable Cox proportional hazards models for patients with newly diagnosed LGG
| Factor | TCGA (Training) (N = 238) | OBTS (Validation) (N = 98) | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P-value | Hazard Ratio | 95% CI | P-value | |
| Grade, III vs II | 3.646 | (1.869, 7.114) | <0.001 | 1.951 | (0.959, 3.967) | 0.065 |
| Age at diagnosis | 1.044 | (1.019, 1.070) | <0.001 | 1.055 | (1.030, 1.081) | <0.001 |
| Sex, male vs female | 0.816 | (0.483, 1.377) | 0.445 | 0.845 | (0.446, 1.601) | 0.606 |
| KPS, imputed | 0.979 | (0.957, 1.001) | 0.063 | 0.968 | (0.948, 0.988) | 0.002 |
| Molecular subtype, imputed, IDHmut-codel vs IDHwt | 0.127 | (0.049, 0.329) | <0.001 | 0.055 | (0.015, 0.196) | <0.001 |
| Molecular subtype, imputed, IDHmut-non-codel vs IDHwt | 0.208 | (0.097, 0.444) | <0.001 | 0.249 | (0.094, 0.661) | 0.005 |
*Adjusts for grade, age at diagnosis, sex, imputed KPS, and imputed molecular subtype.
Internal Cross-Validation
After 10-fold cross-validation was performed on the training set (TCGA), the concordance indices were computed for each statistical method for predicting survival at 3 timepoints: 60, 90, and 120 months (Table 3). The concordance index is a measure of the predictive accuracy of the model being tested, which ranges from 0.5 (completely random prediction) to 1 (perfect prediction). For all 3 timepoints the CPH analysis (60-mo, 90-mo, 120-mo: 0.844, 0.843, 0.841) outperformed RSF (60-mo, 90-mo, 120-mo: 0.806, 0.791, 0.782) and RPA (60-mo, 90-mo, 120-mo: 0.792, 0.792, 0.792). Based on these results, the multivariable CPH model was then independently validated using the OBTS dataset. The RSF ranked the covariates in order of importance, with molecular subtype being the most important variable, followed by age at diagnosis, tumor grade, KPS, and sex. The RPA showed that the most important split in predicting mortality was molecular subtype, followed by age at diagnosis and tumor grade.
Table 3.
Internal 10-fold cross-validation concordance indices (95% CI) for CPH, RSFs, and RPA at 60, 90, and 120 months for patients newly diagnosed with LGG (TCGA training set)
| CPH | RSF | RPA | |
|---|---|---|---|
| 60 mo | 0.844 (0.785–0.902) |
0.806 (0.750–0.863) |
0.792 (0.726–0.858) |
| 90 mo | 0.843 (0.786–0.900) |
0.791 (0.725–0.857) |
0.792 (0.726–0.858) |
| 120 mo | 0.841 (0.783–0.900) |
0.782 (0.715–0.850) |
0.792 (0.726–0.858) |
Nomogram and Independent Validation
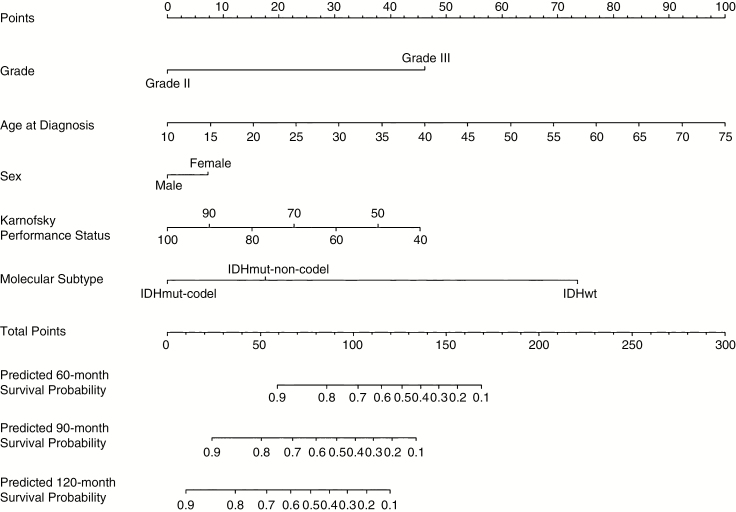
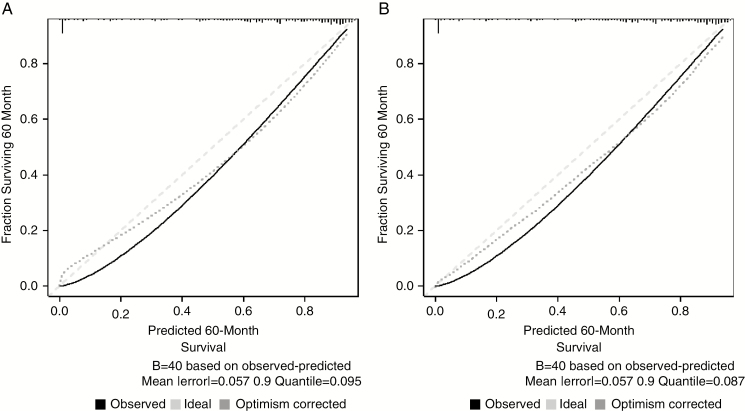
The nomogram to estimate 60-, 90-, and 120-month survival probabilities was built using the training dataset (TCGA) and validated on the independent dataset (OBTS) using the CPH model (Fig. 2). An online calculator for the final nomogram is available via an internet interface at https://hgittleman.shinyapps.io/LGG_Nomogram_H_Gittleman/. The final CPH model was well calibrated with a concordance index of 0.844 (95% CI: 0.785, 0.902). For each quintile group, the estimated versus observed 60-month survival probabilities intersected the 45-degree line, indicating that the predicted value approximated the observed value within a 95% confidence interval (Supplementary Figure 1). Calibration curves were also drawn for the training dataset (TCGA) for predicted 60-, 90-, and 120-month survival, as well as for the independent validation dataset (OBTS) for a visual comparison. In Fig. 3 and Supplementary Figure 2, the black line shows the observed survival rates, the gray line shows the ideal survival rates, and the dark gray line shows the optimism-corrected survival rates. The optimism-corrected (also known as bias-corrected or overfitting-corrected) line is produced using a bootstrap approach to estimate predicted and observed values based on a nonparametric smoother applied to a sequence of predicted values. For the predicted 60-month survival plots (Fig. 3A and B), the observed and optimism-corrected lines are well aligned, although both of these lines fall slightly beneath the ideal 45-degree line, which means the nomogram predicts a greater fraction of survival at 60 months than what is observed. For the predicted 90-month survival plots (Supplementary Figure 2A and C), the observed and optimism-corrected lines are well aligned, although both of these lines fall slightly above the ideal 45-degree line, which means the nomogram predicts a lower fraction of survival at 90 months than what is observed. For the predicted 120-month survival plots (Supplementary Figure 2B and D), all 3 lines are closely aligned, demonstrating good calibration.
Fig. 2.
Validated nomogram for predicted 60-, 90-, and 120-month survival for patients with newly diagnosed LGG; TCGA.
Fig. 3.
Calibration curves for 60-month survival for (A) training data (TCGA) and for (B) testing data (OBTS) for patients with newly diagnosed LGG.
Sensitivity Analysis for Imputation of Molecular Subtype
The same statistical analyses described above were conducted with a subset of the OBTS patients who had complete, unimputed molecular subtype to assess any differences in calibration when molecular marker was known and not imputed. This smaller dataset consisted of 65 patients. The patient demographics between the full, imputed OBTS dataset and the subset of those patients with complete molecular subtype are displayed in Supplementary Table 3. None of the distributions of the variables were statistically different between the 2 sets (all P > 0.249). Imputed molecular subtype did not differ from the complete set of molecular subtype (P = 0.846).
Discussion
The goal of this study was to develop and validate, both internally and externally, an individual survival nomogram for patients with newly diagnosed LGG, where LGG is defined as diffuse low-grade and intermediate gliomas (WHO grades II and III).5 The multivariable CPH regression model had the best fit on the dataset from TCGA (with adjustment for tumor grade, age at diagnosis, sex, KPS, and molecular subtype), and was then independently, externally validated on the OBTS dataset.
A previous nomogram for LGG patient survival by Gorlia et al, which used data from the European Organisation for Research and Treatment of Cancer and the North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group Intergroup, included histologic diagnosis (oligodendroglioma/oligoastrocytoma or astrocytoma), time since first symptoms, presence of neurologic deficit, tumor size, and treatment (delayed radiation or immediate radiation),16 but lacked essential prognostic variables such as tumor grade, age at diagnosis, performance status, and molecular subtype. Another previously developed LGG nomogram by Wang et al, which used clinical data from TCGA and -omic data from the University of California Santa Cruz Xena browser, included sex, histologic diagnosis (oligodendroglioma/oligoastrocytoma or astrocytoma), IDH mutation, tumor grade, age at diagnosis, and Growth Arrest Specific Transcript 5 expression.17 Our nomogram included all of the variables in Wang et al’s nomogram, with the exception of Growth Arrest Specific Transcript 5 expression and histology (as histology is now defined using molecular markers), but also added other important prognostic variables such as postoperative KPS and 1p/19q codeletion, both of which were found to be statistically significant.
Mutation of the telomerase reverse transcriptase (TERT) promoter, which encodes telomerase, is common across all gliomas.2,9 This mutation, which is associated with an older age at diagnosis, is generally unfavorable in the absence of IDH mutation and favorable in the presence of IDH and 1p/19q codeletion.9 Gliomas with IDH mutation, 1p/19q codeletion, and TERT promoter mutation are most strongly associated with the oligodendroglial histology and better overall survival.9 While TCGA data include TERT mutation status, this variable was not collected in OBTS and was thus excluded in the current study. However, TERT mutations are correlated with the IDH‒1p/19q molecular subtype. A study by Eckel-Passow et al found that among IDHmut-codel LGG patients, 96% carried activating TERT promoter mutations.9 While the effect of the TERT mutation alone is uncertain, Eckel-Passow found that gliomas with only TERT mutations were primarily GBM.9 Future work could include adding TERT mutation status to the nomogram.
Clinical presentation, which can be expressed as the presence of seizures, absence of neurologic deficits, or good performance status, is a strong prognostic factor.6 Seizure is the most common presenting symptom, occurring in about 80% of patients.6,8 We found that 53.2% of patients in the dataset from TCGA and 61.2% of patients in the OBTS dataset presented with seizure as their first symptom. Presentation with seizures has traditionally been identified as a positive prognostic factor.8 This may be because patients who present with seizures tend to be younger and have smaller tumor sizes at diagnosis.6 Other literature suggests that the improved survival of patients who present with seizures is correlated with having the IDH mutation. IDHmut gliomas are more likely to cause seizures than IDHwt gliomas,29,30 even independently of WHO grade.31 Our study did not find presentation with seizures to be a statistically significant prognostic factor (TCGA: P = 0.651, OBTS: P = 0.124) and was therefore removed from the final model. Future work should assess the importance of this variable.
The effect of surgery on overall survival is unclear. While some studies have found a survival advantage with more extensive surgery, others did not.6 Therefore, we did not include extent of resection in our nomogram. While radical surgery is currently a staple in the management of gliomas of all grades,10 not all LGGs are amenable to gross total resection.8 However, there is growing evidence in support of extensive surgical resection,8 and perhaps this variable should be considered in the future. Although radiation therapy has been shown to provide some benefit to LGG patients, the efficacy and timing of this treatment has been debated.6,8 Chemotherapy is emerging as an alternate approach to radiation therapy as a neoadjuvant treatment.6 Some studies suggest there may be a need for neoadjuvant chemotherapy before surgical resection.8 However, the value of concomitant and/or maintenance chemotherapy with temozolomide has not been tested prospectively.10 In a recent randomized trial, time to failure of both chemotherapy and radiation was similar whether patients were treated initially with chemotherapy and received radiation at first progression or were treated with initial radiation and received chemotherapy at progression.10 Thus, there is no clear standard of care for LGG patients. Some studies suggest that the standard therapy consists of adjuvant radiation following surgery,10 while others suggest that the optimal treatment strategy includes extensive surgical resection when possible and delaying radiation until progression.8 Due to the nebulous definition for standard of care, our nomogram did not take radiation treatment or chemotherapy into account.
There are several limitations to this study. First, TCGA and OBTS datasets had several differences in their patient populations. Nearly all of the variables of interest had significant differences between the training and validation sets, except for tumor grade and sex. However, upon adjustment using multivariable survival models, results for all key prognostic variables were similar. In addition, even with these differences, the external validation demonstrated good calibration. Second, although race was collected on patients in both datasets, nearly all of the patients were white (95.7% in TCGA and 91.8% in OBTS). Therefore, race was not found to be a significant factor and was dropped from the survival models, despite evidence for differences in survival by race.1 Third, there was a fair amount of missing data in the KPS variable for both datasets and some missing data for molecular subtype in the OBTS validation dataset. Although these variables were imputed using multivariate imputation by chained equations, creating 20 imputed datasets which were pooled together into one final complete dataset, it is possible to have some level of inaccuracy in the imputed values. However, our sensitivity analysis shows that the imputation of molecular subtype in OBTS did not have any substantial impact on the final calibration when compared with patients with complete molecular subtype in the validation dataset. Fourth, our nomogram did not include methylation status of the promoter region of the gene O6-methylguanine-DNA methyltransferase (MGMT), a DNA repair protein that is associated with improved survival in patients with diffuse gliomas.1,10 This variable was not collected in OBTS for LGG patients. Similarly, genome-wide association studies have shown that certain copy number variations affect LGG patient survival, such as TERT (as mentioned previously), coiled-coil domain containing protein 26, cyclin-dependent kinase inhibitor (CDKN)2A-CDKN2b (CDKN2A/B deletion), regulator of telomere elongation helicase 1, and pleckstrin homology like domain family B member 1.32 These variables were not collected in TCGA or OBTS for LGG patients. Future work will include adding MGMT methylation status and additional copy number variants to the nomogram. Fifth, our nomogram did not incorporate extent of surgical resection, because TCGA does not collect information on surgical resection for LGG patients. Although the highly invasive nature of LGG often makes complete surgical resection impossible,4–6 the optimal treatment strategy for LGG includes extensive surgical resection when possible.8 Therefore, future work will include adding extent of surgical resection to the nomogram. Finally, while the internal and external calibration plots yielded good calibration at 120 months, the observed and optimism-corrected lines deviated somewhat from the ideal line in both the internal and external validation at 60 and 90 months. This is likely due to the low proportion of patients who died during their follow-up in both datasets (TCGA: 25.2%, OBTS: 45.9%). Overall, while the nomogram includes the most common genetic mutations for LGG (1p/19q and IDH), the LGG nomogram would be strengthened by including other important variables such as MGMT and additional copy number variants, and these will be incorporated in future work when more complete datasets are available.
In summary, we developed and independently validated a nomogram to enable personalized survival estimates for patients with newly diagnosed LGG. This tool provides an individualized estimate of survival, rather than a group estimate based on specific patient-level characteristics, and should be useful to patients and health care providers for counseling patients and their families regarding treatment decisions, follow-up, and prognosis. To facilitate clinical use of this nomogram, free online software for its implementation is provided (https://hgittleman.shinyapps.io/LGG_Nomogram_H_Gittleman/).
Supplementary Material
Supplementary data are available at Neuro-Oncology online.
Funding
A.E.S. is supported by NIH CA217956, the Peter D Cristal Chair, the Center of Excellence for Translational Neuro-Oncology, the Gerald Kaufman Fund for Glioma Research, the Kimble Family Foundation, and the Ferry Family Foundation at University Hospitals of Cleveland. J.S.B-S. is supported in part by the Sally S. Morley Designated Professorship in Brain Tumor Research and the University Hospitals Research Division.
Conflict of interest statement. There are no conflicts of interest to report.
Authorship statement. Haley Gittleman: study design, data collection, data analysis/interpretation, figure preparation, manuscript drafting, reviewing/editing manuscript. Andrew E. Sloan: reviewing/editing manuscript. Jill S. Barnholtz-Sloan: study design, data collection, data analysis/interpretation, figure preparation, reviewing/editing manuscript.
Supplementary Material
References
- 1. Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol. 2018;20(suppl_4):iv1–iv86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ceccarelli M, Barthel FP, Malta TM, et al. ; TCGA Research Network Molecular profiling reveals biologically discrete subsets and pathways of progression in diffuse glioma. Cell. 2016;164(3):550–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goodenberger ML, Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012;205(12):613–621. [DOI] [PubMed] [Google Scholar]
- 4. Gorovets D, Kannan K, Shen R, et al. IDH mutation and neuroglial developmental features define clinically distinct subclasses of lower grade diffuse astrocytic glioma. Clin Cancer Res. 2012;18(9):2490–2501. [DOI] [PubMed] [Google Scholar]
- 5. Brat DJ, Verhaak RG, Aldape KD, et al. Cancer Genome Atlas Research Network. Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 2015;372(26):2481–2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cavaliere R, Lopes MB, Schiff D. Low-grade gliomas: an update on pathology and therapy. Lancet Neurol. 2005;4(11):760–770. [DOI] [PubMed] [Google Scholar]
- 7. Daniels TB, Brown PD, Felten SJ, et al. Validation of EORTC prognostic factors for adults with low-grade glioma: a report using intergroup 86-72-51. Int J Radiat Oncol Biol Phys. 2011;81(1):218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pouratian N, Schiff D. Management of low-grade glioma. Curr Neurol Neurosci Rep. 2010;10(3):224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eckel-Passow JE, Lachance DH, Molinaro AM, Walsh KM, Decker PA, Sicotte H. Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med. 2015;372(26):2499–2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stupp R, Brada M, van den Bent MJ, Tonn JC, Pentheroudakis G; ESMO Guidelines Working Group High-grade glioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3):iii93–101. [DOI] [PubMed] [Google Scholar]
- 11. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–820. [DOI] [PubMed] [Google Scholar]
- 12. Gittleman H, Lim D, Kattan MW, et al. An independently validated nomogram for individualized estimation of survival among patients with newly diagnosed glioblastoma: NRG Oncology RTOG 0525 and 0825. Neuro Oncol. 2017;19(5):669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gorlia T, van den Bent MJ, Hegi ME, et al. Nomograms for predicting survival of patients with newly diagnosed glioblastoma: prognostic factor analysis of EORTC and NCIC trial 26981-22981/CE.3. Lancet Oncol. 2008;9(1):29–38. [DOI] [PubMed] [Google Scholar]
- 14. Yang T, Mao P, Chen X, et al. Inflammatory biomarkers in prognostic analysis for patients with glioma and the establishment of a nomogram. Oncol Lett. 2019;17(2):2516–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu Z, Zhang T, Jiang H, Xu W, Zhang J. Conventional MR-based preoperative nomograms for prediction of IDH/1p19q subtype in low-grade glioma. Acad Radiol. 2019;26(8): 1062–1070. [DOI] [PubMed] [Google Scholar]
- 16. Gorlia T, Wu W, Wang M, et al. New validated prognostic models and prognostic calculators in patients with low-grade gliomas diagnosed by central pathology review: a pooled analysis of EORTC/RTOG/NCCTG phase III clinical trials. Neuro Oncol. 2013;15(11):1568–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang Y, Xin S, Zhang K, Shi R, Bao X. Low GAS5 levels as a predictor of poor survival in patients with lower-grade gliomas. J Oncol. 2019;2019:1785042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu J, Lichtenberg T, Hoadley KA, et al. ; Cancer Genome Atlas Research Network An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell. 2018;173(2):400–416.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67. [Google Scholar]
- 20. The Cancer Genome Atlas. Supplemental material from doi:10.1016. https://tcga-data.nci.nih.gov/docs/publications/lgggbm_2016/. Accessed May 13, 2019.
- 21. Therneau T._A Package for Survival Analysis in S_. version 2.38, 2015. URL: https://CRAN.R-project.org/package=survival. Accessed April 5, 2019.
- 22. Ishwaran H, Kogalur UB. Random Forests for Survival, Regression, and Classification (RF-SRC), R package version 2.6.1 2018.
- 23. Therneau T, Atkinson B. rpart: Recursive Partitioning and Regression Trees. R package version 4.1–13 2018. https://CRAN.R-project.org/package=rpart. Accessed April 5, 2019.
- 24. Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–526. [Google Scholar]
- 25. Ishwaran H, Kogalur UB, Blackstone EH, Lauer MS. Random survival forests. Ann Appl Stat. 2008;2(3):841–860. [Google Scholar]
- 26. Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–387. [DOI] [PubMed] [Google Scholar]
- 27. Frank EH Jr. rms: Regression Modeling Strategies. R package version 5.1-2 https://CRAN.R-project.org/package=rms. Accessed April 5, 2019.
- 28. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. URL https://www.R-project.org/. [Google Scholar]
- 29. Feyissa AM, Worrell GA, Tatum WO, et al. Potential influence of IDH1 mutation and MGMT gene promoter methylation on glioma-related preoperative seizures and postoperative seizure control. Seizure. 2019;69:283–289. [DOI] [PubMed] [Google Scholar]
- 30. Wang ZF, Chen HL. Relationship between IDH1 mutation and preoperative seizure in low-grade gliomas: a meta-analysis. Clin Neurol Neurosurg. 2016;148:79–84. [DOI] [PubMed] [Google Scholar]
- 31. Chen H, Judkins J, Thomas C, et al. Mutant IDH1 and seizures in patients with glioma. Neurology. 2017;88(19):1805–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shete S, Hosking FJ, Robertson LB, et al. Genome-wide association study identifies five susceptibility loci for glioma. Nat Genet. 2009;41(8):899–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.