Abstract
Aims
Patients with metabolic syndrome (MetS) are known to be at increased risk of postoperative complications, but it is unclear whether MetS is also associated with complications after total hip arthroplasty (THA) or total knee arthroplasty (TKA). Here, we perform a systematic review and meta-analysis linking MetS to postoperative complications in THA and TKA.
Methods
The PubMed, OVID, and ScienceDirect databases were comprehensively searched and studies were selected and analyzed according to the guidelines of the Meta-analysis of Observational Studies in Epidemiology (MOOSE). We assessed the methodological quality of each study using the Newcastle-Ottawa Scale (NOS), and we evaluated the quality of evidence using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE). Data were extracted and meta-analyzed or qualitatively synthesized for several outcomes.
Results
Ten cohort studies involving 1,352,685 patients were included. Qualitative analysis suggested that MetS was associated with a higher incidence of cardiovascular events, and meta-analysis showed that MetS increased the risk of all-cause complications (risk ratio (RR) 1.55, 95% confidence interval (CI) 1.28 to 1.89), surgical site infection (SSI; RR 2.99, 95% CI 1.30 to 6.90), urinary tract infection (UTI; RR 2.58, 95% CI 1.03 to 6.43), and 30-day readmission (RR 1.45, 95% CI 1.33 to 1.59). There was insufficient evidence for assessing an association between MetS and venous thromboembolism events, pulmonary or gastrointestinal complications, or mortality.
Conclusion
Patients with MetS undergoing THA and TKA are at increased risk of all-cause complications, cardiovascular complications, SSI, UTI, and 30-day readmission. Surgeons should be aware of the increased risk of these complications in MetS, and presurgical protocols for these complications should give special consideration to MetS patients.
Cite this article: Bone Joint Res. 2020;9(3):120–129.
Keywords: Metabolic syndrome, Complications, Total hip arthroplasty, Total knee arthroplasty
Article focus
This systematic review and meta-analysis evaluated the impact of metabolic syndrome (MetS) on postoperative complications after total hip arthroplasty (THA) and total knee arthroplasty (TKA).
Key messages
The available evidence shows that THA and TKA patients with MetS are at increased risk of all-cause complications, cardiovascular complications, surgical site infection, urinary tract infection, and 30-day readmission.
Strengths and limitations
This is the first systematic review and meta-analysis to assess whether MetS alters risk of complications after THA and TKA, and it involved more than 1.3 million patients.
We identified several postoperative complications for which MetS significantly increases risk, but we could not meta-analyze several other complications because of heterogeneity between studies, which future studies should address.
Introduction
Metabolic syndrome (MetS) comprises a constellation of abnormal medical conditions that increase the risk of atherosclerotic cardiovascular disease, endocrine dysfunction, thromboembolic events, and osteoarthritis.1–4 There are several definitions of MetS with slight variations in diagnostic criteria, but the presence of central obesity, insulin resistance, hypertension, and dyslipidemia are components contributing to this disease complex.5–7 MetS is estimated to affect 7% to 40% of adults and increases substantially with age, which brings a major burden for the healthcare system.8–10
Several studies show that MetS is associated with an increased risk of postoperative complications and mortality.11–15 For example, patients with MetS undergoing coronary artery bypass grafting surgery stay longer in the intensive care unit than patients without MetS and show higher risk of surgical complications such as atelectasia11 and all-cause mortality outcomes.12 MetS is also associated with an increased risk of mortality in patients undergoing noncardiac surgical procedures,13 and an increased incidence of postoperative complications in patients undergoing fracture surgery.14,15
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are common surgical procedures to relieve pain and improve joint function in patients suffering from severe hip and knee joint disease.16 In the USA, demand for THA is expected to reach 570,000 and demand for TKA to reach 3.5 million by 2030.17 MetS is estimated to affect 10% to 15% of THA and TKA patients, a percentage which is expected to increase as the population ages.18–20 Several studies have reported that MetS increases the risk of cardiovascular complications,21 venous thromboembolism (VTE),22 and pulmonary embolism20 following arthroplasty. MetS was also reported to be an independent risk factor for all-cause complications, wound complications, and readmission following arthroplasty.18 However, a comprehensive understanding of how MetS affects risk of complications and poor outcomes after THA or TKA is still lacking.
Presurgical comorbidities strongly influence postsurgical outcomes, including the incidence of life-threatening complications. A more accurate understanding of how comorbidities impact the results of surgical intervention could help reduce postoperative risks and medical costs, improve quality of treatment, and increase patient satisfaction.18 Considering the absence of systematic reviews in the field, we therefore performed this systematic review and meta-analysis of the literature to provide a detailed critical analysis of the effects of MetS on postoperative THA and TKA outcomes.
Methods
This study was conducted according to the guidelines of the Meta-analysis of Observational Studies in Epidemiology (MOOSE).23 Ethical approval was considered unnecessary as this study is a review of existing, peer-reviewed literature and did not involve any handling of individual patient data.
Search methodology
Two investigators (WR, LRY) independently searched PubMed, OVID, and ScienceDirect databases prior to December 2018 without limitation on language or publication status. The following search terms were used: “total joint arthroplasty”, “total joint replacement”, “total hip arthroplasty”, “total hip replacement”, “total knee arthroplasty”, “total knee replacement”, “TJA”, “TJR”, “THA”, “THR”, “TKA”, “TKR”, “metabolic syndrome”, “insulin-resistance syndrome”, “syndrome X”, and “MetS”. References cited in articles found in the search were also manually searched for additional relevant articles. Language experts were contacted for translation of studies that were not written in English.
Study selection criteria
Studies were included in this meta-analysis if they were cohort studies investigating the impact of MetS on postoperative complications following THA or TKA. Studies were excluded if they were not controlled (e.g. case reports or case series), were published only in abstract form, evaluated the impact of an individual aspect of MetS rather than the syndrome as a whole, or involved patients who underwent hemiarthroplasty, unicompartmental knee arthroplasty, or arthroscopic surgery.
Literature selection
Potentially relevant studies were imported into Endnote X7 (Thomson Scientific, Stamford, Connecticut, USA) and duplicate records were removed. The two investigators (WR, LRY) who had performed the literature search then independently excluded irrelevant studies based on titles and abstracts, read the full texts of the remaining articles, and excluded those that did not meet selection criteria to produce a final list of studies. Discrepancies between the two investigators were resolved by discussion with a third author (WKZ).
Data extraction and assessment of study quality
Two investigators (WR, LRY) independently extracted the following data from each eligible study: first author name, publication year, sample size, study type, Newcastle-Ottawa Scale (NOS) score, clinical definition of MetS, and incidence of complications. The outcomes of interest included all-cause complications, circulatory complications, urinary complications, pulmonary complications, gastrointestinal complications, surgical site infection (SSI), mortality, and 30-day readmission. Circulatory complications were defined as the following: cardiovascular events and VTEs, which included deep vein thrombosis and pulmonary embolism; urinary complications, which were referred to as urinary tract infections (UTIs); and SSI, including superficial and prosthetic infections.
We used the NOS score to evaluate the methodological quality of each study.24 The NOS score is a validated, widely used tool for evaluating the quality of observational studies based on the methods used to select the study groups (zero to four points), the comparability of cases and controls (zero to two points), and the method used to ascertain the outcome of interest (zero to three points). The maximum total points was nine, and this meta-analysis included only the studies deemed of moderate or high methodological quality (at least five points). We assessed the quality of evidence using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) in GRADEpro 3.6 (GRADE Working Group). The quality of evidence for each outcome was categorized as high, moderate, low, or very low25,26 based on the study limitations, inconsistent results, indirectness of evidence, imprecision, and publication bias. Quality of evidence was evaluated by two researchers (WR, LRY) independently, and any discrepancies were resolved by discussion with a third researcher (WKZ).
Statistical analysis
Outcomes were synthesized qualitatively if data could not be directly compared across studies, or if the studies reported insufficient data. Outcomes for sufficient, comparable data reported across studies were meta-analyzed and displayed as forest plots using RevMan 5.2 (The Cochrane Collaboration, Oxford, UK). All evaluated data were dichotomous, and effects were expressed as risk ratios (RRs) with 95% confidence intervals (95% CIs). We used a random-effects meta-analysis model, which can incorporate heterogeneity, because we anticipated that there would be interstudy variability due to differing definitions of MetS. The I2 test was used to examine heterogeneity across studies. Heterogeneity was defined as absent (I2 = 0.0% to 25.0%), low (I2 = 25.1% to 50.0%), moderate (I2 = 50.1% to 75.0%), or high (I2 = 75.1% to 100.0%). Once all outcomes were evaluated, a summary table was created using GRADEpro.
Results
Search results and characteristics of included studies
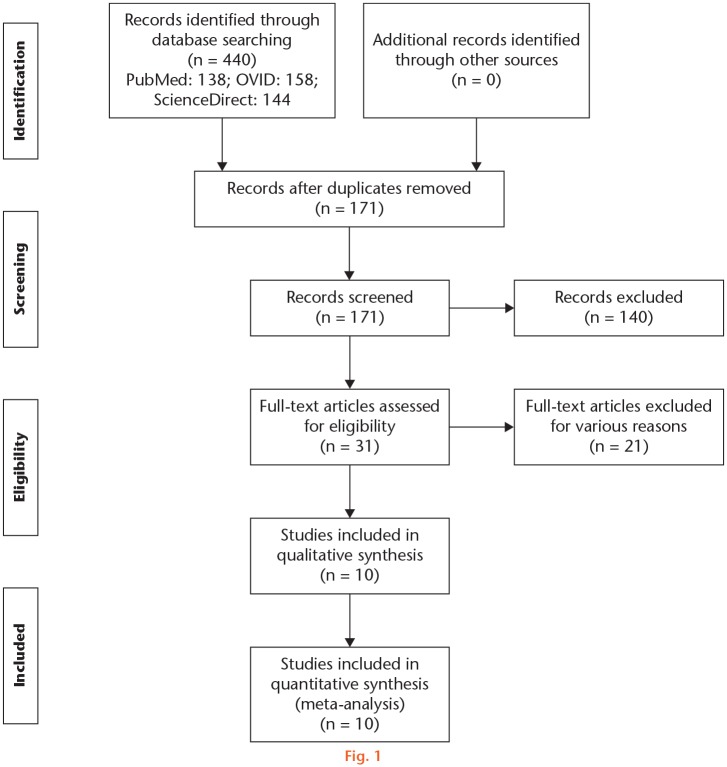
A total of 440 records were identified, with no additional records identified by manually searching references. Screening using Endnote X7 removed 269 duplicates, and 140 records were excluded as irrelevant after reading titles and abstracts. A further 21 records failed to meet selection criteria and were removed. Finally, ten studies involving 1,352,685 cases were included for meta-analysis. The details of study identification, inclusion, and exclusion are shown in Figure 1.
Fig. 1.
Flowchart of study identification, screening, and selection.
Of the ten studies, one was a prospective cohort study22 and nine were retrospective cohort studies.18–21,27–31 All were published within the last ten years, including six studies published within the last five years. Seven studies were conducted at a single centre, and the other three studies at multiple centres.18,29,30 Nine studies assessed the impact of MetS on postoperative outcomes following both THA and TKA, while one study assessed only TKA.22 Although the definition of MetS differed slightly across studies, the presence of obesity, diabetes (insulin resistance or dysglycemia), hypertension, and dyslipidemia were common criteria, except for one study that utilized sleep apnoea as a surrogate for obesity.19 The NOS quality score of the ten included studies ranged from six to eight points. Table I provides a detailed description of the study characteristics and participants, and Table II provides a summary of outcomes data. The details of study identification, inclusion, and exclusion are shown in Figure 1.
Table I.
Description of studies and participants
| Reference | Surgery | Sample size (MetS vs control) | Follow-up | Definition of MetS | Study type | NOS score |
|---|---|---|---|---|---|---|
| Gandhi et al (2009) 22 | TKA | 1,460 (135 vs 1,325) | 3 mths | Obesity, hypertension, diabetes, and dyslipidemia | P-Co, S | 8 |
| Edelstein et al (2017) 18 | THA/TKA | 107,117 (11,030 vs 96,087) | 1 mth | Obesity, hypertension, and diabetes | R-Co, M | 7 |
| Gage et al (2014) 27 | THA/TKA | 168 (39 vs 129) | 1 yr | International Diabetes Foundation criteria* | R-Co, S | 7 |
| Mraovic et al (2013) 20 | THA/TKA | 7,282 (958 vs 6,324) | Unclear | Obesity, hypertension, dysglycemia, and dyslipidemia | R-Co, S | 6 |
| Song et al (2016) 31 | THA/TKA | 1,553 (79 vs 1,474) | 1 mth | World Health Organization criteria† | R-Co, S | 8 |
| Edelstein et al (2016) 19 | THA/TKA | 1,462 (237 vs 1,225) | 1 mth | Three criteria of diabetes, hypertension, dyslipidemia, and sleep apnoea | R-Co, S | 7 |
| Zmistowski et al (2013) 28 | THA/TKA | 257 (35 vs 101 vs 121)‡ | Unclear | Obesity, hypertension, diabetes, and dyslipidemia | R-Co, S | 7 |
| Gandhi et al (2012) 21 | THA/TKA | 4,132 (1,132 vs 3,000) | Hospitalization | Three criteria of obesity, hypertension, diabetes, and dyslipidemia | R-Co, S | 6 |
| Dy et al (2011) 29 | THA/TKA | 16,317 | Mean 48 mths (24 to 71) | Obesity, hypertension, diabetes, and dyslipidemia | R-Co, M | 7 |
| Gonzalez Della Valle et al (2012) 30 | THA/TKA | 1,212,937 (107,121 vs 1,105,816) | Hospitalization | Three criteria of obesity, hypertension, diabetes, and dyslipidemia | R-Co, M | 7 |
International Diabetes Foundation criteria for metabolic syndrome: body mass index > 30 kg/m2 plus three of the following conditions: elevated triglycerides, reduced high-density lipoprotein, hypertension, or diabetes.
World Health Organization criteria for metabolic syndrome: insulin resistance plus two of the following conditions: body mass index > 30 kg/m2, hypertension and/or antihypertensive medication, high-density lipoprotein cholesterol < 35 mg/dl in men or < 39 mg/dl in women, or triglycerides ≥ 150 mg/dl.
Uncontrolled versus controlled versus nonmetabolic syndrome patients.
M, multicentre; MetS, metabolic syndrome; NOS, Newcastle-Ottawa Scale; P-Co, prospective cohort study; R-Co, retrospective cohort study; S, single-centre; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Table II.
Summary of outcomes between metabolic syndrome and nonmetabolic syndrome patients after total hip or knee arthroplasty
| Reference | Outcomes assessed | Summary of postoperative outcomes between groups |
|---|---|---|
| Gandhi et al (2009) 22 | Deep vein thrombosis. | The risk of symptomatic deep vein thrombosis in patients with MetS was 3.2 times that of patients without MetS at three-month follow-up. |
| Edelstein et al (2017) 18 | All-cause complications, wound complications, readmission. | MetS was associated with increased risk of all-cause complications, wound complications, and readmission within 30 days after surgery. |
| Gage et al (2014) 27 | All-cause complications. | MetS increased the risk of all-cause complications during hospitalization and within one year after surgery. |
| Mraovic et al (2013) 20 | Pulmonary embolism. | Patients with MetS were at higher risk of pulmonary embolism than patients without MetS. |
| Song et al (2016) 31 | Deep vein thrombosis. | MetS increased the risk of deep vein thrombosis within 30 days of surgery. |
| Edelstein et al (2016) 19 | All-cause complications, pulmonary complications, cardiac events, pulmonary embolism, SSI, UTI, readmission. | MetS increased the risk of all-cause complications, cardiac events, pulmonary embolism, SSI, and UTI at one-month follow-up, with no difference in pulmonary complications or readmission. |
| Zmistowski et al (2013) 28 | All-cause complications, periprosthetic complications, deep vein thrombosis, pulmonary embolism, cardiac events, UTI, small bowel obstruction, one- and two-year mortality. | Uncontrolled MetS patients showed greater incidence of all-cause complications, cardiac events, pulmonary embolism, and prosthetic joint infection than patients with controlled MetS and patients without MetS. However, not all differences were significantly different between the controlled MetS and non-MetS groups. |
| Gandhi et al (2012) 21 | Cardiovascular complications, pulmonary embolism, deep vein thrombosis. | Patients with MetS were at higher risk of cardiovascular complications and pulmonary embolism than patients without MetS during hospitalization, with no difference in risk of deep vein thrombosis. |
| Dy et al (2011) 29 | Myocardial infarction and VTE. | Patients with MetS were at higher risk of myocardial infarction and VTE than patients without MetS. |
| Gonzalez Della Valle (2012) 30 | Cardiac events, pulmonary complications, VTE, in-hospital mortality. | MetS was associated with increased risk of cardiac events after THA and TKA, and pulmonary complications after TKA. There was no difference in VTE risk. All-cause in-hospital mortality was lower among MetS patients than non-MetS patients. |
MetS, metabolic syndrome; SSI, surgical site infection; THA, total hip arthroplasty; TKA, total knee arthroplasty; UTI, urinary tract infection; VTE, venous thromboembolism.
Outcomes assessments
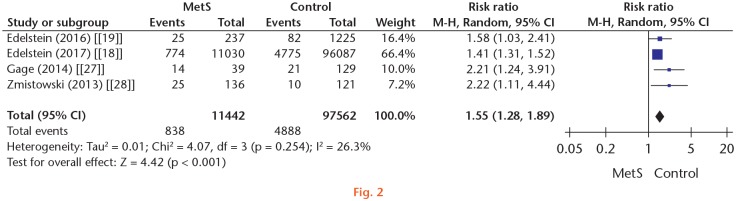
All-cause complications: data on all-cause complications following THA and TKA were extracted from four studies involving 109,004 patients.18,19,27,28 Heterogeneity among the four studies was low (p = 0.254, I2 = 26.3%, forest plot). Meta-analysis showed that patients with MetS had a significantly higher risk of all-cause complications than patients without MetS (RR 1.55, 95% CI 1.28 to 1.89; Figure 2). The quality of evidence (GRADE) was low (Table III).
Fig. 2.
Forest plot of all-cause complications. CI, confidence interval; M-H, Mantel-Haenszel; MetS, metabolic syndrome; Random, random-effects modelling.
Table III.
Summarized outcomes in Grading of Recommendations Assessment, Development, and Evaluation. MetS patients were compared to non-Mets patients for complications after total hip arthroplasty and total knee arthroplasty
| Outcome | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE)† | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk; non-MetS | Corresponding risk; MetS | |||||
| All-cause complications | 50 per 1,000 | 78 per 1,000 (64 to 95) | RR 1.55 (1.28 to 1.89) | 109,004 (4 studies) | ⊕⊕⊝⊝ low | N/A |
| Cardiovascular events | See comment | See comment | N/A | 0 (5) | See comment | Data not presented in a format to allow meta-analysis. Studies found that MetS was associated with higher risk of cardiovascular events. |
| VTE | See comment | See comment | N/A | 0 (8) | See comment | Data not presented in a format to allow meta-analysis. Results are inconsistent across studies. |
| Urinary tract infection | 9 per 1,000 | 24 per 1,000 (9 to 58) | RR 2.64 (1.06 to 6.55) | 1,719 (2) | ⊕⊕⊝⊝ low‡ § | N/A |
| Pulmonary complications | See comment | See comment | N/A | 0 (2) | See comment | Data not presented in a format to allow meta-analysis. Results are inconsistent across studies. |
| Gastrointestinal complications | See comment | See comment | N/A | 0 (1) | See comment | Data not presented in a format to allow meta-analysis. One study found similar incidence of small bowel obstruction between groups. |
| Surgical site infection | 10 per 1,000 | 31 per 1,000 (14 to 72) | RR 2.99 (1.30 to 6.90) | 1,719 (3) | ⊕⊕⊕⊝ moderate§ | N/A |
| Readmission | 31 per 1,000 | 45 per 1,000 (42 to 50) | RR 1.45 (1.33 to 1.59) | 108,579 (2) | ⊕⊝⊝⊝ very low¶ | N/A |
| Mortality | See comment | See comment | N/A | 0 (2) | See comment | Data not presented in a format to allow meta-analysis. Studies found lower in-hospital mortality in the MetS group, but similar one- and two-year mortality between the MetS and non-MetS groups. |
The basis for the assumed risk (e.g. the median control group risk across studies) is provided in the footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
Grading of Recommendations Assessment, Development, and Evaluation Working Group grades of evidence: high quality, further research is very unlikely to change our confidence in the estimate of effect; moderate quality, further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low quality, further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate, very low quality, we are very uncertain about the estimate.
Inconsistent results across studies.
Risk ratio > 2.
Inconsistent results across studies.
CI, confidence interval; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; MetS, metabolic syndrome; N/A, not applicable; RR, risk ratio; VTE, venous thromboembolism.
Circulatory complications
Cardiovascular events: a total of five studies involving 1,235,105 patients reported the incidence of cardiovascular events,19,21,28–30 although the definition of cardiovascular events varied substantially in different studies. All five studies found that MetS was associated with a higher risk of cardiovascular events after THA and TKA. One study21 defined cardiovascular events as nine complications, among them atrial fibrillation, arrhythmia, bradycardia, cardiac arrest, and myocardial infarction. The study reported that patients with MetS had a higher cumulative risk of cardiovascular events than those without MetS (odds ratio (OR) 1.64; 95% CI 1.09 to 2.46). A second study reported significantly higher risk of myocardial infarction and cardiac complications in the MetS group than in the control group, although they did not give a clear definition of cardiac complications.30 A third study found that uncontrolled MetS, but not controlled MetS, led to significantly higher incidence of cardiac events than in non-MetS patients (8.6% vs 0.8%), although cardiac events in this study were also not clearly defined.28 A fourth study reported twofold higher risk of postoperative myocardial infarction in patients with MetS.29 The remaining study also showed a higher incidence of myocardial infarction in the MetS group than in the control group (2.5% vs 1.9%), although the difference was not statistically significant.19
Venous thromboembolism events: incidence of VTEs was assessed in eight studies involving 1,245,400 patients.19–22,28–31 Table IV shows detailed information on VTE prophylaxis, diagnosis, assessment timepoints, incidence, and effect size in each study. Meta-analysis was not possible due to significant heterogeneity in thrombosis type, assessment method, and timepoints. In brief, approximately half of studies reported an association between MetS and VTE after THA or TKA. Dy et al29 reported that MetS patients were more than three times more likely to experience postoperative VTE than patients without MetS, while Della Valle et al30 reported no difference. Another two out of four studies reported that MetS increased the risk of deep vein thrombosis by more than threefold22 or by 1.14- to 4-fold.31 In contrast, Zmistowski et al28 and Gandhi et al21 found that pulmonary embolism, but not deep vein thrombosis, was associated with MetS.21,28 Mraovic et al20 also reported that MetS increased the risk of pulmonary embolism by 1.6-fold, but Edelstein et al19 found no difference in pulmonary embolism incidence between MetS and non-MetS patients.
Table IV.
Details of studies comparing venous thromboembolism events after total knee or hip arthroplasty in patients with or without metabolic syndrome
| Study | Follow-up length | Diagnostic method | Prophylaxis used | Incidence (MetS vs control, %) | Risk estimate (95% CI) | MetS increases thrombus risk? |
|---|---|---|---|---|---|---|
| Venous thrombolism events (including deep vein thrombosis and pulmonary embolism) | ||||||
| Dy et al (2011) 29 | Mean four years | Unclear | Unclear | Not reported | HR 3.20 (0.99 to 10.23)* | Yes |
| Gonzalez Della Valle (2012) 30 | Hospitalization | Unclear | Unclear | THA: 0.47 vs 0.49; TKA: 0.74 vs 0.81 | Not reported | No |
| Deep vein thrombosis | ||||||
| Gandhi et al (2012) 21 | Hospitalization | Doppler ultrasound | Unclear | Not reported | Not reported | No |
| Song et al (2016) 31 | One month | Clinical symptom venography | Rivaroxaban or LMWH | THA: 23.5 vs 18.8 (T) / 14.7 vs 5.0 (S); TKA: 42.2 vs 24.8 (T) / 13.3 vs 3.7 (S) | THA: OR 1.14 (0.50 to 2.59)† / OR 2.96 (1.08 to 8.11); TKA: OR 2.25 (1.19 to 4.22) / OR 4.18 (1.54 to 11.32) | Yes |
| Zmistowski et al (2013) 28 | Unclear | Unclear | Unclear | 2.9 vs 1.0 vs 0.0‡ | Not reported | No |
| Gandhi et al (2009) 22 | Three months | Ultrasound plus clinical symptom | LMWH | 15.5 vs 4.5 (S) | OR 3.2 (1.0-15.4)† | Yes |
| Pulmonary embolism | ||||||
| Zmistowski et al (2013) 28 | Unclear | Unclear | Unclear | 11.4 vs 1.0 vs 0.0‡ | Not reported | Yes |
| Gandhi et al (2012) 21 | Hospitalization | Lung CT or ventilation-perfusion scan | Unclear | Not reported | Not reported | Yes |
| Edelstein et al (2016) 19 | One month | Unclear | Warfarin | 1.3 vs 2.4 | Not reported | No |
| Mraovic et al (2013) 20 | Unclear | Lung CT or ventilation-perfusion scan | Warfarin | 3.09 vs 0.85 | OR 1.61 (1.01 to 2.56)† | Yes |
Effect size was calculated by Cox proportional hazards regression modelling.
Effect size was calculated by multivariate logistic regression analysis.
Uncontrolled versus controlled versus nonmetabolic syndrome patients.
CI, confidence interval; HR, hazard ratio; LMWH, low-molecular-weight heparin; MetS, metabolic syndrome; OR, odds ratio; S, symptomatic deep vein thrombosis; T, total deep vein thrombosis; THA, total hip arthroplasty; TKA, total knee arthroplasty.
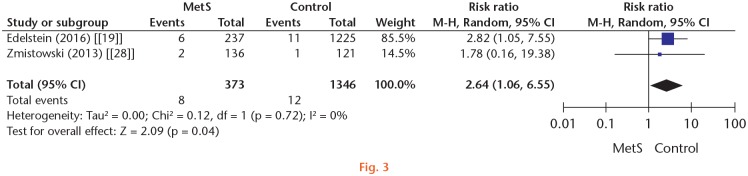
Urinary complications: UTI incidence was investigated in two studies involving 1,719 patients.19,28 Meta-analysis showed that patients with MetS were at higher risk of postoperative UTI than non-MetS patients (pooled RR 2.64, 95% CI 1.06 to 6.55, I2 = 0%; Figure 3). The quality of evidence (GRADE) was low (Table III).
Fig. 3.
Forest plot of urinary tract infection. CI, confidence interval; M-H, Mantel-Haenszel; MetS, metabolic syndrome; Random, random-effects modelling.
Pulmonary complications: pulmonary complications were assessed in two studies involving 1,214,399 patients.19,30 One study found that TKA patients with MetS, but not THA patients with MetS, had a higher incidence of pulmonary complications after surgery than patients without MetS.30 In contrast, Edelstein et al19 reported no difference in the incidence of postoperative pulmonary complications between patients with or without MetS who underwent THA or TKA.
Gastrointestinal complications: gastrointestinal complications were assessed in one study with 257 patients. This study found no difference in the incidence of small bowel obstruction between patients with or without MetS after THA or TKA.28
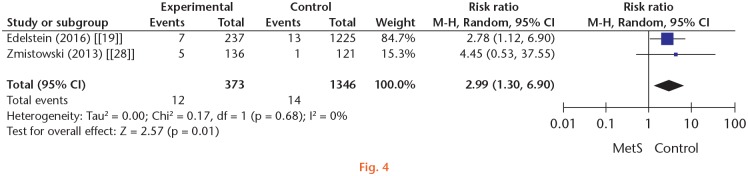
Surgical site infection: SSI was assessed in two studies involving 1,719 patients.19,28 Meta-analysis showed that MetS significantly increased the risk of SSI after TKA or THA (pooled RR 2.99, 95% CI 1.30 to 6.90, I2 = 0%; Figure 4). The quality of evidence (GRADE) was moderate (Table III).
Fig. 4.
Forest plot of surgical site infection. CI, confidence interval; M-H, Mantel-Haenszel; MetS, metabolic syndrome; Random, random-effects modelling.
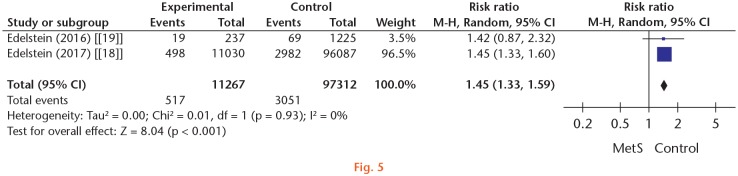
Readmission and mortality: readmission within a 30-day follow-up was assessed in two studies, with a combined total of 108,579 patients.18,19 Meta-analysis showed that patients with MetS were at significantly higher risk of 30-day readmission (pooled RR 1.45, 95% CI 1.33 to 1.59, I2 = 0%; Figure 5). The quality of evidence (GRADE) was very low (Table III). Another two studies involving 1,213,194 patients reported that patients with MetS had lower overall in-hospital mortality than patients without MetS,30 but there was no difference in mortality within two years after surgery.28
Fig. 5.
Forest plot of 30-day readmission. CI, confidence interval; M-H, Mantel-Haenszel; MetS, metabolic syndrome; Random, random-effects modelling.
Discussion
Metabolic syndrome is known to be associated with an increased risk of postoperative complications.11–15 Recent studies have begun to link MetS with complications after THA and TKA, but the results are still controversial. In this study, we performed a systematic review and meta-analysis to identify MetS-related complications after THA and TKA. The available evidence suggests that MetS increases the risk of all-cause complications, cardiovascular complications, SSI, UTI, and 30-day readmission.
Metabolic syndrome is a pathological condition which comprises a cluster of abnormal metabolism-related components. Although it often arises in obese patients, MetS is not a consequence of obesity but rather a distinct state characterized by low-grade inflammation, and should be regarded as an independent risk factor for many diseases and surgical complications.32–35 It appears that low-grade inflammation accompanied by higher than normal circulating levels of inflammatory cytokines is a central feature of MetS.36,37 Elevations in systemic inflammatory biomarkers such as CRP and tumour necrosis factor-α (TNF-α) contribute to increased risk of various diseases and surgical complications.35,36
Our results show that patients with MetS are more likely to experience cardiovascular complications after THA and TKA than those without MetS. The persistent systemic inflammation in MetS is thought to increase cardiovascular risk by inducing endothelial cell dysfunction36,38 and activating monocytes.39 One possibility is that physiological stress caused by surgery may accelerate or potentiate the pathophysiological processes that lead to an acute occurrence of cardiovascular events after surgery.29 The studies included in our analysis found that MetS increases the risk of postoperative cardiovascular events either during hospitalization21,30 or at mean follow-up of 48 months.29 In addition, the risk of cardiovascular events increased with the number of MetS symptoms present, and the overall risk may be greater than the sum of the risks associated with the individual symptoms present.21,29
Recent studies have reported that MetS increases the risk of wound infection in several surgical conditions.32,37 In this study, the results of meta-analyses show that MetS is associated with a higher incidence of both SSI and UTI after THA and TKA. MetS has been reported to have a substantial negative impact on immunity and pathogen defence, including: the disruption of lymphoid tissue integrity; alterations in leucocyte development, phenotypes, and activity; and the coordination of innate and adaptive immune responses.40 Patients with MetS may therefore be at higher risk of infection due to systemic immune dysfunction. The elevated risk of SSI and systemic UTI support the idea that systemic factors increase susceptibility to postoperative infection in MetS patients. Importantly, those previous studies did not analyze the incidence of superficial and prosthetic infections separately.19,28 Further research is needed to determine whether MetS differentially affects the risk of these two types of infections.
The relationship between MetS and VTE is still controversial. Reports indicate that chronic inflammation in MetS patients increases plasma levels of fibrinogen, soluble tissue factor, and factor VII, which promote activation of the coagulation cascade.41,42 Increased levels of plasminogen activator inhibitor-1 (PAI-1) and decreased activity of tissue-type plasminogen activator (t-PA) produce a hypofibrinolytic state,41–43 which could increase the risk of VTE in MetS patients. In support of this, some studies have reported increased thrombosis susceptibility in MetS patients.4,44,45 However, others have reached different conclusions.30,46 Thromboprophylaxis strongly influences the incidence of VTE in patients undergoing arthroplasty,47,48 so understanding thromboprophylaxis history of arthroplasty patients is key to assessing the potential relationship between MetS and VTE. However, most studies in our analysis did not describe the prophylactic strategies used by patients,19,21,28–30 and the studies varied substantially in assessment methods and timepoints. As a result, the impact of MetS on risk of VTE after THA or TKA remains unclear based on the available clinical evidence. We suggest that effective thromboprophylaxis measures be given to MetS patients, but we are unable to assess whether thromboprophylaxis intensity should be higher for MetS patients than for non-MetS patients. Further studies on VTE in MetS patients should include detailed descriptions of thromboprophylaxis strategies, VTE diagnostic methods, and assessment timepoints.
Our systematic review found a higher incidence of 30-day readmission in patients with MetS but did not find evidence of an association between MetS and pulmonary or gastrointestinal complications. Interestingly, one study found that MetS patients had lower in-hospital mortality than non-MetS patients, despite higher complication rates.30 Those authors suggested that this may be because MetS patients are subjected to more rigorous preoperative testing and monitoring after surgery due to higher complication rates.
One study in our review reported that the effective control of MetS components (diabetes, hypertension, and dyslipidemia) can decrease the risk of perioperative complications in arthroplasty patients.28 Although that study involved only 257 patients, the result suggests that it is important to control MetS components before surgery. Further work is needed to verify this finding.
Our study has several limitations. First, several outcomes could not be meta-analyzed due to significant heterogeneity between studies in the definition of complications, assessment method, and the timepoints. The fact that we could only qualitatively synthesize these outcomes makes our conclusions less robust. Second, the risk of some complications such as VTE remains elevated for a substantial period after arthroplasty, but several studies in our sample examined outcomes only during hospitalization21,30 or up to one month after surgery,18,19,31 which may not be long enough to accurately assess their occurrence. Third, functional outcomes are important to prognosis and quality of life, yet we did not find any valuable data on these outcomes to perform the meta-analysis or systematic review, which is also a limitation in our review.
Given the increasing clinical interest of this question and the limitations of current research, more prospective study in this field is needed. Future work should pay particular attention to the outcomes that our comprehensive review could not quantitatively address (e.g. VTE), and should also evaluate the functional outcomes, preferably with mid- to long-term follow-up. In addition, since we focused here on MetS as a single entity, yet the individual components may influence postoperative outcomes quite differently,27,31 future work should apply logistic regression and other statistical models to identify the specific component(s) of MetS most strongly associated with the outcome of interest.
In conclusion, this systematic review and meta-analysis provides an up-to-date overview of the impact of MetS on surgical complications after TKA or THA. We find that MetS is associated with an increased risk of all-cause complications, cardiovascular complications, SSI, UTI, and 30-day readmission, but the evidence is still insufficient to verify a relationship between MetS and VTE. Surgeons should be aware of these increased risks, and presurgical protocols should be developed to prevent and minimize the risk of complications in MetS patients undergoing TKA or THA.
Acknowledgments
We thank Dr GuoRui Cao for discussions and A. Chapin Rodríguez, PhD for English language editing.
Footnotes
Author contributions: C. Guofeng: Drafted and revised the manuscript, Co-first author.
Y. Chen: Drafted and revised the manuscript, Co-first author.
W. Rong: Searched the literature, Processed the data.
L. Ruiyu: Searched the literature, Processed the data.
W. Kunzheng: Conceived the study and served as guarantor, taking responsibility for the integrity of the work as a whole from inception to published article.
Ethical review statement: This study did not require ethical approval.
Follow us @BoneJointRes
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Sherling DH, Perumareddi P, Hennekens CH. Metabolic Syndrome. J Cardiovasc Pharmacol Ther. 2017;22(4):365-367. [DOI] [PubMed] [Google Scholar]
- 2. Xie DX, Wei J, Zeng C, et al. Association between metabolic syndrome and knee osteoarthritis: a cross-sectional study. BMC Musculoskelet Disord. 2017;18(1):533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnson LW, Weinstock RS. The metabolic syndrome: concepts and controversy. Mayo Clin Proc. 2006;81(12):1615-1620. [DOI] [PubMed] [Google Scholar]
- 4. Jang MJ, Choi WI, Bang SM, et al. Metabolic syndrome is associated with venous thromboembolism in the Korean population. Arterioscler Thromb Vasc Biol. 2009;29(3):311-315. [DOI] [PubMed] [Google Scholar]
- 5. Bray GA, Bellanger T. Epidemiology, trends, and morbidities of obesity and the metabolic syndrome. Endocrine. 2006;29(1):109-117. [DOI] [PubMed] [Google Scholar]
- 6. Alberti KG, Eckel RH, Grundy SM, et al. ; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640-1645. [DOI] [PubMed] [Google Scholar]
- 7. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143-3421. [PubMed] [Google Scholar]
- 8. Hajat C, Shather Z. Prevalence of metabolic syndrome and prediction of diabetes using IDF versus ATPIII criteria in a Middle East population. Diabetes Res Clin Pract. 2012;98(3):481-486. [DOI] [PubMed] [Google Scholar]
- 9. Meigs JB, Wilson PW, Nathan DM, D’Agostino RB, Sr, Williams K, Haffner SM. Prevalence and characteristics of the metabolic syndrome in the San Antonio Heart and Framingham Offspring Studies. Diabetes. 2003;52(8):2160-2167. [DOI] [PubMed] [Google Scholar]
- 10. Deedwania PC, Gupta R, Sharma KK, et al. High prevalence of metabolic syndrome among urban subjects in India: a multisite study. Diabetes Metab Syndr. 2014;8(3):156-161. [DOI] [PubMed] [Google Scholar]
- 11. Ardeshiri M, Faritus Z, Ojaghi-Haghighi Z, Bakhshandeh H, Kargar F, Aghili R. Impact of metabolic syndrome on mortality and morbidity after coronary artery bypass grafting surgery. Res Cardiovasc Med. 2014;3(3):e20270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Angeloni E, Melina G, Benedetto U, et al. Metabolic syndrome affects midterm outcome after coronary artery bypass grafting. Ann Thorac Surg. 2012;93(2):537-544. [DOI] [PubMed] [Google Scholar]
- 13. Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology. 2010;113(4):859-872. [DOI] [PubMed] [Google Scholar]
- 14. Cichos KH, Churchill JL, Phillips SG, et al. Metabolic syndrome and hip fracture: epidemiology and perioperative outcomes. Injury. 2018;49(11):2036-2041. [DOI] [PubMed] [Google Scholar]
- 15. Menendez ME, Neuhaus V, Bot AG, Ring D, Johnson AH. The impact of metabolic syndrome on inpatient outcomes after isolated ankle fractures. Foot Ankle Int. 2014;35(5):463-470. [DOI] [PubMed] [Google Scholar]
- 16. NIH Consensus Panel. NIH Consensus Statement on total knee replacement December 8-10, 2003. J Bone Joint Surg Am. 2004;86-A(6):1328-1335. [DOI] [PubMed] [Google Scholar]
- 17. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89-A(4):780-785. [DOI] [PubMed] [Google Scholar]
- 18. Edelstein AI, Lovecchio F, Delagrammaticas DE, Fitz DW, Hardt KD, Manning DW. The Impact of Metabolic Syndrome on 30-Day Complications Following Total Joint Arthroplasty. J Arthroplasty. 2017;32(2):362-366. [DOI] [PubMed] [Google Scholar]
- 19. Edelstein AI, Suleiman LI, Alvarez AP, et al. The Interaction of Obesity and Metabolic Syndrome in Determining Risk of Complication Following Total Joint Arthroplasty. J Arthroplasty. 2016;31(9 Suppl):192-196. [DOI] [PubMed] [Google Scholar]
- 20. Mraovic B, Hipszer BR, Epstein RH, et al. Metabolic syndrome increases risk for pulmonary embolism after hip and knee arthroplasty. Croat Med J. 2013;54(4):355-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gandhi K, Viscusi ER, Schwenk ES, Pulido L, Parvizi J. Quantifying cardiovascular risks in patients with metabolic syndrome undergoing total joint arthroplasty. J Arthroplasty. 2012;27(4):514-519. [DOI] [PubMed] [Google Scholar]
- 22. Gandhi R, Razak F, Tso P, Davey JR, Mahomed NN. Metabolic syndrome and the incidence of symptomatic deep vein thrombosis following total knee arthroplasty. J Rheumatol. 2009;36(10):2298-2301. [DOI] [PubMed] [Google Scholar]
- 23. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012. [DOI] [PubMed] [Google Scholar]
- 24. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. The Ottawa Hospital Research Institute. 2011. www.ohri.ca/prograMetS/clinical_epidemiology/oxford.asp (date last accessed 16 January 2020).
- 25. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380-382. [DOI] [PubMed] [Google Scholar]
- 26. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383-394. [DOI] [PubMed] [Google Scholar]
- 27. Gage MJ, Schwarzkopf R, Abrouk M, Slover JD. Impact of metabolic syndrome on perioperative complication rates after total joint arthroplasty surgery. J Arthroplasty. 2014;29(9):1842-1845. [DOI] [PubMed] [Google Scholar]
- 28. Zmistowski B, Dizdarevic I, Jacovides CL, Radcliff KE, Mraovic B, Parvizi J. Patients with uncontrolled components of metabolic syndrome have increased risk of complications following total joint arthroplasty. J Arthroplasty. 2013;28(6):904-907. [DOI] [PubMed] [Google Scholar]
- 29. Dy CJ, Wilkinson JD, Tamariz L, Scully SP. Influence of preoperative cardiovascular risk factor clusters on complications of total joint arthroplasty. Am J Orthop (Belle Mead NJ). 2011;40(11):560-565. [PubMed] [Google Scholar]
- 30. Gonzalez Della Valle A, Chiu YL, Ma Y, Mazumdar M, Memtsoudis SG. The metabolic syndrome in patients undergoing knee and hip arthroplasty: trends and in-hospital outcomes in the United States. J Arthroplasty. 2012;27(10):1743-1749.e1. [DOI] [PubMed] [Google Scholar]
- 31. Song K, Rong Z, Yao Y, Shen Y, Zheng M, Jiang Q. Metabolic Syndrome and Deep Vein Thrombosis After Total Knee and Hip Arthroplasty. J Arthroplasty. 2016;31(6):1322-1325. [DOI] [PubMed] [Google Scholar]
- 32. Lovecchio F, Fu MC, Iyer S, Steinhaus M, Albert T. Does Obesity Explain the Effect of the Metabolic Syndrome on Complications Following Elective Lumbar Fusion? A Propensity Score Matched Analysis. Global Spine J. 2018;8(7):683-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28(7):1769-1778. [DOI] [PubMed] [Google Scholar]
- 34. Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709-2716. [DOI] [PubMed] [Google Scholar]
- 35. McCracken E, Monaghan M, Sreenivasan S. Pathophysiology of the metabolic syndrome. Clin Dermatol. 2018;36(1):14-20. [DOI] [PubMed] [Google Scholar]
- 36. Devaraj S, Valleggi S, Siegel D, Jialal I. Role of C-reactive protein in contributing to increased cardiovascular risk in metabolic syndrome. Curr Atheroscler Rep. 2010;12(2):110-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ozyazicioglu A, Yalcinkaya S, Vural AH, Yumun G, Bozkurt O. Effects of metabolic syndrome on early mortality and morbidity in coronary artery bypass graft patients. J Int Med Res. 2010;38(1):202-207. [DOI] [PubMed] [Google Scholar]
- 38. Suzuki T, Hirata K, Elkind MS, et al. Metabolic syndrome, endothelial dysfunction, and risk of cardiovascular events: the Northern Manhattan Study (NOMAS). Am Heart J. 2008;156(2):405-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fortuño A, San José G, Moreno MU, Beloqui O, Díez J, Zalba G. Phagocytic NADPH oxidase overactivity underlies oxidative stress in metabolic syndrome. Diabetes. 2006;55(1):209-215. [DOI] [PubMed] [Google Scholar]
- 40. Andersen CJ, Murphy KE, Fernandez ML. Impact of Obesity and Metabolic Syndrome on Immunity. Adv Nutr. 2016;7(1):66-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dentali F, Squizzato A, Ageno W. The metabolic syndrome as a risk factor for venous and arterial thrombosis. Semin Thromb Hemost. 2009;35(5):451-457. [DOI] [PubMed] [Google Scholar]
- 42. Ageno W, Di Minno MN, Ay C, et al. Association between the metabolic syndrome, its individual components, and unprovoked venous thromboembolism: results of a patient-level meta-analysis. Arterioscler Thromb Vasc Biol. 2014;34(11):2478-2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Meltzer ME, Lisman T, de Groot PG, et al. Venous thrombosis risk associated with plasma hypofibrinolysis is explained by elevated plasma levels of TAFI and PAI-1. Blood. 2010;116(1):113-121. [DOI] [PubMed] [Google Scholar]
- 44. Ambrosetti M, Ageno W, Salerno M, Pedretti RF, Salerno-Uriarte JA. Metabolic syndrome as a risk factor for deep vein thrombosis after acute cardiac conditions. Thromb Res. 2007;120(6):815-818. [DOI] [PubMed] [Google Scholar]
- 45. Rattazzi M, Villalta S, Galliazzo S, et al. Low CD34(+) cells, high neutrophils and the metabolic syndrome are associated with an increased risk of venous thromboembolism. Clin Sci (Lond). 2013;125(4):211-218. [DOI] [PubMed] [Google Scholar]
- 46. Steffen LM, Cushman M, Peacock JM, et al. Metabolic syndrome and risk of venous thromboembolism: Longitudinal Investigation of Thromboembolism Etiology. J Thromb Haemost. 2009;7(5):746-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Azboy I, Barrack R, Thomas AM, Haddad FS, Parvizi J. Aspirin and the prevention of venous thromboembolism following total joint arthroplasty: commonly asked questions. Bone Joint J. 2017;99-B(11):1420-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Goel R, Fleischman AN, Tan T, et al. Venous thromboembolic prophylaxis after simultaneous bilateral total knee arthroplasty: aspirin versus warfarin. Bone Joint J. 2018;100-B(1 Supple A):68-75. [DOI] [PMC free article] [PubMed] [Google Scholar]