Abstract
Despite the substantial growth of telemedicine and the evidence of its advantages, the use of telemedicine in neurosurgery has been limited. Barriers have included medicolegal issues surrounding provider reimbursement, interstate licensure, and malpractice liability as well as technological challenges. Recently, the coronavirus disease 2019 (COVID-19) pandemic has limited typical evaluation of patients with neurologic issues and resulted in a surge in demand for virtual medical visits. Meanwhile, federal and state governments took action to facilitate the rapid implementation of telehealth programs, placing a temporary lift on medicolegal barriers that had previously limited its expansion. This created a unique opportunity for widespread telehealth use to meet the surge in demand for remote medical care. After initial hurdles and challenges, our experience with telemedicine in neurosurgery at Penn Medicine has been overall positive from both the provider and the patients' perspective. One of the unique challenges we face is guiding patients to appropriately set up devices in a way that enables an effective neuroexamination. However, we argue that an accurate and comprehensive neurologic examination can be conducted through a telemedicine platform, despite minor weaknesses inherent to absence of physical presence. In addition, certain neurosurgical visits such as postoperative checks, vascular pathology, and brain tumors inherently lend themselves to easier evaluation through telehealth visits. In the era of COVID-19 and beyond, telemedicine remains a promising and effective approach to continue neurologic patient care.
Key words: Clinic, COVID-19, Neurologic examination, Telehealth, Telemedicine
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; CRST, Clinical Rating Scale for Tremor; HIPPA, Health Insurance Portability and Accountability Act; IMLC, Interstate Medical Licensure Compact; MS, Multiple sclerosis; PD, Parkinson disease
Introduction
Telemedicine is the use of electronic, digital, Internet-based, or telephone-based communication for direct patient care. The earliest published use of telemedicine can be traced to the 1970s.1 , 2 With the increasing availability and speed of wireless Internet, there has been a growth in the past 20 years in the incorporation of telemedicine in patient care.2 , 3 For example, there have been studies on the benefits of telemedicine in preventative care and management of osteoarthritis, cardiac rehabilitation, and diabetes care.4 Specific examples of telemedicine in neurosurgery include the adoption of telemedicine models by the Veterans Health Administration neurology clinics and pediatric neurosurgery clinics in the state of Georgia.5 , 6 Despite the growing interest in telemedicine, its use by health care systems has been scarce because of an unclear or unidentifiable need as well as logistical issues, including physician reimbursement, interstate licensure, lack of universal access to technology, patient confidentiality, and liability issues.3
Since the insurgence of the coronavirus disease 2019 (COVID-19) pandemic, there has been an urgent need to build telemedicine programs that are safe and reliable in a relatively short time frame. We outline a guide to implement telehealth in neurosurgery and to conduct a neurologic examination via video platforms. This guide will not only present the benefits and limitations of telemedicine in neurosurgery in the era of COVID-19 and social distancing policies but will also encourage its routine use in future practice.
Historically, the main advantages of telemedicine to improve patient care are as follows: 1) the increased availability of health care to underserved populations, particularly for specialty care such as neurosurgery; 2) streamlining preparation to receive and triage patients at the hospital; and 3) the decrease of patient expenditures, travel time, and work lost due to hospital visits.2 , 3 , 7
-
1.
Subspecialty care has an unbalanced geographic distribution, which affects access to care.8 In the era of COVID-19, travel is cautioned due to the risk of viral spread or exposure. Telemedicine can eliminate geographic barriers while adhering to COVID-19 safety guidelines as physicians can reach patients remotely.
-
2.
Physicians use online examinations of patients in triaging care. For instance, a patient with a medical emergency would be sent to the hospital, whereas a patient with benign radiculopathy may be scheduled for a clinic appointment. Triage of patients before arrival at hospitals is vital in current COVID-19 conditions. The success of telemedicine in triaging patients with stroke holds promise for the application of telemedicine to other acute neurological emergencies.9 , 10
-
3.
Telemedicine can save patients money, travel time, and work lost, as reported by the Veterans Health Administration in a survey of patients who received chronic neurologic care, as well as by parents of pediatric patients receiving neurosurgical care.5 , 6 Davis et al.5 estimated a total saving of more than $48,000 in time and travel costs for 354 patients. Patient satisfaction was increased, with 95% of patients reporting that they would like to continue their neurologic care through telemedicine.
Neurosurgeons working at large hospitals or health systems can easily adopt telemedicine because of the economic capacity of larger institutions, in addition to their capacity to share telemedicine systems across the institution.3 Telemedicine will not replace in-person procedural or emergency services in neurosurgery.7 However, it can serve as a vital adjunct to conserve and distribute resources, ultimately improving neurosurgical patient care.
Pre-COVID-19 Telehealth Implementation and Medicolegal Considerations
Before the COVID-19 health crisis, the use of telehealth varied across medical and surgical specialties. In 2012, George et al.11 surveyed neurology departments in the top 50 hospitals as measured by U.S. News and World Report and found more than 85% either used or planned on implementing telemedicine within the following year. Although this may suggest widespread use of telehealth among providers, by 2016 only 15.4% of physicians worked in practices that had incorporated telemedicine for patient interactions. Major barriers responsible for the limited implementation of telehealth services thus far have included medicolegal issues surrounding provider reimbursement, licensure, and malpractice liability. Eligibility for and the amount of reimbursement varies by state and payer.
Under the requirements of the Centers for Medicare & Medicaid Services, Medicare can only reimburse for telehealth when the beneficiary resides in a designated rural area and travels to a local medical facility for the service.12 With few exceptions, Medicare did not reimburse for other telemedicine modalities such as store-and-forward services or remote patient monitoring. Although universal reimbursement through Medicare does not currently exist, coverage with regard to types of services and geographic area has been expanded in the past decade.13 Private payer reimbursement levels for telehealth services depend on state laws. Only 36 states and the District of Columbia have passed laws covering private insurers and telehealth reimbursement. And while some of these states have full parity for in-person versus telehealth services, other states do not address parity, allowing reimbursement levels to differ significantly.3 , 14 Restrictions and variability in payer reimbursement may have disincentivized the widespread adoption of telehealth programs.
The distribution of neurosurgeons across the United States is widely variable and the availability of emergency neurosurgical care is limited.15 Although telemedicine clinics have the potential to improve access in underserved regions,6 , 16 state medical licensing remains a barrier to its expansion. Most states require a provider to be licensed in the state in which the patient resides. A small number of states have issued special licenses to out-of-state providers practicing telehealth, whereas other states have made exceptions for providers from geographically contiguous states.14 In an effort to address the issue of licensure reciprocity, the Interstate Medical Licensure Compact (IMLC) was introduced. In 29 states, the District of Columbia, and the Territory of Guam where IMLC legislation has been passed, qualified out-of-state providers can undergo an expedited licensure process. However, many states have yet to implement IMLC legislation.17
Liability coverage varies across malpractice insurance carriers. Although telemedicine provider liability is similar to that of in-person medical services, malpractice insurance may only cover claims originating from specific jurisdictions.3 , 14
Government Response During the COVID-19 Pandemic
The COVID-19 crisis has resulted in a surge in telehealth due to increased demand for virtual medical visits as well as a temporary lift on medicolegal barriers that had limited telehealth's expansion in the past. The pandemic has threatened to strain medical resources, prompting governing bodies and professional societies to recommend elective surgeries be cancelled or postponed.18 This created a unique opportunity for widespread telehealth use to meet the surge in demand for remote medical care.
In response to the crisis, federal and state governments took action to facilitate the rapid implementation of telehealth programs across the country's health systems. Retroactive to March 1, 2020, and for the duration of the public health emergency, provisions temporarily removed the requirement that Medicare telehealth reimbursements be limited to beneficiaries seeking care at designated health centers in rural areas, thereby extending telehealth coverage to all.19 This waiver affects reimbursement for federal health care programs, including Medicare, Medicaid, and the Children's Health Insurance Program. These visits are considered the same and reimbursed at the same rate as all in-person visits. In addition, Medicare also expanded the list of eligible services provided via telehealth, including audio-only telephone calls and emergency department visits. Physicians may use telehealth for both new and established patients.20 Expanded Current Procedural Terminology codes applicable to telehealth have been summarized to guide providers.21 , 22 As some private payers are following the Centers for Medicare & Medicaid Services guidance, providers are encouraged to check with specific payers as well as state laws and regulations regarding eligible coverage.23 In an effort to limit licensure restrictions, 44 states have implemented waivers modifying in-state licensure requirements for telehealth services.24 Telehealth providers have also been temporarily allowed to issue prescriptions for controlled substances without in-person evaluations, provided certain requirements are met.25 These factors have all likely contributed to an increase in the proportion of neurosurgeons who have begun to use telehealth during the COVID pandemic.
Considerations in the Implementation of Telehealth
Maintaining patient privacy is a ubiquitous concern with electronic data transfer. Before the COVID-19 pandemic, telemedicine was provided only on Health Insurance Portability and Accountability Act (HIPAA)-compliant platforms, such as Zoom for Healthcare, BlueJeans, Doxy.me, and Vidyo.26 Video communication vendors with the necessary security capabilities to prevent data interception ensured electronic patient health information protection, as stipulated by the HIPAA business associate agreement. Nonpublic-facing communication products employ end-to-end encryption of information. Examples include FaceTime, Facebook Messenger video chat, Google Hangouts, as well as texting applications such as Whatsapp and iMessage. In contrast, public-facing communication applications (e.g., Facebook Live, TikTok or Twitch) are unacceptable platforms for the provision of telehealth. Although providers are still encouraged to use HIPAA-compliant vendors, they will not be penalized for using previously unsanctioned products during the COVID-19 emergency.27
The most imperative element of a remote clinical evaluation is arguably the technology used to transmit information. The most readily available technology are smartphones, owned by 77% of Americans in 2020.28 Furthermore, ongoing developments in videoconferencing software promise fewer technical issues, decreased latency, and higher video quality.29
Even before the COVID-19 pandemic, telemedicine had been successfully implemented for neurosurgical care in select settings. Video and image from smartphones are largely of sufficient quality, mitigating some concerns about decreased exam quality.30, 31, 32, 33 Although outcome data are limited, one study showed no significant difference in emergency department visits and 90-day readmission between patients who had undergone elective neurosurgery and received either in-person or remote follow-up.34 Notably, another study found that any potential reduction in efficacy may be offset by the cost-effectiveness and utilitarian benefits of telemedicine.35
The cognitive demand imposed on users by different video conference platforms may be a key consideration in selecting the appropriate platform. Agnisarman et al.36 compared the usability of 4 platforms—Doxy.me, Vidyo, VSee, and Polycom—with a sample clinical scenario that included a log-in sequence, changing to full screen, muting the microphone, disabling video, communicating over chat, and concluding the session.36 Although there were no significant differences in errors, the authors found significant differences in task completion time, workload, cognitive demand and effort, level of frustration, overall satisfaction, and user interface quality across platforms.36 The primary factor for whether a patient will accept a telemedicine invite is their comfort in initiating the call,37 which argues for choosing a platform with more widespread daily use over platforms specifically designed for telemedicine. Furthermore, with the increasing use of telemedicine, vendors are incentivized to achieve HIPAA compliance. Skype for Business, Zoom, and GoToMeeting are examples of popular video conferencing software with HIPAA-compliant options.
Preceding the COVID-19 pandemic, the telehealth market share was dominated by Teladoc Health, Amwell, and Doctor On Demand. The 2 main types of telemedicine vendors are those with integrated electronic medical records and ones that provide standalone telemedicine service. Stand-alone telemedicine platforms have the flexibility to be employed in conjunction with any electronic medical record. Companies like Zoom, Amwell, and Vidyo have partnered with EPIC to allow direct integration. The ease of use and integration of these traditional video conference platforms, relaxed HIPAA regulations, and the surge in telehealth use have all contributed to their rapid adoption in the telehealth space.38
Smaller centers without the capability for video platforms have implanted telephone-only visits. Although this type of encounter has inherent difficulty and limited examination, it can be effective for certain visits, such as long-term follow-up and evaluation of some incidental radiographic findings.
Institutional Experience
Penn Medicine recently adopted BlueJeans as its telemedicine platform in conjunction with the university-wide licensing of the software for the purpose of all remote communication. Since its implementation, BlueJeans has had overall positive feedback from both providers and patients. Before the scheduled clinic visit, the patient is contacted by a clinic staff member to assist in setting up the BlueJeans call, ensuring any technological issues are addressed, and that all radiologic data have been received and uploaded. On the day of the clinic visit, the patient first enters the virtual “room” with the medical assistant, similarly to a conventional clinic. After the basic patient information is gathered, the provider will “enter” the virtual clinic room. Patient history and physical examinations are completed, and radiology findings are shown to the patient via the screen share function. Additional need for follow-up or intervention is discussed with the patient, and after all the patient's questions are answered, the visit is completed.
Although the satisfaction with the implementation of telemedicine has been overall quite positive, some difficulties have been encountered, including initial set-up for first-time telemedicine users and difficulty navigating the telehealth platform, acclimation to the new clinic workflow, and patients without access to videoconferencing capabilities. For some patients, videoconferencing is done over a smartphone or tablet rather than a computer. We have found that while it is possible to effectively complete a visit this way, the physical examination is more difficult, particularly in regards to cranial nerve testing, and video conferencing with a computer is preferable. If a patient is sitting next to a bright window, the dynamic range of the small sensor camera can present a problem, particularly when examining the eyes, sclera, and face. It is best to have a patient sitting with the light source in front, rather than behind, of them. In addition, it is important that the camera is not too zoomed into the patient's face, limiting the extremity examination, or too wide angle, limiting the cranial nerve examination. For patients without a smartphone or computer camera, an audio-only visit significantly limits the ability for examination.
Certain neurosurgical visits and pathology inherently lend themselves to easier assessment through telehealth visits, such as postoperative checks, vascular pathology, and brain tumors. Other pathologies that have more subtle examination findings, such as peripheral nerve and certain spinal pathologies, and therefore are more difficult to assess via telemedicine.
Efficacy of the Telemedicine Neurologic Examination
Some argue that the most obvious weakness of telemedicine is the inability for providers to perform a face-to-face physical examination. However, as detailed previously, physicians can perform an accurate and comprehensive neurologic examination even through a telemedicine platform (Table 1 ).24 , 39, 40, 41, 42, 43, 44, 45 Currently, perhaps the most common telemedicine service is the field of acute stroke management, a field that demands rapid neurologic evaluation and treatment of patients within the window for intervention.45 Through tele-neurology and tele-stroke, the reliability of remotely administered neurologic assessments, particularly the National Institutes of Health Stroke Scale, has been well established across the full range of stroke severity.46, 47, 48, 49, 50 Furthermore, tele-stroke care has been proven to shorten duration of hospital stay, as well as to facilitate rapid access to rehabilitation assessments and other diagnostic testing and imaging, when compared to standard stroke unit care.46
Table 1.
| General Appearance | Inspection via Video |
| Vital signs∗ | Possible if patient has home equipment for measurement of blood pressure, pulse, and weight |
| Mental status | Video observation
|
| Speech | Evaluate fluency, comprehension (midline and cross-midline commands), naming, repetition, reading, and writing
|
| Cranial nerves | Visual fields∗: may be possible if patient has large screen or with assistance of another individual |
Extraocular movements: use video zoom function
| |
Fundoscopic examination∗: possible with smartphone app, FDA-approved applications include iExaminer, PaxosScope (DigiSight)
| |
| Visual acuity: assess ability to read newsprint with either eye | |
Face: examine visually for symmetric movements, facial weakness
| |
| Hearing: evaluate grossly if intact to voice, can have patient or tele-examiner test bilateral hearing by rubbing fingertips together near ears | |
| Palate: inspect for symmetric palate elevation, may be helpful to use video zoom function | |
| Shoulders: assess for symmetric shoulder shrug | |
| Tongue: Look for midline protrusion. Note asymmetry, deviation, hemiatrophy | |
| Motor examination | Muscle bulk: assess visually via video |
Strength∗: hard to get full strength peripheral neuromuscular examination without tele-examiner present
| |
| Tone∗: difficult to examine | |
| Abnormal movements∗: may be able to assess for bradykinesia, chorea etc. via video | |
| Sensory examination∗ | Need help of a family member or tele-examiner
|
| Cerebellar examination | May need help of family member or tele-examiner
|
Coordination:
| |
| Reflexes∗ | Difficult to assess without skilled examiner present
|
| Limitations of the telemedicine neurologic examination | |
|---|---|
| Comprehensive eye examination |
|
| Neuromuscular examination |
|
| Vestibular examination |
|
| Cerebellar examination |
|
FDA, Food and Drug Administration.
Elements of the examination that may be more difficult to perform.
There have been pilot trials for chronic neurologic care delivery for patients with Parkinson disease (PD), multiple sclerosis (MS), and essential tremor. PD is the most common indication for deep brain stimulation.51 Remote examinations are particularly valuable in patients with PD, as the age and level of disability in this patient population poses difficulties in traveling from their residence to clinic appointments. The current standard for evaluating PD is the Unified Parkinson Disease Rating Scale,42 , 43 consisting of 4 subscales: 1) mentation, behavior and mood; 2) activities of daily living; 3) motor examination, typically assessed by clinicians; and 4) complications of therapy. Among these, subscale 3 is the most pertinent part for tracking disease severity over time.52 Several studies have concluded that subscales 1 and 2 can be effectively self-administered by patients or caregivers, producing consistent results to provider-administered ratings.53, 54, 55 Furthermore, the possibility of remote administration of a modified version of subscale 3 (without rigidity and retropulsion pull testing) has been proposed and found to be reliable.44 One small randomized controlled trial comparing remote versus face-to-face neurologic examinations in patients with PD indicated comparable assessments of speech, facial expression, postural stability, gait, balance (arising from a chair), resting tremor, and hand and body bradykinesia; and a fair degree of inter-rater reliability for finger taps and action tremor. Further, patients in the same study that followed up via telemedicine reported improved quality of life and enhanced motor performance compared to patients receiving usual care.46
Similarly encouraging results have been reported in MS. In a comparison of remote and hands-on neurologic examinations of 20 patients with MS, Kane et al.56 found no significant increase in interspecialist disagreement in ratings of neurologic function when the neurologic exam was observed remotely. Lastly, for patients with spinal cord injuries, tele-neurology visits were shown to be as effective as in-person rehabilitation and to offer significant additional benefits in quality of life and long-term health outcomes.57
Remote neurologic examinations are also vital in the evaluation and clinical management of essential tremor, the most common movement disorder.58 For the evaluation of essential tremor, the Fahn-Tolosa-Marin Clinical Rating Scale for Tremor (CRST) is recommended by the Movement Disorders Society and has been adopted as the gold standard in most clinical research trials in this domain.39 The CRST scale consists of 3 parts: Part A quantifies tremor severity at rest, with posture holding, and with action for 9 parts of the body; Part B assesses action tremor of the upper extremities during writing, drawing, and pouring; and Part C assesses functional disability.40 Notably, in a recent trial published in the New England Journal of Medicine, the most pertinent portions of the CRST (extracted from parts A and C) were effectively assessed by movement disorder neurologists using videos of patients, suggesting the potential for using telemedicine on components of this scale.41
Certainly, some aspects of the neurologic examination may be more difficult to assess remotely than others, notably, deep tendon reflexes,57 rigidity,46 , 59 retropulsion pull testing,45 minor reductions in facial animation, subtle dyskinesia, and limb bradykinesia.60 Other studies noted mildly weaker inter-rater agreement when examining cerebellar, brainstem, and sensory functions.56 , 59 However, performing an accurate and comprehensive neurologic exam remotely is certainly feasible.
Although the remote neurologic examination may have minor weaknesses, amidst the current global COVID-19 pandemic and health care crisis, a remote examination is likely to provide access to care for patients who otherwise would be unable to be examined or seen for follow-up at all. These remote visits can be incredibly efficacious, especially if aided by a trained individual (tele-examiner) or family member on the patient's end, or if being used for follow-up after an initial face-to-face neurologic exam. Telemedicine has proven to be a clinically acceptable and cost-effective approach that not only improves patients' quality of life but also increases efficiency and conserves health care resources.5 , 60 In the era of COVID-19, a time in which social distancing and limited patient contact are imperative, telemedicine is a promising and effective approach to continue neurologic care.
Blueprint for the Post-COVID-19 Era: Telehealth Is Here to Stay
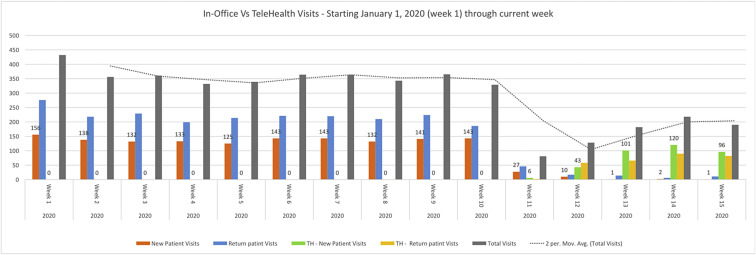
Our institutional experience has demonstrated the feasibility and acceptability of incorporating telehealth into neurosurgical ambulatory practices, even after social distancing restrictions are lifted. As with all new programs, an initial period of refinement was needed prior to arriving at our current workflow, but so far it has proven effective and efficient. During the 10 weeks before the COVID-19 pandemic, our department averaged 139 new patient and 220 return patient visits per week (Figure 1 ). No recorded telemedicine visits were conducted during that time period. Although there was an initial decline in the number of visits immediately after implementation of COVID-19–related policies, during our fifth week using our telemedicine workflow, our department recorded 111 new patient visits, 110 of which were conducted via telemedicine. Return patient visits followed a similar trend, with a sharp drop off and gradual recovery, although the number of return patient visits has not rebounded as robustly as new patient visits with 109 total return visits (95 telemedicine, 14 in-person) recorded during the fifth week following our policy change.
Figure 1.
In-office visits versus telehealth visits at Penn Medicine.
Although the neurologic examination is a useful adjunct, much of the decision-making in neurosurgery hinges on the clinical history and the review of relevant imaging findings, particularly in cranial surgery, which is entirely available via telehealth. In our practice, this has opened up the possibility of high-throughput screening of patients based on pathology, urgency, and need for intervention. For instance, our multidisciplinary Spine Access Center already involves the collaboration of neurosurgeons, orthopedists, physiatrists, and anesthesia pain specialists. Through telehealth, patients can be appropriately screened based on their symptomatology, along with past medical and surgical history, and identified as potential candidates for surgical intervention or more conservative measures, including a trial of physical therapy and/or epidural steroid injections. The physicians can order more focused radiographic or neurophysiological studies in preparation for a subsequent telemedicine or in-office visit. In an elective practice, such an approach can reduce lag time for patient evaluation, improved patient satisfaction, lower cost at the system and individual levels, more efficient use of in-person specialist time, and higher conversion of ambulatory visits to surgical cases. The approach is arguably more resource efficient in that we are using fewer examination rooms and decompressing the waiting room.
Similarly, telehealth clinics in neurosurgery offer a unique opportunity to augment the educational experience for residents and other trainees. Due to service obligations and limited training time, the primary emphasis of surgical subspecialty training across the country is hands-on experience in the operating room. However, one of the difficulties in transitioning to an independent practice after residency training is learning how to manage a clinic independently. Telehealth offers significant flexibility in incorporating this kind of learning into the current training paradigm, so that learners can gain much greater exposure to a variety of teaching and communication styles, including how to handle shared decision-making and informed consent for a wide range of pathologies. Similarly, residents also can gain access to aspects of patient follow-up that may not have been feasible without the widespread adoption of telehealth, including observing patient outcomes in the rehabilitation setting or following patients for whom they helped care for, either in the operating room or in the inpatient setting.
Potential Shortcomings of Telemedicine
As with all new technologies, it is important to consider how barriers to health care access may affect the growing use of telehealth. Health care systems must be vigilant to ensure that the implementation of telehealth does not inadvertently limit access to neurosurgical care along socioeconomic or cultural lines. This may require more up-front investment and regulation at the institutional and policy levels to ensure equal access to care.
Some patients will not participate in telemedicine visits because of they do not have access to the infrastructure required. For example, Internet access may not be fully robust in certain geographic locations or patients may not have a compatible camera. Also, we have identified a small group of patients who are uncomfortable with the technology, have security concerns, or simply want to be seen in person.
There is the potential for missing a significant neurologic deficit with a telemedicine visit. We generally increase the time spent on history acquisition being sensitive for descriptors consistent with a neurological deficit (e.g., double vision, reduction in keyboard skills). Our neurologic examination can then be focused and extended to explore the areas of concern. While we have not identified any significant neurologic deficits missed during the telemedicine examination and subsequently identified at follow-up, we do recognize this as a possibility.
The time commitment for a successful telemedicine visit is significantly extended for the practitioners. We have noticed that the communication techniques change during telemedicine visits, especially if there are more than 2 access portals. Specifically, the slight verbal delay in communication requires that all participants allow a slight delay in their responses. Also, the entire process for the medical team is extended by the need to get the telemedicine connection established.
In our experience, this delay in response as well as the overall experience of the platform can lead to an unfortunate informality and loss of the typical provider/patient relationship that has been so important in developing a therapeutic relationship. This may be as obvious as observing ongoing unrelated activities in the camera background with associated visit interruptions. We also have noticed a tendency to lose focus during the examination with an associated need to re-establish priorities and timelines with the patient.
Conclusions
Although it is difficult to predict how the post-COVID-19 world would look like, current circumstances and changes in policy have encouraged and will likely encourage more physicians to set up telehealth as part of their practice. With the new infrastructure in place, policy makers and providers should work together to sustain the positive changes and paradigm shift in the delivery of health care.61
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Glazer E., Marshall C., Cunningham N. Remote pediatric consultation in the inner city: television or telephone? Am J Public Health. 1978;68:1133–1135. doi: 10.2105/ajph.68.11.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryu S. Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2) Healthcare Informatics Res. 2012;18:153. [Google Scholar]
- 3.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 4.Balas E.A., Jaffrey F., KupermanJ G.J. Electronic communication with patients. Evaluation of distance medicine technology. JAMA. 1997;278:152–159. [PubMed] [Google Scholar]
- 5.Davis L.E., Coleman J., Harnar J., King M.K. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health. 2014;20:473–477. doi: 10.1089/tmj.2013.0217. [DOI] [PubMed] [Google Scholar]
- 6.James H.E. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr. 2016;25:753–757. doi: 10.3171/2016.6.PEDS16202. [DOI] [PubMed] [Google Scholar]
- 7.Brooks N.P. Telemedicine is here. World Neurosurg. 2016;95:603–604. doi: 10.1016/j.wneu.2016.02.113. [DOI] [PubMed] [Google Scholar]
- 8.Harbrecht B.G., Smith J.W., Franklin G.A., Miller F.B., Richardson J.D. Decreasing regional neurosurgical workforce—a blueprint for disaster. J. Trauma Acute Care Surg. 2010;68:1367. doi: 10.1097/TA.0b013e3181d990da. [DOI] [PubMed] [Google Scholar]
- 9.Demaerschalk B.M., Miley M.L., Kiernan T.E.J. Stroke telemedicine. Mayo Clin. Proc. 2009;84:53–64. doi: 10.4065/84.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaMonte M.P., Bahouth M.N., Hu P. Telemedicine for acute stroke: triumphs and pitfalls. Stroke. 2003;34:725–728. doi: 10.1161/01.STR.0000056945.36583.37. [DOI] [PubMed] [Google Scholar]
- 11.George B.P., Scoglio N.J., Reminick J.I. Telemedicine in leading US neurology departments. Neurohospitalist. 2012;2:123–128. doi: 10.1177/1941874412450716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Medicare Medicaid Services Medicare telemedicine health care provider fact sheet. https://www.cms.gov/newsroom/fact-sheets/medicaretelemedicine-health-care-provider-fact-sheet Available at:
- 13.Gilman M., Stensland J. Telehealth and Medicare: payment policy, current use, and prospects for growth. Medicare Medicaid Res Rev. 2013;3 doi: 10.5600/mmrr.003.04.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becker C.D., Dandy K., Gaujean M., Fusaro M., Scurlock C. Legal perspectives on telemedicine part 1: legal and regulatory issues. Perm J. 2019;23 doi: 10.7812/TPP/18-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosman J., Slane S., Dery B. Is there a shortage of neurosurgeons in the United States? Neurosurgery. 2013;73:354–366. doi: 10.1227/01.neu.0000430762.08458.49. [DOI] [PubMed] [Google Scholar]
- 16.Latifi R., Gunn J.K.L., Bakiu E. Access to specialized care through telemedicine in limited-resource country: initial 1,065 teleconsultations in Albania. Telemed J E Health. 2016;22:1024–1031. doi: 10.1089/tmj.2016.0050. [DOI] [PubMed] [Google Scholar]
- 17.Medical Licensure Compact Participating States. https://www.imlcc.org/participating-states/ Available at: Accessed April 4, 2020.
- 18.American College of Surgeons COVID-19: Recommendations for Management of Elective Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at: Accessed April 4, 2020.
- 19.United States. Congress. House. Committee on Rules . 2020. Providing for Consideration of the Resolution (H. Res. 826) Expressing Disapproval of the Trump Administration’s Harmful Actions Towards Medicaid; Providing for Consideration of the Bill (H.R. 2474) to Amend the National Labor Relations Act, the Labor Management Relations Act, 1947, and the Labor-Management Reporting and Disclosure Act of 1959, and for Other Purposes; and Providing for Consideration of the Bill (H.R. 5687) Making Emergency Supplemental Appropriations for the Fiscal Year Ending September 30, 2020, and for Other Purpose: Report (to Accompany H. Res. 833) [Google Scholar]
- 20.CMS payment policies regulatory flexibilities during COVID-19 emergency. https://www.ama-assn.org/practice-management/medicare/cms-payment-policies-regulatory-flexibilities-during-covid-19 Available at: Accessed April 4, 2020.
- 21.American Medical Association Special coding advice during COVID-19 public health emergency. https://www.ama-assn.org/system/files/2020-04/covid-19-coding-advice.pdf Available at: Accessed April 4, 2020.
- 22.AMA quick guide to telemedicine in practice. https://www.ama-assn.org/practice-management/digital/ama-quick-guide-telemedicine-practice Available at: Accessed April 4, 2020.
- 23.American Academy of Neurology Telemedicine and COVID-19 Implementation Guide. https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist--administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf Available at: Accessed April 4, 2020.
- 24.Federation of State Medical Boards States Waiving Telehealth Licensure Requirements. https://www.fsmb.org/siteassets/advocacy/pdf/states-waiving-licensure-requirements-for-telehealth-in-response-to-covid-19.pdf Available at: Accessed April 4, 2020.
- 25.Drug Enforcement Agency COVID-19 Information Page. https://www.deadiversion.usdoj.gov/coronavirus.html Available at: Accessed April 4, 2020.
- 26.Texas Medical Association Telemedicine Vendor Options. 2020. https://www.texmed.org/uploadedFiles/Current/2016_Practice_Help/Health_Information_Technology/Telemedicine/Telemedicine%20Vendor%20Options.pdf Available at: Accessed April 4, 2020.
- 27.US Department of Health and Human Services OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. https://www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html Available at: Accessed April 4, 2020.
- 28.Smartphone users worldwide 2020 | Statista. https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/ Available at:
- 29.Zhang K., Liu W.-L., Locatis C., Ackerman M. Mobile videoconferencing apps for telemedicine. Telemedicine e-Health. 2016;22:56–62. doi: 10.1089/tmj.2015.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park H.-Y., Jeon S.-S., Lee J.-Y., Cho A.-R., Park J.H. Korean Version of the Mini-Mental State Examination using smartphone: a validation study. Telemed J E Health. 2017;23:815–821. doi: 10.1089/tmj.2016.0281. [DOI] [PubMed] [Google Scholar]
- 31.Sahin D., Hacisalihoglu U.P., Kirimlioglu S.H. Telecytology: is it possible with smartphone images? Diagn Cytopathol. 2018;46:40–46. doi: 10.1002/dc.23851. [DOI] [PubMed] [Google Scholar]
- 32.McBeth P., Crawford I., Tiruta C. Help is in your pocket: the potential accuracy of smartphone- and laptop-based remotely guided resuscitative telesonography. Telemed J E Health. 2013;19:924–930. doi: 10.1089/tmj.2013.0034. [DOI] [PubMed] [Google Scholar]
- 33.Craig J.J., McConville J.P., Patterson V.H., Wootton R. Neurological examination is possible using telemedicine. J Telemed Telecare. 1999;5:177–181. doi: 10.1258/1357633991933594. [DOI] [PubMed] [Google Scholar]
- 34.Reider-Demer M., Raja P., Martin N., Schwinger M., Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41:497–501. doi: 10.1007/s10143-017-0878-0. [DOI] [PubMed] [Google Scholar]
- 35.Thakar S., Rajagopal N., Mani S. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus. 2018;44:E17. doi: 10.3171/2018.2.FOCUS17543. [DOI] [PubMed] [Google Scholar]
- 36.Agnisarman S.O., Madathil K.C., Smith K. Lessons learned from the usability assessment of home-based telemedicine systems. Appl Ergon. 2017;58:424–434. doi: 10.1016/j.apergo.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 37.Gardner M.R., Jenkins S.M., O’Neil D.A. Perceptions of video-based appointments from the patient’s home: a patient survey. Telemedicine e-Health. 2015;21:281–285. doi: 10.1089/tmj.2014.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong Y.-R., Lawrence J., Williams D., Jr., Mainous A., III Population-level interest and telehealth capacity of US hospitals in response to COVID-19: Cross-sectional analysis of Google search and national hospital survey data. JMIR Public Health Surveill. 2020;6:e18961. doi: 10.2196/18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elble R., Bain P., Forjaz M.J. Task force report: scales for screening and evaluating tremor: critique and recommendations. Mov Disord. 2013;28:1793–1800. doi: 10.1002/mds.25648. [DOI] [PubMed] [Google Scholar]
- 40.Fahn S., Tolosa E., Marín C. Clinical rating scale for tremor. In: Jankovik J., Tolosa E., editors. Parkinson’s Disease and Movement Disorders. Urban and Schwarzenberg; Baltimore and Munch: 1988. pp. 225–234. [Google Scholar]
- 41.Elias W.J., Lipsman N., Ondo W.G. A randomized trial of focused ultrasound thalamotomy for essential tremor. N Engl J Med. 2016;375:730–739. doi: 10.1056/NEJMoa1600159. [DOI] [PubMed] [Google Scholar]
- 42.Verschuur C.V.M., Suwijin S.R., Boel J.A. Randomized delayed-start trial of levodopa in Parkinson’s disease. N Engl J Med. 2019;380:315–324. doi: 10.1056/NEJMoa1809983. [DOI] [PubMed] [Google Scholar]
- 43.Goetz C.G., Tilley B.C., Shaftman S.R. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–2170. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- 44.Abdolahi A., Scoglio N., Killoran A., Dorsey E.R., Biglan K.M. Potential reliability and validity of a modified version of the Unified Parkinson’s Disease Rating Scale that could be administered remotely. Parkinsonism Rel Disord. 2013;19:218–221. doi: 10.1016/j.parkreldis.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Evans D.A., Benameur K., Busis N.A. March 27, 2020: Telemedicine and COVID-19 – American Academy of Neurology [Webinar]. In AANChannel. https://www.youtube.com/watch?v=Pw-Jdy3-T9g Available at: Accessed April 4, 2020.
- 46.Agarwal S., Warburton E.A. Teleneurology: is it really at a distance? J Neurol. 2011;258:971–981. doi: 10.1007/s00415-011-5920-5. [DOI] [PubMed] [Google Scholar]
- 47.Smith S.N.C., Govindarajan P., Padrick M.M. A low-cost, tablet-based option for prehospital neurologic assessment. Neurology. 2016;87:19–26. doi: 10.1212/WNL.0000000000002799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zerna C., Jeerakathil T., Hill M.D. Telehealth for remote stroke management. Can J Cardiol. 2018;34:889–896. doi: 10.1016/j.cjca.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 49.Handschu R., Littman R., Reulbach U. Telemedicine in emergency evaluation of acute stroke: interrater agreement in remote video examination with a novel multimedia system. Stroke. 2003;34:2842–2846. doi: 10.1161/01.STR.0000102043.70312.E9. [DOI] [PubMed] [Google Scholar]
- 50.LaMonte M.P., Bahouth M.N., Xiao Y. Outcomes from a comprehensive stroke telemedicine program. Telemed. J E Health. 2008;14:339–344. doi: 10.1089/tmj.2007.0062. [DOI] [PubMed] [Google Scholar]
- 51.Lee D.J., Lozano C.S., Dallapiazza R.F., Lozano A.M. Current and future directions of deep brain stimulation for neurological and psychiatric disorders. J Neurosurg. 2019;131:333–342. doi: 10.3171/2019.4.JNS181761. [DOI] [PubMed] [Google Scholar]
- 52.Perlmutter J.S. Assessment of Parkinson disease manifestations. Curr Protoc Neurosci. 2009 doi: 10.1002/0471142301.ns1001s49. Chapter 10:Unit10.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Louis E.D., Lynch T., Marder K., Fahn S. Reliability of patient completion of the historical section of the unified Parkinson’s disease rating scale. Mov Disord. 1996;11:185–192. doi: 10.1002/mds.870110212. [DOI] [PubMed] [Google Scholar]
- 54.Martínez-Martín P., Bendito-Leon J., Alonso F. Patients’, doctors’, and caregivers’ assessment of disability using the UPDRS-ADL section: are these ratings interchangeable? Mov Disord. 2003;18:985–992. doi: 10.1002/mds.10479. [DOI] [PubMed] [Google Scholar]
- 55.Seidel S.E., Tilley B.C., Huang P. Subject-investigator reproducibility of the Unified Parkinson’s Disease Rating Scale. Parkinsonism Relat Disord. 2012;18:230–233. doi: 10.1016/j.parkreldis.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kane R.L., Bever C.T., Ehrmantraut M. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J Telemed Telecare. 2008;14:190–194. doi: 10.1258/jtt.2008.070904. [DOI] [PubMed] [Google Scholar]
- 57.Dorsey E.R., Glidden A.M., Holloway M.R. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. 2018;14:285–297. doi: 10.1038/nrneurol.2018.31. [DOI] [PubMed] [Google Scholar]
- 58.Louis E.D., Ferreira J.J. How common is the most common adult movement disorder? Update on the worldwide prevalence of essential tremor. Mov Disord. 2010;25:534–541. doi: 10.1002/mds.22838. [DOI] [PubMed] [Google Scholar]
- 59.Patel U.K., Malik P., DeMasi M., Lunagariya A., Jani V.B. Multidisciplinary approach and outcomes of tele-neurology: a review. Cureus. 2019;11:e4410. doi: 10.7759/cureus.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Samii A., Tyan-Dykes P., Tsukuda R.A. Telemedicine for delivery of health care in Parkinson’s disease. J Telemed Telecare. 2006;12:16–18. doi: 10.1258/135763306775321371. [DOI] [PubMed] [Google Scholar]
- 61.Klein B.C., Busis N.A. COVID-19 is catalyzing the adoption of teleneurology. https://doi.org/10.1212/WNL.0000000000009494 [e-pub ahead of print]. Neurology. accessed April 4, 2020. [DOI] [PubMed]