Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has created significant obstacles within medical education. For medical students interested in pursuing neurosurgery as a specialty, the educational policies surrounding COVID-19 have resulted in unique challenges. The present study used a nationwide survey to identify the concerns of medical students interested in pursuing neurosurgery during the COVID-19 pandemic.
Methods
Students who had previously registered for medical student neurosurgery training camps were sent an online Qualtrics survey requesting them to assess how the COVID-19 pandemic was affecting their neurosurgical education. The Pearson χ2 test and post hoc pairwise Fisher exact test were used for analysis of categorical variables, and the 2-tailed paired Student t test was used for continuous variables.
Results
The survey was distributed to 852 medical students, with 127 analyzed responses. Concerns regarding conferences and networking opportunities (63%), clinical experience (59%), and board examination scores (42%) were most frequently cited. Of the third-year medical students, 76% reported ≥1 cancelled or postponed neurosurgery rotation. On average, students were more likely to take 1 year off from medical school after than before the start of the COVID-19 pandemic, measured from 0 to 100 (25.3 ± 36.0 vs. 39.5 ± 37.5; P = 0.004). Virtual mentorship pairing was the highest rated educational intervention suggested by first- and second-year medical students. The third- and fourth-year medical students had cited virtual surgical skills workshops most frequently.
Conclusions
The results from the present nationwide survey have highlighted the concerns of medical students regarding their neurosurgery education during the COVID-19 pandemic. With these findings, neurosurgery organizations can consider targeted plans for students of each year to continue their education and development.
Key words: Concerns, COVID-19, Education, Medical student, Neurosurgery, Residency, Training camp
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; OR, Operating room
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has created significant obstacles for physicians and medical educators regarding the delivery of healthcare and medical education. For medical students interested in pursuing neurosurgery as a specialty, the educational policies surrounding COVID-19 have resulted in unique challenges.
Neurosurgery is widely regarded as one of the most competitive specialties, as evidenced by one of the highest average U.S. Medical Licensing Examination Step 1 scores and median publication rates.1 Thus, medical students must be highly engaged and productive during their preclinical and clinical years to build strong residency applications. At most institutions, formal exposure to neurosurgery during medical school is weighted toward the senior years, and it is often the responsibility of the student to explore the field during earlier years.2 , 3 Because of this absence of clinical exposure, medical students' perceptions of the field, often shrouded in stereotypes, weigh heavily in the decision-making process and have been the subject of recent studies.4 , 5 However, as might be expected, student perceptions are not static and are significantly shaped by increased exposure to the field, in particular, after rotating through the neurosurgery electives6 and gaining increased experience in the neurosurgical operating room (OR).7
In a time during which students are prohibited from the OR and exposure to neurosurgery has been further limited, it is essential to recognize these limitations and devise methods to facilitate student engagement. To the best of our knowledge, the factors related to the COVID-19 pandemic that affect medical student education in neurosurgery have not been investigated in a large nationwide cohort of U.S. medical students. In the present study, we used a nationwide survey to identify the concerns held by neurosurgery-minded medical students during the COVID-19 pandemic and understand what educational interventions are most desired by these students to ensure their continued education and development.
Methods
Medical Student Registry
The medical student neurosurgery training camp has been held annually since its inaugural year in 2018.5 , 8 , 9 A registry of 852 medical students from across the United States who had registered for the training camp for any year was maintained by the authors. This large sample of U.S. medical students with an interest in neurosurgery was leveraged to outline the factors in question regarding the effects of the COVID-19 pandemic on neurosurgical education.
Data Collection
The medical students in the training camp registry were sent an online survey via e-mail requesting their assessment of the effects of the COVID-19 pandemic on their neurosurgical education. Their demographic information, including current medical institution, medical trainee program and year, race, ethnicity, and gender, was collected. Their baseline interest in neurosurgery was established by asking participants to rank their interest in neurosurgery as a potential specialty choice from 0 (tangential interest) to 100 (firm commitment) using a sliding scale. Respondents with a stated interest score of <50 were excluded from the statistical analysis to ensure our study had included students most invested in neurosurgery education.
In the survey (Supplementary Figure 1), the respondents were asked to describe how COVID-19 has affected their neurosurgical education within several domains, including their clinical experience, research productivity, and networking opportunities. Students were also requested to identify methods by which neurosurgical organizations might better respond to medical students' evolving educational needs.
The online survey was designed and distributed using survey quality and distribution software (Qualtrics, Provo, Utah, USA). The survey responses were maintained confidential as noted in the opening message of the survey. The Weill Cornell institutional review board approved the present study (protocol no. 20-04021871).
Statistical Analysis
Microsoft Excel (Microsoft Corp., Redmond, Washington, USA) and R statistical software, version 4.0.0 (R Foundation, Vienna, Austria), were used for statistical analysis and data visualization using a database of survey responses exported from Qualtrics. The Pearson χ2 test and post hoc pairwise Fisher exact test were used for analysis of the categorical variables, and the 2-tailed paired Student t test was used for continuous variables. A P value of ≤0.05 was considered to indicate statistical significance.
Results
Demographics and Study Population
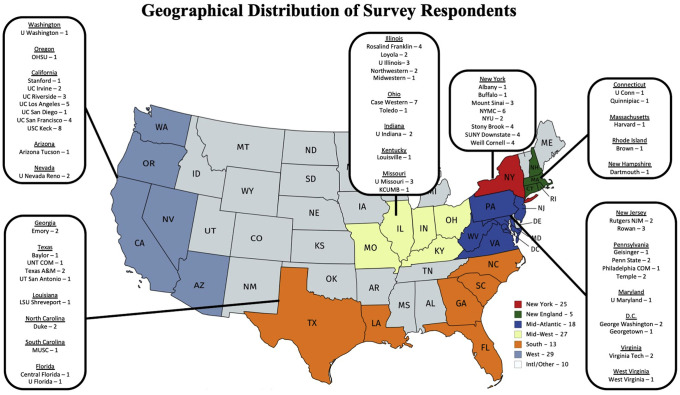
The survey was distributed to 852 students, with 133 complete responses (completion rate, 16%). However, 6 respondents were excluded from the analysis because of a stated interest in neurosurgery of <50 of 100 points. Thus, 127 responses were analyzed. The breakdown of respondents by class year was 39 first-year medical (M1) students, 25 second-year (M2), 34 third-year (M3), and 13 fourth-year medical (M4s) students, with 16 students in a different year of training (e.g., PhD year, research year). All the respondents were seeking MD, MD/PhD, or DO degrees. The demographic data, including gender, race, and ethnicity, were collected and stratified by medical school year (Table 1 ). None of the student demographic factors varied significantly by year of medical training in our sample. However, comparing our aggregate student sample to the historical data from the Accreditation Council of Graduate Medical Education for the 2018-2019 U.S. neurosurgery residents, we found that our sample contained a significantly greater proportion of female students (P < 0.0001), racial minorities (P = 0.03), and ethnic minorities (P < 0.0001).10 The respondents represented 56 different medical institutions from 27 states across the United States (Figure 1 ). The number of students at each medical school that were sent the survey and the number of those who responded are listed in Supplementary Table 1. The large representation from the west and northeast regions of the United States closely mirrors the distribution found in previous studies of students from the medical student neurosurgery training camp.5 , 8 , 9 The mean student interest level in neurosurgery was 88.8 ± 15.2, with 0 indicating tangential interest and 100 indicating firm commitment.
Table 1.
Respondent Demographics Stratified by Medical Student Year∗
| Variable | M1 (n = 39) | M2 (n = 25) | M3 (n = 34) | M4 (n = 13) | Other (n = 16) | Total (n = 127) | 2018-2019 U.S. Neurosurgery Residents (n = 1462) | P Value |
|---|---|---|---|---|---|---|---|---|
| Gender | 5.28e-12 | |||||||
| Female | 43.6 (17) | 56.0 (14) | 32.4 (11) | 30.8 (4) | 37.5 (6) | 40.9 (52) | 17.3 (253) | |
| Male | 51.3 (20) | 44.0 (11) | 67.6 (23) | 46.2 (6) | 50.0 (8) | 53.5 (68) | 82.0 (1199) | |
| Nonbinary | 2.6 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.8 (1) | NA | |
| Prefer not to answer | 0 (0) | 0 (0) | 0 (0) | 7.7 (1) | 0 (0) | 0.8 (1) | NA | |
| Not answered | 2.6 (1) | 0 (0) | 0 (0) | 15.4 (2) | 12.5 (2) | 3.9 (5) | 0.7 (10) | |
| Race | 0.0274 | |||||||
| Native American or Alaskan Native | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.1 (2) | |
| Asian or Pacific Islander | 25.6 (10) | 28.0 (7) | 26.5 (9) | 15.4 (2) | 18.8 (3) | 24.4 (31) | 14.4 (210) | |
| Black | 7.7 (3) | 8.0 (2) | 14.7 (5) | 7.7 (1) | 18.8 (3) | 11.0 (14) | 4.0 (59) | |
| White | 59.0 (23) | 48.0 (12) | 55.9 (19) | 38.5 (5) | 56.3 (9) | 53.5 (68) | 49.9 (729)† | |
| Other | 15.4 (6) | 12.0 (3) | 11.8 (4) | 7.7 (1) | 0 (0) | 11.0 (14) | 7.2 (105) | |
| Prefer not to answer | 0 (0) | 4.0 (1) | 5.9 (2) | 15.4 (2) | 6.3 (1) | 4.7 (6) | NA | |
| Did not answer | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6.3 (1) | 0.8 (1) | 20.2 (295) | |
| Ethnicity | 6.55e-5 | |||||||
| Hispanic or Latino | 23.1 (9) | 12.0 (3) | 5.9 (2) | 15.4 (2) | 6.3 (1) | 13.4 (17) | 4.2 (62) | |
| Non-Hispanic | 74.4 (29) | 84.0 (21) | 85.3 (29) | 53.8 (7) | 81.3 (13) | 78.0 (99) | 75.6 (1105) | |
| Prefer not to answer | 0 (0) | 4.0 (1) | 2.9 (1) | 15.4 (2) | 0 (0) | 3.1 (4) | 0 (0) | |
| Not answered | 2.6 (1) | 0 (0) | 5.9 (2) | 15.4 (2) | 12.5 (2) | 5.5 (7) | 20.2 (295) |
Data presented as % (n).
M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students; NA, not applicable.
No demographic factor varied significantly between medical student years, but our cohort had significantly higher proportions of female and racial/ethnic minorities compared to 2018-2019 neurosurgery residents in the United States.
Non-Hispanic white.
Figure 1.
Map showing the number of respondents from 56 medical institutions within 27 states across the United States.
Medical Student Concerns Related to COVID-19
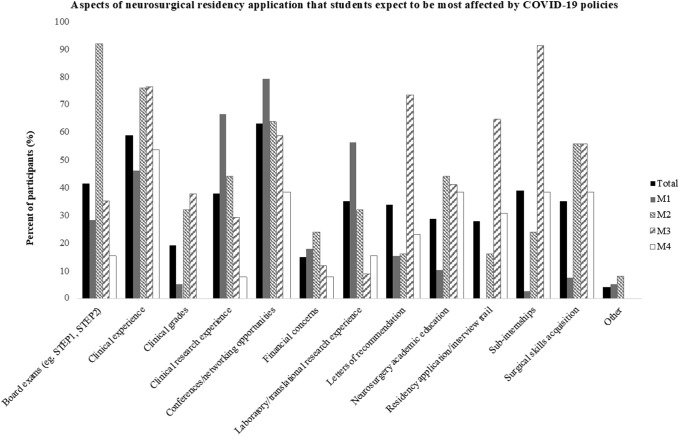
The students were asked which aspects of their neurosurgery residency application cycle would be most affected by the COVID-19 pandemic (Figure 2 ). Concerns regarding conferences and networking opportunities (63%), clinical experience (59%), board examination scores (42%), subinternships (39%), and clinical research experience (38%) were the most frequently cited issues. These factors were also stratified by medical trainee year. Of the 39 M1 students, 31 (79%) were concerned about the effects of COVID-19 on conferences and networking opportunities. Of the 25 M2 students, 23 (92%) and 19 (76%) were concerned about board examinations and clinical experience, respectively. Of the 34 M3 students, 31 (91%) reported concerns about subinternships, 25 (74%) were concerned about letters of recommendation, and 22 (65%) were concerned about the residency application and interview trail. Concerns regarding how COVID-19 would affect surgical skills acquisition increased significantly from M1 to M2 students (8% vs. 56%; P < 0.001) and from M1 to M3 students (8% vs. 56%; P < 0.001). Other reported concerns included effects on preclinical grades, cancellation of summer research programs, and increasing the length of PhD programs.
Figure 2.
Bar graphs showing aspects of neurosurgical residency application students expect to be most affected by coronavirus disease 2019 (COVID-19) policies stratified by medical student year. Students in their PhD or research year (n = 16) were excluded for better visualization. M1, first year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students.
The rates of various clinical experiences affected by COVID-19 are summarized in Table 2 . Most of the M3 students reported cancellation of home (56%) and away (62%) neurosurgical subinternships, with 26 (76%) reporting ≥1 cancelled or postponed neurosurgical rotation. We identified cancellation or postponement of neurosurgery subinternships at 25 different institutions. We also found that 21 of the 39 M1 students (54%) reported cancellation of clinical shadowing days.
Table 2.
Clinical Experience Changes Due To Coronavirus Disease 2019 Policies Stratified by Medical Student Year
| Clinical Experience | M1 | M2 | M3 | M4 | Other |
|---|---|---|---|---|---|
| Cancelled neurosurgical conferences | 77.0 (30) | 64.0 (16) | 70.6 (24) | 69.2 (9) | 62.5 (10) |
| Postponed/shortened away neurosurgery subinternship | 2.6 (1) | 4.0 (1) | 61.8 (21) | 30.8 (4) | 43.8 (7) |
| Postponed/shortened home neurosurgery elective (or subinternship) | 5.1 (2) | 20.0 (5) | 55.9 (19) | 30.8 (4) | 18.8 (3) |
| Postponed/shortened neurology clerkship | 2.6 (1) | 8.0 (2) | 14.7 (5) | 0 (0) | 12.5 (2) |
| Postponed/shortened surgery clerkship | 5.1 (2) | 28.0 (7) | 26.5 (9) | 0 (0) | 0 (0) |
| Scheduled neurosurgery shadowing days cancelled | 53.8 (21) | 40.0 (10) | 20.6 (7) | 0 (0) | 25.0 (4) |
| Other | 7.7 (3) | 16.0 (4) | 2.9 (1) | 7.7 (1) | 18.8 (3) |
Data presented as % (n).
M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students.
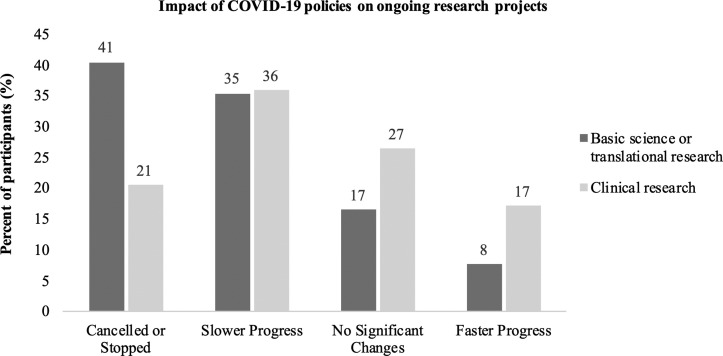
From a research perspective, basic or translational research was stopped in 41% of cases, slowed in 35% of cases, was unchanged in 17% of cases, and was conducted at a faster rate in 8% of cases. Clinical research projects were stopped in 21% of cases, slowed in 36% of cases, experienced no change in 27% of cases, and increased in progress in 17% of cases (Figure 3 ). Other methods by which medical students are maintaining productivity are summarized in Table 3 .
Figure 3.
Bar graph showing effect of institution-specific coronavirus disease 2019 (COVID-19) policies on the progress of ongoing laboratory-based and clinical research.
Table 3.
Methods by Which Medical Students Are Attempting to Stay Productive
| Mode of Productivity | M1 | M2 | M3 | M4 | Other |
|---|---|---|---|---|---|
| Continuing medical record review of clinical research projects | 35.9 (14) | 32.0 (8) | 61.8 (21) | 53.8 (7) | 43.8 (7) |
| Pursuing virtual clinical electives related to COVID-19 patient care | 5.1 (2) | 12.0 (3) | 35.3 (12) | 15.4 (2) | 0 (0) |
| Redeployment to COVID-19 patient care in ER/ICU/telehealth | 0 (0) | 0 (0) | 5.9 (2) | 15.4 (2) | 6.3 (1) |
| Studying∗ | 82.1 (32) | 96.0 (24) | 97.1 (33) | 53.8 (7) | 50.0 (8) |
| Volunteering for COVID-19–related activities† | 56.4 (22) | 24.0 (6) | 38.2 (13) | 30.8 (4) | 37.5 (6) |
| Working on systematic reviews/meta-analyses | 48.7 (19) | 20.0 (5) | 35.3 (12) | 46.2 (6) | 43.8 (7) |
| Other | 0 (0) | 0 (0) | 8.8 (3) | 7.7 (1) | 25.0 (4) |
Data presented as % (n).
M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students; COVID-19, coronavirus disease 2019; ER, emergency room; ICU, intensive care unit.
Board examinations, neurosurgery electives, preclinical curriculum, clerkships, and so forth.
Personal protective equipment donation programs, fundraisers, and so forth.
The students were asked to estimate a score from 0 to 100 regarding how likely they were to take 1 year off from medical school before the COVID-19 pandemic and how likely they were to take 1 year off at the time of their survey response (Figure 4 ). On average, the students reported being more likely to take 1 year off from medical school after COVID-19 than before the start of the pandemic (25.3 ± 36.0 vs. 39.5 ± 37.5; P = 0.004). Although each class had a higher cumulative score for taking 1 year off after the COVID-19 pandemic, no individual class showed statistically significant differences for this measure (Table 4 ).
Figure 4.
Bar graphs showing self-reported likelihood score (0, not taking 1 year off; 100, certainly taking 1 year off) for taking 1 year off from medical school before and after the start of coronavirus disease 2019 (COVID-19) stratified by medical student year (n = 112). Respondents reported they were more likely to take 1 year off after the start of the COVID-19 pandemic than they were previously for each medical student year. However, the differences were not statistically significant when analyzed by each individual year. Plotted values represent the mean self-reported likelihood score. Error bars represent the standard error. M1, first year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students.
Table 4.
Self-Reported Scores for Taking 1 Year Off∗
| Medical Student Year (n) | Before COVID-19 | After COVID-19 | P Value |
|---|---|---|---|
| M1 (36) | 22.3 ± 5.0 | 36.1 ± 5.4 | 0.07 |
| M2 (24) | 16.4 ± 4.9 | 33.4 ± 7.4 | 0.07 |
| M3 (32) | 22.2 ± 6.4 | 39.4 ± 6.6 | 0.07 |
| M4 (10) | 34.6 ± 14.0 | 43.8 ± 14.3 | 0.67 |
| Other (10) | 63 ± 14.6 | 65.5 ± 12.6 | 0.90 |
| Entire cohort (112) | 25.3 ± 3.3 | 39.5 ± 3.5 | 0.004 |
Data presented as mean ± standard error.
COVID-19, coronavirus disease 2019; M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students.
Possible scores ranged from 0 (not taking 1 year off) to 100 (certainly taking 1 year off). The students reported being more likely to take 1 year off after the start of COVID-19 (P = 0.004). Although this relationship remained consistent for each student year, the differences were not statistically significant.
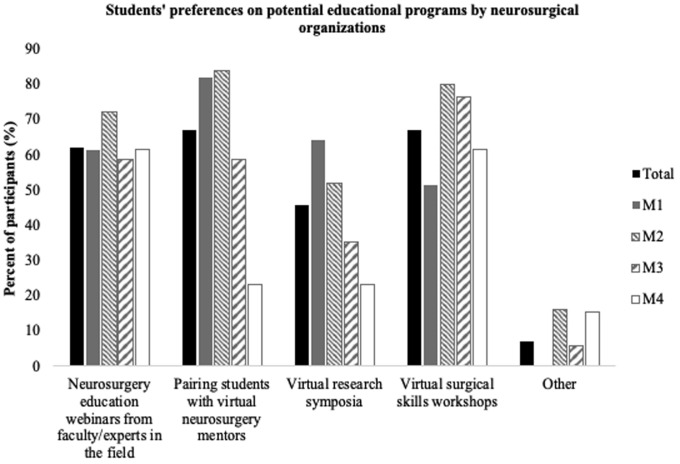
The students were asked to report what educational programs could be offered by neurosurgical organizations (e.g., American Association of Neurological Surgeons, Congress of Neurological Surgeons) to ensure trainee development during this time (Figure 5 ). Virtual mentorship programs and virtual surgical skills workshops were each suggested by 67% of the students, 62% of the respondents suggested neurosurgery education webinars, and 46% suggested virtual research symposia. The highest rated educational intervention suggested by the M1 and M2 students was virtual mentorship pairing with faculty. The M3 and M4 students cited virtual surgical skills workshops most frequently. Other suggestions included establishing a firm consensus on the changes to the 2020 application cycle and expanding access to virtual surgical simulation training.
Figure 5.
Bar graph showing potential educational programs students would prefer to see neurosurgical organizations offer. Students in PhD or research year (n = 16) were excluded for better visualization. M1, first year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students.
Discussion
In the present study, we attempted to quantify the effects of changes resulting from the COVID-19 pandemic on medical student exposure and experience within neurosurgery. We found a near ubiquitous concern among survey responders, with students concerned about the preclinical, clinical, and research portions of their neurosurgery application. This uncertainty faced by students was captured by our finding that the respondents were significantly more likely to take 1 year off after the COVID-19 pandemic.
Among the COVID-19–related changes to the medical students' clinical experiences, the cancellation or postponement of neurosurgical subinternships might have the greatest effect on neurosurgical applicants. Without subinternships, students will lose opportunities to obtain letters of recommendation, gauge the cultural differences among the neurosurgical training programs, and demonstrate their character and competence in clinical and OR settings. Consequently, in the upcoming residency application cycle, the focus might inevitably shift toward the more objective aspects of a residency application, such as board examination scores and clerkship grades.
From a research perspective, the greatest disruptions were to laboratory-based research projects. Most of our respondents involved in basic or translational science research reported the slowing or stopping of their project. This was not surprising, because many institutions have deemed laboratory research as “nonessential” and research projects have been forced to discontinue. Clinical research was less affected than laboratory-based research, as might be expected. However, nearly 1-in-5 respondents stated that clinical research had accelerated, potentially owing to the increased time available for students who no longer had curricular responsibilities.
Cancellation of neurosurgical conferences was among the most frequently cited COVID-19–related changes, consistent with the cohort's high level of concern regarding the cancellation of conferences and loss of networking opportunities. This level of concern potentially stemmed from the weight placed on research productivity in the neurosurgical residency application.11 Medical students were especially concerned about the loss of mentorship opportunities, which was highlighted, not only by a high number of respondents citing this as a concern, but also by virtual mentorship pairing being the most frequently suggested educational intervention by early-year medical students (M1 and M2).
Medical students have been continuously looking for ways to remain productive and stay engaged during these times. Thus, it is imperative for departments to foster continued student engagement, mentorship, and exposure to neurosurgery. Although virtual platforms have been used to facilitate continued productivity within neurosurgical departments, students should also be invited to be involved. As an example, our institution has established a collaborative neurosurgery publication group.12 Weekly virtual meetings are held to discuss ongoing projects, brainstorm new ideas, and foster mentorship with faculty.
Neurosurgical organizations and academic institutions must find creative ways to adapt educational programming for students interested in neurosurgery. Our study should serve as a medium for students to dialogue with organized neurosurgery regarding which interventions they believe will be the most beneficial. The most cited interventions in our survey were virtual mentorship pairings and virtual surgical skills workshops. Some efforts are underway to meet these requests at our own institution, which will be offering virtual simulation training and webinars in neurosurgical anatomy. Another example is the American Association of Neurological Surgeons mentorship program, in which student members can match with mentors according to their needs and interests. This program will be especially valuable for M1 and M2 students who have not yet found mentors in neurosurgery. In addition, increasing numbers of presentation-based webinars are being offered by neurosurgical organizations. Finally, as indicated by many respondents to our survey, medical students have been hoping for a consensus statement from neurosurgical organizations regarding how some of these specific changes will affect students in their residency application process. The Society of Neurological Surgeons recently released a statement cancelling all away neurosurgery rotations. Similar communications from organized neurosurgery on other aspects of the path to residency will deepen trust by students and offer much needed guidance. Above all, the results of our study have highlighted the uncertainty that medical students interested in neurosurgery are facing during this time.
Our study had a number of limitations. First, the present study was limited because the data were collected by self-report survey and, therefore, was susceptible to a response bias. Students might have responded in a manner that overestimated their concern, knowing that the survey might be used to inform neurosurgical education programming. Second, most of our cohort showed high levels of interest in neurosurgery; thus, the results might not have accurately captured the experiences and perceptions of medical students still in the earlier stages of contemplation regarding a career in neurosurgery. Third, the present study was limited by the respondents having been either previous or future registrants for the medical student neurosurgery training camp and, therefore, might not be representative of all medical students intending to pursue a career in neurosurgery. The present study, however, did successfully capture a large, geographically diverse, cohort of U.S. medical students. For example, 34 of our respondents were M3 students, which, given that the average number of U.S. neurosurgery residency applicants during the previous 5 years was 247,13 our study included ~13.8% of next year's applicant cohort. In addition, the cohort of students included in our study included greater proportions of female and ethnic or racial minority students compared with the 2018-2019 U.S. neurosurgery residents found in the Accreditation Council of Graduate Medical Education database. This might illustrate a trend towards diversification of the medical students interested in pursuing a career in neurosurgery. However, it remains unclear whether this relationship will translate into which subsets of students in our study eventually apply for a neurosurgery residency. Finally, although we believe that many of our conclusions will be applicable to trainees at other stages of their neurosurgical training, including residents, our survey focused only on medical students. Additional studies might help to clarify the challenges faced by other neurosurgical trainees to increase the generalizability of our findings.
Conclusions
In the midst of the COVID-19 pandemic, the results from the present nationwide survey have highlighted the concerns of medical students interested in neurosurgery, how their education and research have been altered as a result of the pandemic, and how their preparatory plans for residency might have changed. In addition, we have provided information on what strategies medical students perceive to be beneficial for their continued education and mentorship. Thus, neurosurgery departments and organizations can consider targeted plans, stratified by medical school year, for students to make up for lost experience owing to COVID-19.
CRediT authorship contribution statement
Sergio W. Guadix: Conceptualization, Data curation, Formal analysis, Visualization, Writing - original draft, Writing - review & editing, Methodology. Graham M. Winston: Conceptualization, Data curation, Formal analysis, Writing - original draft, Writing - review & editing, Methodology. John K. Chae: Conceptualization, Data curation, Formal analysis, Visualization, Writing - original draft, Writing - review & editing, Methodology. Arsalan Haghdel: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Justin Chen: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Iyan Younus: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Ryan Radwanski: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Jeffrey P. Greenfield: Conceptualization, Writing - original draft, Writing - review & editing, Methodology. Susan C. Pannullo: Methodology, Conceptualization, Writing - original draft, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Data
Survey used to determine medical students’ concerns relating to neurosurgery during the coronavirus disease 2019 (COVID-19) pandemic. AANS, American Association of Neurological Surgeons; CNS, Congress of Neurological Surgeons; ER, emergency room; ICU, intensive care unit; M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students; PGY-1, postgraduate year 1; PPE, personal protective equipment; Q, question.
Supplementary Table 1.
Students Sent the Survey and Those Who Responded∗
| Medical School | Students Sent Survey (n) | Respondents (n) |
|---|---|---|
| Albany Medical College | 3 | 1 |
| Albert Einstein College of Medicine | 2 | 0 |
| Baylor College of Medicine | 2 | 1 |
| Boston University School of Medicine | 1 | 0 |
| Burrell College of Osteopathic Medicine | 1 | 0 |
| Campbell University Jerry M. Wallace School of Osteopathic Medicine | 1 | 0 |
| Carle Illinois College of Medicine | 1 | 0 |
| Case Western Reserve University School of Medicine | 12 | 7 |
| Charles E. Schmidt College of Medicine at Florida Atlantic University | 2 | 0 |
| Chicago Medical School, Rosalind Franklin University of Medicine and Science | 13 | 4 |
| City University of New York School of Medicine | 5 | 0 |
| Columbia University Vagelos College of Physicians and Surgeons | 25 | 0 |
| Cooper Medical School of Rowan University | 2 | 0 |
| Creighton University School of Medicine | 1 | 0 |
| Donald and Barbara Zucker School of Medicine at Hofstra/Northwell | 1 | 0 |
| Drexel University College of Medicine | 2 | 0 |
| Duke University School of Medicine | 3 | 2 |
| Emory University School of Medicine | 5 | 2 |
| Florida State University College of Medicine | 2 | 0 |
| Frank H. Netter MD School of Medicine at Quinnipiac University | 2 | 1 |
| Geisel School of Medicine at Dartmouth | 1 | 1 |
| Geisinger Commonwealth School of Medicine | 6 | 1 |
| George Washington School of Medicine and Health Sciences | 3 | 2 |
| Georgetown University School of Medicine | 2 | 1 |
| Harvard Medical School | 16 | 1 |
| Howard University College of Medicine | 1 | 0 |
| Icahn School of Medicine at Mount Sinai | 12 | 3 |
| Indiana University School of Medicine | 4 | 2 |
| Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo | 3 | 1 |
| Keck School of Medicine of USC | 60 | 8 |
| Loma Linda University School of Medicine | 3 | 0 |
| Louisiana State University Health Sciences Center, Shreveport | 1 | 1 |
| Loyola University Chicago Stritch School of Medicine | 2 | 2 |
| Mayo Clinic Alix School of Medicine, Phoenix/Scottsdale | 1 | 0 |
| Mayo Clinic Alix School of Medicine, Rochester | 5 | 0 |
| Medical College of Georgia at Augusta University | 1 | 0 |
| Medical University of South Carolina | 2 | 1 |
| Michigan State University College of Human Medicine | 2 | 0 |
| Michigan State University College of Osteopathic Medicine | 2 | 0 |
| New York Institute of Technology College of Osteopathic Medicine | 2 | 0 |
| New York Medical College | 93 | 6 |
| New York University School of Medicine | 20 | 2 |
| Northwestern University Feinberg School of Medicine | 23 | 2 |
| Not listed/listed incorrectly | 59 | 7 |
| Nova Southeastern University Dr. Kiran C. Patel College of Allopathic Medicine | 1 | 0 |
| Oregon Health & Science University School of Medicine | 3 | 1 |
| Pennsylvania State University College of Medicine | 11 | 2 |
| Perelman School of Medicine at the University of Pennsylvania | 1 | 0 |
| Philadelphia College of Osteopathic Medicine | 5 | 1 |
| Rowan University School of Osteopathic Medicine | 16 | 3 |
| Rutgers New Jersey Medical School | 17 | 2 |
| Rutgers Robert Wood Johnson Medical School | 5 | 0 |
| Sackler School of Medicine, Tel Aviv University | 1 | 0 |
| San Juan Bautista School of Medicine | 4 | 3 |
| Seton Hall-Hackensack Meridian | 1 | 0 |
| Sidney Kimmel Medical College at Thomas Jefferson University | 9 | 0 |
| Stanford University School of Medicine | 11 | 1 |
| State University of New York Downstate Medical Center College of Medicine | 41 | 0 |
| State University of New York Upstate Medical University College of Medicine | 8 | 4 |
| Stony Brook University School of Medicine | 13 | 4 |
| Temple University Lewis Katz School of Medicine | 7 | 2 |
| Texas A&M Health Science Center College of Medicine | 12 | 2 |
| Texas College of Osteopathic Medicine | 2 | 1 |
| The Johns Hopkins University School of Medicine | 1 | 0 |
| The Max Rady College of Medicine at University of Manitoba | 1 | 0 |
| The University of Chicago Pritzker School of Medicine | 1 | 0 |
| Touro University College of Osteopathic Medicine | 2 | 0 |
| Tufts University School of Medicine | 3 | 0 |
| University of Alabama School of Medicine | 1 | 0 |
| University of Alberta Faculty of Medicine and Dentistry | 1 | 0 |
| University of Arizona, Tucson, College of Medicine | 3 | 1 |
| University of Arkansas for Medical Sciences | 1 | 0 |
| University of California, Davis, School of Medicine | 3 | 0 |
| University of California, Irvine, School of Medicine | 10 | 2 |
| University of California, Los Angeles, David Geffen School of Medicine | 27 | 5 |
| University of California, Riverside, School of Medicine | 8 | 3 |
| University of California, San Diego, School of Medicine | 2 | 1 |
| University of California, San Francisco, School of Medicine | 14 | 4 |
| University of Central Florida College of Medicine | 9 | 1 |
| University of Connecticut School of Medicine | 1 | 1 |
| University of Florida College of Medicine | 2 | 1 |
| University of Illinois College of Medicine | 7 | 3 |
| University of Kentucky College of Medicine | 1 | 0 |
| University of Louisville School of Medicine | 1 | 1 |
| University of Maryland School of Medicine | 1 | 1 |
| University of Massachusetts Medical School | 4 | 0 |
| University of Miami Miller School of Medicine | 3 | 0 |
| University of Minnesota Medical School | 1 | 0 |
| University of Missouri, Columbia, School of Medicine | 3 | 3 |
| University of Missouri, Kansas City, School of Medicine | 2 | 1 |
| University of Nevada, Reno, School of Medicine | 6 | 2 |
| University of North Dakota School of Medicine and Health Sciences | 1 | 0 |
| University of Oklahoma College of Medicine | 3 | 0 |
| University of Ottawa | 2 | 1 |
| University of Puerto Rico School of Medicine | 4 | 0 |
| University of Rochester School of Medicine | 2 | 0 |
| University of South Florida Morsani College of Medicine | 2 | 0 |
| University of Texas at San Antonio Long School of Medicine | 6 | 1 |
| University of Toledo College of Medicine and Life Sciences | 2 | 1 |
| University of Toronto | 1 | 0 |
| University of Virginia School of Medicine | 1 | 0 |
| University of Washington School of Medicine | 4 | 1 |
| Virginia Tech Carilion School of Medicine | 3 | 2 |
| Warren Alpert Medical School of Brown University | 5 | 1 |
| Wayne State University School of Medicine | 4 | 0 |
| Weill Cornell Medical College | 104 | 4 |
| West Virginia School of Osteopathic Medicine | 1 | 0 |
| West Virginia University School of Medicine | 1 | 1 |
| Western Michigan University Homer Stryker M.D. School of Medicine | 1 | 0 |
| Wright State University Boonshoft School of Medicine | 1 | 0 |
| Yale University School of Medicine | 7 | 0 |
USC, University of Southern California.
Of the 133 students with complete responses, 6 were excluded because of their score for the stated interest in neurosurgery of <50 of 100.
References
- 1.Moeser P.J. The national resident matching program. Arch Intern Med. 1990;150:221–225. doi: 10.1001/archinte.150.1.221b. [DOI] [PubMed] [Google Scholar]
- 2.Fox B.D., Amhaz H.H., Patel A.J. Neurosurgical rotations or clerkships in US medical schools: clinical article. J Neurosurg. 2011;114:27–33. doi: 10.3171/2010.5.JNS10245. [DOI] [PubMed] [Google Scholar]
- 3.Lobel D.A., Kahn M., Rosen C.L., Pilitsis J.G. Medical student education in neurosurgery: optional or essential? Teach Learn Med. 2015;27:201–204. doi: 10.1080/10401334.2015.1011656. [DOI] [PubMed] [Google Scholar]
- 4.Burford C., Hanrahan J., Ansaripour A. Factors influencing medical student interest in a career in neurosurgery. World Neurosurg. 2019;122:e367–e374. doi: 10.1016/j.wneu.2018.10.056. [DOI] [PubMed] [Google Scholar]
- 5.Guadix S.W., Younus I., Winston G. Medical students’ perceived interests and concerns for a career in neurosurgery. https://doi.org/10.1016/j.wneu.2020.03.169 [e-pub ahead of print]. World Neurosurg. accessed May 2, 2020. [DOI] [PubMed]
- 6.Zuckerman S.L., Mistry A.M., Hanif R. Neurosurgery elective for preclinical medical students: early exposure and changing attitudes. World Neurosurg. 2016;86:120–126. doi: 10.1016/j.wneu.2015.08.081. [DOI] [PubMed] [Google Scholar]
- 7.Zuccato J.A., Kulkarni A.V. The impact of early medical school surgical exposure on interest in neurosurgery. Can J Neurol Sci. 2016;43:410–416. doi: 10.1017/cjn.2015.332. [DOI] [PubMed] [Google Scholar]
- 8.Radwanski R.E., Winston G., Younus I. Neurosurgery training camp for sub-internship preparation: lessons from the inaugural course. World Neurosurg. 2019;127:e707–e716. doi: 10.1016/j.wneu.2019.03.246. [DOI] [PubMed] [Google Scholar]
- 9.Radwanski R.E., Winston G., Younus I. Medical student neurosurgery training camp: updates following 2019 course expansion. World Neurosurg. 2019;130:561–563. doi: 10.1016/j.wneu.2019.07.157. [DOI] [PubMed] [Google Scholar]
- 10.Accreditation Council for Graduate Medical Education ACGME Data Resource Book 2018-2019. https://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book Available at: Accessed May 9, 2020.
- 11.Wadhwa H., Shah S.S., Shan J. The neurosurgery applicant's "arms race": analysis of medical student publication in the neurosurgery residency match. https://doi.org/10.3171/2019.8.jns191256 [e-pub ahead of print]. J Neurosurg. accessed May 2, 2020. [DOI] [PubMed]
- 12.Chae J., Haghdel A., Guadix S.W. Letter: COVID-19 impact on the medical student path to neurosurgery. https://doi.org/10.1093/neuros/nyaa187 [e-pub ahead of print]. Neurosurgery. accessed May 2, 2020. [DOI] [PMC free article] [PubMed]
- 13.Yaeger K.A., Munich S.A., Byrne R.W., Germano I.M. Trends in United States neurosurgery residency education and training over the last decade (2009-2019) Neurosurg Focus. 2020;48:E6. doi: 10.3171/2019.12.FOCUS19827. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey used to determine medical students’ concerns relating to neurosurgery during the coronavirus disease 2019 (COVID-19) pandemic. AANS, American Association of Neurological Surgeons; CNS, Congress of Neurological Surgeons; ER, emergency room; ICU, intensive care unit; M1, first-year medical students; M2, second-year medical students; M3, third-year medical students; M4, fourth-year medical students; PGY-1, postgraduate year 1; PPE, personal protective equipment; Q, question.