Abstract
Background
In Italy, the spread of the COVID-19 pandemic has stressed the entire healthcare system and required a huge re-organization of many Divisions, including those of Gastroenterology.
Aims
to assess the impact of COVID-19 pandemic on Gastroenterology Divisions across Italy.
Methods
All members of the Italian Society of Gastroenterology (SIGE) were invited to answer a web-based survey.
Results
Data of 121 hospitals from all 20 Italian regions were analyzed. Overall, 10.7% Gastroenterology Divisions have been converted to Covid Units. Outpatients consultations, endoscopic and ultrasound procedures were limited to urgencies and oncology indications in 85.1%, 96.2% and 72.2% of Units, respectively, and 46.7% of them suspended the screening for colorectal cancer.
Moreover, 72.2% of the staff received a training for use of personal protective equipment, although 45.5% did not have sufficient devices for adequate replacement. Overall, 132 healthcare workers in 41 Gastroenterology Divisions were found to be infected.
Conclusion
This is the first study to evaluate, at a country level, the impact of COVID-19 outbreak on Gastroenterology Divisions. Substantial changes of practice and reduction of procedures have been recorded in the entire country. The long-term impact of such modifications is difficult to estimate but potentially very risky for many digestive diseases.
Keywords: SARS-CoV-2, COVID-19, Pandemic, Gastroenterology, Impact, Survey
1. Introduction
The outbreak of COVID-19, initially developed in China since early December 2019, has rapidly spread to other countries and represents a public health emergency of international concern [1]. On March 11th 2020, the World Health Organization, declared the coronavirus disease 2019 (COVID-19) to be pandemic [2].
At the end of February 2020, the first cases of infections were registered in Italy, progressively spreading throughout the country in a total of 215,858 cumulative confirmed cases and 29,958 death cases registered as of May 7th 2020, so that Italy is currently the third country by number of deaths in the world [3].
The SARS-CoV-2 is characterized by a high infectivity potential trough a human-to-human transmission that occurs primarily via direct contact or air droplets [4].
The COVID-19 generally occurs with fever, cough, asthenia and diarrhea. About half of the patients experience more severe symptomatology with worsening dyspnea and a minority of them develop acute respiratory distress syndrome (ARDS) with an estimated mortality of 3.5% [5,6].
Due to the high virulence of the pathogen and the severity of the disease, the spread of the infection had a significant impact on the Italian healthcare system, as already happened in other countries.
Although the Gastroenterology (GI) Divisions are not primarily involved in the management of COVID-19 patients, many of them underwent a drastic and rapid rearrangement.
Some of them have been converted to COVID Units to deal with the emergency, and many physicians, trainees and nurses were involved in the management of COVID-19 patients. Moreover, several Divisions were forced to reduce the routine workload to prevent the infection spreading, with consequent quantitative and qualitative impairment of the health services provided and potential consequences for patients. Finally, specific, rigorous safety procedures were adopted to maintain some clinical activities unsuited to be postponed. To date, however, a comprehensive picture of the characteristics and effects of the re-organization of Gastroenterology facilities due to the COVID-19 pandemic is not available.
Thus, our aim was to assess the main changes that have occurred in the Italian GI Divisions following the COVID-19 pandemic through a web-based 39-point questionnaire.
2. Materials and methods
2.1. Study design and development of the survey questionnaire
This is a web-based survey designed to assess the impact of COVID-19 pandemic on Gastroenterology Divisions in Italy.
The working group which formulated the survey was composed by six members of the Italian Society of Gastroenterology (SIGE), nominated by the SIGE Steering committee.
A 39-point multiple-choice questionnaire was designed by the working group during videoconference meetings.
The survey questions aimed to address the main changes that have occurred in the Italian Gastroenterology Divisions following the COVID-19 pandemic, including: 1) quantitative and qualitative changes in the provision of health services (ordinary hospital stay, outpatient activities, ultrasound [US] and endoscopic procedures); 2) application of containment measures, with a specific focus on personal protective equipment (PPE) used by healthcare personnel to avoid the spread of the infection within the hospitals and other measures to limit the contagion in the home environment; 3) the psychophysical stress in the medical staff due to the emergency.
2.2. Distribution of questionnaire and collection of data
After approval by all components of the working group and SIGE steering committee, the final version of the questionnaire was viewed via Google Forms.
The link to access the survey was sent via email, together with a brief explanation of the project (the full version of the questionnaire is available as Supplementary File), to all SIGE members from all 20 regions of Italy. A first invitation was sent to all members, followed by a subsequent reminder after a few days.
When possible, data from at least one physician from each regional hospital were collected in order to obtain a comprehensive picture of the national territory.
Two different sets of data were separately analyzed: 1) an analysis set including responses from 121 Divisions was used to evaluate all questions addressing the impact of the pandemic on GI healthcare activities, 2) an analysis set that included responses from 266 GI physicians was used to analyze only the personal and psychophysical questions.
Ethical committee approval was not required for this type of survey. All subjects accepted to participate in the interview through informed consent for the collection, handling and storage of data, which was included in the presentation of the questionnaire. Data collection took place during the peak of the pandemic in Italy between March 30th and April 7h 2020.
2.3. Statistical analysis
Continuous variables were reported as mean ± standard deviation, and categoric variables were summarized as frequency and percentage. Independent-samples t-test and χ2 test were used for comparison of continuous and categorical variables, respectively.
All statistical analyses were performed using SPSS v. 25.0 for Macintosh (SPSS Inc., Chicago, USA).
3. Results
3.1. General information and demographic data
Overall, 266/742 (35.8%) of invited physicians completed the survey, and data from 121/194 (62.4%) invited hospitals were included in the analysis.
59/121 (48.8%) of the hospitals were from northern, 18/121 (14.9%) from central and 44/121 (36.3%) from southern Italy (Fig. 1 ).
Fig. 1.
Map of participant regions and cities.
The most affected areas of northern Italy (Lombardia, Veneto, Piemonte and Emilia-Romagna) were adequately represented, being 39.7% of the total responding Divisions.
Half of the centres (50.4%) were non-academic public hospitals, while the others were academic (33.9%) or private hospitals (15.7%).
3.2. Impact of the pandemic on specialist healthcare activities
3.2.1. Clinical activities
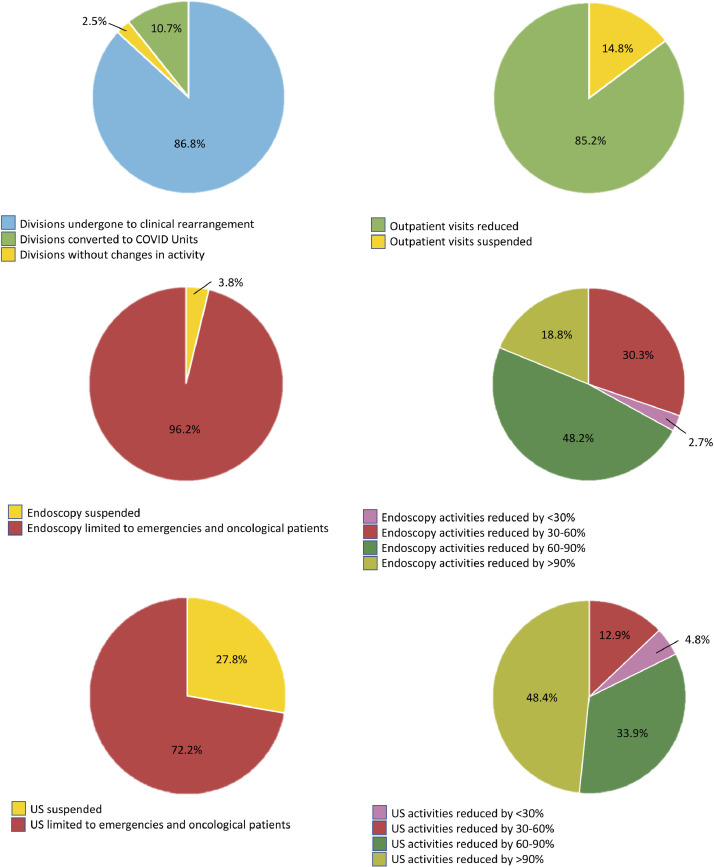
Only 3/121 (2.5%) GI Divisions have continued the same activity carried out before the pandemic, while 118/121 (86.8%) have undergone a clinical rearrangement, and 13/121 (10.7%) have been converted to COVID Units.
Through the country, outpatient activity has suffered a sharp slowdown. In 103/121 (85.1%) GI Divisions, hospital admissions and outpatient consultations have been reduced to the management of clinical emergencies, gastrointestinal oncological diseases and chronic therapies (such as infusions of biological drugs in patients with inflammatory bowel disease - IBD), while in 18/121 (14.9%) outpatient activities have been completely suspended.
To deal with this load of outpatients in charge, 83/121 (68.6%) Divisions activated a remote consultancy service (63.9% by phone, 31.3% by email, 4.8% by video) in order to guarantee the ordinary follow-up.
3.2.2. US and endoscopic services
As a consequence of COVID-19 pandemic, instrumental activities also suffered a strong slowdown.
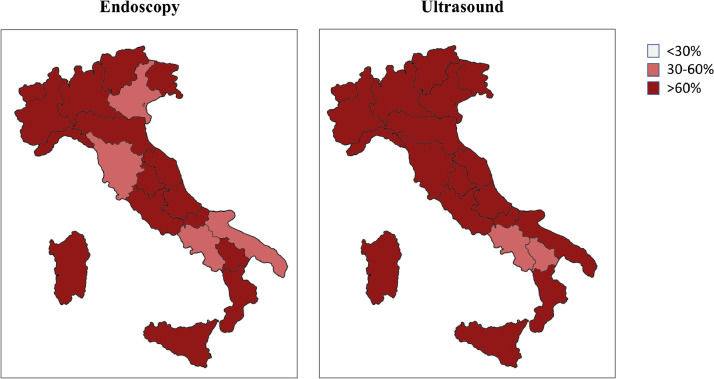
Among 105/121 Divisions with endoscopy Units (86.8% of the participants), 4/105 (3.8%) suspended all the procedures, while all the others limited the procedures to emergencies and oncological indications. Moreover, 66.7% of Units continuing endoscopy activities underwent a >60% reduction of the ordinary volume of procedures performed (Figs. 2 , 3 ). In addition, 49/105 (46.7%) Units suspended the endoscopic screening program for colorectal cancer (CRC).
Fig. 2.
Reduction of the ordinary volume of procedures performed in Gastroenterology Divisions among Italian regions.
Fig. 3.
Main changes occurred in the Italian Gastroenterology Divisions following the COVID-19 pandemic.
Among 72/121 Divisions with US services (59.5% of the participants), 20/72 (27.8%) suspended their activities and the others 52/72 (72.2%) limited the procedures to emergencies and oncological patients. Among the US services continuing the activities, 83.9% reduced >60% the ordinary volume of procedures performed (Figs. 2, 3).
When assessed by COVID-19 prevalence areas, the number of Units undergoing a >60% reduction of instrumental procedures, did not differ between high and low COVID-19 prevalence areas neither for endoscopy (64.4% vs 68.7%, p=0.6) nor for ultrasound (84.6% vs 80.6%, p=0.6) Units (Table 1 ). On the contrary, the suspension of CRC screening program was less common in high-prevalence compared to low prevalence areas (37.8% vs 53.4%, p=0.1) (Table 1).
Table 1.
Main differences between geographic areas of high and low COVID-19 prevalence.
| High COVID-19 prevalence areas(N° of Units = 48) | Low COVID-19 prevalence areas(N° of Units = 73) | p | |
|---|---|---|---|
| Reduction of outpatient consultations (%) | 87.5 | 83.6 | 0.5 |
| Severe (> 60%) reduction of endoscopic procedures (%) | 64.4% | 68.7% | 0.6 |
| Suspension of endoscopic screening for CRC | 37.8% | 53.4% | 0.1 |
| Severe (> 60%) reduction of ultrasound procedures (%) | 84.6% | 80.6% | 0.6 |
| Availability of protocols for the management of patients with suspected or confirmed SARS-CoV-2 infection (%) | 97.9% | 89.0% | 0.07 |
| Level of stress perceived by physicians (mean ± SD) | 6.8 ± 1.4 | 6.7 ± 2.0 | 0.7 |
| Level of stress perceived by physicians’ families (mean ± SD) | 7.4 ± 1.8 | 6.8 ± 2.3 | 0.1 |
Abbreviations: CRC: colorectal cancer; COVID-19: coronavirus disease 2019; SD: standard deviation.
3.3. Protocols for management of patients inside the hospital
In 108/121 (89.2%) of GI Divisions, outpatients underwent a specific triage or stratification of the risk of exposure or infection before entering the division. In 55.7% of them, the body temperature was measured, in 85.9% patients had to wear face masks and gloves, and in almost all cases the patient's stay in the waiting room was limited and access for accompanying persons was prohibited.
Finally, 112/121 (92.6%) GI Divisions issued and followed a specific protocol for the management of patients with suspected or confirmed SARS-CoV-2 infection, in the absence of significant differences between high and low-prevalence areas (97.9% vs 89.0%, p=0.07) (Table 1).
3.4. Protocols for individual protection of the medical staff
With regard to PPE availability, N95/FFP2-3 masks were available in 91/121 (75.2%), surgical masks in 115/121 (95.0%), gloves in 117/121 (96.7%), disposable gowns in 100/121 (82.6%), hairnets in 104/121 (85.9%), goggles in 78/121 (64.5%) and boots in 57/121 (47.1%) of Divisions (Table 2 ).
Table 2.
Availability of personal protective equipment in Gastroenterology divisions.
| Type of personal protective equipment (PPE) | Units with PPE available |
|---|---|
| N95/FFP2-3 masks | 75.2% |
| Surgical masks | 95.0% |
| Gloves | 96.7% |
| Disposable gown | 82.6% |
| Hairnet | 85.9% |
| Goggles | 64.5% |
| Boots | 47.1% |
Nevertheless, only 54.5% of participants receive a sufficient quantity of PPE for disposable replacement.
During endoscopic procedures, 83.4% of participants adhered to specific guidelines for PPE management and dressing modalities suggested by international recommendations [7]. Nevertheless, 43.2% of them adhered to the recommendations only if the patient had a confirmed SARS-CoV-2 infection. As a possible explanation of this finding, only 75.2% of the medical staff interviewed received a training on the correct use of PPE and 45.5% still don't have sufficient availability of all PPE to meet the recommendations.
A regular intensive sanitization of the workplace was performed in 117/121 (96.7%) Divisions, but in 41.9% of them only after the access of patients with suspected or confirmed SARS-SoV-2 infection.
Overall, in 41/121 GI Divisions (33.9%) there was at least one healthcare professional who got infected, in a total of 132 subjects, of which 121/132 from Divisions not-converted to COVID Units and 75/132 from high-prevalence areas.
In 56/121 (46.3%) hospitals, the exposed personnel undergo a nasopharyngeal swab to rule out infection only if symptomatic.
3.5. Psychophysical impact on healthcare personnel
In this section, we separately analyzed individual responses of the 266 physicians interviewed to assess the psychophysical impact of the COVID-19 pandemic on medical staff.
When physicians were asked if they felt confident to work in the current conditions of personal protection, the average score was 5.5 ± 2.2 (minimum confidence 0, maximum confidence 10), while the perceived risk of being infected was 5.6 ± 2.1 (minimum risk 0, maximum risk 10).
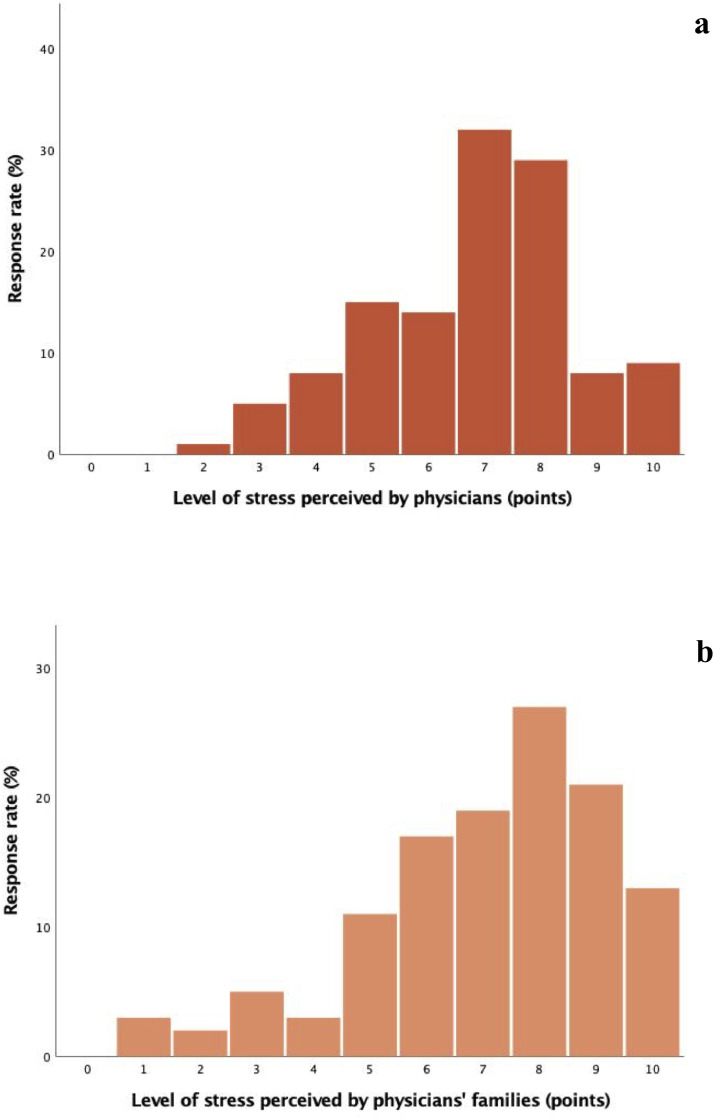
The level of stress perceived by the physicians since the outbreak was 6.8 ± 1.8 (minimum stress score 0, maximum stress score 10) (Fig. 4 a).
Fig. 4.
Level of stress perceived by the physicians (a) and the physicians’ families (b) since the COVID-19 outbreak.
Occupational exposure also produced consequences in the family environment of the medical staff. The families of the interviewed physicians perceived an average degree of stress of 7.1 ± 2.1 (minimum stress score 0, maximum stress score 10) (Fig. 4b). Besides, 254/266 (95.5%) participants changed their family habits: 40/254 (15.8%) moved away from their family home and changed residence, 56/254 (22.0%) remained in their home but separated the living spaces from the other family members, and 158/254 (62.2%) have maintained their previous home and living spaces, but have intensified personal hygiene and social distancing.
No difference between higher and lower prevalence areas was found in the personnel stress score (6.8±1.4 vs 6.7±2.0, p=0.7) as well as in the family stress score (7.4±1.8 vs 6.8±2.3, p=0.1) (Table 1). As expected, a significantly higher level of stress was registered between physicians working in divisions converted to COVID Units and those working in not-converted Units (7.8 ± 1.6 vs 6.7 ± 1.8, p=0.2).
4. Discussion
This large web-based national survey provides a comprehensive picture of the impact of COVID-19 outbreak on GI Divisions in Italy. The answers from 121 GI Divisions from all Italian regions showed that Gastroenterology activities underwent drastic and profound changes throughout the country.
Although urgent services were guaranteed across the territory, all ordinary health care services have been significantly reduced.
Hospital admission for urgency or oncology patients as well as outpatients consultations for oncology patients and for diseases or therapies that require close monitoring, such as biological therapies for IBD, were regularly maintained in most of the hospitals surveyed.
However, all ordinary outpatient activities, including the diagnosis and follow-up of non-urgent conditions, have been temporarily shelved. In several hospitals, telemedicine services have been activated to allow patients to communicate with doctors and to exchange information, such as sending laboratory reports and receiving prescriptions.
Similarly, all endoscopic activities have been reduced. Endoscopy may represent a source of aerosolization with a greater risk of contagion compared to other clinical activities in Gastroenterology. As a matter of fact, the endoscopy staff is at increased risk of infection by COVID-19 from inhalation of airborne droplets, conjunctival contact, and feces contamination [8,9]. In addition, recent evidence shows that SARS-CoV-2 may be still present in sputum and feces even after negative swab results [10]. For this reason, international recommendations on dressing and use of PPE have been recently issued [7,11,12].
Although urgent endoscopic procedures are regularly performed in many hospitals, non-urgent and follow-up tests have been reduced or even suspended. Similar results were recorded for ultrasounds, although the procedure presents a lower risk of contagion.
Contrary to expectations, no significant difference in the reduction of activity was found between areas of higher and lower COVID-19 incidence, strongly suggesting that these changes do not depend exclusively on the incidence of the infection, but rather on the adaptation of the entire health service to the emergency.
This collapse of scheduled non-urgent consultations and/or procedures could lead to significant consequences.
First, it could result in a clinical risk for patients. Even if consultations may be maintained through alternative telemedicine strategies, not performed procedures have no surrogates. This is the case of endoscopic screening of colorectal cancer, that significantly impacts on the prognosis of patients [13] and that has been suspended in nearly half of endoscopic Divisions.
Secondly, it will certainly lead to a large overload of rescheduled procedures difficult to manage when the pandemic will be over, including recommended endoscopy for post-polypectomy surveillance, surveillance of dysplasia in IBD, or ultrasound for HCC surveillance [14], [15], [16], [17], [18].
In confirmation of these findings, 85.6% of the participants judge this reduction in specialist healthcare worrying and hard to manage in the near future.
Along with this, the survey aimed to analyze the current application of prevention measures and the management of PPE during the current pandemic. We found a profound difference between the attitudes of the different GI Divisions, in particular on the presence or absence of defined protocols to be followed, adequate training of the personnel, together with the supply of PPE.
For instance, all Divisions should activate a triage and all patients admitted after triage should wear adequate protection. Similarly, all physicians need PPE in sufficient quantities for exposures and training on adequate dressing.
This need is confirmed by the worrying data of 132 healthcare workers infected across the GI Divisions in Italy. Nevertheless, these data should be interpreted cautiously, as they do not strictly reflect the effective rate of infected healthcare workers in each hospital. The evaluation of the incidence and risk factors of SARS-CoV-2 infection among healthcare personnel is not the aim of this survey and needs to be better assessed by further studies.
Finally, as recommended by regulatory authorities, most hospitals provide a nasopharyngeal swab only to exposed staff members who are symptomatic.
Nevertheless, with increasing availability of resources, this strategy needs to be revised with the aim to contain the infection in Gastroenterology Divisions where the exposed asymptomatic personnel continue to get in touch with other patients, in the absence of a diagnosis.
5. Conclusions
The advent of the COVID-19 pandemic has led to necessary and profound but also largely heterogeneous changes among Gastroenterology activities in Italy.
This is the first study to evaluate, at a country level, the impact and the burden of COVID-19 outbreak on Gastroenterology Divisions. Substantial changes of practice and reduction of procedures have been recorded in the entire country regardless of the local incidence of infection. The long-term impact of such modifications is difficult to estimate but potentially very risky for many digestive diseases and a large part of the Italian population.
Our findings call for an urgent initiative to overcome the shortcomings, improve and homogenize the behaviour of all GI Divisions in the national territory.
All of them must adapt quickly to the global emergency, adopting proper protocols for the management of patients, whether they are suspect or infected with SARS-CoV-2, and providing all healthcare personnel with the appropriate PPE as well as proper training. Given the heavy workload and the amount of stress, we also believe that psychological support should be offered to medical staff, especially those of the GI Divisions converted to COVID Units, in order to take care of their psychophysical health and to preserve the quality of their work.
On the other hand, given the reduction in outpatient activities, alternative health care strategies are needed. In this regard, telemedicine tools provide valuable help, but they must be used with caution due to their limitations.
Besides, in Units where it has been suspended, endoscopic screening of CRC screening should be resumed to avoid the possible long-term consequences deriving from its interruption.
In the meantime, all Divisions should make a wise re-organization plan to sustain the burden of not performed and rescheduled healthcare services. This will represent a new challenge to face at the end of the pandemic, a challenge which the National Health system should be prepared in advance to take on, to avoid further stressing the available resources. In that context, scientific societies will have a paramount role in driving the appropriate actions of GI Divisions to re-establish activities after the COVID-19 pandemic.
Acknowledgments
Conflict of interest
The authors have no proprietary, financial, professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of this manuscript.
Funding
None.
Author contributions
Maida M and Ianiro G are guarantors of the integrity of the entire study and contributed to the manuscript drafting and manuscript revision for important intellectual content; Maida M, Ianiro G, Repici A, Sferrazza S, Savarino E and Fuccio L contributed to the manuscript editing. All authors had full control over the preparation of the manuscript.
Acknowledgements
SIGE steering committee: Alvaro Domenico, Annibale Bruno, Benedetti Antonio, Burra Patrizia, Ianiro Gianluca, Marchi Santino, Morisco Filomena, Repici Alessandro, Ricciardiello Luigi, Savarino Edoardo Vincenzo.
Participant regions and cities: Abruzzo (Chieti, L'Aquila, Teramo), Basilicata (Matera), Calabria (Catanzaro, Cosenza), Campania (Napoli, Salerno, Caserta, Nocera Inferiore, Mercato San Severino, Acerra), Emilia-Romagna (Bologna, Forlì, Imola, Piacenza, Reggio Emilia, Ravenna, Modena, Carpi), FriuliVeneziaGiulia (Trieste, Aviano), Lazio (Roma, Latina), Liguria (Genova, Sanremo, Pietra Ligure, La Spezia, Lavagna), Lombardia (Milano, Rozzano, Rho, Monza, Bergamo, Osio Sotto, Brescia, Como, Pavia, San Donato Milanese), Marche (Ancona, Macerata, Senigallia), Molise (Campobasso, Termoli), Piemonte (Torino, Vercelli, Alessandria, Asti, Alba, Novara, Orbassano, Candiolo, Chivasso), Puglia (Bari, Lecce, Andria, Barletta, Castellana Grotte, Cerignola), Sardegna (Cagliari, Oristano, Nuoro, Olbia), Sicilia (Palermo, Catania, Messina, Caltanissetta, Agrigento, Trapani, Siracusa, Ragusa, Cefalù, Gela, Niscemi), Toscana (Firenze, Arezzo, Empoli, Pisa), TrentinoAlto Adige (Trento, Rovereto), Umbria (Perugia, Terni), Val d'Aosta (Aosta), Veneto (Padova, Verona, Treviso, San Donà di Piave, Santorso, San Bonifacio, Montebelluna, Negrar di Valpolicella, Camposampiero).
Interactive map of participant cities: https://www.click2map.com/v2/mmaida/Italia_survey.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dld.2020.05.017.
Appendix. Supplementary materials
REFERENCES
- 1.World Health Organization. Coronavirus disease (COVID-19) outbreak. https://www.who.int(Accessed April 2th 2020)
- 2.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-COVID-19—11-march-2020 (Accessed April 2th 2020)
- 3.Johns Hopkins University. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html(Accessed May 7th 2020)
- 4.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry B.M., Vikse J. Clinical Characteristics of COVID-19 in China. N Engl J Med. 2020 Mar 27;382 doi: 10.1056/NEJMc2005203. pii: 10.1056/NEJMc2005203#sa4. [DOI] [PubMed] [Google Scholar]
- 6.Chan Jasper F.W., Yuan S.F., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person to-person transmission: a study of a family cluster. Lancet. 2020 doi: 10.1016/S0140-6736(20)30154-9. https://doi. org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Update 1 (18.03.2020). https://www.esge.com/esge-and-esgena-position-statement-on-gastrointestinal-endoscopy-and-the-COVID-19-pandemic/(Accessed April 2th 2020). [DOI] [PMC free article] [PubMed]
- 8.Wu C., Chen X., Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 Mar 13 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young B.E., Ong S.W.X., Kalimuddin S. Singapore 2019 Novel Coronavirus Outbreak Research Team. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020 doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen C., Gao G., Xu Y. SARS-CoV-2–Positive Sputum and Feces After Conversion of Pharyngeal Samples in Patients With COVID-19. Ann Intern Med. 2020 Mar 30 doi: 10.7326/M20-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Repici A., Maselli R., Colombo M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020 Mar 14 doi: 10.1016/j.gie.2020.03.019. pii: S0016-5107(20)30245-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiu P.W.Y., Ng S.C., Inoue H. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements) Gut. 2020 Apr 2 doi: 10.1136/gutjnl-2020-321185. pii: gutjnl-2020-321185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brenner H., Stock C., Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ. 2014;348:g2467. doi: 10.1136/bmj.g2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hassan C., Quintero E., Dumonceau J.M. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. Oct 2013;45(10):842–851. doi: 10.1055/s-0033-1344548. [DOI] [PubMed] [Google Scholar]
- 15.Rex D.K., Boland C.R., Dominitz J.A. Colorectal cancer screening: recommendations for physicians and patients from the U.S. multi- society task force on colorectal cancer. Gastroenterology. Jul 2017;153(1):307–323. doi: 10.1053/j.gastro.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Annese V., Daperno M., Rutter M.D. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. Dec 2013;7(12):982–1018. doi: 10.1016/j.crohns.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 17.European Association for the Study of the Liver EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. Jul 2018;69(1):182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Marrero J.A., Kulik L.M., Sirlin C.B. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. Aug 2018;68(2):723–750. doi: 10.1002/hep.29913. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.