Abstract
Aims
Cigarette smoking has a negative impact on the skeletal system, causes a decrease in bone mass in both young and old patients, and is considered a risk factor for the development of osteoporosis. In addition, it disturbs the bone healing process and prolongs the healing time after fractures. The mechanisms by which cigarette smoking impairs fracture healing are not fully understood. There are few studies reporting the effects of cigarette smoking on new blood vessel formation during the early stage of fracture healing. We tested the hypothesis that cigarette smoke inhalation may suppress angiogenesis and delay fracture healing.
Methods
We established a custom-made chamber with airflow for rats to inhale cigarette smoke continuously, and tested our hypothesis using a femoral osteotomy model, radiograph and microCT imaging, and various biomechanical and biological tests.
Results
In the smoking group, Western blot analysis and immunohistochemical staining revealed less expression of vascular endothelial growth factor (VEGF) and von Willebrand factor (vWF). The smoking group also had a lower microvessel density than the control group. Image and biochemical analysis also demonstrated delayed bone healing.
Conclusion
Cigarette smoke inhalation was associated with decreased expression of angiogenic markers in the early bone healing phase and with impaired bone healing.
Cite this article: Bone Joint Res. 2020;9(3):99–107.
Keywords: Cigarette, Smoking, Angiogenesis, Bone healing, Fracture union
Article focus
Cigarette smoke inhalation may suppress angiogenesis and delay fracture healing.
Key messages
Cigarette smoke inhalation results in decreased expression of angiogenicmarkers and impairs bone healing.
Strengths and limitations
This study proved that cigarette smoke inhalation could lead to delays in fracture union.
However, many substances in cigarettes have a negative effect on bone healing and it is not clear from our study that a single substance may be responsible.
Smoke inhalation may cause worse results during fracture healing period in aspects of image, biochemical, and immunohistochemistry analysis.
Introduction
Cigarette smoking has a negative impact on the skeletal system, causes a decrease in bone mass in both young and old patients, and is considered a risk factor for the development of osteoporosis.1–3 Even exposure to secondhand smoke is positively correlated with postmenopausal osteoporosis.4 Cigarette smoking also increases fracture risk and increases the burden on the healthcare system.5–7 In addition, it disturbs the bone healing process and prolongs the healing time after fractures.8
The effects of cigarette smoke inhalation on fracture healing have been investigated in both in vitro and in vivo studies. Cigarette smoke alters fibroblast migration and survival, which is essential for callus formation.9 Certain compounds contained in cigarettes are also potent inhibitors of chondrogenesis.10 Cigarette smoke also inhibits osteogenic differentiation and proliferation of human osteoprogenitor cells.11 Administration of nicotine and other compounds in cigarettes has been shown to impair the mechanical properties of healing bone following closed fractures in rats.12 Another animal study showed that the chondrogenic phase of murine tibial fracture healing was delayed by smoking.13 In yet another study, in which the authors used a distraction osteogenesis model, cigarette smoking delayed mineralization during the bone healing process and further decreased the mechanical strength of the regenerating bone.14 A previous study indicated that long-term cigarette smoking exposure impaired bone growth and increased osteoclast numbers while increasing bone volume.15
In smokers, bone morphogenetic protein (BMP) gene expression of human periosteum is reduced.16 Smoking is also a predictor of worse trabecular mechanical performance in hip fracture patients.17 A retrospective case-controlled study confirmed that cigarette smoking is deleterious to diaphyseal bone healing.18 Smoking places patients with limb-threatening open tibial fractures at risk of increased time to union and a number of other complications. A previous smoking history also increases the risk of osteomyelitis and delays fracture union.19 Finally, a smoking cessation intervention programme during the first six weeks after acute fracture surgery was found to partially reverse the negative impacts of cigarette smoking and decrease the risk of postoperative complications.20,21
The mechanisms by which cigarette smoking impairs fracture healing are not fully understood. There is some evidence that smoking may alter the initial inflammatory response and interfere with chondrogenesis,10,13 as well as osteoblast differentiation and osteogenesis.11 In sites of bone healing, cigarette smoke inhalation modulates gene expression of alkaline phosphatase, BMP-2, receptor activator of nuclear factor kappa B ligand (RANKL), and osteoprotegerin,22 signalling factors that are essential for new bone formation. Cigarette smoke also inhibits fibroblast migration, which is vital for an efficient healing process.9 A main function of fibroblasts in the fracture healing process is migration into the fracture site where growth factors and cytokines are secreted. Fibroblasts are also important for the deposition and remodelling of extracellular matrix. Most importantly, growth factors and cytokines trigger healing processes such as new vessel formation. Disruption of this process leads to poor healing.23 von Willebrand factor (vWF) is believed to be related to several vascular functions at vascular injury sites by influencing the formation of Weibel-Palade bodies (WPB), endothelial storage organelles which contain many vascular regulators.24
Angiogenesis, defined as the process of new blood vessel formation, is essential for fracture healing and, after a fracture, is triggered to supply oxygen, deliver nutrients, eliminate waste, and transport cells and mediators. Angiogenesis also promotes further intramembranous bone formation and endochondral ossification.25 In a sheep osteotomy model, the regulation of blood vessel formation was shown to differ between a standard and delayed bone healing process.26 This result suggests that various angiogenic factors may be deficient in conditions of impaired fracture healing. In another mouse tibial implant model angiogenesis and osteogenesis, resulting from orthopaedic implants, were shown to be related to the vascular endothelial growth factor pathway.27
There are few studies reporting the effects of cigarette smoking on new blood vessel formation during the early stage of fracture healing. We tested the hypothesis that cigarette smoke inhalation may suppress angiogenesis and delay fracture healing. In this study, we established a custom-made chamber with airflow for rats to inhale cigarette smoke continuously and tested our hypothesis using a femoral osteotomy model, radiograph and microCT imaging, as well as various biomechanical and biological tests.
Methods
Animals and study design
A total of 48 Sprague-Dawley (SD) adult rats weighing between 300 g to 350 g, with age of ten weeks, were divided into two groups – the smoking group and the control group – for comparison of angiogenesis and bone healing. Each rat was housed individually in our animal care centre with a 12-hour light/dark cycle, and with free access to food and water. The experimental protocol was reviewed and approved by the Institutional Animal Care and Use Committee of our institution.
All rats underwent surgical osteotomy to create a transverse fracture in the middle femoral shaft. The fracture was fixed with an intramedullary nail. The rats in the smoking group were placed in the smoking chamber and subjected to cigarette smoke inhalation for two hours each day from one week before the osteotomy surgery and continuing until sacrifice. The rats in the control group were placed in the smoking chamber with the same regularity and for the same duration, but the cigarette was not lit. The rats were sacrificed one, two, four, and eight weeks after surgery in order to evaluate fracture healing. In all, four rats in each group were sacrificed for Western blot analysis28 and histology29 in weeks one and two. Another four in each group were sacrificed for radiographs, Western blot analysis, and histology in week four. A total of twelve rats in each group were sacrificed for radiograph images, microCT (n = 12), biomechanical study (n = 6), and histology (n = 4).
Smoking chamber
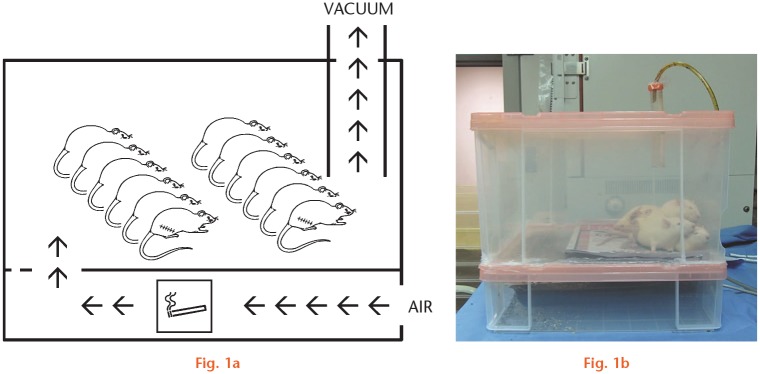
The sidestream smoke was generated in a custom-made smoking chamber (Figure 1). The cigarettes were lit in the lower level and left to glow to produce smoke. The animals were placed in the upper level for exposure. The outflow airway was connected to a vacuum suction system to maintain airflow.
Fig. 1.
Smoking chamber used to expose animals to cigarette smoke. Animals were housed on the upper level. Cigarettes were lit on the lower level. The outflow airway was connected to a vacuum suction system to maintain airflow.
Surgical procedures
Femoral shaft fractures were created by open osteotomies and were fixed with retrograde intramedullary nailing. The rats were anaesthetized intraperitoneally with sodium thiopental (50 mg/kg Sodium Pentothal; Abbott Laboratories, Lake Bluff, Illinois, USA). The depth of anaesthesia was determined by noting the withdrawal reflex on tail pinch. All of the surgical procedures were carried out in an aseptic manner. Core temperature was monitored with a probe in the rectum and connected to a multichannel thermometer (model 3087, Portable Hybrid Recorder; Yokogawa Hokushin Electric, Tokyo, Japan). The rat was then placed in a lateral position with its head fixed firmly in a stereotactic frame for further management.
The thigh was cleaned and shaved for surgery. We made a longitudinal incision in the lateral aspect of the thigh. The incision was extended to the knee area. The muscles were retracted to expose the femur. The knee capsule was opened to expose the femoral intercondylar area. A tunnel connecting to the femoral canal was created by using a 1.2 mm drill bit and power drill system. We then performed an osteotomy of the mid-femoral shaft with a power microsaw system (Stryker F1, Stryker Corporation, Kalamazoo, Michigan, USA). The soft tissue was carefully protected to avoid injury by the saw blade. A 1.4 mm Kirschner wire was inserted in a retrograde manner from the intercondylar hole to the metaphysis of the proximal femur. The wound was then closed. After surgery, there was no restriction of activity. The animals could freely access food and water. Each rat was housed in its own cage and was monitored for infection and other complications.
Radiograph and 3D microCT imaging
We performed radiograph and microCT imaging studies with a SkyScan 1076 in vivo MicroCT scanner (SkyScan, Kontich, Belgium). A cylindrical volume of interest (VOI) was created, which encompassed the callus around the fracture site. The diameter of the VOI cylinder was 1,000 pixels and the height was 5 mm proximal and distal to the fracture site. The bone volume and total volume of the whole callus was measured using CT analyzer software (SkyScan). The ratio of bone and total tissue volume was presented by percentage. Both extreme outliers in each tail were excluded in the final statistical analysis.
The fracture union was evaluated with radiographs, confirmed with microCT images, and judged by two individual experienced orthopaedic surgeons (TTW, TWT). They judged fracture union by bridging callus according to the radiographic union score for tibial (RUST) fractures scoring system.30 In the event of any disagreement, the surgeons reached consensus by discussion.
Biomechanical test
After the rats were euthanized, we dissected their femora for a three-point bending test. All of the soft tissue was removed. The contralateral femora served as internal controls. The proximal and distal sides of the femora were well fixed in the platform in the materials test machine (AG-X; Shimadzu, Tokyo, Japan). A 20 mm free length was allowed between two sides. The osteotomy site was placed at the centre. The bending force was applied directly at the level of osteotomy from anterior to posterior. A quasistatic load was applied in a three-point bending mode at a deflection rate of 1 mm per minute and a maximum force of 10 N. During the tests, we used a 0.5% sodium chloride (NaCl) solution to moisten the bone.
The bending force of the yield point was recorded. The data were presented as percentages. The bending force of the contralateral femur (internal control) in each animal was set at 100%.
Western blotting
The animals were deeply anaesthetized intraperitoneally with a sodium pentobarbital overdose (80 mg/kg) one, two, and four weeks after fracture, and perfused transcardially with phosphate-buffered saline (PBS) (pH 7.3) for six minutes. The calluses were collected, frozen in liquid nitrogen, and then stored at -80°C until further processing. The tissue was homogenized in tissue extraction reagent I (FNN0071; Thermo Fisher, Carlsbad, California, USA) with protease inhibitor cocktail (Roche, Basel, Switzerland) and 1 mM phenylmethylsulfonyl fluoride (PMSF). Total protein concentration was determined using a Bradford protein assay (Bio-Rad, Hercules, California, USA). A total of 30 µm of total protein was loaded, separated on a 10% polyacrylamide gel, and then transferred to the polyvinylidene fluoride (PVDF) membrane. The membrane was blocked with 5% non-fat milk for one hour at room temperature (RT) followed by incubation with 1:1,000 diluted primary antibody, including vWF (Abcam, Cambridge, UK), vascular endothelial growth factor (VEGF) (Abcam), and actin (Millipore, Burlington, Massachusetts, USA) at 4°C overnight. Subsequently, the membrane was washed three times in PBS and incubated with horseradish-peroxidase (HRP)-conjugated goat anti-rabbit IgG (immunogloblin G) for one hour at RT. After washing with PBS, the membrane was developed by an enhanced chemiluminescent substrate (ECL) and visualized on film (Fuji Medical X-Ray Film; Fujifilm, Tokyo, Japan), after which it was analyzed via Image-Pro Plus 4.5.1 software (Media Cybernetics, Rockville, Maryland, USA).
Histology and immunohistochemistry
After deparaffinizing and rehydrating the sections, antigen retrieval was performed with a citrate buffer (Bio SB, Santa Barbara, California, USA) at 90°C for 30 minutes. Endogenous peroxidase activity and blocking were quenched with an Expose Mouse and Rabbit Specific HRP/DAB Detection IHC kit (ab94710; Abcam). Sections were stained overnight in a humid chamber at 4°C with specific antibodies against vWF antibody (ab6994, dilution 1:1,000; Abcam). After being washed three times, goat anti-rabbit HRP-conjugate secondary antibody (ab94710; Abcam) was performed. Localization of these proteins was visualized by adding 3, 3’-diaminobenzidine (DAB) substrate solution and incubating for three minutes. Haematoxylin and eosin (H&E) was used for counterstaining. Microvessel density was counted microscopically by two independent observers (TTW, TWT). A total of three random high-power fields were counted in each specimen. The data were presented as number of vessels per mm2.
Statistical analysis
The Mann-Whitney U test was used to compare the data between the smoking and nonsmoking (control) groups. The significance was set at p < 0.05. Data are shown as means (SD). We processed the statistics with the statistical software SPSS v. 16.0 (SPSS Inc., Chicago, Illinois, USA).
Results
Analysis of fracture union and biomechanical strength
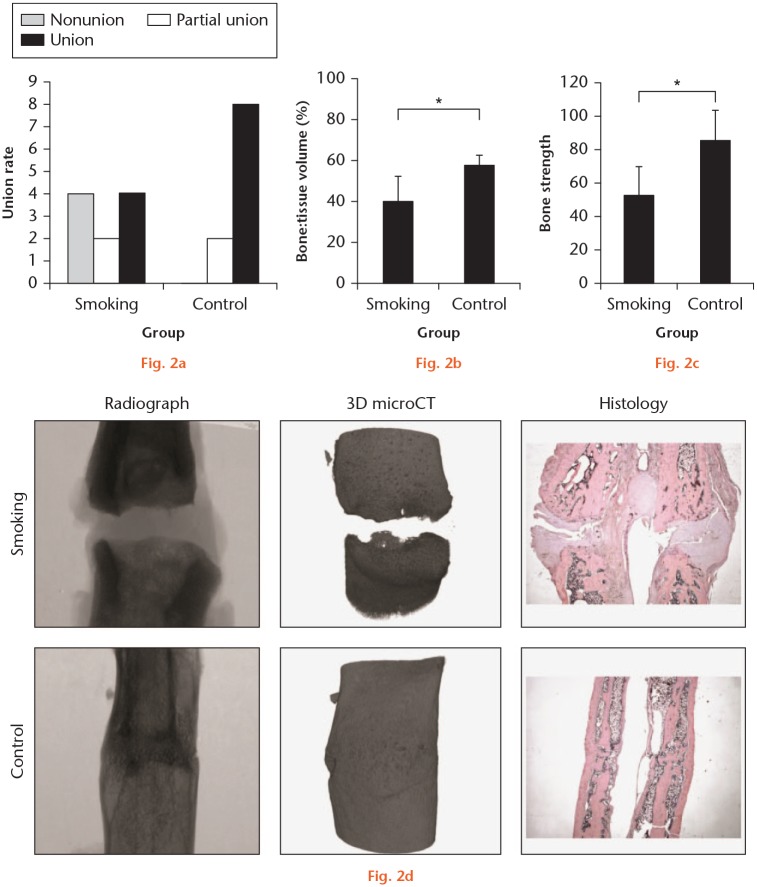
The healing of the fractures was evaluated using microCT and histological examination. It revealed only four out of ten united femora in the smoking group and eight out of ten unions in the control group (Figure 2a). In addition, the smoking group had a lower ratio of bone:tissue volume compared with the control group in microCT imaging analysis (40% (SD 14.6%) vs 57.5% (SD 5.3%); p = 0.006, Mann-Whitney U test) (Figure 2b). The biomechanical three-point bending test demonstrated that bones in the smoking group were weaker than those in the control group. (52.7% (SD 18.3%) vs 85.6% (17.3%); p = 0.01, Mann-Whitney U test) (Figure 2c). The representative samples of radiograph and microCT images and histological sections with H&E staining are shown in Figure 2d. These results confirmed that cigarette smoke inhalation compromised fracture healing.
Fig. 2.
Cigarette smoke inhalation compromised fracture healing. a) Bone healing analysis with microCT and histological examination eight weeks after fracture revealed the union rate (n = 10). b) MicroCT imaging demonstrated the ratio of bone:tissue volume.( p = 0.006, Mann-Whitney U test) c) The ultimate load of biomechanical three-point bending test showed strength of healing bone. The contralateral femur served as an internal control (100%) (n = 6). (p = 0.013, Mann-Whitney U test) d) One representative sample is shown in each group with radiograph, microCT images, and histological sections with haematoxylin and eosin (H&E) staining. *Statistically significant.
Angiogenic protein expression
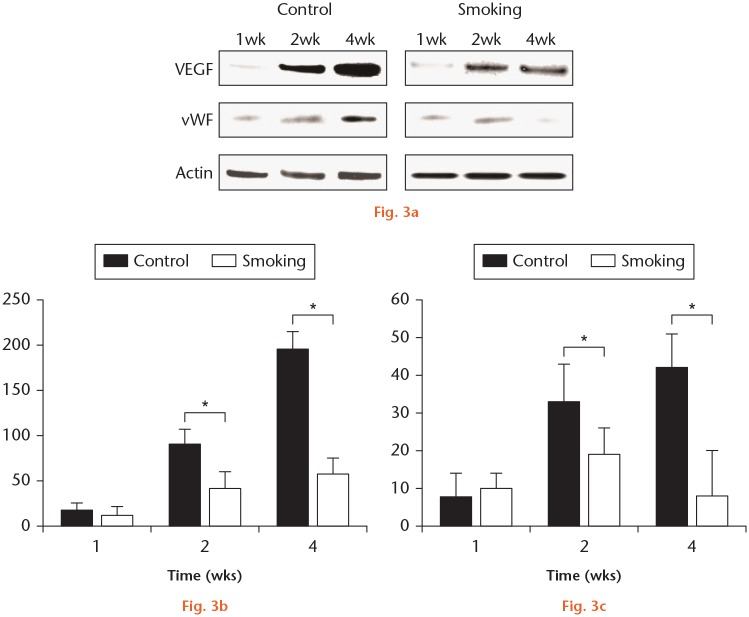
Western blot analysis was used to detect the expression of VEGF and vWF protein in the fracture calluses at weeks one, two, and four postoperatively (Figure 3a). Compared with the results in the control group, the quantified data of Western blot analyses showed a lower expression of VEGF in the smoking group in weeks two and four after the fracture. The results also showed lower vWF expression in the smoking group than in the control group in weeks two and four after the fracture. These data clearly demonstrate that cigarette smoke inhalation reduced the expression of angiogenic factors VEGF and vWF protein in the fracture callus.
Fig. 3.
Cigarette smoke inhalation reduced the expression of vascular endothelial growth factor (VEGF) and von Willebrand factor (vWF) protein in the fracture callus. a) Western blot analysis was used to detect the expression of VEGF and vWF protein in the fracture callus. β-actin was used as an internal control (n = 4). One representative data set obtained from repeated experiments is shown. b) Quantified data of Western blot analysis for the expression of VEGF in the smoking group, two and four weeks after the fracture (n = 4). c) Quantified data of Western blot analysis for expression of vWF in the smoking group, two and four weeks after the fracture (n = 4). Data are shown as the mean (SD) of six experiments. *p < 0.001 (Mann-Whitney U test).
The smoking group showed significantly less microvessel density than the control group after one week (median 6 vessels per mm3 (2.5 to 9.0) vs median 27.5 vessels per mm3 (24.0 to 34.5); p < 0.001, Mann-Whitney U test). The smoking group also showed fewer microvessels than the control group after two weeks, although the results did not reach statistical significance (median 25.5 vessels per mm3 (20.5 to 28.0) versus median 31 vessels per mm3 (25.0 to 34.0); p = 0.118, Mann-Whitney U test).
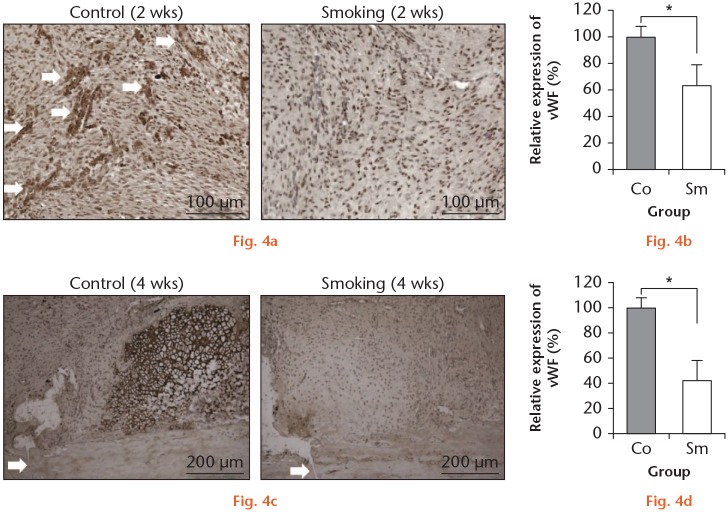
We used immunohistochemical staining to observe vWF expression and capillary formation. In week two after the fracture, a substantial amount of fibrous tissue was observed around the fracture site. In the control group, histological sections showed abundant vWF expression. The structure of capillaries could also be observed (Figure 4a). There was little vWF expression in the smoking group. Quantified image analysis also confirmed less vWF expression in the smoking group (Figure 4b). After week four of healing, vWF expression was mainly observed around the cartilage area of the soft calluses in the control group. However, the smoking group showed little vWF expression or cartilage formation (Figure 4c). The quantified results also confirmed this finding (Figure 4d).
Fig. 4.
Immunohistochemical staining of von Willebrand factor (vWF) showed lower expression in the fracture callus both at two and four weeks after the fracture. a) After two weeks of healing, the callus of the control group showed abundant vWF expression around the vessel-like structures, indicated by the white arrows. In the smoking group, there was little expression of vWF protein or new vessel formation. b) The vWF immunohistochemical staining was quantified with image analysis software (Image-Pro Plus 4.5.1 software; Media Cybernetics, Rockville, Maryland, USA ) (n = 4). Data are shown as mean (SD). c) After four weeks of healing, vWF expression was mainly observed around the cartilage area of the soft callus in the control group. However, the smoking group showed little vWF expression or cartilage formation. d) Quantified results of vWF in the smoking group four weeks after fracture (n = 4). Data are shown as the mean (SD). *p < 0.001 (Mann-Whitney U test). Co, control; Sm, smoking.
Discussion
The most important finding of this study was that cigarette smoke inhalation was associated with impaired bone healing and decreased expression of angiogenic markers in the early bone healing phase. In the smoking group, Western blot analysis and immunohistochemical staining revealed less expression of VEGF and vWF. Image and biochemical analysis also demonstrated delayed bone healing.
The bone healing process can be divided into the following three phases: inflammatory, reparative, and remodelling.31 After a fracture, haematomas form as a result of bleeding from bone and periosteal vessels. The injured tissue releases prostaglandins, which lead to local vasodilatation and attract inflammatory cytokines to the injured site.32 New blood vessels then develop from outside the bone during the reparative phase, supplying nutrients to the fracture site. The soft callus begins to form across the fracture site. Cartilage is eventually replaced by a hard callus through endochondral ossification, which increases the stability of the fracture site.33 In the subsequent remodelling phase, highly organized and mechanically strong cortical bone replaces the weaker woven bone, allowing favourable alignment of bone along the line of stress.
Smoking has been reported to have a negative effect on the musculoskeletal system. Cigarette smoking causes osteoporosis, increases the risk of injury and perioperative complications, and impairs the fracture healing process.34 A retrospective study of open tibial fractures showed that smokers had a longer time to union (32 weeks compared with 28 for nonsmokers).35 Smokers also required more bone grafting to stimulate bone healing. Another study showed that smokers had a high risk of nonunion of long bone fractures compared with non-smokers (odds ratio: 2.16).7 Similar results were found in a series of two-level spinal fusions.36 The nonunion rate in the smoking group was 40%, compared with 4% in the non-smoking group. In one rabbit model study, increased spinal fusion nonunions were noted in the systemic nicotine administration group, while an improvement in fusion rates was observed when nicotine was discontinued for the week before surgery.37
Several hypotheses have been proposed to explain how smoking impacts the fracture healing process, including reduced blood supply to the injured site, low levels of antioxidants and vitamins, high levels of reactive oxygen intermediates in the circulation, and the attenuating effect of nicotine on endothelial nitric oxide synthase.38 A series of studies demonstrated that carbon monoxide and nicotine decrease tissue oxygenation and microperfusion, and increase platelet aggregation and cause endothelial damage, producing a state of hypercoagulation and increasing blood viscosity which can lead to microclotting.39,40
Ten minutes of smoking has been shown to reduce O2 tension in tissues for one hour.41 One study observed that smoking had significant deleterious effects on bone mineral density (BMD) and cortical thickness in young adults. Moreover, the mean duration of smoking in this study was only 4.1 years, indicating that the side effects of smoking occur rapidly.42
Cigarette smoking decreases serum concentrations of transforming growth factor-beta (TGF-β), a marker of bone formation, for as long as four weeks after long bone fracture surgery.43 Another animal study also showed that nicotine inhibits the expression of genes related to osteogenic activity such as alkaline phosphatase, BMP, VEGF, TGF-β, and platelet-derived growth factor (PDGF).44
Nicotine has also been found to decrease prostacyclin production, a known vasodilator that is important in the fracture healing process.45,46 An observational study using laser Doppler flowmetry further demonstrated that one cigarette induced vasoconstriction for 90 minutes and decreased blood flow to the extremities by 24%.47 However, some studies have reported that the impact of nicotine on fracture healing is dose-dependent.38,48,49 High doses of nicotine were reported to have a toxic effect on proliferating osteoblasts, while low doses of nicotine stimulated the growth of these cells.
Recent studies have shown promising results in bone healing. A study conducted by Yoshikawa et al50 found that skeletal muscle supernatant, which contained several cytokines and growth factors, enhanced the capability of cell proliferation, osteoinduction, and angiogenesis in human mesenchymal stem cells and human umbilical cord vein endothelial cells. In another study of a rat femur nonunion model, quality and quantity control-cultured peripheral blood mononuclear cells had been demonstrated to promote angiogenesis and bone union.51
It is worth mentioning that one systemic review study in foot and ankle surgery demonstrated that smoking had a negative impact on plastic surgery, fracture fixation, and operations involving arthrodesis. However, surgeries such as amputation or total ankle arthroplasty, which did not involve osseous unions, did not have a worse outcome associated with smoking.52
There are some limitations in this study. First, because many substances in cigarettes have a negative effect on bone healing, it is not clear from our study that a single substance may be responsible. Two phases were included in cigarette smoking: a particulate phase of nearly 3,500 chemicals (e.g. nicotine, nornicotine, anabasine, anatabine); and a volatile phase of approximately 500 different gases (e.g. nitrogen, ammonia, carbon monoxide, carbon dioxide, and hydrogen cyanide).53
Approximately 2 mg to 3 mg of nicotine and 20 ml to 30 ml of carbon monoxide are inhaled from each cigarette.54 Although many studies have indicated that nicotine is the major cause of bony nonunion, one animal study found that the mechanical strength of the healing fractures was influenced by tobacco extract plus nicotine rather than nicotine alone.48 This article suggested that tobacco extract, rather than nicotine, impaired the mechanical strength of fracture healing.
Second, we simulated cigarette smoking by smoke inhalation in this study, which is the same as secondhand smoking. It is difficult to simulate active smoking in an animal model. Therefore, our results may not apply directly to smokers. Nevertheless, we believe that the population of secondhand smokers is larger than active smokers. The differences between active smoking and secondhand smoking require further study.
Third, although we demonstrated a negative effect of smoke inhalation on the expression of angiogenic markers, whether or not rescuing angiogenesis at the fracture sites would improve bone healing is controversial. A recent study revealed that the local application of simvastatin, an agent known to stimulate both angiogenesis and osteogenesis, might help fracture healing in rats.55 However, another study suggested that BMPs were more important than VEGF.56
In summary, this animal study showed that cigarette smoke inhalation can lead to the decreased expression of angiogenic markers, such as VEGF and vWF, in the early bone healing phase and can impair bone healing. Further studies are required to determine whether rescuing angiogenesis might be a potential therapeutic target for delayed union or nonunion of fractures.
Acknowledgments
The study is funded by a grant from the Ministry of Science and Technology (MOST) of Taiwan (Grant No.: MOST 104-2314-B-006-005-MY2). We thank Dr Chia-Jung Ho for the technical support with the building and design of the smoking chamber.
Footnotes
Author contributions: C-J. Chang: Drafted the manuscript.
I-M. Jou: Designed the study, Approved the manuscript.
T-T. Wu: Analyzed and interpreted the data, Drafted the manuscript.
F-C. Su: Designed the study.
T-W. Tai: Research design, Analysis or interpretation of data, Drafting the paper, Approval of the submitted versions
Ethical review statement: The experimental protocol was reviewed and approved by the Institutional Animal Care and Use Committee of our institution (approval no: 101046).
ICMJE COI statement: None declared
Follow us @BoneJointRes
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Tamaki J, Iki M, Fujita Y, et al. Impact of smoking on bone mineral density and bone metabolism in elderly men: the Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) study. Osteoporos Int. 2011;22(1):133-141. [DOI] [PubMed] [Google Scholar]
- 2. Ortego-Centeno N, Muñoz-Torres M, Jódar E, Hernández-Quero J, Jurado-Duce A, de la Higuera Torres-Puchol J. Effect of tobacco consumption on bone mineral density in healthy young males. Calcif Tissue Int. 1997;60(6):496-500. [DOI] [PubMed] [Google Scholar]
- 3. Pompe E, de Jong PA, van Rikxoort EM, et al. Smokers with emphysema and small airway disease on computed tomography have lower bone density. Int J Chron Obstruct Pulmon Dis. 2016;11:1207-1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim KH, Lee CM, Park SM, et al. Secondhand smoke exposure and osteoporosis in never-smoking postmenopausal women: the Fourth Korea National Health and Nutrition Examination Survey. Osteoporos Int. 2013;24(2):523-532. [DOI] [PubMed] [Google Scholar]
- 5. Baron JA, Farahmand BY, Weiderpass E, et al. Cigarette smoking, alcohol consumption, and risk of hip fracture in women. Arch Intern Med. 2001;161(7):983-988. [DOI] [PubMed] [Google Scholar]
- 6. Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ. 1997;315(7112):841-846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Scolaro JA, Schenker ML, Yannascoli S, Baldwin K, Mehta S, Ahn J. Cigarette smoking increases complications following fracture: a systematic review. J Bone Joint Surg Am. 2014;96(8):674-681. [DOI] [PubMed] [Google Scholar]
- 8. Pearson RG, Clement RG, Edwards KL, Scammell BE. Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open. 2016;6(11):e010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wong LS, Martins-Green M. Firsthand cigarette smoke alters fibroblast migration and survival: implications for impaired healing. Wound Repair Regen. 2004;12(4):471-484. [DOI] [PubMed] [Google Scholar]
- 10. Kung MH, Yukata K, O’Keefe RJ, Zuscik MJ. Aryl hydrocarbon receptor-mediated impairment of chondrogenesis and fracture healing by cigarette smoke and benzo(a)pyrene. J Cell Physiol. 2012;227(3):1062-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu XD, Zhu YK, Umino T, et al. Cigarette smoke inhibits osteogenic differentiation and proliferation of human osteoprogenitor cells in monolayer and three-dimensional collagen gel culture. J Lab Clin Med. 2001;137(3):208-219. [DOI] [PubMed] [Google Scholar]
- 12. Hastrup SG, Chen X, Bechtold JE, et al. Effect of nicotine and tobacco administration method on the mechanical properties of healing bone following closed fracture. J Orthop Res. 2010;28(9):1235-1239. [DOI] [PubMed] [Google Scholar]
- 13. El-Zawawy HB, Gill CS, Wright RW, Sandell LJ. Smoking delays chondrogenesis in a mouse model of closed tibial fracture healing. J Orthop Res. 2006;24(12):2150-2158. [DOI] [PubMed] [Google Scholar]
- 14. Ueng SW, Lin SS, Wang CR, Liu SJ, Tai CL, Shih CH. Bone healing of tibial lengthening is delayed by cigarette smoking: study of bone mineral density and torsional strength on rabbits. J Trauma. 1999;46(1):110-115. [DOI] [PubMed] [Google Scholar]
- 15. Sasaki M, Chubachi S, Kameyama N, et al. Effects of long-term cigarette smoke exposure on bone metabolism, structure, and quality in a mouse model of emphysema. PLoS One. 2018;13(1):e0191611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chassanidis CG, Malizos KN, Varitimidis S, et al. Smoking affects mRNA expression of bone morphogenetic proteins in human periosteum. J Bone Joint Surg Br. 2012;94-B(10):1427-1432. [DOI] [PubMed] [Google Scholar]
- 17. Rodrigues AM, Caetano-Lopes J, Vale AC, et al. Smoking is a predictor of worse trabecular mechanical performance in hip fragility fracture patients. J Bone Miner Metab. 2012;30(6):692-699. [DOI] [PubMed] [Google Scholar]
- 18. Hernigou J, Schuind F. Smoking as a predictor of negative outcome in diaphyseal fracture healing. Int Orthop. 2013;37(5):883-887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM; LEAP Study Group. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005;19(3):151-157. [DOI] [PubMed] [Google Scholar]
- 20. Nåsell H, Adami J, Samnegård E, Tønnesen H, Ponzer S. Effect of smoking cessation intervention on results of acute fracture surgery: a randomized controlled trial. J Bone Joint Surg Am. 2010;92(6):1335-1342. [DOI] [PubMed] [Google Scholar]
- 21. Nieboer MF, Gosens T. Effect of smoking on orthopaedic conditions: an overview for everyday practice. Ned Tijdschr Geneeskd. 2017;161(161):D925-D925. (Article in Dutch) [PubMed] [Google Scholar]
- 22. Giorgetti AP, César Neto JB, Ruiz KG, Casati MZ, Sallum EA, Nociti FH., Jr Cigarette smoke inhalation modulates gene expression in sites of bone healing: a study in rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(4):447-452. [DOI] [PubMed] [Google Scholar]
- 23. Shabestari M, Kise NJ, Landin MA, et al. Enhanced angiogenesis and increased bone turnover characterize bone marrow lesions in osteoarthritis at the base of the thumb. Bone Joint Res. 2018;7(6):406-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Randi AMSK, Smith KE, Castaman G. von Willebrand factor regulation of blood vessel formation. Blood. 2018;132(2):132-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harper J, Klagsbrun M. Cartilage to bone—angiogenesis leads the way. Nat Med. 1999;5(6):617-618. [DOI] [PubMed] [Google Scholar]
- 26. Lienau J, Schmidt-Bleek K, Peters A, et al. Differential regulation of blood vessel formation between standard and delayed bone healing. J Orthop Res. 2009;27(9):1133-1140. [DOI] [PubMed] [Google Scholar]
- 27. Ji G, Xu R, Niu Y, et al. Vascular endothelial growth factor pathway promotes osseointegration and CD31hiEMCNhi endothelium expansion in a mouse tibial implant model: an animal study. Bone Joint J. 2019;101-B(7_Supple_C):108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kurien BT, Scofield RH. Western blotting. Methods. 2006;38(4):283-293. [DOI] [PubMed] [Google Scholar]
- 29. Ward JM, Rehg JE. Rodent immunohistochemistry: pitfalls and troubleshooting. Vet Pathol. 2014;51(1):88-101. [DOI] [PubMed] [Google Scholar]
- 30. Azevedo Filho FA, Cotias RB, Azi ML, Teixeira AA. Reliability of the radiographic union scale in tibial fractures (RUST). Rev Bras Ortop. 2016;52(1):35-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Einhorn TA. The cell and molecular biology of fracture healing. Clin Orthop Relat Res. 1998;(355 Suppl):S7-S21. [DOI] [PubMed] [Google Scholar]
- 32. Miller SC, Marks SC., Jr Effects of prostaglandins on the skeleton. Clin Plast Surg. 1994;21(3):393-400. [PubMed] [Google Scholar]
- 33. Haverstock BD, Mandracchia VJ. Cigarette smoking and bone healing: implications in foot and ankle surgery. J Foot Ankle Surg. 1998;37(1):69–78. [DOI] [PubMed] [Google Scholar]
- 34. Duthon VB, Ozturk M, El-Achachi S, Menetrey J. Deleterious effects of smoking on the musculoskeletal system. Rev Med Suisse. 2014;10(437):1466-1471. (Article in French) [PubMed] [Google Scholar]
- 35. Adams CI, Keating JF, Court-Brown CM. Cigarette smoking and open tibial fractures. Injury. 2001;32(1):61-65. [DOI] [PubMed] [Google Scholar]
- 36. Brown CW, Orme TJ, Richardson HD. The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine (Phila Pa 1976). 1986;11(9):942-943. [DOI] [PubMed] [Google Scholar]
- 37. Wing KJ, Fisher CG, O’Connell JX, Wing PC. Stopping nicotine exposure before surgery. The effect on spinal fusion in a rabbit model. Spine (Phila Pa 1976). 2000;25(1):30–34. [DOI] [PubMed] [Google Scholar]
- 38. Gaston MS, Simpson AH. Inhibition of fracture healing. J Bone Joint Surg Br. 2007;89-B(12):1553-1560. [DOI] [PubMed] [Google Scholar]
- 39. Grines CL, Topol EJ, O’Neill WW, et al. Effect of cigarette smoking on outcome after thrombolytic therapy for myocardial infarction. Circulation. 1995;91(2):298-303. [DOI] [PubMed] [Google Scholar]
- 40. El-Zayadi ARSO, Selim O, Hamdy H, El-Tawil A, Moustafa H. Heavy cigarette smoking induces hypoxic polycythemia (erythrocytosis) and hyperuricemia in chronic hepatitis C patients with reversal of clinical symptoms and laboratory parameters with therapeutic phlebotomy. Am J Gastroenterol. 2002;97(5):1264-1265. [DOI] [PubMed] [Google Scholar]
- 41. Sørensen LT, Jørgensen S, Petersen LJ, et al. Acute effects of nicotine and smoking on blood flow, tissue oxygen, and aerobe metabolism of the skin and subcutis. J Surg Res. 2009;152(2):224-230. [DOI] [PubMed] [Google Scholar]
- 42. Lorentzon M, Mellström D, Haug E, Ohlsson C. Smoking is associated with lower bone mineral density and reduced cortical thickness in young men. J Clin Endocrinol Metab. 2007;92(2):497-503. [DOI] [PubMed] [Google Scholar]
- 43. Moghaddam A, Weiss S, Wölfl CG, et al. Cigarette smoking decreases TGF-b1 serum concentrations after long bone fracture. Injury. 2010;41(10):1020-1025. [DOI] [PubMed] [Google Scholar]
- 44. Truntzer J, Vopat B, Feldstein M, Matityahu A. Smoking cessation and bone healing: optimal cessation timing. Eur J Orthop Surg Traumatol. 2015;25(2):211–215. [DOI] [PubMed] [Google Scholar]
- 45. Effeney DJ. Prostacyclin production by the heart: effect of nicotine and carbon monoxide. J Vasc Surg. 1987;5(2):237-247. [PubMed] [Google Scholar]
- 46. Nadler JL, Velasco JS, Horton R. Cigarette smoking inhibits prostacyclin formation. Lancet. 1983;1(8336):1248-1250. [DOI] [PubMed] [Google Scholar]
- 47. van Adrichem LN, Hovius SE, van Strik R, van der Meulen JC. Acute effects of cigarette smoking on microcirculation of the thumb. Br J Plast Surg. 1992;45(1):9-11. [DOI] [PubMed] [Google Scholar]
- 48. Skott M, Andreassen TT, Ulrich-Vinther M, et al. Tobacco extract but not nicotine impairs the mechanical strength of fracture healing in rats. J Orthop Res. 2006;24(7):1472–1479. [DOI] [PubMed] [Google Scholar]
- 49. Rothem DE, Rothem L, Soudry M, Dahan A, Eliakim R. Nicotine modulates bone metabolism-associated gene expression in osteoblast cells. J Bone Miner Metab. 2009;27(5):555-561. [DOI] [PubMed] [Google Scholar]
- 50. Yoshikawa M, Nakasa T, Ishikawa M, Adachi N, Ochi M. Evaluation of autologous skeletal muscle-derived factors for regenerative medicine applications. Bone Joint Res. 2017;6(5):277-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mifuji K, Ishikawa M, Kamei N, et al. Angiogenic conditioning of peripheral blood mononuclear cells promotes fracture healing. Bone Joint Res. 2017;6(8):489-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kim JH, Patel S. Is It Worth Discriminating Against Patients Who Smoke? A Systematic Literature Review on the Effects of Tobacco Use in Foot and Ankle Surgery. J Foot Ankle Surg. 2017;56(3):594–599. [DOI] [PubMed] [Google Scholar]
- 53. Benowitz NL. Clinical pharmacology of nicotine. Annu Rev Med. 1986;37:21–32. [DOI] [PubMed] [Google Scholar]
- 54. Sherwin MA, Gastwirth CM. Detrimental effects of cigarette smoking on lower extremity wound healing. J Foot Surg. 1990;29(1):84–87. [PubMed] [Google Scholar]
- 55. Fukui T, Ii M, Shoji T, et al. Therapeutic effect of local administration of low-dose simvastatin-conjugated gelatin hydrogel for fracture healing. J Bone Miner Res. 2012;27(5):1118–1131. [DOI] [PubMed] [Google Scholar]
- 56. Garcia P, Pieruschka A, Klein M, et al. Temporal and spatial vascularization patterns of unions and nonunions: role of vascular endothelial growth factor and bone morphogenetic proteins. J Bone Joint Surg Am. 2012;94-A(1):49–58. doi: 10.2106/JBJS.J.00795 [DOI] [PubMed] [Google Scholar]