Letter:
Telemedicine, or telehealth, is the distribution of information and services via telecommunication and electronic information technologies. This approach to medicine enables long-distance patient and clinician contact, reminders, education, care, intervention, monitoring, and remote admissions.1 , 2 Though not a novel concept, the role of telehealth has grown with the advent of wireless Internet. In recent years, there has been an increased number of studies evaluating telemedicine use and its incorporation in patient care.3 However, surgical specialties have been seemingly less willing to incorporate aspects of telehealth into their practice. To date, there exist only 2 reports of telehealth adoption in neurosurgery.4 , 5 In addition, our department previously performed a pilot study evaluating a telehealth application for spine surgery perioperative care, with expanded utilization planned in the future.6 Nevertheless, there remains relatively minor use of this technology throughout medical fields. This is likely contributable to a number of factors including an unclear or unidentifiable need and logistical issues, such as reimbursement, interstate licensure, accessibility of technology, liability, and patient confidentiality.2
Amidst the COVID-19 pandemic, our department recognized an urgent need to care for patients in a manner safe for both patients and health care providers. Because neurologic issues are often nonemergent, but also rarely elective, each upcoming appointment was reviewed and scheduled in 1 of 3 categories: on-site evaluation (emergent decline representing a likely need for admission), acceptable for telehealth, or acceptable to be delayed for after the COVID-19 outbreak (i.e., patient with 20 years of stable back pain). This communication intends to discuss 1 institutional experience of rapidly implementing a telehealth workflow, from scheduling through the end of the clinical visit, with a preliminary report of patient volumes since the COVID-19 pandemic began. The approach was to take the recipe for an ambulatory visit and break it down to the most essential ingredients, in an effort to streamline telehealth visits and eliminate any unnecessary components of their in-person predecessors.
Scheduling
The department uses BlueJeans (BlueJeans Network, San Jose, California, USA) as its platform for providing telehealth services, primarily due to a university-wide licensing of this software. Patients, providers, and ancillary staff have widely regarded BlueJeans in a positive light for clinical communications.
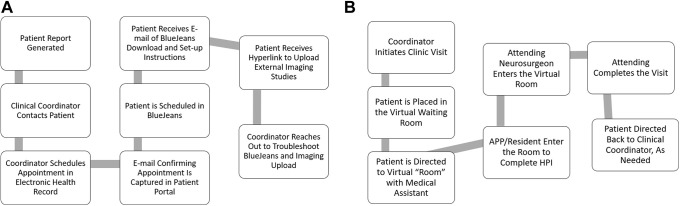
Scheduling for telehealth appointments begins by gathering reports on patients who were due to have appointments in the coming weeks (Figure 1A ). The patient is then contacted and scheduled, in the electronic health record, by the clinical coordinator. An e-mail confirming the appointment is captured in the patient portal. Subsequently, the patient is scheduled in the BlueJeans software and provided with specific instructions via e-mail on how to download and set up BlueJeans. In addition, patients are sent a hyperlink to upload outside imaging, which is retrieved by the coordinator using Life Image Referral Box (Life Image, Newton, Massachusetts, USA). Once received, the imaging is incorporated into the electronic health record and accessible to the provider in a manner similar to a typical ambulatory visit. When appointments are scheduled in BlueJeans, they are assigned a discrete appointment identification number to maximize patient security and confidentiality. The coordinator then follows up with the patient to troubleshoot any issues with either BlueJeans or image uploading, in order to assure the clinic visit is streamlined on the scheduled appointment day.
Figure 1.
Workflow for newly developed telehealth clinic. (A) Scheduling workflow. (B) Clinic visit workflow. APP, advanced practice provider; HPI, history of present illness.
Clinic Visit
For the majority of practices in the department, the clinical coordinator is the first point of contact on the day of the clinic visit. The coordinator prepares the patient via telephone and, again, assures that all technologic concerns are addressed, at which time the patient is placed in the virtual waiting room. The coordinator joins the patient in the virtual waiting room to confirm successful placement. When the advanced practice provider (APP)/resident is ready, the patient is directed to the virtual “room” with the medical assistant, similarly to a conventional clinic. Once all data are captured and films are visualized in the system, the APP/resident then “enters” the virtual clinic room to complete the history of present illness (HPI). At this time the coordinator leaves the virtual room and calls the next patient in line. If that patient is not available, the next patient is contacted. When the APP/resident has completed his or her portion of the evaluation, the telemedicine attending neurosurgeon then “enters.” The attending will examine the patient, further assess the HPI, and then screen share and describe the radiology findings as the patient observes and discusses. In addition, the attending will place orders and discuss the treatment plan. Attendings are then tasked with triaging patients to the following categories: 1) emergency surgery—plan direct admission to avoid emergency department exposure, 2) need for elective surgery—post-COVID full shutdown, 3) conservative management, and 4) no surgery needed at this time. Further need for follow-up or intervention is discussed with the patient, and after all questions from the patient are addressed, the visit is completed. The patient is then directed back to the clinical coordinator, as needed, to schedule any additional care (see Figure 1B). Given the virtual nature of the visit, the clinicians, coordinators, and patients are all in disparate locations, thus eliminating any risk of virus transmission.
Implementation Data
The institutional experience described herein demonstrates the feasibility of rapidly incorporating telehealth into neurosurgical ambulatory practices. Feedback regarding the implementation of telehealth has been resoundingly positive, though some difficulties have been encountered. These include initial setup for first-time telemedicine users, acclimating providers and staff to the new clinic workflow, as well as ensuring that care was not inadvertently limited to those with better access to technology. For patients without access to videoconferencing capabilities, encounters were conducted by telephone to make sure that urgent clinical issues were not missed. For patients who only had access to a smartphone or tablet, we encountered barriers to the physical examination including inadequate lighting and incomplete cranial nerve testing (e.g., extraocular movements). Video conferencing by computer offered better lighting and field of view for physical examination. Patients using only a smart phone found it more challenging to review the images with the attending clinician, and in these cases the attending clinician spent more time zooming in to areas of pathology for the patient. Some patients declined to use the technology and would only do a telephonic visit after submitting images to the department. These evaluations were certainly more limited; however, this cohort represented <3% of the total clinic population.
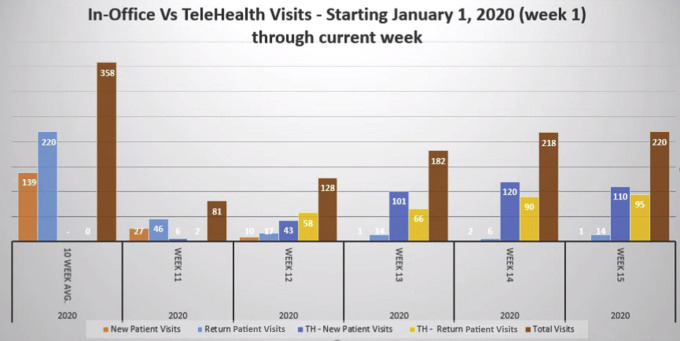
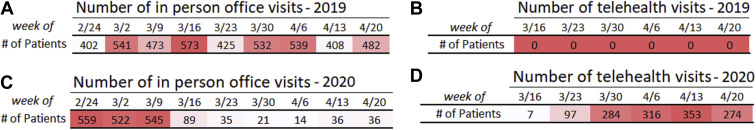
An initial period of refinement was necessary before arriving at the current workflow described earlier, but to this point it has proven both efficient and effective, with fairly seamless implementation. In the 10 weeks leading up to the COVID-19 outbreak, before any restrictions regarding in-person visits, the department averaged 139 new patient visits and 220 return patient visits per week (Figure 2 ), with 0 telemedicine visits conducted during that time. The number of in-person visits sharply declined immediately after the onset of COVID-19−related policies. However, during the fifth week after telehealth implementation, the department recorded 111 new patient visits, 110 (99%) of which were conducted via telehealth. Return patient visits followed a similar trend, although the total number of return patient visits has not rebounded in as robust a manner as new patient visits, with 109 total return visits recorded (95 telemedicine, 14 in person). One year before the COVID-19 outbreak, during this same portion of the year, there were no telehealth visits, as this is an entirely new process in our department (Figure 3 ).
Figure 2.
New and return patient visit data: in person versus telehealth (TH).
Figure 3.
(A–D) Telehealth and in-person visit summary for 2019 and 2020.
Telehealth certainly has inherent limitations. Some neurosurgical visits and pathology inherently lend themselves to more straightforward assessment by telehealth including routine postoperative checks, vascular pathology, and incidentally discovered benign, brain tumors. Other pathologies, such as peripheral nerve conditions, tend to have more subtle findings on physical examination, which are more difficult to assess remotely. Another challenge of telehealth is the reliance of a patient's technologic sophistication and availability. Despite its limitations, we have seen a number of benefits of telehealth. Patient wait times in the BlueJeans virtual waiting room have been averaging 8 minutes. Because efficiency has improved, overall visit length has become shorter, which has improved both patient and surgeon satisfaction. Further, given the efficiencies that telehealth has created, as well as an overall reduction in new patient visit requests during COVID-19, patient lag time, previously 50% of patients waiting more than 2 weeks for an appointment, has been eliminated for all clinicians. Further, additional time can be dedicated toward ensuring that patients have a more thorough understanding of their condition. This is augmented by the screen share function, which allows the attending neurosurgeon to show the patient the exact same images he or she is reviewing, and to highlight salient radiographic features with the highlight cursor function. Furthermore, the video platform enables patients to be “examined” from the comfort of their own home, a setting that may be perceived as less intimidating, in turn making them feel comfortable enough to ask additional questions. Press Ganey and institution-specific satisfaction surveys are included in all telehealth clinical encounters, which our department intends to study moving forward. Future data acquisition will be targeted toward evaluating outcomes for patients seen via telehealth. However, it is to be expected that, at a minimum, telehealth is better for patients than no access to neurosurgical care.
Conclusion
Before the COVID-19 pandemic, utilization of telehealth in neurosurgery remained scarce. This communication detailed how 1 department was able to effectively and quickly pivot its ambulatory practice to a safe telehealth alternative. Telehealth presents a viable option to continue treating patients during the pandemic and offers numerous benefits for both patients and providers, which may be carried over into the post−COVID-19 period.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Ryu S. Telemedicine: opportunities and developments in member states: report on the Second Global Survey on eHealth 2009 (Global Observatory for eHealth Series, Volume 2) Healthcare Inform Res. 2012;18:153. [Google Scholar]
- 2.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 3.Balas E.A., Jaffrey F., Kuperman G.J. Electronic communication with patients. Evaluation of distance medicine technology. JAMA. 1997;278:152–159. [PubMed] [Google Scholar]
- 4.James H.E. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr. 2016;25:753–757. doi: 10.3171/2016.6.PEDS16202. [DOI] [PubMed] [Google Scholar]
- 5.Davis L.E., Coleman J., Harnar J., King M.K. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed JE Health. 2014;20:473–477. doi: 10.1089/tmj.2013.0217. [DOI] [PubMed] [Google Scholar]
- 6.Glauser G., Ali Z.S., Gardiner D. Assessing the utility of an IoS application in the perioperative care of spine surgery patients: the NeuroPath Pilot Study. mHealth. 2019;24:40. doi: 10.21037/mhealth.2019.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]