Abstract
Aims
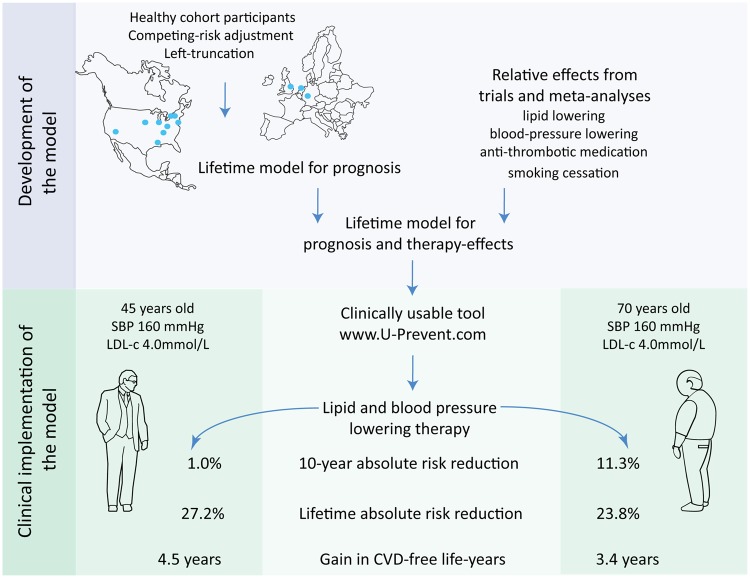
The benefit an individual can expect from preventive therapy varies based on risk-factor burden, competing risks, and treatment duration. We developed and validated the LIFEtime-perspective CardioVascular Disease (LIFE-CVD) model for the estimation of individual-level 10 years and lifetime treatment-effects of cholesterol lowering, blood pressure lowering, antithrombotic therapy, and smoking cessation in apparently healthy people.
Methods and results
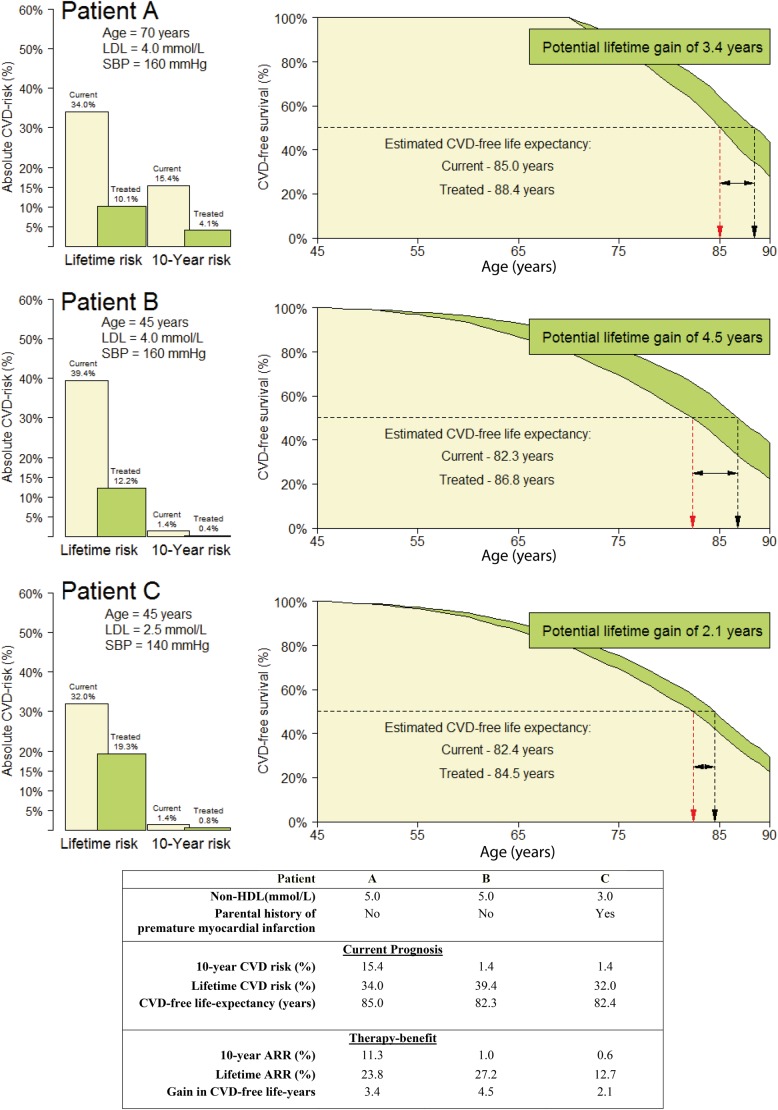
Model development was conducted in the Multi-Ethnic Study of Atherosclerosis (n = 6715) using clinical predictors. The model consists of two complementary Fine and Gray competing-risk adjusted left-truncated subdistribution hazard functions: one for hard cardiovascular disease (CVD)-events, and one for non-CVD mortality. Therapy-effects were estimated by combining the functions with hazard ratios from preventive therapy trials. External validation was performed in the Atherosclerosis Risk in Communities (n = 9250), Heinz Nixdorf Recall (n = 4177), and the European Prospective Investigation into Cancer and Nutrition-Netherlands (n = 25 833), and Norfolk (n = 23 548) studies. Calibration of the LIFE-CVD model was good and c-statistics were 0.67–0.76. The output enables the comparison of short-term vs. long-term therapy-benefit. In two people aged 45 and 70 with otherwise identical risk-factors, the older patient has a greater 10-year absolute risk reduction (11.3% vs. 1.0%) but a smaller gain in life-years free of CVD (3.4 vs. 4.5 years) from the same therapy. The model was developed into an interactive online calculator available via www.U-Prevent.com.
Conclusion
The model can accurately estimate individual-level prognosis and treatment-effects in terms of improved 10-year risk, lifetime risk, and life-expectancy free of CVD. The model is easily accessible and can be used to facilitate personalized-medicine and doctor–patient communication.
Keywords: Cardiovascular disease prevention, Therapy-benefit, Lifetime prediction, Apparently healthy people
See page 1200 for the editorial comment on this article (doi: 10.1093/eurheartj/ehz515)
Introduction
Cardiovascular disease (CVD) is a significant cause of worldwide morbidity and healthcare costs. While healthy lifestyles are universally recommended, in people without CVD lipid-lowering, blood pressure lowering, and antithrombotic therapy are recommended only when a certain risk-factor burden, 10-year CVD-risk, or combination of both has been reached.1–6 However, the benefit an individual can expect from preventive therapy varies based on risk, risk-factor burden, competing risks, and treatment duration, with higher pre-treatment risk and longer treatment duration providing a greater absolute risk reduction (ARR).
Various risk-assessment models have been endorsed by national and international guidelines.5–9 Age is a major driver of 10-year risk, and consequentially, the use of such short-term risk may delay treatment in young individuals with a high lifetime-benefit until an age at which a 10-year risk threshold is crossed. Conversely, therapy may provide a large 10-year ARR in older individuals, but advanced age and limited life-expectancy restrict the gain in healthy life-years from preventive therapy.10,11 In recent years, guidelines have begun endorsing the use of lifetime risk-assessment in conjunction with short-term estimations.5,6 Existing lifetime scores such as QRISK-lifetime12 and the Pooled Cohorts Equations (PCE)13 provide estimations of lifetime risk and the potential benefits of risk-factor modification. However, there are certain obstacles regarding implementation of some scores. Not accounting for competing-risks and using older development data commonly lead to risk overestimation. Moreover, lifetime risk is not estimated across all ages and the international generalizability or external availability of the algorithms is lacking.5,6 There is thus a need to develop an internationally validated competing-risk adjusted model with the ability to estimate both 10-year and lifetime therapy-benefit. Such a model should estimate the effects of starting, stopping, altering, or postponing specific pharmacotherapies and lifestyle strategies.
The objective of this study was to develop and validate the competing-risk adjusted LIFEtime-perspective model for individualizing CardioVascular Disease prevention strategies in apparently healthy people (LIFE-CVD). The LIFE-CVD model aims to estimate the effect of cholesterol lowering, blood pressure lowering, aspirin-equivalent antithrombotic therapy, and smoking cessation in terms of 10-year and lifetime CVD-risk, and life-years gained free of CVD in apparently healthy people. The model will be made available via an interactive online calculator.
Methods
Study populations
The study was conducted using data from multiple North-American and European cohorts (details described in Supplementary material online, Table S1). The Multi-Ethnic Study of Atherosclerosis (MESA) cohort commenced recruitment in 2000 and is an ethnically and geographically diverse American cohort.14 The Atherosclerosis Risk in Communities Study (ARIC) commenced approximately 10 years earlier than MESA but was otherwise similar in recruitment strategy and design. Due to the difference in commencement years, the 4th follow-up visit in ARIC (1996–1998) was used as the baseline for these analyses.15 The Heinz Nixdorf Recall (Risk factors, Evaluation of Coronary Calcium and Lifestyle) study (HNR, 2000–2003) is a population-based cohort study from the German Ruhr area.16 The European Prospective Investigation into Cancer-Netherlands (EPIC-NL, 1993–1997) study is formed by the Dutch MORGEN-EPIC and the Prospect-EPIC cohorts.17 The European Prospective Investigation into Cancer-Norfolk (EPIC-Norfolk, 1993–1997) is a population-based cohort from Norfolk, the UK.18 Participants <45 years, with a history of CVD, heart failure, chronic kidney disease epidemiology collaboration estimated glomerular filtration rate (CKD-EPI eGFR) <30 mL/min/1.73 m2 (unavailable in EPIC-NL), and terminal malignancy (unavailable in HNR) at baseline were excluded. As the model aims to estimate both therapy initiation, cessation, and alteration, no exclusion of participants was made based on medication use. As the model aims to estimate 10-year and lifetime risk for people aged 45–80 years, those >80 years at baseline were not included in validation cohorts. Patients aged >80 years at baseline were included in the development cohort to stabilize estimations between the 80th and 90th life-years. The upper age was set because predictions become unstable when age-group size becomes small.5,6
Clinically applicable predictors
Predictors were pre-specified based on the literature and availability in clinical practice: gender, systolic blood pressure (SBP, mmHg), non-high-density lipoprotein cholesterol (non-HDLc, mmol/L), body mass index (kg/m2), smoking status (current, former, and never), presence of diabetes mellitus (yes/no, 2007 American Diabetes Association fasting criteria), and a positive history of premature (prior to age 60) myocardial infarction (MI) in either parent.5,6,12 Missing data handling is described in Supplementary material online, Methods S1.
Outcomes
Cardiovascular disease-events were defined as fatal or non-fatal MI or stroke, resuscitated cardiac arrest, and coronary heart disease (CHD)-death. The competing-risk outcome was death from any non-CVD cause. Follow-up time was defined as years until the first CVD-event, death, or end of follow-up. Supplementary material online, Table S2 provides outcome definitions and adjudication processes.
Model development
The model was developed in the MESA cohort due to the wide range of baseline ages, relatively recent commencement (2000), and a high degree of racial/ethnic diversity. The statistical methods have previously been described in detail.19 The model comprises of two complementary Fine and Gray competing-risk adjusted left-truncated subdistribution hazard functions: one for CVD-events (subdistribution hazard function A) and one for non-CVD mortality (subdistribution hazard function B). Age was used as the time-scale (i.e. left truncation), meaning participants contributed from the age at cohort entry to the age at end of follow-up. Continuous predictors were winsorized at the 1st and 99th percentile and transformed if this improved model fit. An age-predictor interaction was used if predictor strength changed with age (Schoenfeld residual P < 0.05). Supplementary material online, Methods S1 describes transformations and non-proportional hazards.
Individual estimation of prognosis
Individual estimations are based on lifetables with 1-year age intervals. Each life-year has an age-specific 1-year baseline survival for both CVD-events and CVD-mortality (Supplementary material online, Table S3). The baseline survival was combined with clinical predictors to estimate the risk of having a CVD-event or non-CVD mortality for each life-year (Supplementary material online, Table S4). The cumulative survival for each life-year was subsequently estimated by multiplying the survival probability of that life-year (1 minus CVD risk minus non-CVD mortality risk) by the survival probability at the beginning of each life-year. The (cumulative) survival thus depends on the combination of CVD-risk and non-CVD risk. The process was repeated until age 90 years to provide estimations of 10-year risk for people with baseline ages less than or equal to 80 years. A complete, reproducible, patient example of a lifetable is provided Supplementary material online, Table S5. Lifetime risk was defined as the risk of having a CVD-event before the 90th life-year. The CVD-free life-expectancy is defined as the median survival without a CVD-event or death and is thus equivalent to the age at which the cumulative survival probability becomes <0.5.
Model validation
Internal validation was performed on a set of MESA participants drawn by bootstrapping from the dataset of individuals aged 45–80 years at baseline. Lifetime models are based on 1-year lifetable intervals and may thus require internal intercept recalibration. Hence, the expected vs. observed ratio of CVD-events and non-CVD mortality in MESA was used to recalibrate the intercepts. External validation was then performed in ARIC, HNR, EPIC-NL, and EPIC-Norfolk. Model discrimination was assessed using c-statistics and agreement between expected-and-observed 10-year risk was assessed using calibration plots for CVD-events, non-CVD mortality, and the combined risk of these two events (i.e. the LIFE-CVD model). Geographical differences in event rates were corrected based on the intercept recalibration in the HNR-study, and the same recalibration coefficients were used for the other European cohorts. No recalibration was performed in ARIC as this has the same geographic location as MESA.
Race sensitivity analyses
Race/ethnicity was not selected as a predictor due to the heterogeneity of definitions between countries and the complex and poorly generalizable mechanisms via which race may mediate cardiovascular risk.20 However, to investigate model accuracy for different race/ethnicities, a race-stratified validation of the developed LIFE-CVD model was performed for African Americans and Caucasians in MESA and ARIC. Additionally, to compare the effects of race/ethnicity in the separate cohorts, two exploratory models were developed (one derived in MESA, the other in ARIC) which included race (i.e. African American, Caucasian or other) as a predictor. The hazard ratios (HRs) for race in these two models were compared.
Individual therapy-benefit
The alteration of patient-characteristics to reflect updated risk-factors provides an observational, rather than causal, assessment of risk-factor changes.13 To estimate the causal effects of therapy, the developed subdistribution hazard functions were combined with HRs obtained from randomized clinical trials and meta-analyses for cholesterol-lowering, blood pressure lowering, aspirin-equivalent antithrombotic therapy, and smoking.13 By using the HRs from meta-analyses which included people both receiving and not receiving preventive therapy at baseline, the effect of starting, stopping, intensifying, postponing, or reducing therapy can be estimated (details in Supplementary material online, Methods S2). Cause-specific 1-year on-treatment survival was calculated by inserting the HR of treatment into either subdistribution hazard function (A), (B), or both (Supplementary material online, Table S4). The 10-year and lifetime ARR is the difference between on- and off-treatment predicted CVD-risk after 10 years or until 90 years of age, respectively. The gain in life-years free of CVD is the difference between on- and off-treatment CVD-free life-expectancy. Three patient examples demonstrate using the LIFE-CVD tool to predict therapy-effects.
Results
Study population
Baseline characteristics of the 69 523 participants are shown in Table 1. The 6715 MESA participants used for the derivation of the LIFE-CVD model were ethnically diverse, with 39% self-reporting as Caucasian, 28% as African American, 22% as Hispanic, and 12% as Chinese American. In MESA, 621 CVD-events and 795 non-CVD deaths occurred over a median follow-up duration of 13.0 years.
Table 1.
Baseline characteristics
| MESA (n = 6715) | ARIC (n = 9250) | HNR (n = 4177) | EPIC-NL (n = 25 833) | EPIC-Norfolk (n = 23 548) | |
|---|---|---|---|---|---|
| Age (years) | 62 (53–70) | 62 (58–67) | 59 (52–65) | 55 (51–60) | 59 (52–67) |
| Gender (male) | 53% | 42% | 47% | 17% | 44% |
| Race | |||||
| Caucasian | 39% | 78% | 100% | 96% | 100% |
| African American | 28% | 22% | 0% | 0% | 0% |
| Other | 34% | 0% | 0% | 4% | 0% |
| Parental history of premature MI | 15% | 16% | 22% | 13% | 7% |
| Body mass index (kg/m2) | 28 (25–31) | 28 (25–31) | 27 (25–30) | 26 (23–28) | 26 (24–28) |
| Non-HDL (mmol/L) | 3.7 (3.1–4.2) | 3.9 (3.3–4.5) | 4.4 (3.8–5.1) | 4.3 (3.6–5.0) | 4.7 (3.9–5.5) |
| Systolic blood pressure (mmHg) | 124 (111–140) | 125 (114–138) | 132 (118–145) | 129 (117–141) | 134 (123–147) |
| Smoking status | |||||
| Current | 14% | 14% | 23% | 27% | 12% |
| Former | 37% | 42% | 33% | 35% | 42% |
| Diabetes mellitus | 14% | 15% | 12% | 3% | 2% |
Data are presented as median (25th–75th percentile) or frequency (%).
EPIC-NL is assumed to be 96% Caucasian based on genetic analyses. HNR is assumed to be 100% Caucasian.
MI, myocardial infarction; non-HDL, non-high-density lipoprotein cholesterol.
Development of the LIFE-CVD model
Subdistribution HRs for CVD-events (A) and non-CVD mortality (B) are shown in Table 2. These HRs are prognostic and should not be viewed causally. Age-specific baseline survival (Supplementary material online, Table S3) and the completed algorithm for both subdistribution hazard functions (Supplementary material online, Table S4) are provided to enable external use of the model.
Table 2.
Multivariable hazard ratios in the LIFE-CVD model
| Subdistribution hazard function A (CVD-events) | Subdistribution hazard function B (non-CVD mortality) | |
|---|---|---|
| Gender (male) | 1.62 (1.38–1.92) | 0.98 (0.83–1.17)a |
| Systolic blood pressure (per 10 mmHg) | 1.12 (1.08–1.17)a | 1.03 (1.00–1.07) |
| Non-HDL cholesterol (mmol/L) | 1.13 (1.03–1.24) | 0.83 (0.64–1.07)b |
| Body mass index (kg/m2) | 1.01 (1.00–1.03) | 0.98 (0.62–1.56)b |
| Former smoker | 1.03 (0.86–1.23) | 1.26 (1.07–1.47) |
| Current smoker | 1.59 (1.25–2.02)a | 2.04 (1.65–2.52)a |
| Diabetes mellitus | 1.76 (1.42–2.20)a | 1.30 (1.04–1.63)a |
| Parental history of premature MI | 1.46 (1.19–1.79) | 0.93 (0.76–1.14) |
Age-dependent. HRs shown for median age of 62 years.
Transformed variable. HRs shown for the 75% vs. 25% percentile (non-HDL-c 4.24 mmol/L vs. 3.08 mmol/L; body mass index 31 kg/m2 vs. 25 kg/m2).
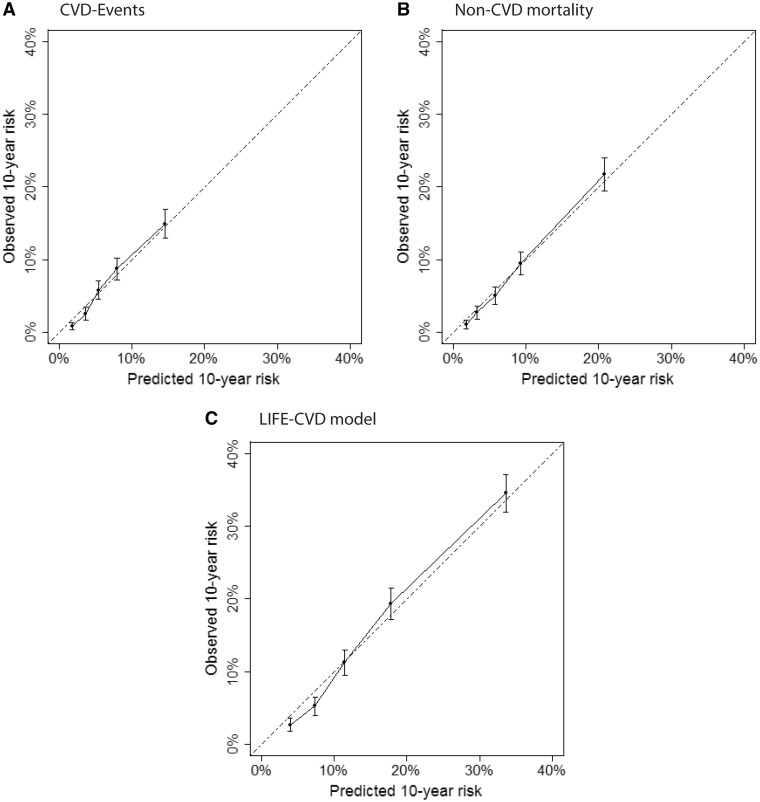
Internal validation
Of the 6715 participants used for derivation, the 6526 individuals aged 45 through 80 years at baseline were resampled with replacement. The median predicted 10-year CVD risk is depicted in Supplementary material online, Table S6. In this validation-set, the predicted 10-year risk for CVD-events, non-CVD mortality, and combined outcome of CVD-events and non-CVD mortality (i.e. the LIFE-CVD model), showed good agreement with the 10-year observed risk (Figure 1). C-statistics for discrimination of 10-year CVD-risk was 0.73 [95% confidence interval (CI) 0.71–0.75], non-CVD mortality risk was 0.76 (95% CI 0.75–0.78), and combined risk was 0.74 (95% CI 0.73–0.75).
Figure 1.
Internal calibration of predicted vs. observed 10-year risk with 95% confidence intervals in the Multi-Ethnic Study of Atherosclerosis validation cohort for (A) cause-specific cardiovascular disease-event risk, (B) cause-specific non-cardiovascular disease mortality risk, and (C) cardiovascular disease-event and non-cardiovascular disease mortality risk combined (i.e. the LIFE-CVD model).
External validation
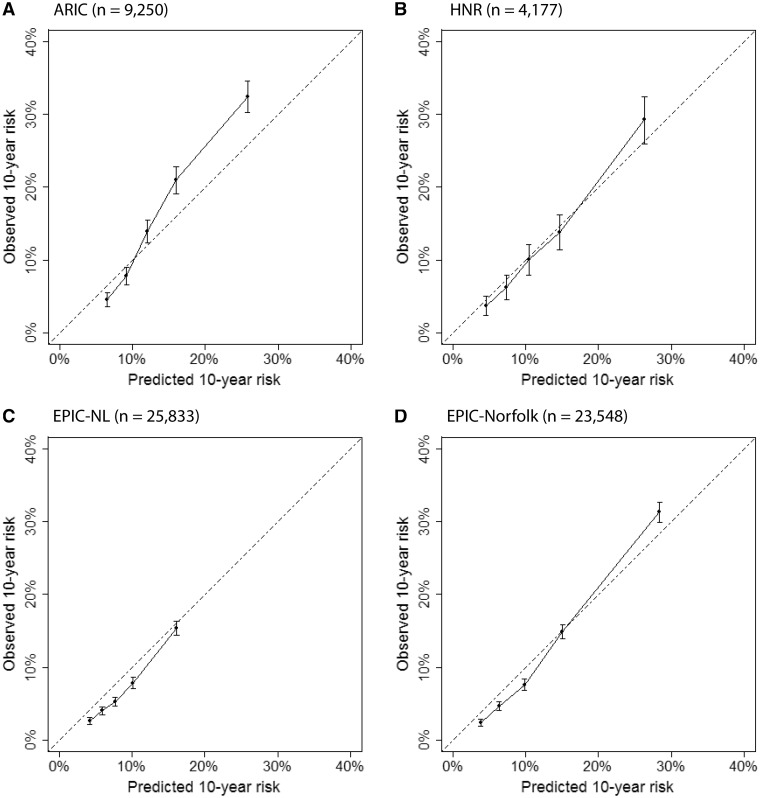
The expected vs. observed ratio in the HNR study was 1.17 for CVD-events and 0.85 for non-CVD mortality. These recalibration coefficients were used and validated in the EPIC-NL and EPIC-Norfolk cohorts. The predicted and observed 10-year risk for the combined outcome of CVD-events and all-cause mortality showed good agreement (Figure 2). C-statistics for discrimination ranged from 0.68–0.76 for CVD-risk, 0.67–0.74 for non-CVD mortality risk, and 0.69–0.76 for combined risk (Supplementary material online, Table S7).
Figure 2.
External calibration of predicted vs. observed 10-year risk of cardiovascular disease-event and non-cardiovascular disease mortality risk combined (i.e. the LIFE-CVD model) with 95% confidence intervals in (A) the Atherosclerosis Risk in Communities Study (ARIC), (B) the Heinz Nixdorf Recall (HNR), (C) the European Prospective Investigation into Cancer-Netherlands (EPIC-NL), and (D) the European Prospective Investigation into Cancer-Norfolk (EPIC-Norfolk).
Race sensitivity analyses
Race-stratified analyses were performed on the 1887 African Americans and 2600 Caucasians in the MESA validation set and the 2029 African Americans and 7194 Caucasians in the ARIC study. Stratified calibration plots are provided in Supplementary material online, Figure S1. C-statistics ranged from 0.69 to 0.76 for African Americans and 0.67 to 0.77 for Caucasians (Supplementary material online, Table S8). In the exploratory model derived in MESA, which included race as a predictor, the multivariate HR for African-American vs. Caucasians was non-significant. When the model was derived in ARIC, HRs were significant but of different direction than those derived in MESA (Supplementary material online, Table S9).
Individual estimation of prognosis
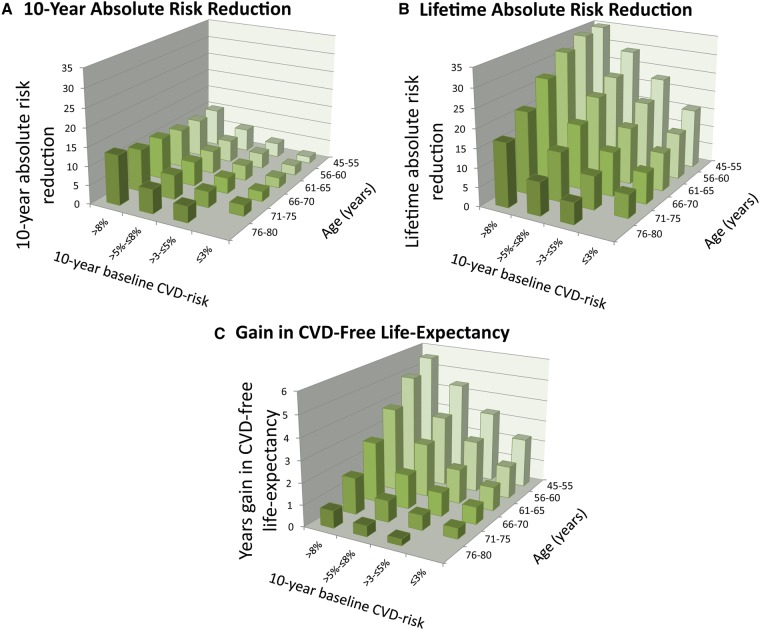
The developed LIFE-CVD model can be accessed via www.U-Prevent.com. Patient characteristics, current and future treatment, and age of treatment initiation can be entered into the tool. Three patient-examples are provided in Figure 3, in which the effect of concurrently achieving an SBP of 130 mmHg and initiating daily atorvastatin 40 mg are compared. The 70-year-old Patient A has the exact same risk-profile as the 45-year-old Patient B. However, Patient A has a higher 10-year CVD risk (15.4% vs. 1.4%), but a lower lifetime risk (34.0% vs. 39.4%) and a higher life-expectancy (85.0 vs. 82.3 years). Patients B and C have the same age and 10-year risk. Patient B has higher SBP and LDL-c levels and a greater gain in CVD-free life-expectancy from modifying these risk-factors. The same risk-modifying strategy modelled in the individual patient examples (start atorvastatin 40 mg and achieve SBP of 130 mmHg) was applied to the MESA-validation population (Figure 4). Ten-year ARR increased with increasing baseline risk, and remained relatively consistent over each age stratum. Lifetime ARR and gain in CVD-free life-expectancy increased with increasing baseline risk, but decreased with baseline age.
Figure 3.
Therapy-benefit from atorvastatin 40 mg and achieving an systolic blood pressure of 130 mmHg in three non-diabetic, former-smoking, European males with a body mass index of 28 kg/m2.
Figure 4.
Distribution of individual (A) 10-year ARR%, (B) lifetime ARR%, and (C) gain in life-expectancy for the 6526 individuals in the Multi-Ethnic Study of Atherosclerosis validation cohort associated with the initiation of atorvastatin 40 mg and achieving a systolic blood pressure of 130 mmHg stratified by baseline 10-year risk and age. Smoking status and aspirin use were not altered.
Take home figure.
Development and clinical implementation of a model to estimate lifetime therapy-effects illustrated with two patient examples.
Discussion
In this study of 69 523 individuals, we developed and validated the LIFE-CVD model for apparently healthy people without CVD between 45 and 80 years of age. Validation demonstrated the predictive reliability of the model. Individualized effects cholesterol lowering, blood pressure lowering, aspirin-equivalent antithrombotic therapy, and smoking cessation can be estimated in terms of 10-year ARR, lifetime ARR, and gain in CVD-free life-years using readily available clinical characteristics. Calibration and discrimination are comparable to existing primary prevention models such as the PCE.5 For researchers, the full algorithm with completed examples are provided to enable external use. The clinical tool can be accessed freely on www.U-Prevent.com.
Although the atherosclerotic process can begin in early adulthood, the majority of CVD-events happen after middle-age.21 Therefore, most younger adults have a low 10-year CVD risk whereas most older adults have a high 10-year risk, regardless of risk-factor burden. However, the lifetime benefit decreases with age and increases with increasing risk-factor burden. Early initiation of risk-modifying strategies therefore results in greater lifetime therapy-benefit,10 intuitively demonstrated by the greater lifetime gain from smoking cessation at age 30 vs. age 60.22 A benefit-based approach to other therapies would shift eligibility away from older individuals and towards younger individuals with a high risk-factor burden. Lifetime risk in the American College of Cardiology/American Heart Association Atherosclerotic Cardiovascular Disease (ACC-AHA-ASCVD) risk-estimator (based on the PCE) is defined as the cumulative risk of CVD-events over 30 years. The score does not provide estimations of CVD-free life-expectancy. Although 30-year risk provides a greater time-horizon than 10 years, the use of a fixed time-horizon makes it difficult to compare the therapy-benefit between individuals of different ages. Accordingly, the risk-calculator for the PCE does not provide 30-year risk estimations for individuals past a certain age.2
Lifetime estimates may be easier for the patient to understand. Integrating these estimates into decision-tools may enhance the clinician-patient risk-discussion.23 The use in clinical practice could help patients and clinicians gain insight into the individual effects of prevention when considering starting therapy, but also when therapy cessation or dose-lowering is considered due to the presence of side-effects. Lifetime estimates can also help identify patients who would benefit from early therapy-initiation. Early initiation also means a longer treatment duration, and thus greater costs. On a population-level, cost-effectiveness studies can determine what gain in CVD-free life-years would outweigh the increased costs and harms of early treatment.
The strengths of this study include combining a competing-risk adjusted model with the best available evidence on risk-reduction from therapy. Not accounting for competing risks leads to an overestimation of pre-treatment CVD-risk in young individuals over the long-term, or in any individual where the risk of a competing event is high. Trials and meta-analyses provide a comprehensive group-level analysis for individuals both on- and off-medications. As reliable evidence become available in the future, new prevention strategies will be added to the LIFE-CVD model. Furthermore, the study used data from ethnically and geographically diverse population-based cohorts, allowing for both geographic recalibration, and the subsequent validation of the recalibration coefficients. In external validation, a slight underestimation of risk was seen in the highest risk-quintile, where the observed (non)-fatal CVD-event risk >10%. However, this finding may be of reduced clinical relevance as the estimated (non)-fatal CVD-event risk also exceeds treatment thresholds (>7.5%) above which pharmacotherapy is often indicated in people without prior CVD in American guidelines.2,5 In European guidelines, pharmacotherapy is often indicated for those with a 10-year risk of fatal CVD-events >5%.1,6 Race can be poorly defined and have different cultural definitions and gene/environment interactions in separate regions24; a view point reflected in the HRs for race found in the exploratory models when derived in both MESA and ARIC. For these reasons, the model was derived in a multi-ethnic cohort, and risk-factors thought to mediate the biological effects of race were included. A third strength is the use of the contemporary MESA cohort to derive the model, which commenced in 2000. Models derived using older baseline data may provide clinically significant overestimations of CVD-risk in contemporary populations.25,26
Certain limitations should be acknowledged. Validation is performed for 10-year risk, as it is not feasible to perform validation over the course of an individual’s lifetime, and the model assumes baseline risks for each life-year remain stable over time. Previous studies have however shown the validity of lifetime predictions for up to 17 years.19 Nevertheless, as the follow-up duration in the validation cohort increases, the LIFE-CVD model could be updated and validated over the long-term. Also, lifetime estimations assume that all risk-factors, except age, remain stable over time. In reality, a patient may have an increase in blood pressure of the course of a few years, or may develop comorbidities. Therefore, lifetime estimations should be performed at regular time-intervals, such as every 10-years. Another important assumption of lifetime therapy-benefit estimations is that patients will be fully adherent to the prescribed medication for their remaining lifetimes. However, therapy-adherence is a common problem, and the LIFE-CVD model could be used as communication aid to address the importance of adherence and the consequences of non-adherence.
CVD-prevention guidelines suggest lifetime estimates may be useful for communicating risk, but that competing risks make providing lifetime CVD estimates for some groups problematic.5,6 Although a few scores such as the QRISK provide lifetime estimations,12 there are no competing-risk adjusted lifetime models developed for the primary prevention populations in Europe as a whole.6 Similarly, the PCE is lacks competing-risk adjustment and only provides long-term estimates for younger individuals. The competing-risk adjusted LIFE-CVD model therefore fills an important gap in risk-prediction. For populations not used in the development or validation (e.g. eastern European or Asian), the LIFE-CVD model represents the best available model to estimate treatment-effects. Further investigations may also involve specific validation and eventual recalibration of the model to these geographic locations. In the future, including characteristics such as the presence of a monogenetic dyslipidaemias might improve predictions for those with these relatively rare characteristics. However, the addition of new markers to a well-functioning prognostic model rarely provides meaningful prognostic value to the model as a whole.27
In conclusion, the LIFE-CVD model can estimate therapy-benefit from CVD risk-modification in apparently healthy people. The developed tool is freely available via www.U-Prevent.com and estimates the individualized benefit from cholesterol- and blood pressure lowering, aspirin-equivalent antithrombotic therapy, and smoking cessation in terms of 10-year and lifetime absolute CVD-risk reduction, and gain in CVD-free life-expectancy. Use of the tool may increase insight into therapy-benefit via the complementary use of 10-year and lifetime estimates and may facilitate individualized medicine and doctor–patient communication.
Supplementary Material
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; the Department of Veterans Affairs; or the U.S. Department of Health and Human Services.
The authors thank the staff and participants of the ARIC study for their important contributions. The authors acknowledge and thank study participants, general practitioners, and the EPIC Norfolk study team for their contribution to the work.
Funding
This work was partially funded by a grant from the Netherlands Heart Foundation (2016T026).
The MESA study is supported by contracts HHSN268201500003I, N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, and N01-HC-95169 from the National Heart, Lung, and Blood Institute, and by grants UL1-TR-000040, UL1-TR-001079, and UL1-TR-001420 from NCATS. The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). The EPIC-NL study is supported by the ‘Europe Against Cancer’ programme of the European commission; Dutch ministry of health, Welfare and Sports; Netherlands Organization for Research and Development; and World Cancer Research Fund. The EPIC-Norfolk study was supported by the Medical Research Council, UK http://www.mrc.ac.uk/ (Ref: G9502233 and MR/N003284/1) and Cancer Research UK http://www.cancerresearchuk.org/ (CRUK, Ref: SP2024/0201 and 14136). The HNR study was funded by the Heinz Nixdorf Foundation [Chairman: Martin Nixdorf; Past Chairman: Dr jur. Gerhard Schmidt (deceased)]. This study is also supported by the German Ministry of Education and Science (BMBF), and the German Aero-space Center [Deutsches Zentrum für Luft- und Raumfahrt (DLR)], Bonn, Germany. The German Research Council Assessment supported the study (DFG project: ER 155/6-2) and funded the study of psychosocial factors and neighbourhood level information (DFG project SI 236/8-1 and SI 236/9-1). The sponsor of the study transferred the monitoring of the study to the German Ministry of Education and Science, Bonn, using an international advisory board and quality control as well as event committee.
Conflict of interest: V.N. is on the editorial board of Dynamed. All other authors declared no conflict of interest.
References
- 1. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, Hoes AW, Jennings CS, Landmesser U, Pedersen TR, Reiner Z, Riccardi G, Taskinen MR, Tokgozoglu L, Monique Verschuren WM, Vlachopoulos C, Wood DA, Luis Zamorano J, Additional C, Cooney MT.. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Rev Esp Cardiol (Engl Ed) 2017;70:115.. [DOI] [PubMed] [Google Scholar]
- 2. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J.. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018. [Google Scholar]
- 3. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e484–e594. [DOI] [PubMed] [Google Scholar]
- 4. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 5. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O'Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC Jr, Sorlie P, Stone NJ, Wilson PW, Jordan HS, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S49–S73. [DOI] [PubMed] [Google Scholar]
- 6. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WM; Authors/Task Force Members. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Board JBS. Joint British Societies' consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014;100: ii1–ii67. [DOI] [PubMed] [Google Scholar]
- 8. Rabar S, Harker M, O'Flynn N, Wierzbicki AS, Guideline Development G.. Lipid modification and cardiovascular risk assessment for the primary and secondary prevention of cardiovascular disease: summary of updated NICE guidance. BMJ 2014;349:g4356.. [DOI] [PubMed] [Google Scholar]
- 9.Network SIG. Risk Estimation and the Prevention of Cardiovascular Disease. A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2007. [Google Scholar]
- 10. Ferket BS, van Kempen BJ, Heeringa J, Spronk S, Fleischmann KE, Nijhuis RL, Hofman A, Steyerberg EW, Hunink MG.. Personalized prediction of lifetime benefits with statin therapy for asymptomatic individuals: a modeling study. PLoS Med 2012;9:e1001361.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koller MT, Leening MJ, Wolbers M, Steyerberg EW, Hunink MG, Schoop R, Hofman A, Bucher HC, Psaty BM, Lloyd-Jones DM, Witteman JC.. Development and validation of a coronary risk prediction model for older U.S. and European persons in the Cardiovascular Health Study and the Rotterdam Study. Ann Intern Med 2012;157:389–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hippisley-Cox J, Coupland C, Robson J, Brindle P.. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ 2010;341:c6624.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lloyd-Jones DM, Huffman MD, Karmali KN, Sanghavi DM, Wright JS, Pelser C, Gulati M, Masoudi FA, Goff DC Jr.. Estimating longitudinal risks and benefits from cardiovascular preventive therapies among medicare patients: the million hearts longitudinal ASCVD risk assessment tool: a special report from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2017;69:1617–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP.. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–881. [DOI] [PubMed] [Google Scholar]
- 15. ARIC Atherosclerosis Risk in Communities Study Protocol, Manual 1, General Description and Study Management Bethesda, MD: The National Heart, Lung, and Blood Institute of the National Institutes of Health; 1987.
- 16. Schmermund A, Mohlenkamp S, Stang A, Gronemeyer D, Seibel R, Hirche H, Mann K, Siffert W, Lauterbach K, Siegrist J, Jockel KH, Erbel R.. Assessment of clinically silent atherosclerotic disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: rationale and design of the Heinz Nixdorf RECALL Study. Risk Factors, Evaluation of Coronary Calcium and Lifestyle. Am Heart J 2002;144:212–218. [DOI] [PubMed] [Google Scholar]
- 17. Beulens JW, Monninkhof EM, Verschuren WM, van der Schouw YT, Smit J, Ocke MC, Jansen EH, van Dieren S, Grobbee DE, Peeters PH, Bueno-de-Mesquita HB.. Cohort profile: the EPIC-NL study. Int J Epidemiol 2010;39:1170–1178. [DOI] [PubMed] [Google Scholar]
- 18. Day N, Oakes S, Luben R, Khaw KT, Bingham S, Welch A, Wareham N.. EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer 1999;80: 95–103. [PubMed] [Google Scholar]
- 19. Dorresteijn JA, Kaasenbrood L, Cook NR, van Kruijsdijk RC, van der Graaf Y, Visseren FL, Ridker PM.. How to translate clinical trial results into gain in healthy life expectancy for individual patients. BMJ 2016;352:i1548. [DOI] [PubMed] [Google Scholar]
- 20. Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA Jr.. Risk factors for coronary heart disease in African Americans: the atherosclerosis risk in communities study, 1987-1997. Arch Intern Med 2002;162:2565–2571. [DOI] [PubMed] [Google Scholar]
- 21. Berenson GS, Srinivasan SR, Hunter SM, Nicklas TA, Freedman DS, Shear CL, Webber LS.. Risk factors in early life as predictors of adult heart disease: the Bogalusa Heart Study. Am J Med Sci 1989;298:141–151. [DOI] [PubMed] [Google Scholar]
- 22. Doll R, Peto R, Boreham J, Sutherland I.. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ 2004;328:1519.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Martin SS, Sperling LS, Blaha MJ, Wilson PWF, Gluckman TJ, Blumenthal RS, Stone NJ.. Clinician-patient risk discussion for atherosclerotic cardiovascular disease prevention: importance to implementation of the 2013 ACC/AHA Guidelines. J Am Coll Cardiol 2015;65:1361–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fumo MT, Teeger S, Lang RM, Bednarz J, Sareli P, Murphy MB.. Diurnal blood pressure variation and cardiac mass in American blacks and whites and South African blacks. Am J Hypertens 1992;5:111–116. [DOI] [PubMed] [Google Scholar]
- 25. DeFilippis AP, Young R, McEvoy JW, Michos ED, Sandfort V, Kronmal RA, McClelland RL, Blaha MJ.. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J 2017;38:598–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cook NR, Ridker PM.. Calibration of the pooled cohort equations for atherosclerotic cardiovascular disease: an update . Ann Intern Med 2016;165:786–794. [DOI] [PubMed] [Google Scholar]
- 27. Austin PC, Pencinca MJ, Steyerberg EW.. Predictive accuracy of novel risk factors and markers: a simulation study of the sensitivity of different performance measures for the Cox proportional hazards regression model. Stat Methods Med Res 2017;26:1053–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.