Abstract
Objective
To explore the implications of direct-to-consumer pharmacogenomic testing for community pharmacy practice.
Summary
In October 2018, the U.S. Food and Drug Administration provided approval for direct-to-consumer genetic testing company, 23andMe® (Mountain View, CA), to return select pharmacogenomic test results to their customers. Given the community pharmacist’s high accessibility to the public and in-depth knowledge of pharmacology, as well as the availability of direct-to-consumer genetic testing kits at pharmacies, it is likely that patients will present their pharmacogenomic test results to their pharmacists and expect them to incorporate those results into their care. It is important, therefore, that community pharmacists are aware of the clinical implications of these results, know where to turn for evidence-based clinical pharmacogenomics information, and be mindful of the need for confirmatory testing before changing therapy.
Conclusion
Community pharmacists are at the frontlines of healthcare and as such, will be at the frontlines of direct-to-consumer pharmacogenomic testing. In the near future, it is likely that community pharmacists will need to counsel patients on the interpretation and appropriate use of direct-to-consumer pharmacogenomic test results.
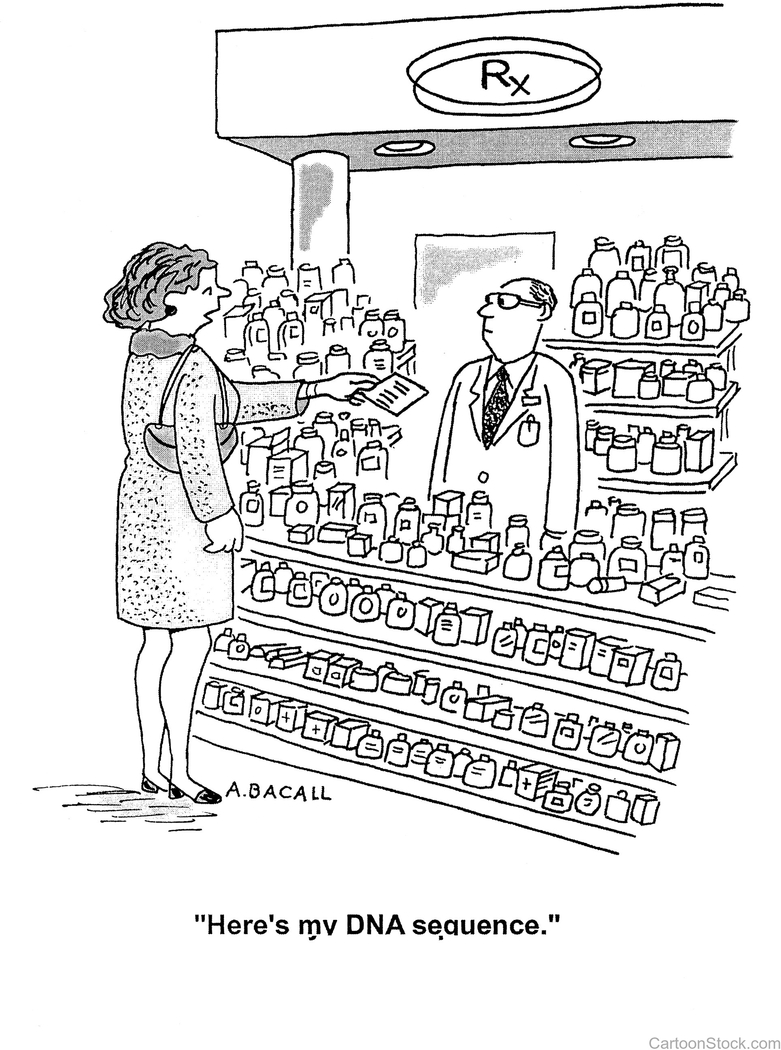
In the year 2000, three years shy of the completion of the Human Genome Project, artist Aaron Bacall (1939–2015) drew a cartoon featuring a woman nonchalantly handing a piece of paper to her (somewhat perplexed-looking) community pharmacist with a caption that read, “Here’s my DNA sequence” (Figure 1). The image was a vision of the future – the lofty goal of the tremendous international efforts underway to sequence all three billion base pairs of the human genome. One day, our genetic blueprint would find its way into routine medical care, and even into the hands of our local community pharmacist.
Figure 1.
Aaron Bacall’s “Here’s my DNA sequence” cartoon published in 2000. Licensed for publication in JAPhA by www.CartoonStock.com.
That day has come (almost)
On October 31, 2018, the U.S. Food and Drug Administration (FDA) gave the green light to direct-to-consumer genetic testing company 23andMe® (Mountain View, CA) to return select pharmacogenomic test results to their customers (Table 1).1,2 The test includes 33 genetic variants across eight pharmacogenes that are relevant for the prescribing of several medications, some of which are commonly prescribed. The popularity of this test offering remains to be seen, but with current trends and public interest in direct-to-consumer genetic testing, the impact could be substantial.3,4 Direct-to-consumer genetic testing kits are currently available for sale at community pharmacies; therefore, a critical pre-test counseling point for pharmacists to convey to their patients purchasing these kits is that they should not make any changes to their medication therapy on their own based on the results. Despite acknowledging the accuracy of the test results, the FDA contends that these results should not be used to change a patient’s medication therapy and that confirmatory pharmacogenomic testing should be completed by a clinical laboratory before any medical decisions are made. Nonetheless, patients armed with this new information about their genetic predisposition to medication response will undoubtedly approach their physicians and pharmacists with questions about its clinical utility. This new development will drive a paradigm shift in how community pharmacists interact with pharmacogenomic data; no longer is pharmacogenomics primarily relevant for the minority of community pharmacists whose pharmacies offer clinical pharmacogenomic testing services – it is now fair game for everyone.
Table 1.
Genes and variants approved by FDA for 23andMe’s® direct-to-consumer pharmacogenomic test and corresponding medications with Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines (as of March 2019).2
| Gene | Variants | Drugs with CPIC guidelines |
|---|---|---|
| CYP2C9 | *2, *3, *5, *6, rs7089580 | phenytoina, warfarina |
| CYP2C19 | *2, *3, *17 | amitriptylinea, citaloprama, clomipramine, clopidogrela, doxepin, escitaloprama, imipramine, sertralinea, trimipramine, voriconazole |
| CYP2D6 | *2, *3, *4, *5, *6, *7, *8, *9, *10, *11, *15, *17, *20, *29, *35, *40, *41 | amitriptylinea, atomoxetinea, clomipramine, codeine, desipramine, doxepin, fluvoxamine, imipramine, nortriptylinea, ondansetrona, paroxetinea, tamoxifen, tramadola,b, trimipramine |
| CYP3A5 | *3 | tacrolimus |
| DPYD | *2A, rs67376798 | 5-fluorouracil, capecitabine |
| TPMT | *2, *3C | 6-mercaptopurine, azathioprine, thioguanine |
| SLCO1B1 | *5 | simvastatina |
| UGT1A1 | *6, *28 | atazanavir |
For nearly a decade, community pharmacists have been called upon to champion pharmacogenomic testing in their practices.5,6 Community pharmacists are highly accessible healthcare providers with in-depth knowledge of pharmacology; thus, they are particularly well-positioned to advance the use pharmacogenomics in clinical practice.7 Interpreting pharmacogenomic test results and using them to optimize medication-related outcomes seems like a natural extension of traditional medication therapy management services.6,8 However, challenges remain and uptake of pharmacogenomic testing services in community pharmacies remains slow. A search of the PubMed® database (1966 to November 2018) with the keywords (pharmacogenomics or pharmacogenetics) and (community) and (pharmacy or pharmacist) yields few primary articles describing or evaluating a pharmacogenomic testing service in a community pharmacy setting in the United States.9–12 Most of those (n = 3) focus solely on the implementation of CYP2C19-guided clopidogrel therapy, with one recent feasibility study focusing on testing for CYP2C9, CYP2C19, CYP2D6, SLCO1B1, and VKORC1.9 Several papers report on surveys of community pharmacists13–15 and patients4 about their attitudes towards, and experiences with, pharmacogenomic testing in the community pharmacy setting. Although these studies revealed positive perceptions of patients and community pharmacists towards pharmacogenomic testing, the majority of community pharmacists are not confident in their ability to make gene-based dosing recommendations due to lack of knowledge of genetic variation and its impact on drug response.
The introduction of direct-to-consumer pharmacogenomic testing will force a new model of pharmacogenomics implementation in community pharmacy settings. Current models of pharmacogenomics implementation in community pharmacies are reactive in nature (e.g., a patient has already been prescribed clopidogrel, which prompts a recommendation for CYP2C19 genotyping), with the test ordering driven by a healthcare provider at the community pharmacist’s recommendation. 23andMe’s direct-to-consumer pharmacogenomic test provides an avenue for preemptive testing, which in turn shifts the central question of “should I order a pharmacogenomic test for this patient?” to “what should I do with the test results in hand?” As a result, cost and insurance reimbursement for the test are no longer part of the equation at the point of interaction between patient and pharmacist, and neither is clinician involvement in the decision to order the test in the first place. Nonetheless, it is important for the community pharmacist to be prepared to provide the necessary counseling to these patients if presented with direct-to-consumer pharmacogenomic test results.
So, what does a community pharmacist need to know to be prepared to counsel their patients on direct-to-consumer pharmacogenomic test results? Here are some important considerations to keep in mind:
At this time, direct-to-consumer pharmacogenomic test results should not be used to change a patient’s medication therapy. Per FDA guidance, confirmatory pharmacogenomic testing should be completed by a clinical laboratory before any medical decisions are made. Pharmacists should also be aware that some clinical laboratories return pharmacogenomic test results that may not have clinical utility.
Evidence-based gene/drug clinical practice guidelines are available through the Clinical Pharmacogenetics Implementation Consortium (CPIC; www.cpicpgx.org). These guidelines provide genotype to phenotype translation and offer gene-based prescribing recommendations.16–30 New guidelines for additional gene/drug pairs are published each year, and guideline updates are posted to the CPIC website as new evidence emerges.
Over 200 medications have pharmacogenomic information in their FDA-approved drug label, some of which is relevant to drug dosing. A complete list of pharmacogenomic biomarkers in FDA-approved drug labels, along with the section of the label where the relevant information is found, is available on the FDA website.31
A wild-type (e.g., *1/*1) result (no abnormal genetic variation detected) is not a guarantee of “normal” metabolism. Most clinical pharmacogenomic tests interrogate a limited number genetic variants; therefore, it is possible that the patient harbors additional variants that impact drug metabolism and response. More comprehensive testing may be warranted, and repeat test results may differ from the direct-to-consumer test results if another lab tests for different genetic variants.
Not all “non-normal” phenotypes are actionable (i.e., require a change in drug dosing or drug choice). Consult CPIC guidelines to determine which phenotypes are actionable for which medications.
Pharmacogenomic test results should not always be acted upon, even if the phenotype is considered “actionable.” In the case of ongoing therapy where a patient is tolerating a medication well with good effect, intervening based on pharmacogenomic test results may not be appropriate (e.g., patient has a high-risk result for simvastatin-induced myopathy, but the patient does not report symptoms of myalgia).
Genetics is just one piece of the clinical puzzle and must be used in the context of other clinical variables to derive the best pharmacotherapeutic plan for a patient. For example, drug-drug interactions may impact the patient’s phenotype for a particular gene (e.g., a CYP2D6 normal metabolizer by genotype may require the dosing recommendation of a CYP2D6 poor metabolizer if the patient is taking a strong CYP2D6 inhibitor).
Using pharmacogenomic test results is not a magic bullet, but using them to guide drug selection and dosing can increase the probability of a favorable medication outcome, minimize trial and error prescribing, and help clinicians choose between therapeutic equals.
Pharmacogenomic test results are relevant lifelong, so patients should be counseled to inform all future prescribers of their results. Ideally, these test results should be recorded in the patient profile, with high-risk phenotypes flagged, so that other pharmacists are aware of them upon dispensing future medications. This relates to the larger issue of needing drug-gene interaction decision support – akin to commonly used drug-drug interaction decision support – for optimal use of pharmacogenomic information over time. However, until such decision support systems are created, the patient must take responsibility for their medical information and inform future prescribers of their results so that their therapy can be tailored accordingly.
Ultimately, although no medication changes should be made based on the direct-to-consumer pharmacogenomic test results alone, an important role for the community pharmacist will be to recognize when a pharmacogenomic test is actionable for a patient’s current or potential future therapy and provide appropriate guidance as to whether it would be beneficial for patients to consider confirmatory testing and seek further consultation with their primary care provider. This role is consistent with the American Pharmacists Association (APhA) 2018 policy statements on the use of genomic data within pharmacy practice, which states that APhA “emphasizes genomics as an essential aspect of pharmacy practice” and “recognizes pharmacists as the health care professional best suited to provide medication-related consults and services based on a patient’s genomic information.”32 In addition, this statement acknowledges the value of pharmacists’ services in this area, and likewise “demands that payers include pharmacists as eligible providers for covered genomic interpretation and related services to support sustainable models that optimize patient care and outcomes.”
The science and clinical application of pharmacogenomics was added to the Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree in 2016.33 While this is an important step in ensuring student pharmacists are introduced to basic pharmacogenomics concepts and key resources (e.g., CPIC guidelines), the pressing issue of educating our current pharmacy workforce remains. Pharmacogenomics competencies for pharmacists have previously been described and can be found on the Genetics/Genomics Competency Center (G2C2) website (https://genomicseducation.net/). 34 As the medication experts, pharmacists have a responsibility to understand all clinical factors that impact drug response, including genetics. As such, all pharmacists need to be ready to field clinical pharmacogenomics questions from both patients and providers alike. For community pharmacists looking to advance their pharmacogenomics knowledge, several professional pharmacy organizations and academic institutions are offering pharmacogenomics certificate programs for continuing education credit. In addition, helpful online resources include the Pharmacogenomics Knowledge Base (PharmGKB; www.pharmgkb.org) and St. Jude Children’s Research Hospital’s pharmacogenomics implementation resources for professionals, which includes links to publications and presentations on pharmacogenomics.35 To ensure an adequately trained workforce, community pharmacies may want to encourage or require a specified number of continuing education credits related to pharmacogenomics. The core educational needs and preferences of community pharmacists, as pertaining to the successful provision of clinical pharmacogenomics services in community pharmacies, have recently been described.36 A focused effort on educating current and future pharmacists about pharmacogenomics is critical to improving pharmacist confidence and competence in making gene-based dosing recommendations. Beyond ensuring the preparedness of individual pharmacists through education, at the corporate and ownership levels, it may be prudent for pharmacy management to create standards and policies that support pharmacists in the implementation of any program related to direct-to-consumer pharmacogenomic testing in order to mitigate the potential burden from additional workload.
Community pharmacists are at the frontlines of healthcare and as such, will be at the frontlines of direct-to-consumer pharmacogenomic testing. Just as cartoonist Aaron Bacall envisioned nearly 20 years ago, it is likely that in the near future patients will be presenting their pharmacogenomic test results to their local community pharmacist and asking for interpretation and integration of these results into their care. Community pharmacists, therefore, will need to be ready to provide the appropriate counseling with respect to the clinical implications of those results and the need for confirmatory testing.
KEY POINTS.
- Background:
- The U.S. Food and Drug Administration recently provided approval for direct-to-consumer genetic testing company, 23andMe® (Mountain View, CA), to return select pharmacogenomic test results to their customers.
- Given the community pharmacist’s high accessibility to the public and in-depth knowledge of pharmacology, as well as the availability of direct-to-consumer genetic testing kits at pharmacies, it is likely that patients will present their pharmacogenomic test results to their pharmacists and expect them to incorporate those results into their care.
- Findings:
- Community pharmacists will need to counsel patients on the interpretation and potential clinical application of direct-to-consumer pharmacogenomic test results as well as the need for confirmatory testing prior to any medication changes.
- Evidence-based resources, like Clinical Pharmacogenetics Implementation Consortium guidelines, are available to help community pharmacists understand the clinical implications of patients’ direct-to-consumer pharmacogenomic test results and provide appropriate counseling.
Acknowledgments
Funding: RSG and KEC are funded by the National Institutes of Health (NIH) for CPIC (R24GM115264 and U24HG010135).
Footnotes
Declarations of interest: None
Contributor Information
Roseann S. Gammal, Assistant Professor of Pharmacy Practice, MCPHS University School of Pharmacy, Boston, MA.
Jason Mayes, Pharmacy Manager, Kroger Pharmacy, Cold Spring, KY.
Kelly E. Caudle, CPIC Director, St. Jude Children’s Research Hospital, Memphis, TN.
REFERENCES
- 1.FDA authorizes first direct-to-consumer test for detecting genetic variants that may be associated with medication metabolism. 2018; https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm Accessed Feb. 14, 2019.
- 2.2019; https://www.accessdata.fda.gov/cdrh_docs/pdf18/DEN180028.pdf Accessed Feb. 15, 2019.
- 3.Ramos E, Weissman SM. The dawn of consumer-directed testing. Am J Med Genet C Semin Med Genet. 2018;178(1):89–97. [DOI] [PubMed] [Google Scholar]
- 4.Gibson ML, Hohmeier KC, Smith CT. Pharmacogenomics testing in a community pharmacy: patient perceptions and willingness-to-pay. Pharmacogenomics. 2017;18(3):227–233. [DOI] [PubMed] [Google Scholar]
- 5.Padgett L, O’Connor S, Roederer M, McLeod H, Ferreri S. Pharmacogenomics in a community pharmacy: ACT now. J Am Pharm Assoc (2003). 2011;51(2):189–193. [DOI] [PubMed] [Google Scholar]
- 6.Reiss SM, American Pharmacists A. Integrating pharmacogenomics into pharmacy practice via medication therapy management. J Am Pharm Assoc (2003). 2011;51(6):e64–74. [DOI] [PubMed] [Google Scholar]
- 7.Johnson JA, Weitzel KW. Advancing Pharmacogenomics as a Component of Precision Medicine: How, Where, and Who? Clin Pharmacol Ther. 2016;99(2):154–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haga SB, Allen LaPointe NM, Moaddeb J. Challenges to integrating pharmacogenetic testing into medication therapy management. J Manag Care Spec Pharm. 2015;21(4):346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haga SB, Moaddeb J, Mills R, Voora D. Assessing feasibility of delivering pharmacogenetic testing in a community pharmacy setting. Pharmacogenomics. 2017;18(4):327–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bright DR, Kisor DF, Smith A, Conaway M, Yu M. Implementation of a pharmacogenetic management service for postmyocardial infarction care in a community pharmacy. Per Med. 2015;12(4):319–325. [DOI] [PubMed] [Google Scholar]
- 11.Kisor DF, Bright DR, Conaway M, Bouts BA, Gerschutz GP. Pharmacogenetics in the Community Pharmacy: Thienopyridine Selection Post-Coronary Artery Stent Placement. J Pharm Pract. 2014;27(4):416–419. [DOI] [PubMed] [Google Scholar]
- 12.Ferreri SP, Greco AJ, Michaels NM, et al. Implementation of a pharmacogenomics service in a community pharmacy. J Am Pharm Assoc (2003). 2014;54(2):172–180. [DOI] [PubMed] [Google Scholar]
- 13.Moaddeb J, Mills R, Haga SB. Community pharmacists’ experience with pharmacogenetic testing. J Am Pharm Assoc (2003). 2015;55(6):587–594. [DOI] [PubMed] [Google Scholar]
- 14.Alexander KM, Divine HS, Hanna CR, Gokun Y, Freeman PR. Implementation of personalized medicine services in community pharmacies: perceptions of independent community pharmacists. J Am Pharm Assoc (2003). 2014;54(5):510–517, 515 p following 517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tuteja S, Haynes K, Zayac C, Sprague JE, Bernhardt B, Pyeritz R. Community pharmacists’ attitudes towards clinical utility and ethical implications of pharmacogenetic testing. Per Med. 2013;10(8):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caudle KE, Rettie AE, Whirl-Carrillo M, et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin Pharmacol Ther. 2014;96(5):542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson JA, Caudle KE, Gong L, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for Pharmacogenetics-Guided Warfarin Dosing: 2017 Update. Clin Pharmacol Ther. 2017;102(3):397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott SA, Sangkuhl K, Stein CM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther. 2013;94(3):317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hicks JK, Sangkuhl K, Swen JJ, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hicks JK, Bishop JR, Sangkuhl K, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Selective Serotonin Reuptake Inhibitors. Clin Pharmacol Ther. 2015;98(2):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moriyama B, Obeng AO, Barbarino J, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines for CYP2C19 and Voriconazole Therapy. Clin Pharmacol Ther. 2017;102(1):45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crews KR, Gaedigk A, Dunnenberger HM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther. 2014;95(4):376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell GC, Caudle KE, Whirl-Carrillo M, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 genotype and use of ondansetron and tropisetron. Clin Pharmacol Ther. 2017;102(2):213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goetz MP, Sangkuhl K, Guchelaar HJ, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and Tamoxifen Therapy. Clin Pharmacol Ther. 2018;103(5):770–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Birdwell KA, Decker B, Barbarino JM, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines for CYP3A5 Genotype and Tacrolimus Dosing. Clin Pharmacol Ther. 2015;98(1):19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amstutz U, Henricks LM, Offer SM, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for Dihydropyrimidine Dehydrogenase Genotype and Fluoropyrimidine Dosing: 2017 Update. Clin Pharmacol Ther. 2018;103(2):210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Relling MV, Schwab M, Whirl-Carrillo M, et al. Clinical Pharmacogenetics Implementation Consortium Guideline for Thiopurine Dosing Based on TPMT and NUDT15 Genotypes: 2018 Update. Clin Pharmacol Ther. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramsey LB, Johnson SG, Caudle KE, et al. The clinical pharmacogenetics implementation consortium guideline for SLCO1B1 and simvastatin-induced myopathy: 2014 update. Clin Pharmacol Ther. 2014;96(4):423–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gammal RS, Court MH, Haidar CE, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for UGT1A1 and Atazanavir Prescribing. Clin Pharmacol Ther. 2016;99(4):363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown JT, Bishop JR, Sangkuhl K, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 Genotype and Atomoxetine Therapy. Clin Pharmacol Ther. 2019. [Google Scholar]
- 31.Table of Pharmacogenomic Biomarkers in Drug Labeling. https://www.fda.gov/drugs/science-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling Accessed May 6, 2019.
- 32.Actions of the 2018 American Pharmacists Association House of Delegates. 2018; https://www.pharmacist.com/sites/default/files/files/2018%20Report%20of%20the%20APhA%20House%20of%20Delegates%20-%20FINAL.pdf Accessed March 10, 2019.
- 33.Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. 2016; https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf Accessed Feb. 15, 2019.
- 34.Roederer MW, Kuo GM, Kisor DF, et al. Pharmacogenomics competencies in pharmacy practice: A blueprint for change. J Am Pharm Assoc (2003). 2017;57(1):120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Implementation Resources for Professionals. 2019; https://www.stjude.org/research/clinical-trials/pg4kds-pharmaceutical-science/implementation-resources-for-professionals.html Accessed March 18, 2019.
- 36.Berenbrok LAHK, Harriman S, Coley KC, Somma McGivney MA, Empey PE. Community pharmacists’ educational needs for implementing clinical pharmacogenomic services. J Am Pharm Assoc 2019: 10.1016/j.japh.2019.1003.1005. [DOI] [PubMed] [Google Scholar]
- 37.Fuentes AV, Pineda MD, Venkata KCN. Comprehension of Top 200 Prescribed Drugs in the US as a Resource for Pharmacy Teaching, Training and Practice. Pharmacy (Basel). 2018;6(2). [DOI] [PMC free article] [PubMed] [Google Scholar]