Abstract
Social isolation is a key predictor of mortality in the US and may be heightened in communities affected by violence. Qualitative studies have documented that people living in high-crime neighborhoods often report being confined to their homes due to safety concerns. However, few quantitative studies have empirically assessed relationships between violence exposure and social isolation. In 2018, we conducted hour-long, in-person surveys with 504 adults in Chicago. Prior exposure to community violence was associated with a 3.3-point reduction (on a 100-point scale) in the frequency of interaction with network confidantes, a 7.3-point reduction in perceived social support from friends, and a 7.8-point increase in loneliness. At a time when public health and policy leaders are calling for solutions to the “epidemic of loneliness,” identifying populations at higher risk due to violence might help target interventions and ensure equitable access to social and medical support.
Introduction
A 2018 antiviolence campaign in Chicago resulted in closure of the Dan Ryan Expressway,1 a major traffic artery that runs north and south in parallel with the city’s social gradients.2 Campaign leaders blockaded the expressway near neighborhoods with some of the highest rates of violence in the city,1 attempting to force more affluent Northside residents to exit the expressway and drive through these unfamiliar and disadvantaged communities. The result, in part, was greater recognition of the steeped sentiments—largely, fear and isolation—that residents living in unsafe communities experience and must navigate on a daily basis.
While linkages between violence and social isolation are still emerging in public health, social isolation has been the source of ardent attention in recent years, and its scope is well documented.3 Epidemiological studies have estimated that one-quarter of older American adults, or approximately 7.7 million people, are socially isolated.4 Objective measures of social isolation may include living alone, having limited social contacts, or participating in few social activities.5 Loneliness, which refers to the subjective experience of being left out or excluded,6 may occur regardless of having social contacts and opportunities and affects nearly one-third of American adults ages forty-five and older.7 In the United Kingdom, high rates of loneliness have led government officials to declare loneliness a health epidemic, even appointing a minister for loneliness to oversee national strategies to curb its growth.8 Importantly, loneliness has been identified as a key predictor of mortality,9 proportional to traditional clinical risk factors such as hypertension and smoking, and it may also exacerbate adverse health behaviors.10,11
Living in an unsafe neighborhood may be an important risk factor for social isolation and loneliness. In one qualitative study, participants described community violence as a physical barrier to leaving home, as well as a social barrier to trust and neighborhood cohesion.12 John Cacioppo and colleagues theorized that human relationships require not just the presence of others but also trust, security, and the feeling of being meaningfully connected.6 The perception of a hostile or violent social environment can erode this foundation, accommodating processes that lead to subjective forms of isolation and disconnect (for example, loneliness).6 Although rich qualitative and conceptual research suggests that people living in high-crime neighborhoods may be at higher risk for social isolation,12,13 there is a paucity of quantitative data to confirm and assess the extent of this relationship.
The purpose of this study was to examine associations between exposure to community violence—including direct and indirect types of violence—using a broad subset of social isolation measures in a high-risk sample. Following typology developed by the World Health Organization, we defined community violence, broadly, as violence between people who may or may not know each other that generally takes place in public spaces outside the home.14 We hypothesized, based on prior qualitative studies,12 that there was a positive association between exposure to community violence and objective measures of social isolation. However, since distrust and anxiety in a hostile environment are not necessarily mollified by the physical presence of other people,6 we hypothesized that there was a stronger association between exposure to community violence and subjective loneliness. As a secondary objective, we examined the associations between loneliness and adverse health behaviors that constitute traditional clinical risk factors, including unhealthy dietary behavior, inadequate physical activity, medication non-adherence, alcohol consumption, and tobacco use.
Study Data And Methods
In the period June–December 2018, we recruited a sample of adult participants to complete a one-time, in-person survey. Participants were purposefully recruited from medical clinics located in two city-defined geographic regions that are epicenters of violent crime—Chicago’s South and West Sides. The South Side epicenter contained the South Side region and twenty-one adjacent community areas, including the Englewood and Avalon Park neighborhoods. This region has a population of 473,207 residents, a large proportion of whom are African American (71 percent) and have incomes below the federal poverty level (32 percent).15 The West Side epicenter contained the West Side region, including the Garfield Park and Lawndale neighborhoods. This region has a population of 481,491 residents, many of whom are African American (44 percent) or Hispanic or Latino (35 percent) and have incomes below poverty (30 percent).15
Trained research assistants approached potential participants consecutively in clinic waiting rooms. Participants were eligible to participate if they were ages eighteen and older, lived at a Chicago-based address, and were a patient at the clinical site. Surveys were administered in person either using computer-assisted personal interviewing software or verbally with a research assistant. Each survey lasted approximately sixty minutes. Upon completing the survey, participants received $20 in compensation.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guideline and was approved by the University of Chicago Institutional Review Board with written documentation of informed consent.
Measures
The primary independent variable was lifetime violence exposure, measured using items from the Brief Trauma Questionnaire.16 The questionnaire was developed by the National Center for Posttraumatic Stress Disorder (PTSD) of the Department of Veterans Affairs and is based on the Criterion A standard for classification as a traumatic event in the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition. Individual items queried participants about being a direct victim of violence (“Have you ever been [mugged or robbed or physically attacked or beaten]?”), a witness to violence (“Have you ever witnessed a situation in which someone was seriously injured or killed?”), or a close friend or family member of someone who died violently (“Has a close friend or family member died violently, for example, in an altercation, mugging, or attack?”).16 All measures were analyzed as binary variables based on yes or no responses. Being a witness of a violent death or the close friend or family member of someone who died violently was classified as having indirect exposure; being a direct victim of violence was classified as having direct exposure.
Participants were also screened for PTSD using the National Center for PTSD’s Primary Care PTSD Screen (PC-PTSD).17 This screen is considered positive if a patient answers yes to any three out of the four items.17 Although PTSD is not a violence exposure type, we analyzed this construct alongside items in the Brief Trauma Questionnaire, reasoning that violence exposure with PTSD might have stronger associations with social isolation than exposure without PTSD.
The primary dependent variables were social isolation characteristics, measured using validated items from the National Social Life, Health, and Aging Project.5,18 Individual items queried participants about social network characteristics (network confidantes, network size, spousal relationship tie, frequency of interaction, and perceived closeness), living arrangements (living alone versus with others), social participation (a five-item scale), perceived social support (a two-item scale), and loneliness (a three-item scale).18 The instrument defines a network confidante as “a person you tend to talk to about things that are important to you.”18 Similarly, a spousal relationship tie is defined as a network confidante who is a spouse or romantic partner. Social participation refers to participation in social activities, such as an organized group or volunteering. A detailed description of each social isolation measure has been described in previous work.18 All measures were normalized to a 100-point scale in the main analysis for ease in comparing data across measures. In subsequent analyses that assessed loneliness alone, loneliness was analyzed as a binary variable—similar to the practice in previous studies.5 Participants who reported “never” to all three scale items were categorized as having “no loneliness,” and those reporting “some of the time,” “often,” or “always” to any scale item were categorized as having “loneliness at least some of the time.”
Using items adapted from large national surveys, we analyzed patient-reported health behaviors as secondary dependent variables of interest.19,20 Participants were asked to think about the number of days per week during which they participated in a given health behavior “on average over the past month.” Individual items queried participants about dietary behavior (“eat five or more servings of fruits and vegetables”), physical activity (“do at least 30 minutes of physical activity”), medication adherence (“take all medications as directed by your doctor”), binge alcohol consumption (“have [four or five] or more drinks on one occasion”), and tobacco use (“use tobacco products, such as cigarettes, cigars, or chewing tobacco”), based on national guidelines published in Healthy People 2020.21
Statistical Analysis
Descriptive statistics were calculated for the sample population. Unadjusted and adjusted generalized linear models were used to independently assess each social isolation characteristic on a 100-point scale as a function of community violence exposure, controlling for age, sex, race/ethnicity, educational attainment, insurance type, and clinic location.
Chi-square independence tests were used to examine bivariate associations between the type of violence exposure (direct, indirect, or PTSD) and loneliness (no loneliness or loneliness at least some of the time). Generalized linear models, using a binomial distribution and logit link, were used to calculate the odds ratios and adjusted odds ratios for loneliness as a function of violence exposure type, controlling for the factors listed above and spousal relationship status. We also tested an interaction effect for age group (ages 35–49, 50–64, or 65 and older), reasoning that associations between violence exposure and loneliness might be stronger among older adults.
Finally, unadjusted and adjusted generalized linear models were used to assess all health behaviors (measured ordinally as the average number of days per week the behavior was performed) as a function of loneliness, controlling for all abovementioned sociodemographic characteristics. Independent models tested for fruit and vegetable consumption, physical activity, medication adherence, binge alcohol consumption, and tobacco use.
Of the 504 participants, 4.8 percent had missing data on violence exposure data (see online appendix exhibit 1),22 and an additional 4.2 percent had missing covariate data, primarily for educational attainment. We conducted analyses examining differences in participant characteristics between those with and those without missing data for the violence exposure variable (see appendix exhibit 1).22 Although by convention, a missing rate of less than 5–10 percent is generally considered acceptable,23 we minimized the effect of missing data by conducting both a complete case analysis (analyzing only cases with complete data and adjusting for all abovementioned demographic characteristics in primary analyses) and multiple imputation analyses (imputing missing data in sensitivity analyses) (see appendix exhibits 2 and 3).22 Due to high rates of missing data for annual household income (22 percent), this variable was not included in primary analyses. However, in sensitivity analyses, annual household income was imputed in addition to violence exposure and educational attainment.
Data were analyzed using Stata/SE, version 13.1.
Limitations
There were several limitations to this study. First, this was an observational study, and any causal claim is limited.
Second, the population in this study consisted of a high-exposure sample in Chicago. Results should be interpreted as most directly applicable to older members of racial/ethnic minority populations who live in high-crime urban neighborhoods.
Third, annual household income was not included in primary models because a large proportion (22 percent) had missing data for this item, as noted above. Income may be an important confounder, given the substantial literature that has documented associations between socioeconomic status and social isolation.24,25 However, we included educational attainment and insurance type in all models, and our results did not change substantively when we imputed income in sensitivity analyses (see appendix exhibits 3 and 4).22
Fourth, violence exposure measures were self-reported and therefore vulnerable to response bias. It is possible that participants were uncomfortable disclosing information about violence, despite assurances of confidentiality. However, we selected the Brief Trauma Questionnaire to measure lifetime exposure to violence because it is a DSM-based measure with applications to clinical samples.16
Study Results
The cooperation rate, defined by the American Association for Public Opinion Research as the proportion of those who were interviewed of all who were eligible and approached,26 was 61 percent. The participants’ mean age was 59.5 years (data not shown). Participants were predominantly female (71.0 percent) and non-Hispanic black (74.6 percent) (exhibit 1). A large proportion had attained a high school diploma or more (84.7 percent). More than half reported having had exposure to community violence (58.9 percent), either directly (38.9) or indirectly (46.8 percent). One in five participants screened positive for PTSD.
Exhibit 1:
Characteristics of 504 study participants in Chicago, 2018
| No. | % | |
|---|---|---|
| Type of clinic | ||
| Academic medical center | 417 | 82.7 |
| Federally qualified health center | 87 | 17.3 |
| Age group (years) | ||
| 18–34 | 5 | 1.0 |
| 35–49 | 112 | 22.2 |
| 50–64 | 200 | 39.7 |
| 65–79 | 160 | 31.8 |
| 80 and older | 27 | 5.4 |
| Female | 358 | 71.0 |
| Race/ethnicity | ||
| Non-Hispanic white | 37 | 7.3 |
| Non-Hispanic black | 376 | 74.6 |
| Hispanic or Latino | 70 | 13.9 |
| Other | 21 | 4.2 |
| Primary language | ||
| English | 447 | 88.7 |
| Spanish | 51 | 10.1 |
| Other | 6 | 1.2 |
| Educational attainment | ||
| Less than high school graduate | 77 | 15.3 |
| High school graduate or GED | 101 | 20.0 |
| Some college or a 2-year degree | 156 | 31.0 |
| 4-year college degree or more | 129 | 25.6 |
| Don’t know or refused to answer | 41 | 8.1 |
| Insurance type | ||
| Private | 165 | 32.7 |
| Medicaid, with or without Medicare | 182 | 36.1 |
| Medicare | 108 | 21.4 |
| Other | 12 | 2.4 |
| None | 32 | 6.4 |
| Don’t know or refused to answer | 5 | 1.0 |
| Exposure to community violencea | ||
| Direct | 196 | 38.9 |
| Indirect | 236 | 46.8 |
| Direct or indirect | 297 | 58.9 |
| PTSD screenb | 100 | 19.8 |
SOURCE Authors’ analysis. NOTE GED is General Educational Development certification.
Direct exposure refers to having been the victim of a robbery or assault. Indirect exposure refers to being a witness of a violent death or the close friend or family member of someone who died violently.
Having had a positive screen for posttraumatic stress disorder (PTSD) using the Primary Care PTSD Screen (see note 17 in text).
Mean social network size was similar in the groups that were exposed or not exposed to community violence (2.4 people and 2.2 people, respectively). However, prior exposure to community violence was associated with a 3.3-point reduction (95% confidence interval: −6.4, −0.3) in frequency of interaction with social network confidantes in adjusted models. A 3.4-point reduction (95% CI: −6.8, 0) in perceived closeness with network confidantes approached but did not achieve statistical significance. Prior exposure to community violence was not associated with having a spousal relationship tie, living alone, or perceived social support from family, but it was associated with a 7.3-point reduction (95% CI: −12.5, −2.0) in perceived social support from friends in adjusted models. Prior exposure to community violence was also associated with a 7.8-point increase (95% CI: 3.4, 12.2) in perceived loneliness in adjusted models. In sensitivity analyses that used multiple imputation for missing values, the results did not change significantly—even when we imputed violence exposure, educational attainment, and annual household income (see appendix exhibit 2).22
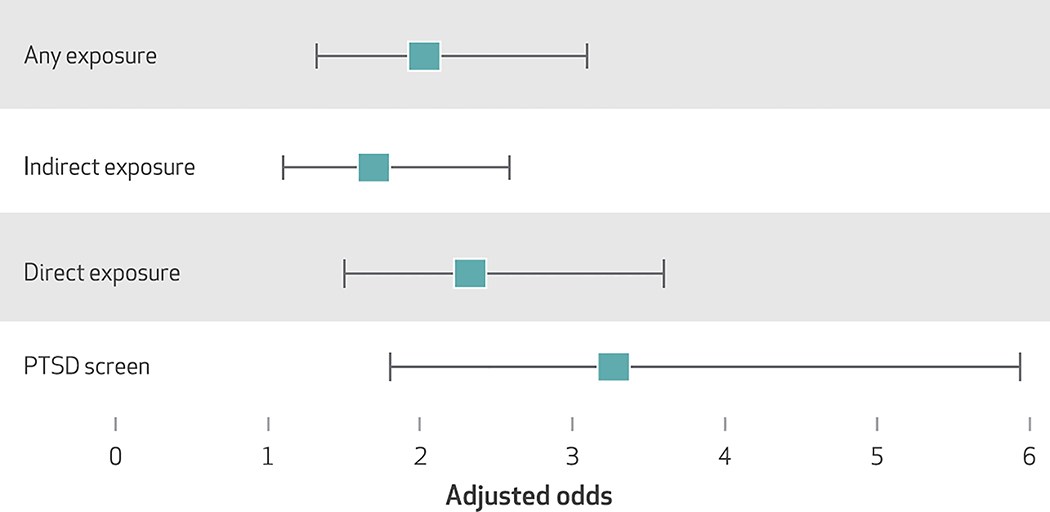
Of 450 participants, 291 (65%) reported loneliness at least some of the time. The association between exposure to community violence and loneliness increased in a graded fashion from indirect to direct exposure, with the largest effect for those who screened positive for PTSD (exhibit 3). Indirect exposure to community violence was associated with 1.7-fold higher adjusted odds (95% CI: 1.1, 2.6) of reporting loneliness at least some of the time; direct exposure was associated with 2.3-fold higher adjusted odds (95% CI: 1.5, 3.6); and PTSD was associated with 3.3-fold higher adjusted odds (95% CI: 1.8, 5.9). In stratified analyses by age, we observed a consistent trend toward higher loneliness among older adults relative to younger adults (see appendix exhibit 4),22 but the effect was not significant.
EXHIBIT 3. Adjusted odds of being lonely among study participants in Chicago, Illinois, by type of exposure to community violence and presence of posttraumatic stress disorder (PTSD), 2018.
SOURCE Authors’ analysis of data for 2018 from the Chicago Violence, Neighborhoods, and Health Study. NOTES Generalized linear models were used to estimate differences between groups that were or were not exposed to community violence, adjusting for age, sex, race/ethnicity, educational attainment, spousal relationship status, insurance type, and clinical location (academic medical center or federally qualified health center). “Indirect exposure” refers to being a witness of a violent death or the close friend or family member of someone who died violently. “Direct exposure” refers to having been the victim of a robbery or assault. “PTSD screen” refers to having had a positive screen for PTSD using the Primary Care PTSD Screen (see note 18 in text). The error bars indicate 95% confidence intervals.
Loneliness at least some of the time was associated with fewer days per week of fresh fruit and vegetable consumption (−0.5 days; 95% CI: −0.9, −0.1) and medication adherence (−0.6 days; 95% CI: −1.0, −0.2) and more days per week of binge alcohol consumption (0.4 days; 95% CI: 0.1, 0.6) and tobacco use (0.5 days; 95% CI: 0.1, 0.9) (exhibit 4). Physical activity did not differ significantly between groups by loneliness status. In sensitivity analyses with imputed income, our results remained substantively unchanged, although the association between loneliness and fresh fruit and vegetable consumption was somewhat reduced and only marginally significant (see appendix exhibit 3).22
Exhibit 4:
Association between loneliness and health behaviors of 450 study participants in Chicago, 2018
| Group | Difference between groups | |||
|---|---|---|---|---|
| Behavior | Never lonely (n = 159) | Lonely at least some time (n = 291) | Unadjusted | Adjusteda |
| Positive | ||||
| Fruit and vegetable consumptionb | 3.90 | 3.36 | −0.55*** | −0.50** |
| Physical activityb | 3.46 | 3.31 | −0.15 | −0.30 |
| Medication adherence | 6.55 | 5.89 | −0.67**** | −0.59*** |
| Adverse | ||||
| Binge alcohol consumption | 0.23 | 0.63 | 0.40*** | 0.35*** |
| Tobacco use | 0.48 | 1.09 | 0.61*** | 0.50** |
SOURCE Authors’ analysis of participants with complete data. NOTES The exhibit shows the mean number of days per week on which both groups engaged in the health behaviors listed.
Generalized linear models were used to estimate differences between people who reported being lonely and those who did not, adjusting for the variables listed in the notes to exhibit 3.
Based on the recommended daily fresh fruit and vegetable consumption and physical activity guidelines in Healthy People 2020 (see note 21 in text).
p < 0.05
p < 0.01
p < 0.001
Discussion
Exposure to community violence was associated with less frequent interaction with network confidantes, lower perceived social support from friends, and higher loneliness in this sample of urban-dwelling adults. Loneliness was nearly twice as prevalent than in the general US population,7 with 65 percent of participants reporting that they felt lonely at least some of the time. These findings build on previous qualitative studies that documented narratives of social isolation in many low-income urban communities. In an ethnographic account of the 1995 Chicago heat wave, Eric Klinenberg performed a “social autopsy” of the conditions that resulted in death for over 700 residents, many of whom were poor, elderly, and living alone.24,27 He described the pervasiveness of fear among older adults living in high-crime public housing structures, where social withdrawal was seen as a strategy for survival; and he attributed these deaths, in part, to “the alone and the afraid protecting themselves from a social world in which they no longer felt secure.”24[p507]
In our study, while network size and living arrangements were similar between groups, the frequency of interaction with network confidantes was lower among those who had been exposed to violence. Similarly, these patients reported less social support from friends, which might reflect the former finding (that is, less frequent interaction) or other barriers to meaningful support. In prior qualitative work, residents described feelings of guilt and anxiety associated with asking close friends and family members to visit them, especially if these people had “gotten out” and now lived in safer neighborhoods.12 Taken together, these findings corroborate narratives of social dehiscence,24,25 possibly resulting from pragmatic challenges related to interacting with and supporting network confidantes.
It is notable that loneliness increased in a graded fashion from indirect to direct exposure, with the highest loneliness reported among participants who screened positive for PTSD. In a survey of 2,025 older adult veterans, Philipp Kuwert and colleagues documented similarly strong and positive associations between PTSD and loneliness.28 These findings may support theoretical mechanisms that point to maladaptive cognitive processes (for example, automatic thoughts) as most salient for driving subjective experiences of loneliness,6 particularly when social contacts and opportunities are present. We also documented positive associations between indirect exposure and loneliness, which might support additional mechanisms that are not solely based on traumatic stress. For instance, someone who learns that a family member was robbed may not meet the criteria for PTSD but might have rational behavioral responses (such as avoiding activities after dark) that exacerbate loneliness. Our study might be among the first to demonstrate this type of graded association in a sample of community-dwelling adults who experienced chronic exposure to violence in many forms. Interestingly, the association did not differ significantly by age, but it did trend toward higher odds of loneliness among older adults relative to younger adults (see appendix exhibit 4).22 Given that 77 percent of the participants were ages fifty and older, our ability to detect significant differences between age groups might have been limited.
Importantly, loneliness was associated with adverse health behaviors and higher clinical risk for poor health outcomes, similar to prior studies.29–32 Lonely adults reported less frequent adherence to dietary guidelines and medication regimens, as well as more frequent binge alcohol consumption and tobacco use. Despite growing recognition that loneliness contributes to poor health at a similar or greater magnitude than traditional clinical risk factors do,9,33 clinical assessment for loneliness has not been integrated into routine care.32 Particularly for communities with high levels of chronic exposure to violence, short validated scales that measure loneliness, such as the three-item scale used in this study,18 could be implemented into routine work flows. Implementation may be especially timely, as screening for health-related social needs is becoming more common and standardized in the US and elsewhere.34,35
Notably, Medicare’s Accountable Health Communities is a health care delivery model that is currently being tested in thirty US health care organizations and addresses social needs by bridging the gap between clinical and community-based services.34 Under this model, program participants must implement comprehensive screening for health-related social needs, build enhanced linkages to social and community-based services, and support capacity building to meet demand for services.34 The model may provide a convenient vehicle for the routine assessment and management of loneliness. Clinical teams that deliver medical care in the model would develop a higher awareness of social support resources in the community, create systems to link patients to these resources, and build higher capacity for these resources if needs are unmet.
In the UK, the first governmental strategy implemented to combat loneliness in 2018 was to support “social prescribing,” whereby health care providers could directly prescribe social activities to their patients.36 This type of prescribing could be targeted toward populations at higher risk for violence or even used in direct victim service provision. Moreover, resources could be specifically tailored to address safety concerns. For instance, rather than prescribing an outdoor walking group, providers might prescribe an indoor fitness class. Ultimately, greater financial accountability to communities, such as reimbursement for population-based outcomes, might also encourage health care systems to participate in violence prevention and intervention efforts. Arguably, violence prevention is a critical first step in reducing the adverse health, social, and financial consequences of violence in high-risk communities.
In addition to health care solutions, our study might have implications for broader social and environmental policies. For middle-age and older adults living in neighborhoods with high rates of violence, clinical interventions could provide only a little support for the daily challenges of aging in this setting. The AARP Foundation recently published a framework for social isolation in older adults that cites unsafe or inaccessible communities as one of ten primary risk factors for social isolation.25 The AARP report recommends engaging urban planners to ensure the walkability of neighborhoods, safe transportation, and safe local events.25 Justin Heinze and colleagues studied the Clean and Green program, a community-based effort to green vacant lots in Flint, Michigan, and found that greening vacant lots was associated with a 40 percent reduction in neighborhood violent crime.37 Similar positive associations have been observed between green space and reductions in loneliness.38 Thus, strategies to address community violence might be synergistic with and integral to the effectiveness of broader policies that address loneliness in disadvantaged neighborhoods.
Conclusion
Exposure to community violence was associated with higher social isolation, and in particular with higher loneliness, in a sample of urban community-dwelling adults. Loneliness increased in a graded fashion by severity of violence exposure type, and it was also associated with adverse health behaviors. At a time when public health and policy leaders are calling for solutions to the “epidemic of loneliness,” identifying populations at higher risk for social isolation and loneliness due to community violence might help target interventions and ensure equity in the provision of social and medical support.
Supplementary Material
Exhibit 2:
Association between exposure to community violence and social isolation characteristics of 460 study participants in Chicago, 2018
| Group | Difference between groups | |||
|---|---|---|---|---|
| Characteristic | Unexposed (n = 172) | Exposed (n = 288) | Unadjusted | Adjusteda |
| Social network | ||||
| Network size (mean people)b | 2.16 | 2.42 | 0.26 | 0.22 |
| Spousal relationship tie (mean %) | 26.06 | 23.78 | −2.28 | −3.83 |
| Frequency of interactionc | 87.75 | 84.04 | −3.72** | −3.34** |
| Perceived closenessc | 91.89 | 89.19 | −2.71 | −3.42* |
| Living alone (mean %) | 32.94 | 33.45 | 0.51 | 0.77 |
| Social participationc | 43.13 | 43.79 | 0.65 | 2.01 |
| Perceived social support | ||||
| Support from familyc | 62.28 | 57.41 | −4.87* | −4.51 |
| Support from friendsc | 49.20 | 42.55 | −6.65** | −7.26*** |
| Lonelinessc | 14.07 | 22.85 | 8.78**** | 7.80**** |
SOURCE Authors’ analysis of participants with complete data.
Generalized linear models were used to estimate differences between groups that were or were not exposed to community violence, adjusting for age, sex, race/ethnicity, educational attainment, insurance type, and clinic location (academic medical center or federally qualified health center).
Number of unique confidantes mentioned in response to the question, “Looking back over the past year, who are the people that you most often discussed important things with?”
Mean score on a 100-point scale.
p < 0.10
p < 0.05
p < 0.01
p < 0.001
Acknowledgment
An earlier version of this article was presented at the Annual Meeting of the Society of General Internal Medicine, Washington, D.C., May 10, 2019, and received the Milton W. Hamolsky Award for the most outstanding scientific abstract oral presentation by a junior faculty member. The research reported in this article was supported by an Agency for Healthcare Research and Quality grant in patient-centered outcomes research (Grant No. 5K12HS023007 to Elizabeth Tung) and by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases’ Chicago Center for Diabetes Translation Research (Grant No. NIDDK P30DK092949 to Tung). Tung had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the US government or National Institutes of Health. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contributor Information
Elizabeth L. Tung, Section of General Internal Medicine and Center for Health and the Social Sciences; University of Chicago, Chicago, IL.
Kathleen A. Cagney, Department of Sociology and Population Research Center; University of Chicago, Chicago, IL.
Louise C. Hawkley, NORC at the University of Chicago, Chicago, IL.
Monica E. Peek, Section of General Internal Medicine; University of Chicago, Chicago, IL.
Notes
- 1.O’Connell PM, Gorner J, Crepeau M. Anti-violence protesters shut down Dan Ryan: “Today was the attention-getter, but now comes the action.” Chicago Tribune [serial on the Internet]. 2018. July 7 [cited 2019 Jul 23]. Available from: http://www.chicagotribune.com/news/breaking/ct-met-dan-ryan-pfleger-violence-protest-20180706-story.html
- 2.Sampson RJ. Great American city: Chicago and the enduring neighborhood effect. Chicago (IL): University of Chicago Press; 2012. p. 149–61. [Google Scholar]
- 3.Klinenberg E Is loneliness a health epidemic? New York Times; 2018. February 9. [Google Scholar]
- 4.Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ Jr. The epidemiology of social isolation: National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci. 2018. March 26 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci. 2009;64(Suppl 1):i38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson C, Moulton B. Loneliness among older adults: a national survey of adults 45+ [Internet]. Washington (DC): AARP; 2010. September [cited 2019 Jul 23]. Available from: https://www.aarp.org/content/dam/aarp/research/surveys_statistics/general/2012/loneliness-2010.doi.10.26419%252Fres.00064.001.pdf [Google Scholar]
- 8.Prime Minister’s Office [Internet]. London: Prime Minister’s Office; 2018 Press release, PM launches government’s first loneliness strategy; 2018. October 15 [updated 2018 Oct 16; cited 2019 Jul 23]. Available from: https://www.gov.uk/government/news/pm-launches-governments-first-loneliness-strategy [Google Scholar]
- 9.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviours in lonely and non-lonely populations. Psychol Health Med. 2006;11(2):233–45. [DOI] [PubMed] [Google Scholar]
- 11.Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71. [DOI] [PubMed] [Google Scholar]
- 12.Tung EL, Johnson TA, O’Neal Y, Steenes AM, Caraballo G, Peek ME. Experiences of community violence among adults with chronic conditions: qualitative findings from Chicago. J Gen Intern Med. 2018;33(11):1913–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen L, Davis R, Lee V, Valdovinos E. Addressing the intersection: preventing violence and promoting healthy eating and active living. Oakland (CA): Prevention Institute; 2010. May [cited 2019 Jul 23]. Available from: https://www.preventioninstitute.org/sites/default/files/publications/VNPA_Addressing%20the%20Intersection_051810.pdf [Google Scholar]
- 14.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–8. [DOI] [PubMed] [Google Scholar]
- 15.CMAP Data Hub. 2010 census data summarized to Chicago community areas [Internet]. Chicago (IL): Chicago Metropolitan Agency for Planning; 2015. June 26 [cited 2019 Jul 23]. Available from: https://datahub.cmap.illinois.gov/dataset/2010-census-data-summarized-to-chicago-community-areas [Google Scholar]
- 16.National Center for Posttraumatic Stress Disorder. Brief Trauma Questionnaire (BTQ) [Internet]. Washington (DC): Department of Veterans Affairs, National Center for PTSD; 1999. [cited 2019 Jul 23]. Available from: https://www.ptsd.va.gov/professional/assessment/documents/BTQ.pdf [Google Scholar]
- 17.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI (2003). The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics (PDF). Primary Care Psychiatry, 9, 9–14. doi: 10.1185/135525703125002360 PTSDpubs ID: 26676 [DOI] [Google Scholar]
- 18.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–50. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey questionnaire. Atlanta (GA): CDC; 2015. [Google Scholar]
- 21.Department of Health and Human Services. Washington (DC): Healthy People 2020; 2010. [Google Scholar]
- 22. To access the appendix, click on the Details tab of the article online.
- 23.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3–15. [DOI] [PubMed] [Google Scholar]
- 24.Klinenberg E Dying alone: the social production of urban isolation. Ethnography. 2001;2(4):501–31. [Google Scholar]
- 25.Elder K, Retrum J. Framework for isolation in adults over 50 [Internet]. Washington (DC): AARP Foundation; [last revised 2012 May 30; cited 2019 Jul 24]. Available from: https://www.aarp.org/content/dam/aarp/aarp_foundation/2012_PDFs/AARP-Foundation-Isolation-Framework-Report.pdf [Google Scholar]
- 26.American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys [Internet]. Oakbrook Terrace (IL): AAPOR; [last revised 2016; cited 2019 Jul 24]. Available from: https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf [Google Scholar]
- 27.Klinenberg E Heat wave: a social autopsy of disaster in Chicago. Chicago (IL): University of Chicago Press; 2002. [DOI] [PubMed] [Google Scholar]
- 28.Kuwert P, Knaevelsrud C, Pietrzak RH. Loneliness among older veterans in the United States: results from the National Health and Resilience in Veterans Study. Am J Geriatr Psychiatry. 2014;22(6):564–9. [DOI] [PubMed] [Google Scholar]
- 29.Brady SS. Lifetime community violence exposure and health risk behavior among young adults in college. J Adolesc Health. 2006;39(4):610–3. [DOI] [PubMed] [Google Scholar]
- 30.Murray J, Craigs CL, Hill KM, Honey S, House A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc Disord. 2012;12:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dyal SR, Valente TW. A systematic review of loneliness and smoking: small effects, big implications. Subst Use Misuse. 2015;50(13):1697–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perissinotto C, Holt-Lunstad J, Periyakoil VS, Covinsky K. A practical approach to assessing and mitigating loneliness and isolation in older adults. J Am Geriatr Soc. 2019;67(4):657–62. [DOI] [PubMed] [Google Scholar]
- 33.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8–11. [DOI] [PubMed] [Google Scholar]
- 35.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the Accountable Health Communities screening tool [Internet]. Washington (DC): National Academy of Medicine; 2017. May 30 [cited 2019 Jul 24]. Available from: https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf [Google Scholar]
- 36.National Health Service England. Social prescribing and community-based support: summary guide [Internet]. UK (Leeds): NHS; [cited 2019 Jul 24]. Available from: https://www.england.nhs.uk/wp-content/uploads/2019/01/social-prescribing-community-based-support-summary-guide.pdf [Google Scholar]
- 37.Heinze JE, Krusky-Morey A, Vagi KJ, Reischl TM, Franzen S, Pruett NK, et al. Busy streets theory: the effects of community-engaged greening on violence. Am J Community Psychol. 2018;62(1–2):101–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van den Berg MM, van Poppel M, van Kamp I, Ruijsbroek A, Triguero-Mas M, Gidlow C, et al. Do physical activity, social cohesion, and loneliness mediate the association between time spent visiting green space and mental health? Environ Behav. 2019;51(2):144–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.