Abstract
The study sought to describe the occurrence of adolescent driving after drinking (DD) and riding with a driver who had been drinking (RWDD) and associations with substance use for both males and females. As part of screening for a randomized controlled trial, we surveyed 16–20 year olds (N=3418) recruited from an emergency department (ED) and analyzed data from those reporting past-year alcohol consumption (n=2150, 58% females). DD was reported by 22% of females and 28% of males and RWDD was reported by 39% of females and 38% of males, also in the past year. In regression models, risky alcohol use and past-year marijuana use were associated with increased odds of DD and RWDD for females and males. Marijuana use was a strong predictor, with odds increased by 2.3 and 1.7 times for DD among females and males respectively and 1.4 times for RWDD for females and males. Prescription drug misuse was also associated with DD for females and for both males and females’ reported RWDD. The findings highlight the alarming rate of DD and RWDD among both males and females and suggest ED- based injury prevention efforts consider such risky road behavior as well as consider their substance use. Future research might also further examine the effects of driving under influence of substances, particularly marijuana, and the negative synergistic effects of co-ingestion prior to driving.
Keywords: alcohol-impaired driving, riding with a drinking driver, injury prevention, drink driving, drunk driving, emergency department, cannabis, substance use, prescription drug misuse
Introduction
Motor vehicle crashes (MVCs) are the leading cause of death for 15–24 year-olds (1). Recent data show 41% of mortality among 15–24 year-olds was due to unintentional injury. Further, 57% of those injuries were MVC-related, with males over-represented compared with females (2). A significant factor in MVCs is driving after drinking (DD) (3). DD is associated with riding with a driver who has been drinking (RWDD). Further, adolescents and emerging adults who DD are more likely to RWDD, with demographic differences evident in the occurrence of these risky road behaviors (4).
DD is especially significant among those under the legal drinking age. Youth are more likely than adults to have a MVC when DD (5) and young drinkers have a higher risk of death in alcohol-related crashes than older drivers (6). DD has been related to increased crash-related injury severity, even at low BAC levels (e.g., 0.01) (7). Impairment in driving is also elevated when alcohol is combined with other substances, including marijuana as well as other illicit drugs and drugs available by prescription that may be misused (e.g. benzodiazapines, opioids) (8, 9).Further, studies undertaken in driving simulators have shown concurrent alcohol and marijuana use produce additive rather than synergistic effects on poor driving (10), with other studies of driving performance showing greater impairment to driving after consumption of both alcohol and marijuana as well as alcohol and other substances, including those that can be obtained by prescription or that are illicit (11, 12). Thus among adult drivers at least, impairing effects of alcohol on driving can be compounded with marijuana or other drug use.
National data from adolescents recruited in schools indicate that substance use and DD or RWDD are associated in this population (13). Among those reporting DD (13%), there were 36% who reported past year drug use (marijuana, illicit drugs, and prescription drugs to get high) and among those who had ridden with driver who was impaired (24%), there were 44% reporting such drug use. In this study impaired did not differentiate between impairment from marijuana, illicit drugs, and prescription drug misuse. They also did not differentiate predictive factors separately for males and females. Using the same sample, general risky driving was however also shown to be more common among adolescents who also reported more substance use. Indeed, substance use and previous heavy drinking are persistent longitudinal predictors of impaired driving into young adulthood (14).
Prior research examining DD and RWDD among youth samples in the ED has focused on subgroups of youth, namely injured adolescents, adolescents who primarily are not of driving age, or on college student populations. Spirito et al. (15) reported lifetime DD and past year RWDD among injured 13–17 year-olds was higher among those who presented to the ED with a positive blood alcohol level (31% lifetime DD, 59% RWDD past year) as compared to those who were alcohol negative (9% DD, 40% RWDD). Additional characteristics of these youth, such as their other substance use, are rarely considered in relation to driving behavior and may provide critical information for intervention efforts particularly given the concerning impact of combining alcohol and substance use prior to driving. Few studies also examine such factors separately for males and females which may be relevant given the different rates of injury and different engagement in such risky driving (4). Adolescents and emerging adults seeking care for an acute injury or acute MVC-related injury may only be a fraction of those at risk for DD or RWDD who seek care annually in EDs. Understanding the background risks, including marijuana and other substance use, may inform future ED-based prevention efforts for those of driving age. This study sought to determine the occurrence and associated risk factors of DD and RWDD among driving-age male and female underage drinkers presenting to an ED.
Methods
Participants and Procedure
The protocol was approved by the institutional review board. Recruitment and screening took place at the University of Michigan, a large academic level-1 trauma center with an annual census of approximately 85,000 patients/ year. Patients were identified through electronic patient tracking logs and approached in waiting rooms or treatment spaces as part of screening for a randomized controlled trial (16,17). The current analyses however focus on screened patients of driving age (16–20 years). Patients were recruited 7 days a week except major holidays from September 2010 to March 2013. After obtaining written consent (including from a guardian if under 18, for which participant assent was also obtained), participants self-administered a 15- minute computerized screening questionnaire on a tablet computer in private. The survey was paused for medical intervention. Patients received a gift ($1 value) at completion.
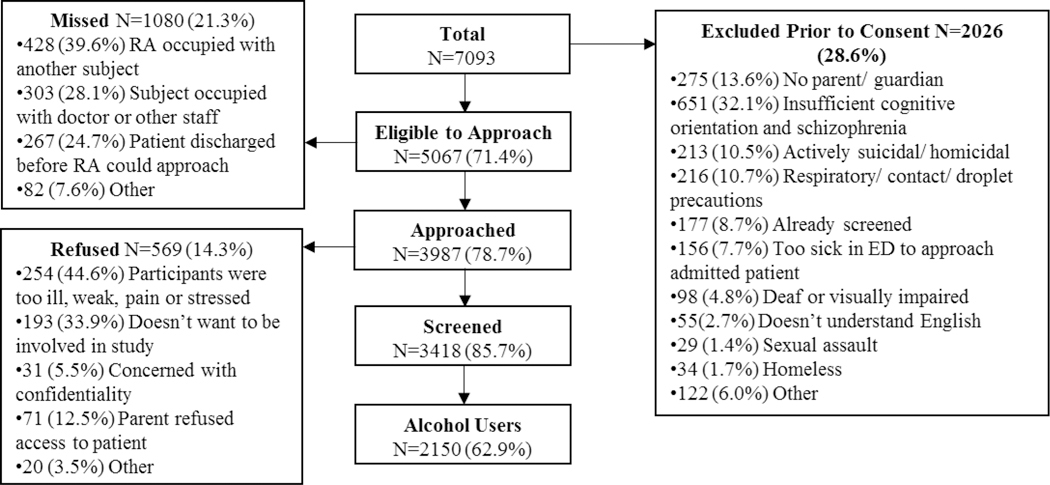
During recruitment, 7093 patients aged 16–20 years old presented to the ED for a medical or injury complaint; 5067 (71.4%) were eligible for screening with 3418 completing screening (Figure 1). There were 2150 patients (62.9%) who reported past-year alcohol use; 58.1% were female (n=1250), 74.6% (n=1603) were Caucasian, 81.3% (n=1747) enrolled in school, and their mean age was 18.7 years (SD = 1.2). The majority of the sample presented for a medical complaint rather than an injury-related chief complaint (32.0%, n=688).
Figure 1.
Flowchart of study participants
Measures
Driving After Drinking (DD).
The Young Adult Driving Questionnaire (18) assessed past-12 month DD (Chronbachs’ alpha = .90). Responses were dichotomized into whether or not participants had engaged in any of five behaviors (i.e., 1) driving within 1 hour of drinking 1–2 drinks and 2) 3 or more drinks, 3) driving when feeling high or light-headed, 4) driving when the participant knew drinking may have impaired his/her coordination, and 5) drinking in a car while driving).
Riding with a Driver who had been Drinking (RWDD).
A single-item based on the YRBS, 2009 (19) assessed RWDD in 12-months. Participants responses were dichotomized to, no engagement (0 = 0 times) or any engagement (1 = 1 time, 2 = 2 or 3 times, 3 = 4 or 5 times, 4 = 6 or more times).
Prior Experience with Injury.
Patients completed the Adolescent Injury Checklist (20) assessing whether or not (yes/no) they experienced any past year injury; 11-items (e.g., getting cut, a fight-related injury). Patients who responded affirmatively were categorized as having had a past-year injury.
Alcohol use.
We used a version of the 3-item Alcohol Use Disorders Identification Test- Consumption (AUDIT-C) that used modifications from Chung et al.’s (21) adolescent version. (Chronbach’s alpha = .80). Age (in years) of first alcohol consumption was measured with the question “About how old were you when you first started drinking, not counting small tastes or sips?” (22).
Substance use.
Participants completed the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) (23), reporting whether or not they had used each of the following substances in the previous 12 months: marijuana, cocaine, inhalants, hallucinogens, methamphetamines, and street opioids. Participants also reported if they misused each of the following prescription drugs: opioids, sedatives, or stimulants (defined as: taken to get high, taken someone else’s prescription, or taking more than prescribed). For analyses, we collapsed items to create three dichotomous variables of use/ no use of: (1) marijuana use, (2) prescription drug misuse, and (3) other illicit drug use.
Demographic Measures.
We assessed standard demographics, including sex, age, race, and school enrollment, using items from national surveys (24,25). Reason for the current ED visit (coded: medical or injury) was extracted from the patient’s ED chart.
Results
Risky Substance Use
There were 21.8% (n=523) of females and 27.7% (n=523) of males who reported past- year DD and 39.4% (n=830) of females and 37.6% (n=523) of males who reported past-year RWDD. More than half of males (62.2%, n=560) and half of females (52.6%, n=657) reported past-year marijuana use regardless of their reported DD or RWDD. There was less reports of prescription drug misuse (23.3% of males, 18.4% of females) and of other illicit drug use (17.9% of males, 10.5% of females) in the sample.
Multivariate Logistic Regression Analyses
The overall models including substance use, injury, and demographic variables were significant in predicting DD [Model χ2(11) =148.66, p<.001] and RWDD [Model χ2(1) =180.01, p<.001] for females (Table 1) and were significant for males, DD [Model χ2(11) =109.32, p<.001] and RWDD [Model χ2(11) =153.43, p<.001]. For both males and females, marijuana use and a higher AUDIT-C score were significantly associated with increased odds of both DD and RWDD using 95% confidence intervals. For females, prescription drug misuse was associated with both risky road use behaviors but was only associated with RWDD for males. Illicit drug use was only related to males’ DD.
Table 1.
Sample descriptives and odds ratios associated with DD and RWDD among males and females (N=2150)
| Driving after drinking | Riding with a driver who had been drinking | |||||||
|---|---|---|---|---|---|---|---|---|
| Males N=900; yes, n=250 | Females N=1250; yes, n=273 | Males N=900; yes, n=338 | Females N=1250; yes, n=492 | |||||
| OR (95% CI) | %, M (S.D.) | OR (95% CI) | %, M (S.D.) | OR (95% CI) | %, M (S.D.) | OR (95% CI) | %, M (S.D.) | |
| Age | 1.11 (.95–1.29) | 18.9 (1.1) | 1.00 (.88–1.14) | 18.6 (1.2) | 1.13 (.99–1.30) | 18.8 (1.2) | 1.00 (.89–1.12) | 18.6 (1.2) |
| Caucasian | .91 (.61–1.36) | 78.8% | .52 (.38–.73)*** | 67.8% | .69 (.49–.98)* | 74.0% | .53 (.40–.71)*** | 66.7% |
| Public Assistance | 1.07 (.69–1.67) | 20.0% | .86 (.61–1.13) | 31.5% | 1.49 (1.01–2.02)* | 23.4% | 1.76(1.31–2.37)*** | 37.6% |
| Enrolled in school | .58 (.38–.39)* | 70.8% | .80 (.54–1.18) | 75.8% | .66 (.45–.97)* | 71.9% | .88 (.62–1.23) | 76.4% |
| ED visit – injurya | .80 (.56–1.22) | 44.4% | .98 (.67–1.42) | 22.7% | .86 (.63–1.17) | 45.6% | .69 (.50-.96)* | 20.1% |
| Past injury experienceb | 1.32 (.92–1.89) | 69.2% | 1.22 (.88–1.67) | 53.9% | 1.71 (1.24–2.36)** | 69.8% | 1.73 (1.32–2.27)*** | 54.1% |
| Age of first drink | .91 (.83–.99)* | 15.3 (2.0) | .93 (.85–1.01) | 15.6 (1.9) | .91 (.83–.99)* | 15.5 (2.2) | .93 (.87–1.00) | 15.8 (2.0) |
| AUDIT-C score | 1.17 (1.10–1.25)*** | 6.0 (2.8) | 1.19 (1.12–1.27)*** | 4.7 (2.5) | 1.08 (1.02–1.15)** | 5.4 (2.9) | 1.11 (1.04–1.17)** | 4.1 (2.5) |
| Marijuana use | 1.69 (1.14–2.51)** | 80.0% | 2.33 (1.67–3.27)*** | 75.8% | 1.43 (1.02–2.00)* | 74.3% | 1.46 (1.11–1.91)** | 65.5% |
| Prescription drug misuse | 1.75 (1.16–2.62)** | 42.4% | 1.54 (1.06–2.24)* | 32.2% | 1.44 (.98–2.13) | 34.0% | 1.88 (1.33–2.65)*** | 28.9% |
| Illicit drug use | 1.79 (1.15–2.80)* | 36.0% | 1.11 (.71–1.75) | 20.9% | 1.47 (.95–2.27) | 28.1% | 1.54 (.98–2.42) | 17.9% |
| Model overview | AIC diff from null=131.4. χ2=122.7(11), p<.001 | AIC diff from null=126.7. χ2=126.8(11), p<.001 | AIC diff from null=87.3. χ2=93.4(11), p<.001 | AIC diff from null=158.0. χ2=148.9(11), p<.001 | ||||
Versus presenting for a medical complaint (non-injury)
Experience in past year. OR: adjusted odds ratio.
p< .05
p< .01
p< .001.
Note. Standardized predictors are as follows in each model (where possible for the variables): Model - Males DD; for Age, OR=1.27, for Age of first drink, OR=.83, for AUDIT-C score, OR=1.51, Model - Females DD; for Age, OR=1.00, for Age of first drink, OR=.86, for AUDIT-C score, OR=1.58; Model - Males RWDD; for Age, OR=1.16, for Age of first drink, OR=.83, for AUDIT-C score, OR=1.24; Model - Females DD; for Age, OR=1.01, for Age of first drink, OR=.88, for AUDIT-C score, OR=1.30.
With regard to injury and demographics, being of Caucasian background lowered females’ odds of reporting DD and RWDD, as did an injury-related ED visit in the RWDD model. Previous injury experiences however increased odds of RWDD for both males and females. For males, being enrolled in school and older age at first alcohol consumption lowered the odds of reporting DD and RWDD.
Discussion
These findings show the high occurrence of DD and RWDD among underage drinkers presenting to an ED setting. Among these driving-age underage drinkers, 22% of females and 28% of males endorsed DD and 39% of females and 38% of males endorsed RWDD. Results regarding the occurrence of DD and RWDD are consistent with prior work focused on those who had presented to the ED with an injury (15). A key contribution of this study however, is that it highlights an association between DD and/ or RWDD and marijuana use and may suggest that when considering driving after drinking or marijuana use that the other risk behavior also be considered. Findings further suggest that there are associations between engagement in risky road behavior and other drug use that is relevant to consider; illicit drug use relating to males’ DD and prescription drug misuse relating to males’ and female’ RWDD and females’ DD.
The study found that around eight-in-ten of the adolescents who reported DD and seven- in-ten of those reporting RWDD also reported past-year marijuana use, which was similar but slightly lower for females. This is concerning from a public health standpoint and particularly in transportation safety because it is unclear how many of these youth may also be driving when “high.” As legislation that eases access to marijuana and/or reduces marijuana penalties increases (e.g., medical marijuana, legalization for recreational use, decriminalization), it is critical to understand the role of marijuana use in risk for impaired driving among adolescents, and future studies should assess rates of, and risk factors for, drug-impaired driving in addition to alcohol- impaired driving among those of a younger driving age.
Further concern for drug use and driving is the association of adolescents’ prescription drug misuse and driving, with increased odds associated with male and females’ DD and females’ RWDD. Future research should also evaluate whether brief interventions are best combined, for example including alcohol, alcohol-involved driving, and addressing marijuana or other substance use to thus enhance the most effective and efficient way to improve safety. In this regard, a recent study, Project Reduce, found reductions in conjoint use days (alcohol and marijuana) following a brief intervention (26), although this study did not examine DD and RWDD specifically. Further, Cunningham et al. (27) showed a computer-delivered brief intervention reduced the frequency of DD at a 12-month follow-up. The current study adds to the literature in the finding that marijuana use is associated with DD and RWDD for both males and females with prescription drug misuse associated with both males’ and females’ DD and females’ RWDD. Given the risk for these youth driving while substance impaired, it provides urgency to including substance use and driving behavioral messages to youth receiving brief interventions.
An additional feature of the current study is the examination of models separately for males and females and the distinction of road-related risks (DD and RWDD), with notable differences across the models. Identifying as Caucasian was associated with lower odds for males and females’ RWDD and females’ DD. Further, only the model of males’ DD included illicit drug use as a significant associated factor. There was a significant association for receipt of public assistance with RWDD, but it was not significant in the models for DD. Being enrolled in school and older age of first alcohol consumption was associated with reduced odds for males’ DD and RWDD, but not for females. The nature of the ED visit was only a significant predictor in the model of RWDD for females and previous reports of injury only a significant predictor in the RWDD models, despite injury often being a criteria for intervention studies (15). Overall the findings suggest further understanding, and considering, marijuana use with brief assessment, given the high rates of use among those reporting DD and RWDD; however, a more complex assessment should consider different factors for males’ and females’ risky road behavior.
There are however study limitations, due to the cross-sectional analysis, causal attributions cannot be made. The study was conducted at a single academic medical center, limiting generalizability. In addition, DD and RWDD behaviors may vary in urban, suburban, or rural regions that have different availability of public transportation (28). The absence of driving history or license status is also a potential limitation although our sample consisted of patients of driving age and such behavior has injury-risk regardless of license status. The use of self-report surveys is a further potential limitation, but has previously been shown to have high reliability and validity among adolescents who are more likely to report sensitive information on a computer where privacy and confidentiality are assured (29) and we have used standardized measures where possible. The independent variable was dichotomized and thus does not differentiate any associations relative to the degree of risk for individuals, for example, relative to the regularity in which they engage in road risks or their degree of intoxication. However any DD, including driving after one or two drinks can increase crash risk particularly for adolescents (5).
The high occurrence of DD (24%) and RWDD (39%) among male and female underage drinkers is of high relevance to those in transportation safety and suggests that interventions are warranted. Moreover, marijuana use is alarmingly high among alcohol-consuming adolescents and emerging adults who report DD and RWDD. Future studies should assess how often these youth are driving high, with and without being under the influence of alcohol.
Highlights:
Underage drinkers past year driving after drinking (DD) rates are high for males (28%) and females (22%)
Riding with those who drive after drinking (RWDD) rates also are high (39%)
Marijuana use is a clear concern; associated with both behaviors
Acknowledgments
Funding: This study was funded by NIAAA [#5R01AA018122].
Role of funding sources: Funding for this study was provided by NIAAA Grant #5R01AA018122. NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: All authors declare that they have no conflicts of interest.
References
- [1].Centers for Disease Control & Prevention. Vital signs: Unintentional injury deaths among persons aged 0–19 years - United States, 2000–2009. MMWR 2012;61:270. [PubMed] [Google Scholar]
- [2].Centers for Disease Control & Prevention. WISQARs leading causes of death reports, national and regional,1999–2014. Available at: http://webappa.cdc.gov/sasweb/ncipc/leadcaus10_us.html. [Google Scholar]
- [3].SAMSHA. Results from the 2013 national survey on drug use and health: Summary of national findings, NSDUH series H-48, HHS publication No. (SMA) 14–4863. Rockville, MD: US Department of Health and Human Services; 2014. [Google Scholar]
- [4].Kann L, McManus T, Harris WA et al. Youth risk behavior surveillance – United States, 2015. MMWR 2016; 65(No.SS-6):1–180. [DOI] [PubMed] [Google Scholar]
- [5].Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. Journal of Studies on Alcohol 2000;61:387–395. [DOI] [PubMed] [Google Scholar]
- [6].Phillips DP, Brewer KM. The relationship between serious injury and blood alcohol concentration (BAC) in fatal motor vehicle accidents: BAC= 0.01% is associated with significantly more dangerous accidents than bac= 0.00%. Addiction 2011;106:1614–1622. [DOI] [PubMed] [Google Scholar]
- [7].Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: Systematic review of observational studies and meta-analysis. BMJ 2012;344:e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Dassanayake T, Michie P, Carter G et al. Effects of benzodiazepines, antidepressants and Opioids on driving. A systematic review and meta-analysis of epidemiological and experimental evidence. Drug Safety 2011;34(2):125–156. [DOI] [PubMed] [Google Scholar]
- [9].Dubois S, Mullen N, Weaver B, et al. The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forensic science international 2015;248:94–100. [DOI] [PubMed] [Google Scholar]
- [10].Hartman RL, Brown TL, Milavetz G, et al. Cannabis effects on driving lateral control with and without alcohol. Drug and Alcohol Dependence 2015;154:25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kelly E, Darke S, Ross J A review of drug use and driving: Epidemiology, impairment, risk factors and risk perceptions. Drug and Alcohol Review 2004;23(3):319–344. [DOI] [PubMed] [Google Scholar]
- [12].Ramaekers JG, Robbe H, O’Hanlon J. Marijuana, alcohol and actual driving performance. Human Psychopharmacology Clinical and Experimental 2000;15:551–558. [DOI] [PubMed] [Google Scholar]
- [13].Li KG, Simons-Morton BG, Vaca FE, et al. Association between riding with an impaired driver and driving while impaired. Pediatrics 2014;133:620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Vaca FE, Li K, Hingson R, et al. Transitions in riding with an alcohol/drug-impaired driver from adolescence to emerging adulthood in the United States. Journal of Studies on Alcohol and Drugs 2016;77:77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Spirito A, Barnett NP, Lewander W, et al. Risks associated with alcohol-positive status among adolescents in the emergency department: A matched case-control study. Journal of Pediatrics 2001;139:694–699. [DOI] [PubMed] [Google Scholar]
- [16].Cunningham RM, Chermack ST, Ehrlich PF et al. Alcohol interventions among underage drinkers in the ED: A randomized controlled trial. Pediatrics 2015;136(4):e783–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Walton MA, Chermack ST, Blow FC et al. Components of brief interventions for youth in the emergency department. Substance Abuse 2015; 36(3):339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Donovan JE. Young adult drinking-driving: Behavioral and psychosocial correlates. Journal of Studies on Alcohol 1993;54:600–613. [DOI] [PubMed] [Google Scholar]
- [19].Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance-United States, 2009. MMWR 2010;59:1–142. [PubMed] [Google Scholar]
- [20].Jelalian E, Spirito A, Rasile D, et al. Risk taking, reported injury, and perception of future injury among adolesecents. Journal of Pediatric Psychology 1997;22:513–531. [DOI] [PubMed] [Google Scholar]
- [21].Chung T, Colby SM, Barnett NP, et al. Screening adolescents for problem drinking: Performance of brief screens against DSM-IV alcohol diagnoses. Journal of Studies on Alcohol 2000;61:579–587. [DOI] [PubMed] [Google Scholar]
- [22].Hingson RW, Heeren T, Edwards EM. Age at drinking onset, alcohol dependence, and their relation to drug use and dependence, driving under the influence of drugs, and motor-vehicle crash involvement because of drugs. Journal of Studies on Alcohol and Drugs 2008;69:192–201. [DOI] [PubMed] [Google Scholar]
- [23].Humeniuk R, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction 2008;103:1039–1047. [DOI] [PubMed] [Google Scholar]
- [24].NIDA. Drug abuse treatment outcome study—adolescent (datos-a), 1993–1995: [United States]. ICPSR03404-v3. Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2008. [Google Scholar]
- [25].Bearman PS, Jones J, Udry JR. The national longitudinal study of adolescent health: Research design. Available at http://www_cpc_unc_edu/projects/addhealth/design. [Google Scholar]
- [26].Woolard R, Baird J, Longabaugh R, et al. Project Reduce: Reducing alcohol and marijuana misuse: Effects of a brief intervention in the emergency department. Addictive behaviors 2013;38:1732–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Cunningham RM, Chermack ST, Ehrlich PF, et al. Alcohol interventions among underage drinkers in the ed: A randomized controlled trial. Pediatrics 2015;136:e783–e793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Leadbeater BJ, Foran K, Grove‐ White A. How much can you drink before driving? The influence of riding with impaired adults and peers on the driving behaviors of urban and rural youth. Addiction 2008;103:629–637. [DOI] [PubMed] [Google Scholar]
- [29].Turner CF, Ku L, Rogers SM, et al. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science 1998;280:867–873. [DOI] [PubMed] [Google Scholar]