To the Editor,
We have read the article by Indini et al [1] with great interest. The current health crisis owing to the coronavirus disease-2019 (COVID-19) outbreak represents a serious challenge for cancer patient management. Furthermore, in Italy a high proportion of patients travel from one region to another for healthcare, increasing the risk of spreading the virus [2].
A crucial point is optimizing cancer treatment and diagnostic procedures on a patient-by-patient basis, taking into account the risk of COVID-19 infection risk to avoid negatively impacting patient outcome [3].
One of the most interesting aspect not well focused by the survey is the management of patients with bone metastases (BMs). This aspect may not immediately appear to be a priority in an organizational model, but patients with BM are known to be very fragile and at risk of skeletal complications defined as skeletal-related events (SREs) [4].
During this pandemic, we must first and foremost be more vigilant than ever to the symptoms reported by patients with BMs. This is particularly the case for spinal cord compression (SCC), which requires rapid diagnosis and treatment to minimise neurologic complications.
In this scenario, a multidisciplinary approach is useful because it permits a more accurate identification of SRE risk, avoiding unnecessary medical visits, orienting patients towards the right procedure/treatment, reducing contact with healthcare operators and consequently lowering the risk of COVID-19 contamination even if the multidisciplinary meeting seems to be contraindicated [5].
The first dilemma is how we can reduce the outpatient visits number, try to have multidisciplinary meetings between physician whilst also guaranteeing the same therapeutic and diagnostic quality and continuity of care. Furthermore another issue is the time-saving and to not increasing the work of health operators committed to face the COVID-19 and at the same time to manage adequately patient needs.
In the last years, the use of technologies to support and promote long distance clinical care, education, and health administration is exploded and can helping this particular situation [6].
In the present emergency, we have developed different strategies for cancer patients, in particular those with BMs:
-
1.
A dedicated patient triage software has been developed that enables operators to identify: area of origin, presence of symptoms and contact with COVID-19 infected cases. All patients are monitored closely by nurses by phone contact, and if a Covid-19 symptom was suspected, the National procedures are activated.
-
2.
Clinical activities have been reduced and tele-consultations are carried out when appropriate. In particular, multidisciplinary tele-consultation for bone metastatic patients took place weekly in this period. The specialists involved have been as follows: oncologist, radiologist, nuclear medicine specialist, orthopaedic surgeon, rehabilitation specialist and radiotherapist.
-
3.
Assess bone instability and ensure the proper orthesis to prevent complications such as pathological fractures
-
4.
Treatment regimens have been adapted.
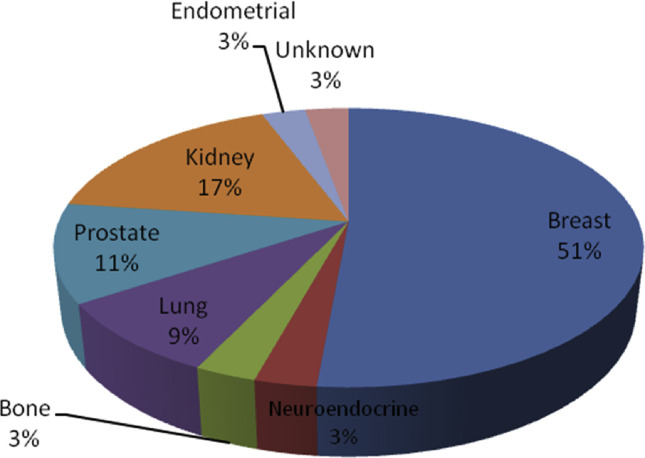
This approach seems to be not feasible or realistic, and owing to these reasons, we briefly report our experience from 9th of March to 17th of April. More than 3348 patients were screened with our software. Of those with a diagnosis of BM from different primitive tumors (Fig. 1 ), 37 from several geographic areas underwent multidisciplinary tele-consultations to evaluate the risk of SREs (Table 1 ). Thirteen patients (35.1%) reported bone pain. In 8 of 13 patients use (61.5%) opioids, 3 of 13 (23.1%) use paracetamol and 2 of 13(15.4%) use a combination of opioids and corticosteroids. A total of 15 SREs were found: 12 (80%) pathological fractures, 2 (13.3%) SCC and in one patient (0.7%) both. Interestingly, of 26 patients with indication of BM at high risk of SREs, 10 (38.5%) have no risk and 4 (36.3%) of 11 patients were sent to multidisciplinary consultation for other reasons who have high risk of complications. De-escalating regimens [7,8] for bone-targeted agents were adopted, with a total of 170 (70% of zoledronic acid and 30% of denosumab) delays. Up to 17th April, none of the healthcare operators and only one of the 37 patients had tested positive for COVID-19.
Fig. 1.
Primitive cite of bone metastases.
Table 1.
Main characteristics of patients with BM managed with multidisciplinary tele-consultations.
| Patients' characteristics | No. (%) |
|---|---|
| Median age, year | 66 |
| Distance from the center (km) | |
| 0-50 | 26 (70,2) |
| 51-250 | 8 (21.6) |
| >250r | 7 (8.1) |
| Indication for multidisciplinary consultationa | |
| First diagnosis of BM | 11 (29.7) |
| Evaluation of SREs risk in patients with BM | 26 (70.3) |
| Bone lesions to be characterized | 2 (5.4) |
| Severe bone pain | 13 (35.1) |
| Interventions | |
| Orthesis prescribed | 18 (48.6) |
| Zoledronic acid | 17 (45.9) |
| Denosumab | 8 (21.6) |
| Surgery indication | 1 (2.7) |
| Radiotherapy | 4 (10.8) |
| Biopsy | |
SREs, skeletal-related events.
The same patient may have more than one indication.
In conclusion, patients with BM are susceptible to frequent complications, and a multidisciplinary approach has proven highly effective in dealing with them. However, in the present COVID-19 emergency, greater emphasis is needed on risk assessment, prevention strategies and effective therapies to optimise oncologic resources and to guarantee the patients’ continuum of care. We believe our experience could provide a feasible model of care to manage patients with BMs and at the same time prevent and reduce COVID-19 infection.
Conflict of interest statement
The authors declare that they do not have any potential conflict of interest.
References
- 1.Indini A., Aschele C., Cavanna L., Clerico M., Daniele B., Fiorentini G. Grossi F Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur J Canc. 2020 Apr 6;132:17–23. doi: 10.1016/j.ejca.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 2.Rosenbaum L. Facing covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic's front line. N Engl J Med. 2020 doi: 10.1056/NEJMp2005492. [published online ahead of print, 2020 Mar 18] [DOI] [PubMed] [Google Scholar]
- 3.van de Haar J., Hoes L.R., Coles C.E., Seamon K., Fröhling S., Jäger D. Caring for patients with cancer in the COVID-19 era. Nat Med. 2020;26:665–671. doi: 10.1038/s41591-020-0874-8. [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim T., Flamini E., Fabbri L., Serra P., Mercatali L., Ricci R. Multidisciplinary approach to the treatment of bone metastases: osteo-Oncology Center, a new organizational model. Tumori. 2009;95:291–297. doi: 10.1177/030089160909500304. [DOI] [PubMed] [Google Scholar]
- 5.Bongiovanni A., Recine F., Fausti V., Foca F., Casadei R., Falasconi M.C. Ten-year experience of the multidisciplinary osteoncology center. Support Care Canc. 2019;27:3395–3402. doi: 10.1007/s00520-019-4635-5. [DOI] [PubMed] [Google Scholar]
- 6.Hollander J.E., Carr B. Virtually perfect? telemedicine for covid-19. NEJM. March 11 2020 doi: 10.1056/NEJMp2003539. [Perspective] [DOI] [PubMed] [Google Scholar]
- 7.Amadori D., Aglietta M., Alessi B., Gianni L., Ibrahim T., Farina G. Efficacy and safety of 12-weekly versus 4-weekly zoledronic acid for prolonged treatment of patients with bone metastases from breast cancer (ZOOM): a phase 3, open-label, randomised, non-inferiority trial. Lancet Oncol. 2013 Jun;14(7):663–670. doi: 10.1016/S1470-2045(13)70174-8. [DOI] [PubMed] [Google Scholar]
- 8.Liu C., Wang L., Liu L., Zhuang J., Tang S., Zhang T. Efficacy and safety of de-escalation bone- modifying agents for cancer patients with bone metastases: a systematic review and meta-analysis. Canc Manag Res. 2018 Sep 21;10:3809–3823. doi: 10.2147/CMAR.S176811. [DOI] [PMC free article] [PubMed] [Google Scholar]