ABSTRACT
Aim
To evaluate the antibacterial effect of herbal water, ozonated water, and chlorhexidine mouthrinses on salivary Streptococcus mutans level and to assess their effectiveness of these mouthrinses on the oral health status of children.
Materials and methods
A parallel multiarm randomized controlled trial was conducted in 100 children aged 10–12 years. Debris index-simplified (DI-S), calculus index-simplified (CI-S), oral hygiene index-simplified (OHI-S) scores, and Streptococcus mutans counts were recorded at baseline (T1). They were randomly divided into four equal groups (n = 25): HW, herbal water; OW, ozonated water; W, water; and CHX, chlorhexidine. Intervention period was 15 days and data collection was repeated after 15 days (T2) and 30 days (T3). Saliva samples were used to evaluate S. mutans count. Results were tabulated and analyzed statistically.
Results
OW had minimum DI-S score at T2 and T3 periods. HW had the minimum CI-S score at T2 and T3 periods. CHX had the minimum S. mutans count at T2 and T3 periods. OW showed maximum reduction in OHI-S score at T2 period. HW showed maximum reduction in OHI-S score at T3 period.
Conclusion
Herbal water and ozone water can be used as an alternative to chlorhexidine in maintaining the oral health status.
Clinical significance
Herbal water and ozonated water can be used in children instead of chemical mouthrinses to avoid any adverse effects.
How to cite this article
Mon J, Asokan S, Priya PRG, et al. Effect of Herbal Water, Ozonated Water, Water, and Chlorhexidine Mouthrinses on Oral Health Status of Children: A Randomized Controlled Trial. Int J Clin Pediatr Dent 2019;12(6):514–519.
Keywords: Herbal mouthrinse, Herbal water, Mouthrinses, Ozonated water, Ozone, Randomized controlled trial, Tulsi
INTRODUCTION
Dental caries is a major oral health problem in most industrialized countries, affecting 60–90% of schoolchildren and the vast majority of adults. It has shown an increasing trend in developing countries including India.1
Research in the field of caries prevention has been focusing on the ways for reducing or totally eradicating cariogenic flora from the oral cavity. Studies have shown that caries can be prevented by regular tooth brushing and flossing. However, it is difficult to eliminate Streptococcus mutans (S. mutans) from pits, fissures, and approximal surfaces by mechanical means alone. For effective caries control, it is better to combine these strategies with the chemoprophylactic agents such as mouthrinses, toothpastes, gels, and varnishes.1,2
Mouthrinses have been popularly used as a supplementary oral hygiene aid. They have the ability to deliver therapeutic ingredients and benefits to all accessible surfaces in the mouth including interproximal surfaces.3 Among them, the most commonly used is chlorhexidine (CHX) which is known to be the most potent chemotherapeutic agent against S. mutans and the most effective antiplaque agent.4,5 But the long-term use of CHX possess few adverse effects which have restricted its usage in pediatric age group and necessitated the search for alternatives.6,7
An effective and safe alternative to CHX mouthwash is herbal products which have lesser side effects, cheaper, and locally available.2,4,5 Tulsi is an aromatic shrub from the basil family Lamiaceae (Tribe ocimeae) and is one of the best examples of ayurveda's holistic lifestyle approach to health. Tulsi has long been recognized as possessing antioxidant properties, as a COX2 inhibitor and to provide protection from radiation poisoning and cataracts. Agarwal et al. reported that tulsi extract had demonstrated a significant antimicrobial potential against S. mutans.8
Ozone is a powerful nonantibiotic biocide that is effective as a gas and can be dissolved in water.9 Its antimicrobial spectrum includes a wide variety of bacteria, viruses, and fungi. Its mechanism of action is by inducing oxidation of the cell wall and cytoplasmic membranes that leads to the lysis of the microorganism. Nagayoshi et al. examined the effect of ozonated water on oral microorganisms and dental plaque in vitro and almost no microorganisms were detected after being treated with ozonated water for 10 seconds.3 The effectiveness of ozone is currently a subject of intensive research in the treatment of oral diseases.9–12 Currently, in the literature search, there are no studies conducted using ozonated water as mouthrinse in children. To consider ozone as a potential antimicrobial agent against oral pathogens, it is important to compare its effectiveness with established agents currently used in dentistry.
Hence, the aim of this study was to evaluate the antibacterial effect of herbal water, ozonated water, and chlorhexidine on salivary Streptococcus mutans level and to compare their effect on the oral health status of children.
MATERIALS AND METHODS
A parallel multiarm randomized controlled trial was conducted from the Department of Pediatric and Preventive Dentistry, KSR Institute of Dental Science and Research (KSRIDSR), Tiruchengode, Tamil Nadu. The study design and protocol was analyzed and approved by the Institutional Review Board and Institutional Ethics Committee of KSRIDSR (165/KSRIDSR/EC/2016). Permission of the Assistant Elementary Educational Officer was obtained to carry out the study. One government-aided school was randomly selected by lottery method. The purpose of the study was explained to the school authorities and their approval was obtained. A total of 206 children aged were screened, and a study population of 100 was selected based on the following inclusion and exclusion criteria.
Inclusion Criteria
Schoolchildren aged 10–12 years
DMFT/deft score ≤3
Exclusion Criteria
Children with systemic diseases
Children with history of antibiotics usage in past 1 month
Children undergoing orthodontic treatment
A written consent in native language (Tamil) was also obtained from the parents of the children who participated in the study. The study was conducted between July and August 2018.
Sample size estimation was done based on the study by Ahmed et al., with the power of test at 80% and p value <0.05 considered significant. The sample size was determined to be 20 in each group. Anticipating an attrition rate of 25%, 5 samples were added to each group.
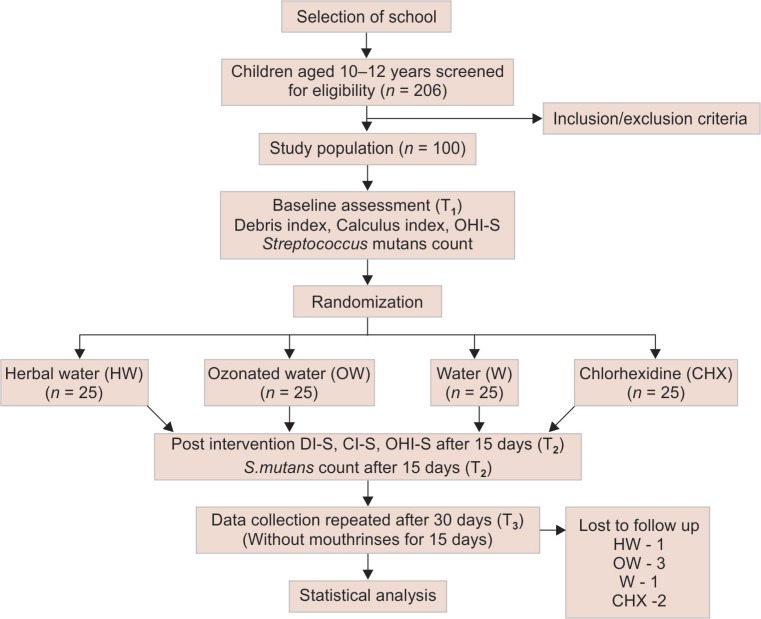
Hundred children were randomly divided into 4 groups with 25 children in each group using table of random numbers. Sequence generation and allocation was done by two dental residents who were not involved in the study (allocation ratio 1:1:1:1). The recruited children were allocated to the following groups: HW, herbal water; OW, ozonated water; W, water; CHX, chlorhexidine (Flowchart 1). Primary investigator was not blinded as the mouthrinses were prepared by him. He was aware of the odor and color of the mouthrinses prepared. The study population and the secondary investigators (lab technicians) who did the microbiological assessment and the statistician were blinded.
Flowchart 1.
Methodology
In vitro Study
Dosage optimization of herbal water against S. mutans (MTCC-890) was done using well-diffusion method in Muller Hilton agar medium for intervention purpose. Screening of antimicrobial efficacy of herbal water, ozonated water, water, and chlorhexidine was determined against S. mutans before the conduction of intervention. Triplicates were maintained for all the three samples.
In vivo Study
Measurement of Oral Health Status
Debris and calculus scores were recorded using oral hygiene index-simplified (OHI-S) as described by John C. Greene and Jack R. Vermillion (1964) by the blinded secondary investigator. Oral prophylaxis was performed for all children, 5 days prior to the intervention. Children were instructed to carry on with their routine oral hygiene practices.
Salivary Streptococcus mutans Colony Count
All children were instructed not to eat or drink 30 minutes prior to the saliva sample collection. Unstimulated salivary samples were collected at mid-morning using sterile uricups by the primary investigator. S. mutans count was evaluated using spread plate method in brain heart infusion agar (BHI). One milliliter of the diluted saliva was plated on the agar media and the plates were inverted and incubated at 37°C for 48–72 hours. The colonies were identified by colony morphological characteristics and confirmed using Gram staining (minute spherical, translucent, and pinpoint colonies that are Gram positive cocci arranged in short chains or pairs). All the counts were established for 105 dilution and were converted to CFU/mL.
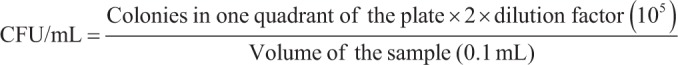 |
Preparation of Mouthrinses
Herbal water was freshly prepared everyday by adding 10 drops of Deltas Pancha tulasi drops [Delta Pharma, Mumbai, India; composition—Ocimum sanctum (60%), Ocimum gratissimum (5%), Ocimum canum (5%), Ocimum basilicum (5%), Ocimum citriodorum (5%)] mixed in 10 mL of water and were given to the children in a container.
Ozonated water was freshly prepared each day by ozonation of water for 1 minute by using ozone generator (Ozone Engineers, Coimbatore). Two hundred and five liters of normal water was placed in the system with a glass tube coupled to the ozone generator. Next, triatomic form of oxygen (O3) was bubbled through the water for 1 minute, thereby producing O3 at a concentration of 2.4 mg/L per minute (>2 ppm). From that, 10 mL were given to each child in a container immediately.
Five milliliters of 0.12% CHX mouthwash (Chlorhex ICPA health products Ltd, India) was diluted in 5 mL of water every day and was given to the children in a container.
Ten milliliters of normal water was given every day to the children in a container.
All children were asked to rinse each day with the respective mouthrinses for 1 minute continuously in the morning for 15 days during school hours under the presence of the primary investigator. They were asked to refrain from eating 2 hours prior to the start of rinsing. OHI-S was taken and salivary samples were collected at 3 time periods for the determination of S. mutans count—at baseline (T1), after 15 days (T2), and after 30 days (T3). Duration of the study was 1 month.
Statistical Analysis
The statistical analysis was done using IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. The statistical significance was set at p ≤ 0.05. Intragroup comparison was done using Friedman test followed by post hoc analysis using Wilcoxon signed rank test. Intergroup comparison was done by one-way ANOVA (Kruskall Wallis) test followed by post hoc analysis using Mann–Whitney U test.
RESULTS
Table 1 shows zone of inhibition in the four groups against S. mutans. HW, OW, and CHX groups showed zone of inhibition. HW showed the maximum zone of inhibition among the groups studied.
Table 1.
Zone of inhibition against S. mutans
| Groups | Zone of inhibition (mm) mean ± SD |
|---|---|
| HW | 30.33 ± 0.88 |
| OW | 16 ± 0.58 |
| W | No zone observed |
| CHX | 28.33 ± 0.33 |
Table 2 shows the intragroup comparison of all variables at each time intervals in all groups. There was a significant reduction in DI-S score between T1 and T2 intervals and between T1 and T3 intervals in all the four groups. Maximum reduction in DI-S scores for all groups was seen between T1 and T2 intervals. HW showed a significant reduction in CI-S score between T1 and T2 intervals. There was a significant increase in CI-S score between T1 and T3 intervals and T2 and T3 intervals in OW, CHX, and W. There was a significant reduction in OHI-S score between T1 and T2 intervals and T1 and T3 intervals in HW, OW, and CHX. There was a significant increase in OHI-S score between T2 and T3 intervals in OW and CHX. Maximum reduction in OHI-S score in HW, OW, and CHX was seen between T1 and T2 intervals. There was a significant reduction in S. mutans count in HW, OW, and CHX between T1 and T2 intervals, T1 and T3 intervals, and T2 and T3 intervals, respectively. HW, OW, and CHX showed maximum reduction in S. mutans count between T1 and T3 intervals.
Table 2.
Intragroup comparison of all variables at each time intervals in all groups
| Variables | T1 mean ± SD | T3 mean ± SD | T2 mean ± SD | p value* | T1 vs T2** | T1 vs T3** | T2 vs T3** | |
|---|---|---|---|---|---|---|---|---|
| H | DI-S | 1.73 ± 0.48 | 0.80 ± 0.37 | 0.91 ± 0.31 | <0.001 | 0.001 | 0.001 | |
| CI-S | 0.20 ± 0.31 | 0.09 ± 0.17 | 0.11 ± 0.18 | 0.04 | 0.01 | |||
| OHI-S | 1.93 ± 0.70 | 0.89 ± 0.43 | 1.02 ± 0.36 | 0.001 | 0.001 | 0.001 | ||
| S. mutans | 19.20 ± 30.5 | 4.87 ± 3.5 | 2.87 ± 1.56 | <0.001 | <0.001 | <0.001 | 0.01 | |
| OW | DI-S | 1.86 ± 0.39 | 0.73 ± 0.40 | 0.86 ± 0.28 | <0.001 | 0.001 | 0.001 | |
| CI-S | 0.11 ± 0.19 | 0.10 ± 0.17 | 0.24 ± 0.24 | 0.002 | 0.02 | 0.005 | ||
| OHI-S | 1.97 ± 0.43 | 0.83 ± 0.44 | 1.11 ± 0.43 | 0.001 | 0.001 | 0.001 | 0.031 | |
| S. mutans | 12.76 ± 9.7 | 6.14 ± 4.04 | 2.23 ± 0.76 | <0.001 | 0.003 | <0.001 | <0.001 | |
| W | DI-S | 1.74 ± 0.62 | 1.25 ± 0.39 | 1.27 ± 0.39 | <0.001 | 0.001 | 0.001 | |
| CI-S | 0.14 ± 0.21 | 0.29 ± 0.33 | 0.50 ± 0.32 | 0.005 | 0.001 | 0.001 | ||
| OHI-S | 1.87 ± 0.76 | 1.54 ± 0.61 | 1.77 ± 0.63 | 0.08 | ||||
| S. mutans | 15.41 ± 11.89 | 17.37 ± 17.25 | 15.33 ± 3.0 | 0.42 | ||||
| CHX | DI-S | 1.69 ± 0.39 | 0.76 ± 0.37 | 0.87 ± 0.23 | <0.001 | 0.001 | 0.001 | |
| CI-S | 0.095 ± 0.50 | 0.095 ± 0.49 | 0.25 ± 0.39 | <0.001 | 0.004 | 0.001 | ||
| OHI-S | 1.80 ± 0.50 | 0.83 ± 0.49 | 1.125 ± 0.39 | 0.001 | 0.001 | 0.001 | 0.003 | |
| S. mutans | 14.13 ± 12.8 | 3.043 ± 1.9 | 1.86 ± 1.74 | <0.001 | <0.001 | <0.001 | 0.01 |
*Friedman test; **post hoc Wilcoxon signed rank test
Table 3 shows intergroup comparison of all variables at different time intervals. There was no significant difference in DI-S score between the groups at T1 period. A significant difference was seen in all the groups at T2 and T3 periods. At T2 and T3 periods, there was a significant difference between HW and W, OW and W, and W and CHX. OW had minimum DI-S score at T2 and T3 periods. There was no significant difference between the groups in CI-S score at T1 period. A significant difference was seen at T2 and T3 periods. At T2 period, there was a significant difference between HW and W, OW and W, and W and CHX. At T3 period, there was a significant difference between HW and W, H and CHX, OW and W, and W and CHX. HW had the minimum CI-S score at T2 and T3 periods. There was no significant difference in OHI-S between the groups at T1 period. At T2 and T3 periods, there was a significant difference seen in OHI-S score. At T2 and T3 periods, there was a significant difference between HW and W, OW and W, and W and CHX. OW followed by CHX showed maximum reduction in OHI-S score at T2 period. HW showed maximum reduction in OHI-S score at T3 period. There was no significant difference in S. mutans count between the groups at T1 period. A significant difference was seen at T2 and T3 periods. At T2 and T3 periods, there was a significant difference in S. mutans count between HW and W, HW and CHX, OW and W, and W and CHX. CHX had the minimum S. mutans count at T2 and T3 periods.
Table 3.
Intergroup comparison of all variables at different time intervals
| Variables | Intervals | HW | OW | W | CHX | p value* | HW vs OW | HW vs W | post hoc** HW vs CHX | OW vs W | OW vs CHX | W vs CHX |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DI-S | T1 | 1.73 ± 0.48 | 1.86 ± 0.39 | 1.74 ± 0.62 | 1.69 ± 0.39 | 0.59 | ||||||
| T2 | 0.80 ± 0.37 | 0.73 ± 0.40 | 1.25 ± 0.39 | 0.76 ± 0.37 | 0.000 | 0.001 | 0.001 | 0.001 | ||||
| T3 | 0.91 ± 0.31 | 0.86 ± 0.28 | 1.27 ± 0.39 | 0.87 ± 0.23 | 0.001 | 0.005 | 0.001 | 0.001 | ||||
| CI-S | T1 | 0.20 ± 0.31 | 0.11 ± 0.11 | 0.14 ± 0.21 | 0.095 ± 0.16 | 0.65 | ||||||
| T2 | 0.09 ± 0.17 | 0.10 ± 0.14 | 0.29 ± 0.33 | 0.095 ± 0.14 | 0.009 | 0.001 | 0.001 | 0.01 | ||||
| T3 | 0.11 ± 0.18 | 0.24 ± 0.24 | 0.50 ± 0.32 | 0.25 ± 0.24 | 0.000 | 0.002 | 0.03 | 0.001 | 0.001 | |||
| OHI-S | T1 | 1.93 ± 0.7 | 1.97 ± 0.43 | 1.87 ± 0.76 | 1.80 ± 0.50 | 0.62 | ||||||
| T2 | 0.89 ± 0.43 | 0.83 ± 0.44 | 1.54 ± 0.61 | 0.83 ± 0.49 | 0.000 | 0.007 | 0.001 | 0.005 | ||||
| T3 | 1.028 ± 0.36 | 1.11 ± 0.43 | 1.77 ± 0.63 | 1.125 ± 0.39 | 0.000 | 0.001 | 0.001 | 0.001 | ||||
| S. mutans | T1 | 19.2 ± 13.75 | 12.76 ± 9.7 | 15.41 ± 11.89 | 14.13 ± 12.88 | 0.94 | ||||||
| T2 | 4.87 ± 5 | 6.14 ± 4 | 17.37 ± 17.25 | 3.043 ± 1.91 | <0.001 | <0.001 | 0.04 | <0.001 | 0.006 | <0.001 | ||
| T3 | 2.87 ± 2 | 2.23 ± 0.76 | 15.33 ± 3 | 1.86 ± 1.74 | 0.001 | <0.001 | 0.002 | <0.001 | 0.006 | <0.001 |
*One-way ANOVA (Kruskall Wallis) test; **Post hoc Mann–Whitney U test
DISCUSSION
This study was conducted to evaluate and compare the antibacterial effect of herbal water, ozonated water, and CHX on salivary S. mutans level in children. Age group of 10–12 years were selected because they belong to the concrete operational stage of Jean Piaget's cognitive theory. Hence, they accept the rules and they follow the instructions given to them.13 This age group of children can easily rinse the mouthwash without swallowing it and hence side effects of mouthrinses can be avoided.6,14 Oral prophylaxis was carried out for all the study subjects to maintain homogeneity in baseline data between the groups.5
In vitro Trials
In our study, we used Deltas Pancha tulasi drops which is in liquid form and is chemical and alcohol free. According to the manufacturer, it can be used as a natural water purifier. It has antibacterial, antimicrobial, anti-infective, immune modulator, powerful antioxidant activity, and is also used as natural adjuvant in the management of cough and cold. Its antimicrobial activity was demonstrated by Agarwal et al. who obtained a zone of inhibition of 22 mm with 4% tulsi extract.15 In our study, we found herbal water with a mean zone of inhibition of 30 ± 0.88 mm, which was slightly better than CHX with a zone of inhibition of 28.3 ± 0.33 mm. Zone of inhibition against S. mutans was least in ozonated water which was 16 ± 0.58 mm when compared to herbal water and CHX. This might be due to the fact that ozonated water has a short half-life as ozone lasts at full strength in water for as little as 20 minutes. This was in contrast with an in vitro study by Anand et al. where ozonated water showed complete inhibition of S. mutans and E. feacalis.16 Concentration of O3 was 2.4 mg/L per minute (>2 ppm) similar to the study by Katti et al.17
Oral Health Status
Debris Index-simplified Score
All the groups including water group showed a reduction of DI-S score after 15 days. These values slightly increased after a follow-up of 15 days (T3) without using mouthrinses but was significantly lesser than the baseline scores. All groups showed maximum reduction in DI-S score during the use of mouthrinses. From this study, it was clear than even normal rinsing with water can remove debris. Ozonated water was comparatively better in reducing debris after 15 days of usage of mouthrinses and at the end of the follow-up period.
Calculus Index-simplified Score
The reduction in CI-S score was seen only in herbal water group, whereas there was no change in calculus status in ozonated water and CHX groups after using mouthrinses for 15 days. Supragingival calculus is essentially a mineralized plaque. Immature calculus formation would be more accelerated due to other factors like poor brushing, diet, or any medications, as mouthrinse is just an adjunct that can lead to early mineralization. Moreover, there is a higher tendency to calculus formation in lingual aspects of lower anterior and buccal aspects of upper posterior tooth surfaces due to the location of the submandibular and parotid ducts location. The presence of the low sucrose concentration in saliva with a high saliva film velocity promoting clearance of salivary sugar and acid from plaque, and the higher plaque pH associated to better access to salivary urea in these areas tends to promote base formation to plaque and calcium phosphate precipitation.18,19 This can lead to calculus formation in a faster stage. Clearly, herbal water was the only mouthrinse that was found to be better in reducing calculus when compared to others after 30 days. A probable explanation might be that herbal water was successful in reducing the immature calculus formation. After follow-up for 15 days without mouthrinses, CI-S score increased significantly more than the baseline value in all the groups except herbal water group. This was another conclusive finding in our study that after cessation of mouthrinses use, there was more calculus formation than when with use of mouthrinses. In water group, CI-S score increased throughout the study period in both with/without rinsing. Water rinsing might not be effective in preventing further calculus formation.
Oral Hygiene Index-simplified Score
There was a reduction in OHI-S score in herbal water, ozonated water, and CHX groups after 15 days. Ozonated water and CHX showed a significant increase in OHI-S after 15 days without mouthrinses but did not reach up to their previous baseline values. Maximum reduction of OHI-S score was during the use of mouthrinse. Though water had a slight decrease in OHI-S score, it was not clinically significant. Ozonated water was more effective in reducing overall OHI-S score followed by CHX after 15 days of use of mouthrinses. But, by the end of the study, herbal water was found to be effective in having the least OHI-S score which might be due to the Hawthorne effect. This was in contrast with the study conducted by Ahmed et al., where he found CHX was more effective than tulsi extract (herbal) mouthrinse in the age group of 15 years in reducing OHI-S score. But their study had a short duration of 2 weeks.6 Our study period was 30 days which involved a follow-up of 15 days without mouthrinses.
Salivary S. mutans
There was a reduction in S. mutans count in all the groups except water after usage of mouthrinses for 15 days. Interestingly, these counts further decreased in all the groups except water at the end of 30 days. CHX was found to be more effective in reducing S. mutans count followed by herbal water and ozonated water. CHX indirectly affects the enzymatic function of dehydrogenase and adenosine triphosphatase present in the cell wall of bacteria resulting in the disruption of cell membrane.6,20 Various studies in the literature have showed the superiority of chlorhexidine when compared with other ingredients in reducing S. mutans.6 Effectiveness of herbal water may be attributed to single active component (tulsi) or combination of other herbal ingredient traces acting against S. mutans. Moreover, the dosage optimization of herbal water was obtained in vitro from its zone of inhibition against S. mutans to know its antimicrobial activity. Ozonated water had significantly influenced the S. mutans population under in vivo condition rather than in vitro study against S. mutans. Ozone when dissociates into oxygen, creates an oxygen-rich environment, thus disturbing the normal ecosystem of the plaque. The enzymatic control system of the cell is blocked as ozone inhibits glycoproteins, glycolipids, and other amino acids; the outcome of which is the functional cessation and death of the microorganism.21 Anumula et al. compared the antibacterial efficacy of freshly prepared ozonated water with CHX against S. mutans for 14 days and concluded that ozonated water showed significant reduction of mutan Streptococcus count and could be used as an alternative to CHX.22 Though CHX was found to be superior to herbal water and ozonated water, one cannot rule out that it has shortcomings such as mucosal desquamation, impaired wound healing, and fibroblast attachment to the tooth surfaces.12,23
The literature search showed no ill effects of tulsi on human beings, so one can confidently recommend the use of tulsi as a mouthrinse, especially for rural population which has an easy access to tulsi and it is also highly cost-effective. One disadvantage using tulsi we observed in our study was that few participants initially had a slight unacceptance toward the bitter taste of tulsi. Tulsi tastes hot and bitter but is said to penetrate the deep tissue and dry tissue secretions.8 Ozonated water is also cost-effective as for purifying water with a lower power, ozone generators at cheaper rates are also available in the market. In our study, the participants who used ozonated water were more willingful to use it as its appearance did not differ much from the normal water other than in slight change in odor and taste. The only shortcoming is that O3 molecule is unstable and ozonated water should be prepared immediately before use. Its oxidizing property gradually decreases with time.22
Limitations
There is a need to study the long-term effects of the mouthrinses on oral health with a larger sample. The role of these mouthrinses needs to be assessed with emphasis on individuals with poor oral hygiene with different caries status, to get better picture of the antibacterial properties of these mouthrinses. Further studies are required to find the optimum ozonation time and concentration as required for mouthrinse.
CONCLUSION
Ozonated water was more effective in reducing debris followed by herbal water and CHX.
Herbal water was the only mouthrinse that was found to be effective in reducing calculus.
Chlorhexidine was found to be the most effective in reducing S. mutans count when compared with other mouthrinses studied.
From this study, it is clear that herbal water and ozonated water can be used as an alternative to CHX.
CLINICAL SIGNIFICANCE
Herbal water and ozonated water can be used in children instead of chemical mouthrinses to avoid any adverse effects. Moreover, they are safer and cost-effective.
ACKNOWLEDGMENT
ICPA Health Products LTD, India.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. Am J Dent. 2009;22(1):3–8. [PubMed] [Google Scholar]
- 2.Kaur RK, Singh MP, Chopra R, et al. To evaluate the efficacy of three commercially available herbal mouthwashes in treatment of chronic gingivitis: a comparative clinical study. Int J Dent Med Res. 2014;1(4):42–46. [Google Scholar]
- 3.Nagayoshi M, Fukuizumi T, Kitamura C, et al. Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol Immunol. 2004;19(4):240–246. doi: 10.1111/j.1399-302X.2004.00146.x. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Deshmukh MA, Dodamani AS, Karibasappa G, et al. Comparative evaluation of the efficacy of probiotic, herbal and chlorhexidine mouthwash on gingival health: a randomized clinical trial. J Clin Diagn Res. 2017;11(3):ZC13–ZC16. doi: 10.7860/JCDR/2017/23891.9462. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagappan N, John J. Antimicrobial efficacy of herbal and CHX mouth rinse –a systematic review. J Dent Med Sci. 2012;2(4):5–10. [Google Scholar]
- 6.Ahmed SI, Sekhara Reddy VC, Sudhir KM, et al. Effect of tulsi extract and honey mouthrinses on salivary Streptococcus mutans count in comparison with 0.2% of chlorhexidine: a randomized controlled trial. J Indian Assoc Public Health Dent. 2017;15:306–311. doi: 10.4103/jiaphd.jiaphd_55_17. DOI: [DOI] [Google Scholar]
- 7.Mehta S, Pesapathy S, Joseph M, et al. Comparative evaluation of a herbal mouthwash (Freshol) with chlorhexidine on plaque accumulation, gingival inflammation, and salivary Streptococcus mutans growth. J Int Soc Prev Communit Dent. 2013;3(1):25–28. doi: 10.4103/2231-0762.115717. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal P, Nagesh L. Comparative evaluation of efficacy of 0.2% chlorhexidine, listerine and tulsi extract mouth rinses on salivary Streptococcus mutans count of high school children-RCT. Contemp Clin Trials. 2011;32(6):802–808. doi: 10.1016/j.cct.2011.06.007. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Hems RS, Gulabivala K, Ng YL, et al. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. 2005;38(1):22–29. doi: 10.1111/j.1365-2591.2004.00891.x. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Arita M, Nagayoshi M, Fukuizumi T, et al. Microbicidal efficacy of ozonated water against Candida albicans adhering to acrylic denture plates. Oral Microbiol Immunol. 2005;20(4):206–210. doi: 10.1111/j.1399-302X.2005.00213.x. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Baysan A, Lynch E. The use of ozone in dentistry and medicine. Part 2. Ozone and root caries. Prim Dent Care. 2006;13(1):37–41. doi: 10.1308/135576106775193897. DOI: [DOI] [PubMed] [Google Scholar]
- 12.Bezrukova IV, Petrukhina NB, Voinov PA. Experience in medical ozone use for root canal treatment. Stomatologiia (Mosk) 2005;84(6):20–22. [PubMed] [Google Scholar]
- 13.Piaget J. Piaget and his school. Piaget's theory. Springer Berlin Heidelberg; 1976. pp. 11–23. [Google Scholar]
- 14.WHO Oral Health Surveys - Basic Methods, 4th ed., New Delhi: A. I. T. B. S. Publishers and Distributors; 1997. [Google Scholar]
- 15.Agarwal P, Nagesh L, Murlikrishnan. Evaluation of the antimicrobial activity of various concentrations of Tulsi (Ocimum sanctum) extract against Streptococcus mutans: an in vitro study. Indian J Dent Res. 2010;21(3):357–359. doi: 10.4103/0970-9290.70800. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Anand SK, Ebenezar AV, Anand N, et al. A comparative analysis of antimicrobial property of wine and ozone with calcium hydroxide and chlorhexidine. J Clin Diagn Res. 2015;9(6):ZC04–ZC06. doi: 10.7860/JCDR/2015/11355.6030. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katti SS, Chava VK. Effect of ozonised water on chronic periodontitis - a clinical study. J Int Oral Health. 2013;5(5):79–84. [PMC free article] [PubMed] [Google Scholar]
- 18.Dawes C, MacPherson LM. The distribution of saliva and sucrose around the mouth during the use of chewing gum and the implications for the site specificity of caries and calculus deposition. J Dent Res. 1993;72(5):852–857. doi: 10.1177/00220345930720050401. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Löe H, Mandell M, Derry A, et al. The effect of mouthrinses and topical application of chlorhexidine on calculus formation in man. J Periodontal Res. 1971;6(4):312–314. doi: 10.1111/j.1600-0765.1971.tb00623.x. DOI: [DOI] [PubMed] [Google Scholar]
- 20.Löe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5:79–83. doi: 10.1111/j.1600-0765.1970.tb00696.x. DOI: [DOI] [PubMed] [Google Scholar]
- 21.Celiberti P, Pazera P, Lussi A. The impact of ozone treatment on enamel physical properties. Am J Dent. 2006;19:67–72. [PubMed] [Google Scholar]
- 22.Anumula L, Kumar KVS, Krishna CM, et al. Antibacterial activity of freshly prepared ozonated water and chlorhexidine on mutans streptococcus when used as an oral rinse – a randomised clinical study. J Clin Diagn Res. 2017;11(7):ZC05–ZC08. doi: 10.7860/JCDR/2017/26708.10129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cline NV, Layman DL. The effects of chlorhexidine on the attachment and growth of cultured human periodontal cells. J Periodontol. 1992;63(7):598–602. doi: 10.1902/jop.1992.63.7.598. DOI: [DOI] [PubMed] [Google Scholar]