Abstract
Objective
the pandemic of coronavirus disease 2019 (COVID-19), hospitals worldwide are at risk of nosocomial infection. Preoperative identification of COVID-19 in patients who are scheduled to be admitted to the hospital is essential to preventing the collapse of medical facility. In Japan, the preoperative observation and screening tests with the RT-PCR testing for the new coronavirus (SARS-CoV-2) and chest CT scan are recommended for head and neck cancer surgery during the COVID-19 pandemic.
Method
We conducted surveys of the current situation in Japan through the internet.
Results
Chest CT scan was fully performed (90%), but the RT-PCR testing was not adequately performed (51%).
Conclusion
Although the current screening system can be considered effective to a certain extent, we recommend further widespread use of pre-admission RT-PCR testing not only for patients with head and neck cancer surgery but also for all the hospitalized patients, in order to promote safer treatments, during the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Head and neck cancer, RT-PCR, Chest CT scan
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) began in Wuhan, China, in December 2019, and has since spread exponentially, resulting in a worldwide outbreak. On January 30, 2020, the World Health Organization (WHO) declared COVID-19 a public health emergency of international concern [1], and on March 11, the WHO declared COVID-19 to be a pandemic [2]. Given the high risk of exposure and infection from aerosol and droplet contamination of the new coronavirus (SARS-CoV-2), the current COVID-19 pandemic presents a significant occupational hazard for physicians and other health care workers who perform and participate in examinations and procedures within the head and neck region and airway [3], [4], [5], [6], [7], [8], [9], [10], [11].
During the COVID-19 pandemic, full personal protective equipment (full PPE: N95 respirator and face shield or powered air-purifying respirator, disposable cap and gown, gloves) is required for any otolaryngology patient with unknown, suspected, or positive COVID-19 status. Elective procedures should be postponed indefinitely, and clinical practice should be limited to patients with urgent or emergent needs, such as tracheotomy [3,10,12]. However, appropriate preoperative screening tests for COVID-19 is currently not sufficiently established.
On the other hand, in Japan, for non-waiting surgery such as head and neck cancer surgery, ``the Guide to Treating Patients with Head and Neck Tumors'' from the Oto-Rhino-Laryngological Society of Japan (2020/04/07 edition) recommends surgical treatments with the choice of intraoperative standard or full PPE based on conditions such as reverse transcriptase-polymerase chain reaction (RT-PCR) testing for SARS-CoV-2, 2 weeks of staying at home before surgery, chest computed tomography (CT) scan, and the presence or absence of intraoperative tracheotomy (Table 1 ).
Table 1.
 |
(www.jibika.or.jp/members/information/info_corona_0409_01.pdf)
This is because the preoperative observation and screening tests, including RT-PCR testing and chest CT scan, are considered essential to preventing perioperative cluster infection of SARS-CoV-2 in the perioperative period and to avoiding wastage of medical resources.
In addition, there have been some reports on guidelines for the management of patients with COVID-19, but few reports have evaluated the preoperative screening with RT-PCR testing and chest CT scan [3], [4], [5], [6], [7], [8], [9], [10], [11]. Therefore, we conducted questionnaire surveys of head and neck cancer specialists in Japan, to determine whether the preoperative screening system for head and neck cancer surgery is widespread and utilized.
2. Materials and methods
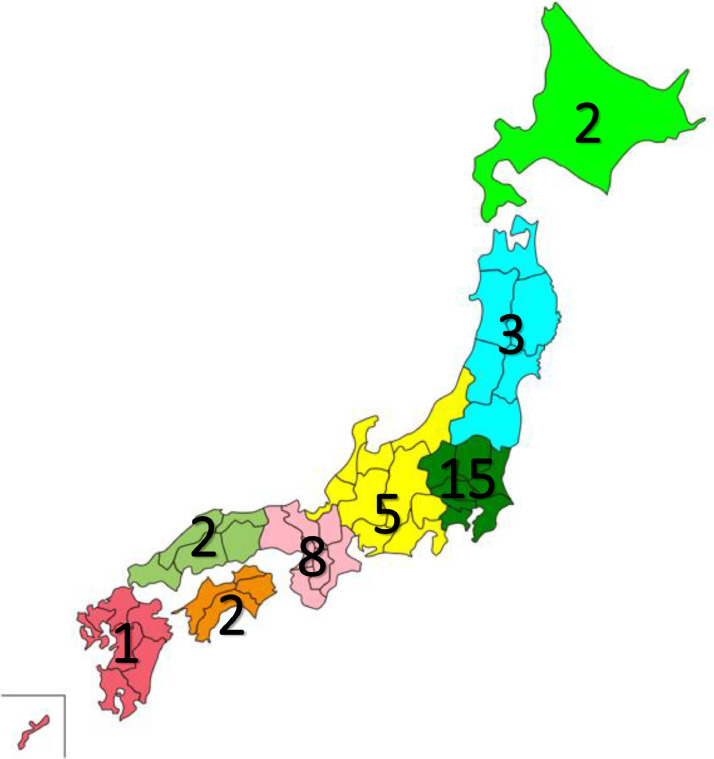
The questionnaires (Table 2 ) were twice administered to head and neck cancer specialists affiliated with so-called high-volume cancer centers, such as university hospitals and regional cancer centers in Japan through the internet: Survey #1 on Apr 17, 2020, Survey #2 on Apr 24, 2020. The total number of respondents was 38. The regional distribution is shown in Fig. 1 .
Table 2.
The questionnaires about preoperative direction and screening tests for COVID-19.
| Q1. Do you perform the surgery in accordance with the Guide to Treating Patients with Head and Neck Tumors (2020/04/07 edition)? |
| Q2. Do you perform the preoperative RT-PCR testing? |
| Q3. Do you perform the preoperative chest CT scan? |
| Q4. Do you ask your patients to stay at home for two weeks before surgery? |
| Q5. Does your hospital offer the same preoperative screening system in other departments as your department? |
| Q6. Do you think RT-PCR testing is necessary as the preoperative screening test?(at Survey #2 only) |
Fig. 1.
The regional distribution in Japan for the surveys. The number in each region indicates the amount of people who responded to the surveys. n = 38, Hokkaido area, 2; Tohoku area, 3; Kanto area, 15; Chubu area, 5; Kinki area, 8; Chugoku area, 2; Shikoku area, 2; Kyushu area, 1.
3. Results
The results of the surveys (Table 3 ) are presented as follows:
Table 3.
The results of questionnaires.
 |
``Q1. Do you perform the surgery in accordance with the Guide to Treating Patients with Head and Neck Tumors (2020/04/07 edition)?''
In the survey #1, the guide had already penetrated many facilities (79%), and in the survey #2, most facilities (92%) have adopted it. These data suggest that the importance of this guide has been well recognized throughout many head and neck cancer specialists in Japan, since the introduction.
“Q2. Do you perform the preoperative RT-PCR testing?”
Although the adoption rate of RT-PCR testing had increased from 38% to 51%, it had not yet been fully implemented. This may be due to the low capacity of the RT-PCR testing in each institution and the delay in the introduction the RT-PCR testing at the administrative level in Japan. As a result, the number of RT-PCR testing that can be performed as a preoperative test could be limited in Japan.
``Q3. Do you perform the preoperative chest CT scan?''
The chest CT scan had already been performed in many facilities since the survey #1.
This could reflect the current situation in Japan, where the preoperative RT-PCR testing is difficult to introduce at the survey #1, nevertheless chest CT scan is not always recommended as a preoperative test for COVID-19 in low-prevalence (<10%) countries [11,13].
``Q4. Do you ask your patients to stay at home for two weeks before surgery?''
The staying at home had penetrated nearly 90% of facilities by the survey #2.
This could be likely boosted by the fact that just prior to the survey #2, the nationwide state of emergency in Japan was declared on April 16, 2020.
``Q5. Does your hospital offer the same preoperative screening system in other departments as your department?''
In Japan, there was sufficient penetration in the department of otolaryngology, but hospital-wide recognition of such procedures is still inadequate. Leaving this situation untreated is dangerous and will not only lead to the depletion of medical resources, but may also lead to the withdrawal of medical personnel and the collapse of medical care.
``Q6. Do you think RT-PCR testing is necessary as the preoperative screening test?''
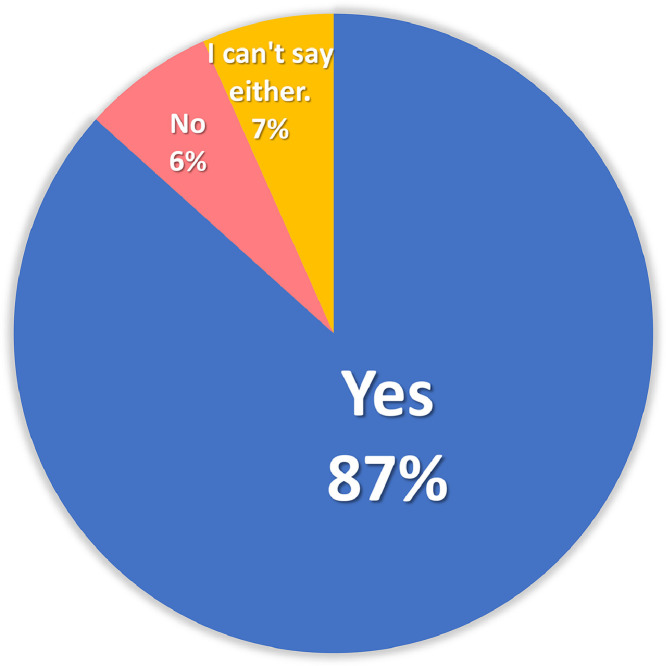
Preoperative identification of COVID-19 in patients who scheduled to be admitted to the hospital could be essential to preventing the collapse of medical facility. Most physicians (87%) felt the need for the RT-PCR testing, as expected (Fig. 2 ). On the other hand, the fact that some physicians do not feel the need to do so may reflect regional differences in the prevalence of COVID-19 in Japan.
Fig. 2.
The results of questionnaire #6 “Do you think RT-PCR testing is necessary as the preoperative screening test?”.
4. Discussion
The RT-PCR testing has been deemed the ``gold standard'' for clinical diagnosis of COVID-19 but takes hours to perform and requires specialized reagents, equipment, and training [14]. In a recent meta-analysis, the pooled sensitivity of RT-PCR was 89% (95% CI: 81%, 94%). In low-prevalence (<10%) countries, the positive predictive value of RT-PCR ranged from 47.3% to 84.3% [13]. Thus, the RT-PCR testing is not perfect as a screening test. On the other hand, chest CT scan for the primary screening or diagnosis of COVID-19 would not be beneficial in a low-prevalence region due to the substantial rate of false-positives [11,13].
This screening system in Japan is a flexible guide that combines observation of clinical symptoms, including 2 weeks of staying at home, with chest CT scan and takes into account the inability to perform the RT-PCR testing.
Consequently, this screening system can help us to prevent intraoperative infection even without the RT-PCR testing, which could lead to the depletion of medical resources, such as full PPE. Thus, it is best to perform the RT-PCR testing as frequently as possible.
Interestingly, the positive rate of RT-PCR testing in the present surveys was zero (data not shown). The results suggest that all the facilities in Japan were able to avoid nosocomial infection in advance and to conserve medical resources during such difficult times of COVID-19 pandemic by generally following the guide shown in Table 1.
The currently universal RT-PCR testing is performed via a swab from the nasopharyngeal mucosa. Saliva could be also a reliable tool to detect SARS-CoV-2 with RT-PCR testing [15]. Considering the burden and simplicity of specimen ingestion to patients, it is desirable to establish and disseminate RT-PCR testing by saliva ingestion in the nearest future.
Moreover, simple and rapid detection methods of SARS-CoV-2, including the reverse transcription-loop-mediated isothermal amplification (RT-LAMP) method, has been rapidly developed all over the world [14]. We hope that these methods will be introduced as soon as possible.
On the other hand, COVID-19 IgM/IgG Rapid Test has not yet been recommended for triage of patients with suspected COVID-19 [16]. If the accuracy is improved in the future, it will be valuable as a preoperative test.
Finally, we would like to recommend that during the COVID-19 pandemic, in order to prevent medical disruption due to hospital-acquired infections of SARS-CoV-2, the screening system, including RT-PCR testing, is firstly mandatory for all patients requiring inpatient cares, not just surgical treatments. Furthermore, the development and introduction of simple and rapid methods to identify SARS-CoV-2 is also an urgent issue.
5. Conclusion
The preoperative screening system for head and neck cancer surgery in Japan is effective to prevent medical disruption caused by the COVID-19 pandemic and should be applied to all the hospitalized patients. For this purpose, it is urgent to increase the capacity of RT-PCR testing in Japan during the COVID-19 pandemic.
Acknowledgements
We would like to acknowledge all the physicians for completing the surveys.
Declaration of Competing Interest
None.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) outbreak. https://www.who.int/westernpacific/emergencies/covid-19. Accessed March 27, 2020.
- 2.World Health Organization. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed April 8, 2020.
- 3.Bann D.V., Patel V.A., Saadi R., Gniady J.P., Goyal N., McGinn J.D. Impact of coronavirus (COVID-19) on otolaryngologic surgery: brief commentary. Head Neck. 2020 Apr 9 doi: 10.1002/hed.26162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coimbra R., Edwards S., Kurihara H., Bass G.A., Balogh Z.J., Tilsed J. European society of trauma and emergency surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020 Apr 17 doi: 10.1007/s00068-020-01364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crossley J., Clark C., Brody F., Maxwell J.H. Surgical considerations for an awake tracheotomy during the COVID-19 pandemic. J Laparoendosc Adv Surg Tech A. 2020 Apr 20 doi: 10.1089/lap.2020.0239. [DOI] [PubMed] [Google Scholar]
- 6.Day A.T., Sher D.J., Lee R.C., Truelson J.M., Myers L.L., Sumer B.D. Head and neck oncology during the COVID-19 pandemic: reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105 doi: 10.1016/j.oraloncology.2020.104684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Givi B., Schiff B.A., Chinn S.B., Clayburgh D., Iyer N.G., Jalisi S. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020 Mar 31 doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 8.Kowalski L.P., Sanabria A., Ridge J.A., Ng W.T., de Bree R., Rinaldo A. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020 Apr 9 doi: 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saadi R.A., Bann D.V., Patel V.A., Goldenberg D., May J., Isildak H. A Commentary on safety precautions for otologic surgery during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020 Apr 14 doi: 10.1177/0194599820919741. 194599820919741. [DOI] [PubMed] [Google Scholar]
- 10.Topf M.C., Shenson J.A., Holsinger F.C., Wald S.H., Cianfichi L.J., Rosenthal E.L. A framework for prioritizing head and neck surgery during the COVID-19 pandemic. Head Neck. 2020 Apr 16 doi: 10.1002/hed.26184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubin G.D., Ryerson C.J., Haramati L.B., Sverzellati N., Kanne J.P., Raoof S., et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Chest. 2020 Apr 7. pii: S0012-3692(20)30673-5. doi: 10.1016/j.chest.2020.04.003. [DOI] [PMC free article] [PubMed]
- 12.Hiramatsu M., Nishio N., Ozaki M., Shindo Y., Suzuki K., Yamamoto T. Anesthetic and surgical management of tracheostomy in a patient with COVID-19. Auris Nasus Larynx. 2020 Apr 18 doi: 10.1016/j.anl.2020.04.002. pii: S0385-8146(20)30082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim H., Hong H., Yoon S.H. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020 doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esbin M.N., Whitney O.N., Chong S., Maurer A., Darzacq X., Tjian R. Overcoming the bottleneck to widespread testing: a rapid review of nucleic acid testing approaches for COVID-19 detection. RNA. 2020 May 1 doi: 10.1261/rna.076232.120. pii: rna.076232.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azzi L., Carcano G., Gianfagna F., Grossi P., Gasperina D.D., Genoni A. Saliva is a reliable tool to detect SARS-CoV-2. J Infect. 2020 Apr 14 doi: 10.1016/j.jinf.2020.04.005. pii: S0163-4453(20)30213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cassaniti I., Novazzi F., Giardina F., Salinaro F., Sachs M., Perlini S. Performance of VivaDiag COVID-19 IgM/IgG rapid test is inadequate for diagnosis of COVID-19 in acute patients referring to emergency room department. J Med Virol. 2020 Mar 30 doi: 10.1002/jmv.25800. [DOI] [PMC free article] [PubMed] [Google Scholar]