To the Editor: First described in Wuhan, China, in late December 2019, coronavirus disease 2019 (COVID-19) has emerged as a global public health emergency. Countries across the world are rapidly reporting new infections and case fatalities.1 As the COVID-19 pandemic rapidly evolves, understanding symptoms and clinical characteristics of affected persons is essential. Patients with COVID-19 often present with fever, cough, and fatigue, although organ-specific symptoms have been reported.2 , 3 The primary aim of this study was to systematically review published and preprint articles describing cutaneous symptoms associated with COVID-19 presentation.
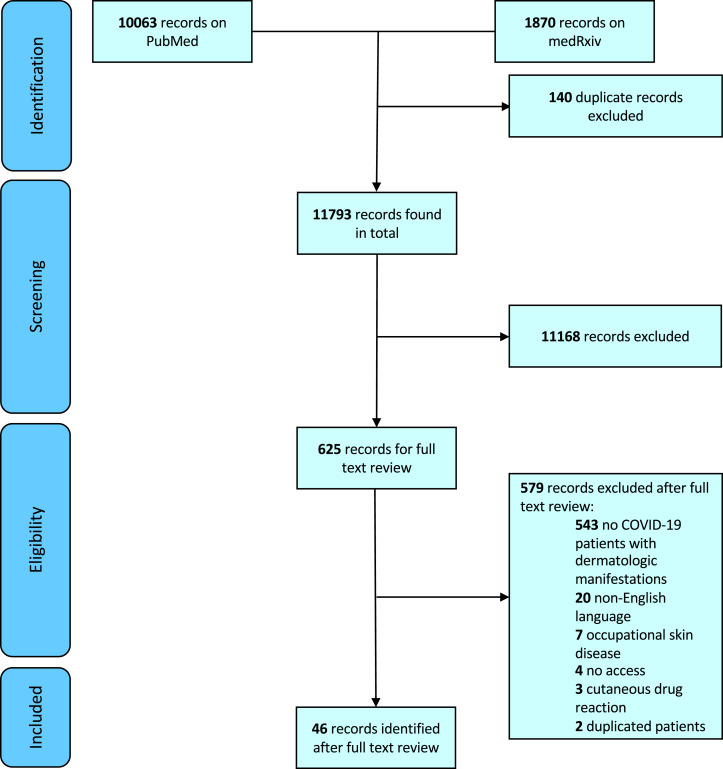
Literature for this review was identified by searching the PubMed/MEDLINE database for published articles and the medRxiv database for preprint ones. Search terms “COVID-19,” “2019-nCoV,” and “coronavirus” were used to capture articles associated with COVID-19. All articles published between December 31, 2019, and May 3, 2020, were included. Screening and review of articles were conducted in accordance with the Preferred Reporting Items for Systematic and Meta-Analysis (Fig 1 ). Reviewers conducted full-text reviews for 625 articles to identify English-language studies describing cutaneous manifestations associated with COVID-19.
Fig 1.
PRISMA diagram for inclusion of records in systematic review.
Forty-six articles met inclusion criteria, with a pooled total of 998 unique patients from 9 countries with skin manifestations related to COVID-19. A minority of articles contained more than 5 patients with cutaneous presentations of COVID-19 (Table I ). The most commonly reported skin finding was chilblain-like lesions (402, 40.2%), followed by maculopapular lesions (227, 22.7%), urticarial lesions (89, 8.9%), vesicular lesions (64, 6.4%), livedoid and necrotic lesions (28, 2.8%), and other or nondescript rashes and skin lesions (192, 19.8%). Pain and burning was reported in at least 85 cases, and itch was reported in at least 256 cases. Reported prevalence of cutaneous manifestations of COVID-19 were variable. In non–case report studies that contained patients with and without skin findings related to COVID-19, skin disease prevalence varied from 0.19% to 20.45%.11 , 13
Table I.
Articles with more than 5 patients that described skin disease associated with presentation of COVID-19
| Article | Year and location | Design | Population | Cases with cutaneous manifestations related to COVID-19 (%) | Cutaneous manifestations | Anatomic location of skin lesion | Notes |
|---|---|---|---|---|---|---|---|
| Bouaziz et al4 | 2020; France | Retrospective; multicenter | 14 | 14 (100) | Inflammatory lesions (7), vascular lesions (7) | COVID-19 symptoms before skin lesion onset (14) | |
| Duong et al5 | 2020; France | Prospective; crowdsourced social media | 295 | 295 (100) | Chilblain-like lesion (146), other skin eruption (149) | ||
| Fernandez-Nieto et al6 | 2020; Spain | Retrospective | 346 | 132 (38.2)∗ | Chilblain-like lesion (95), erythema multiform–like lesion (37) | Chilblain-like lesions (hand [33], feet [73]), erythema multiform–like lesions (hand [8], feet [35]) | Skin lesion at COVID-19 symptom onset (3), COVID-19 symptoms before skin lesion onset (16); no diagnosis of pneumonia (132/132) |
| Galván Casas et al7 | 2020; Spain | Prospective; crowdsourced survey | 429 | 375 (87.4) | Maculopapular lesion (176), urticarial lesion (73), pseudochilblain lesion (71), vesicular lesion (34), livedoid/necrotic lesion (21) | Pseudochilblain (acral), vesicular (some trunk, limbs, diffuse), urticarial (mostly trunk or diffuse, few palmar), maculopapular (diffuse, few extremities), livedoid/necrotic (trunk, acral) | Itch (213), pain (32), burning (22) |
| Landa et al8 | 2020; Spain | Retrospective; multicenter | 6 | 6 (100) | Chilblain-like lesions (6) | Foot (5), hand and foot (1) | Pain (3), itch (2); skin lesion led to diagnosis of pneumonia (1) |
| Marzano et al9 | 2020; Italy | Prospective; multicenter | 22 | 22 (100) | Varicella-like exanthem (22) | Trunk (18), trunk and limbs (4) | Itch (8), pain (2), burning (2), itch/burning (1); COVID-19 symptoms usually before skin findings |
| Piccolo et al10 | 2020; Italy | Prospective; crowdsourced survey | 63 | 63 (100) | Chilblain-like lesions ([63: 54 had photos]; 31/54 erythematous-edematous, 23/54 blistering) | Feet (86%), hands (6%), both (7%) | Pain (27%), itch (27%), pain/itch (21%); most patients had lesions at diagnosis |
| Recalcati11 | 2020; Italy | Prospective; single institution | 88 | 18 (20.5) | Erythematous rash (14), widespread urticaria (3), chicken pox–like vesicles (1) | Trunk was most involved region | Cutaneous manifestations at onset (8); cutaneous manifestation developed after hospitalization (10) |
| Recalcati et al12 | 2020; Italy | Prospective; single institution | 121 | 14 (11.6) | Erythematoviolaceus acral rash, digital welling | Feet (8), hands (4), hands and feet (2) | Itch (3); children (11), young adults (3) |
COVID-19, Coronavirus disease 2019.
Nonacral skin lesions excluded from counts per article methods.
Higher reporting of chilblain-like lesions may have occurred because some studies focused on this finding or anatomic region specifically.6 , 8 , 10 Disparities among reported cutaneous manifestation prevalence suggest a potential underreporting of skin diseases associated with COVID-19. This is concerning because cutaneous manifestations can be the presenting complaint of COVID-19 patients amid mild or absent more common COVID-19 symptoms.6 , 8 , 14 For instance, the presenting symptom for one patient with COVID-19 was urticaria; the patient sought care twice before being identified as having coronavirus.14 Misclassification of COVID-19 patients as not having the disease can hinder community transmission control efforts because of potential asymptomatic transmission.15 Future studies should include race/ethnicity information because some skin findings may be more common in skin of color. Limitations of this systematic review include few large or comprehensive studies, and that some articles included patients with suspected but unverified COVID-19.
The American Academy of Dermatology has recently launched a much-needed COVID-19 registry to track cutaneous manifestations associated with disease presentation.16 , 17 Careful documentation and robust reporting of cutaneous manifestations associated with COVID-19 are needed to augment our understanding of disease presentation and epidemiology.17 Improved understanding of cutaneous manifestations, comorbidities, and treatments will enhance our ability to provide better clinical care and support our colleagues on the front lines of this rapidly evolving pandemic.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
Reprints not available from the authors.
References
- 1.World Health Organization Coronavirus disease 2019 (COVID-19) situation report - 112. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200511-covid-19-sitrep-112.pdf?sfvrsn=813f2669_2 Accessed May 4, 2020.
- 2.Guan W., Ni Z., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158(6):1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouaziz J.D., Duong T., Jachiet M., et al. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duong T.A., Velter C., Rybojad M., et al. Did Whatsapp® reveal a new cutaneous COVID-19 manifestation? J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandez-Nieto D., Jimenez-Cauhe J., Suarez-Valle A., et al. Characterization of acute acro-ischemic lesions in non-hospitalized patients: a case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–e63. doi: 10.1016/j.jaad.2020.05.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galván Casas C., Català A., Carretero Hernández G., et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020 doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landa N., Mendieta-Eckert M., Fonda-Pascual P., Aguirre T. Chilblain-like lesions on feet and hands during the COVID-19 pandemic. Int J Dermatol. 2020;59:739–743. doi: 10.1111/ijd.14937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marzano A.V., Genovese G., Fabbrocini G., et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83(1):280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piccolo V., Neri I., Filippeschi C., et al. Chilblain-like lesions during COVID-19 epidemic: a preliminary study on 63 patients. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 12.Recalcati S., Barbagallo T., Frasin L.A., et al. Acral cutaneous lesions in the time of COVID-19. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guan W., Liang W., Zhao Y., et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu S., Lin J., Zhang Z., et al. Alert for non-respiratory symptoms of coronavirus disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. [DOI] [PubMed] [Google Scholar]
- 15.Bai Y., Yao L., Wei T., et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freeman E.E., McMahon D.E., Fitzgerald M.E., et al. The AAD COVID-19 Registry: crowdsourcing dermatology in the age of COVID-19. J Am Acad Dermatol. 2020;83(2):509–510. doi: 10.1016/j.jaad.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant-Kels J.M., Sloan B., Kantor J., Elston D.M. Letter from the editors: big data and cutaneous manifestations of COVID-19. J Am Acad Dermatol. 2020;83(2):365–366. doi: 10.1016/j.jaad.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]