Abstract
The pandemic diffusion of the SARS-CoV-2 infection throughout the world required measures to prevent and strategies to control the infection, as well as the reallocation of the hospital structures in order to take care of an increased number of infected patients. Endoscopy Units should be able to perform endoscopic procedures on COVID-19 infected as well as on noninfected patients. The aim of this manuscript is to propose a model for a fast reorganization of the endoscopy department environment in order to safely perform endoscopic procedures in this Pandemic COVID-19 scenario, according to the current advices given by the Scientific Societies
Keywords: Endoscopy digestive unit, COVID-19 emergency, Layout redesign, Pathways
1. Background
Early reports of SARS-CoV-2/Novel Coronavirus19 (COVID-19) infection came from China in November 2019 and, due to the rapid diffusion of this infection throughout the world, on March 11th,2020 COVID-19 was classified as Pandemic [1].
According to the current knowledge, the SARS-CoV-2 virus is transmitted between people through close contact and droplets, but evidences exist suggesting a possible transmission through the stools and contaminated surfaces [2], [3], [4], [5]. According to the World Health Organization (WHO), the airborne transmission of COVID 19 is not yet adequately documented, although it is possible during invasive procedures that generate aerosols [2,6,7]. Rational use of personal protective equipment (PPE) could prevent infection among Healthcare Workers (HWs), who are exposed to an increased risk of COVID-19 infections [8,9].
Digestive endoscopy procedures pose a potential risk of infection for HWs due to the potential exposure of HW to the transmission of microbial agents from patients [10].
In this emergency situation related to the SARS-CoV-2 pandemic infection, it was necessary to convert hospitals into dedicated structures to assist and treat COVID-19 patients in order to contain disease spreading, but also to guarantee adequate levels of assistance to other patients. In the current phase of emergency several strategies have been implemented such as postponing elective procedures, using telemedicine (when feasible), limiting points of entry to a facility, implementing source control for everyone entering the facility and screening everyone for COVID-19 symptoms before entering a facility [11]. However, if an endoscopy department has to be prepared to deal simultaneously with both COVID-19 positive and COVID-19 negative patients and to avoid infection transmission, an environment reconversion will be needed.
Additionally, literature data regarding detailed schemes of endoscopy unit environment implementation and/or reallocation for a simultaneous management of both types of patients are limited. The aim of this manuscript is to share our model of fast reconversion of the endoscopy unit, which has been developed according to current scientific evidence and the recommendations of Scientific Societies, in order to safely manage both classes of patients.
2. Summary
In this manuscript we propose a prompt redesign and a new organization of a digestive endoscopy unit to respond to the COVID-19 emergency aimed at minimizing the risk of infection for HWs and/or patients in the endoscopic setting. The workplace should be redesigned and set-up in order to create a risk-based layout, as outlined in the following Key Concepts:
-
1)
Reduce hospital risk infection, minimizing the chance of exposure of patients and HW through the established routes of transmission of SARS-CoV-2, such as droplets, airborne, direct contact with surfaces [2].
-
2)
Ensure immediate identification of patients with confirmed or suspected COVID-19 before accessing the endoscopy unit, in order to isolate them as soon as possible and provide separate pathways.
-
3)
Help the personnel in acquiring specific COVID-19 infection prevention skills, in order to comply with precautions, to improve their adherence to current procedural guidelines while performing the assigned tasks, particularly with respect to PPE usage, and to carefully operate according to the risk of infection of patients.
To meet these needs we had to implement the following changes in our digestive endoscopy unit:
-
1.
Layout modifications, by means of a risk-based color-coding redesign of current spaces: waiting room, recovery room and endoscopy suites.
-
2.
Implementation of new areas: check points, areas for PPE donning and doffing and endoscopy procedure room droplet areas
-
3.
Create separate pathways and processes according to the new color-code design and the new dedicated areas
3. Layout modifications
3.1. Redefinition of the current spaces with working areas with differential color code classification
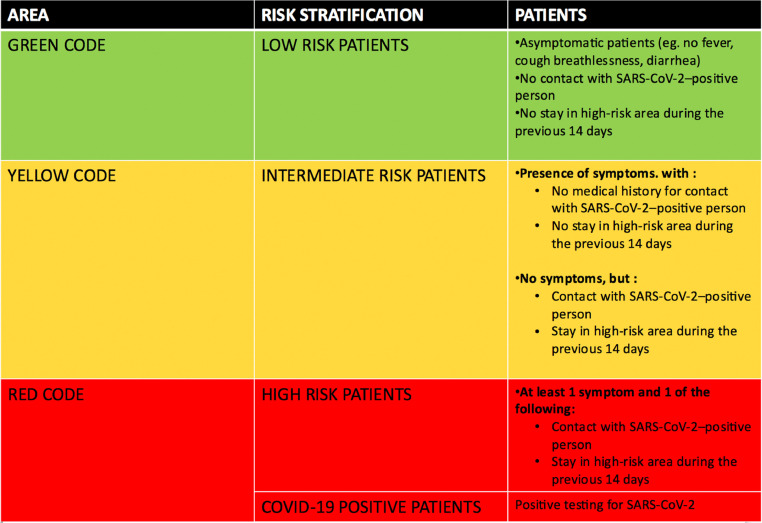
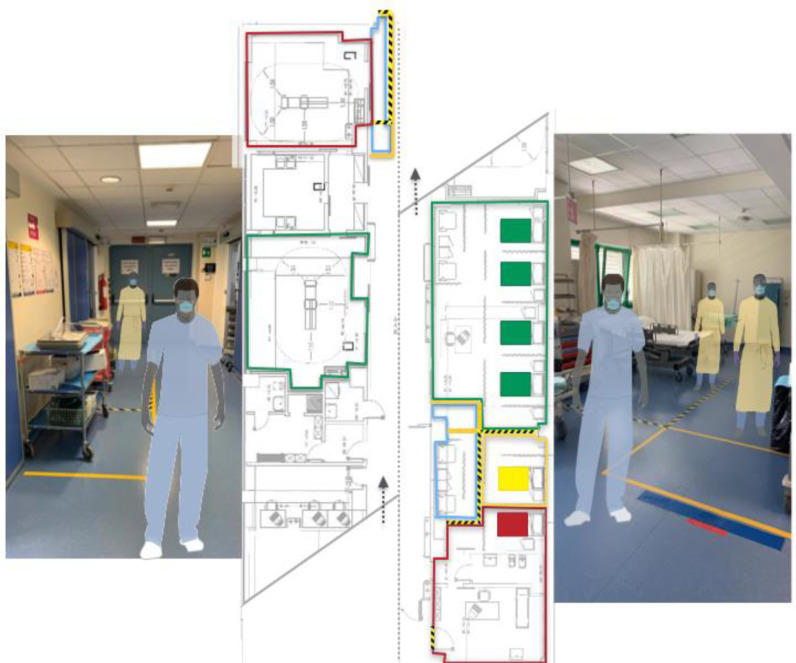
Taking into account the risk classification of COVID-19 patients proposed by Repici et al. [12], the areas in the endoscopy unit have been reclassified by means of a color coding system as “green” for low risk patients, “yellow” for intermediate risk patients and “red” for high-risk or confirmed COVID-19 patients (Fig. 1 ).
Figure 1.
Color code assignation and patients risk stratification according to Repici et al. [12] recommendations.
The color-coding strategy can allow patients and HWs to associate certain colors with specific areas or actions, with the goal to minimize the hazards of cross-contamination. This allows HWs to quickly and easily move around the facility, complete their tasks and find what they are looking for. The color-coding assignment lasts for the whole duration of the patient's visit, from arrival to discharge.
Furthermore, the color-code we adopted refers to the American National Standards Institute (ANSI) and Occupational Safety and Health Administration (OSHA) safety color coding system that all businesses must adhere to, as a safety program requires the implementation of colors that quickly identify and draw attention to potential safety hazards. Red is the most well recognized sign for hazards. Red is also used to highlight areas of specific protective equipment.
Yellow denotes caution. Yellow can be used with black checkers or stripes to draw attention to the hazard. Green is used to signify safe areas of a workplace [13].
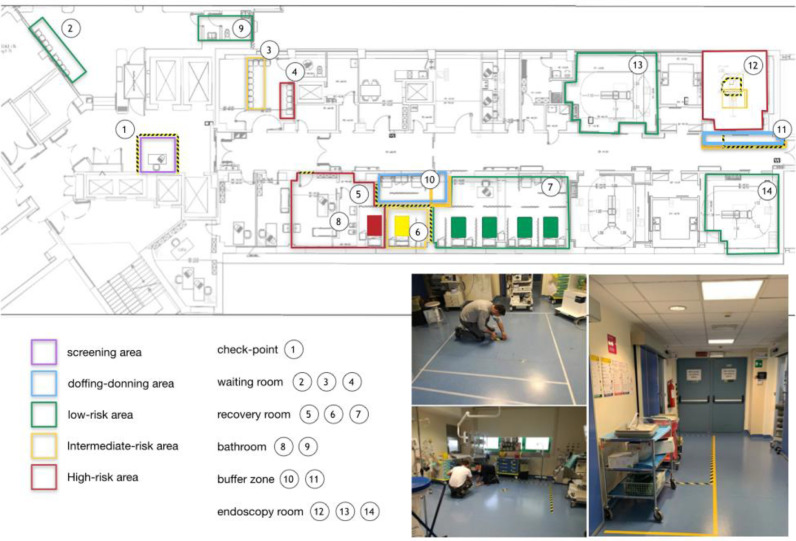
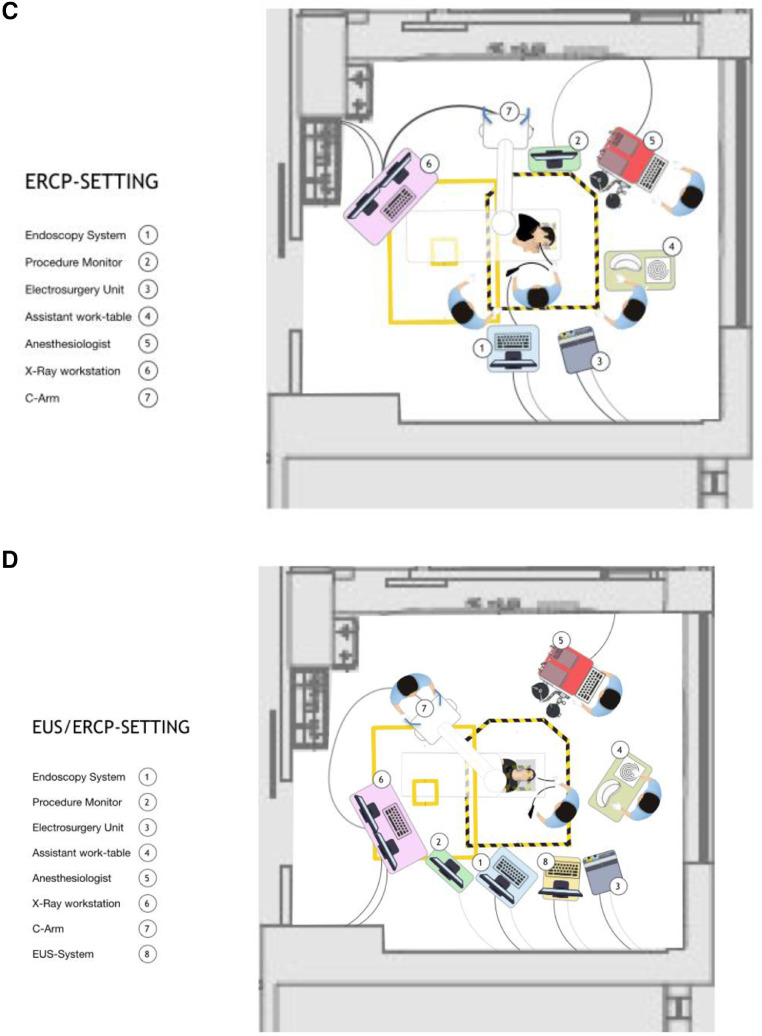
After risk stratification, patients receive a color code based on their COVID-19 risk and are assigned to the respective code-color areas. These include a green waiting room with dedicated bathroom, a green recovery room, two green endoscopic suites for low risk patients, a yellow and a red waiting room and a yellow and a red recovery room with dedicated bathrooms.
By contrast, to avoid too complex tasks for HWs, a single red color code has been assigned to the endoscopic room where intermediate, high risk and COVID-19 patients undergo endoscopic procedures, although a specific and risk based workflow sequence has been defined as strategy protocol, as described below.
A consistent wall and door marking color system has been used to easily allow employees and patients to associate certain colors with certain areas or actions. According to this system (Table 1 , Fig. 2 ), each patient's color has a specific waiting room, recovery room, but also a dedicated bathroom. All spaces are also organized respecting the internal requirements for spatial distance and hygiene rules. Alcohol based hand sanitizer for hand hygiene is available at each entrance and in all common areas.
Table 1.
Color code definition of working areas.
| Waiting room | |
| Green area | Low risk COVID-19 patient |
| Yellow area | Intermediate risk COVID-19 patient |
| Red area | COVID-19 patient confirmed |
| Recovery room | |
| Green area | Low risk COVID-19 patient |
| Yellow area | Intermediate risk COVID-19 patient |
| Red area | COVID-19 patient confirmed |
| Endoscopic rooms | |
| Green area | Low risk COVID-19 patient |
| Red area | COVID-19 patient suspected or confirmed |
Figure 2.
Layout of our endoscopy unit modified in accordance with green, yellow and red areas.
4. Implementation of new areas
4.1. Checkpoint
Outpatients with a planned endoscopic procedure will receive a questionnaire for COVID-19 risk assessment by a phone call from a HW one day before the procedure, as advised by the European Society of Gastrointestinal Endoscopy (ESGE) [11]. Additionally, a checkpoint, serving as a triage station, has been set up outside the entrance of the endoscopic unit with dedicated staff, with the aim of screening patients before they enter the endoscopy facilities. (Fig. 2) The personnel should have a supply of facemasks and tissues for patients with symptoms of respiratory infection and should carry out again a screening questionnaire for COVID-19 risk assessment for all patients and any caregiver. The checkpoint consists of a specific desk delimited by floor marker tape and is equipped with a plastic transparent shield. It is supplied with equipment such as gloves, surgical masks, hydroalcoholic solution and items of disposable stationery. In any case, the external checkpoint must allow adequate contact distance guaranteed by access restriction and specific signs.
Thanks to the screening questionnaire, patients and caregivers (in case of outpatients) are assigned to a COVID-19 risk class (Fig. 1) characterized by a color code (green, yellow, red), which will allow the patient to be allocated to the waiting area corresponding to the color code of his risk class.
Checkpoint staff will hand over the color-coded card to the nurse of the recovery room before allowing patient access to the endoscopy unit. Signs are posted at entrances with instructions to individuals with symptoms of respiratory infection to: immediately put on a mask and keep it on during their assessment, cover their mouth/nose when coughing or sneezing, use and dispose of tissues, and perform hand hygiene after contact with respiratory secretions. Facemasks are provided to coughing patients and other symptomatic individuals upon entry to the facility. Signs are posted in triage areas advising patients with fever or symptoms of respiratory infection to immediately notify triage personnel, so that appropriate precautions can be put in place.
4.2. Areas for PPE donning/doffing
The areas for PPE donning and doffing, as reported in Fig. 2, are “buffer zones” that separate the so-called “clean” and “dirty” spaces. They are located respectively in access areas to the endoscopy room (red room) and to the recovery room section, both dedicated to intermediate, high-risk or confirmed COVID-19 patients (yellow and red recovery room area).
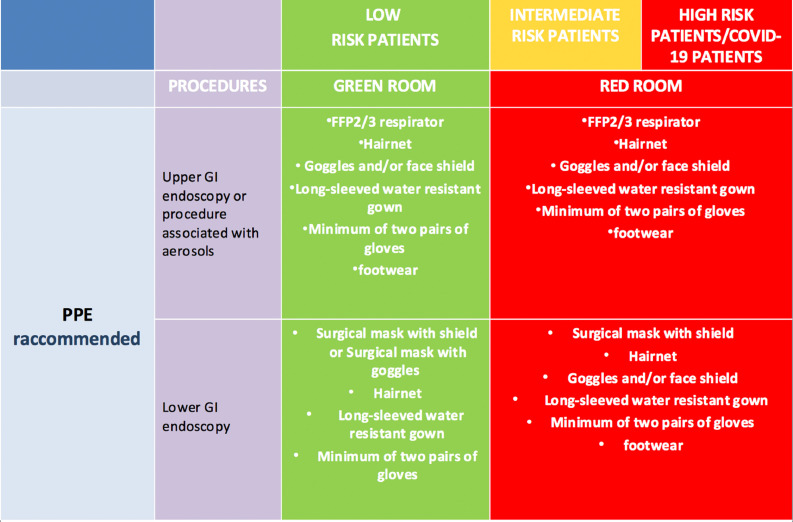
The PPE donning and doffing areas are delimited by means of a floor marking tape and include a space for contaminated waste, a clean area wall support point, a dirty area wall support point, also delimited by markers. The hydroalcoholic solution, the list of devices to wear and the devices themselves are available in an accessible position (Fig. 3 ). Signs are posted in entrances with instruction and sequence for safely donning and doffing specific PPE in accordance with institution procedural regulations and infection exposure risk.
Figure 3.
PPE recommended for HWs based on patient and procedure risk.
4.3. Endoscopy Procedure room droplet areas
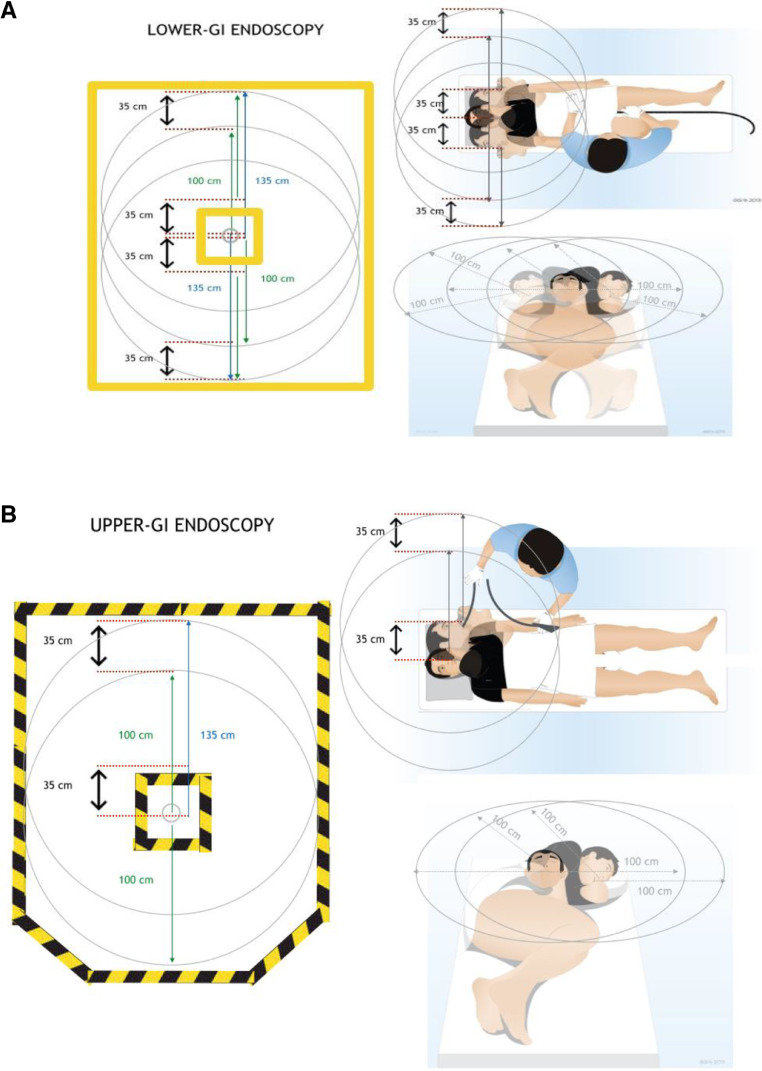
According to our current knowledge, an HW, who operates at less than 1meter distance from a COVID-19 patient, is exposed to a high risk of patient -to-healthcare provider transmission because of droplets exposure [2]. In order to remark this concept, specific markers will be placed inside the endoscopy room using warning tapes to highlight:
-
1.
the positioning of the patient's head on the bed.
-
2.
the “droplet safety distance”
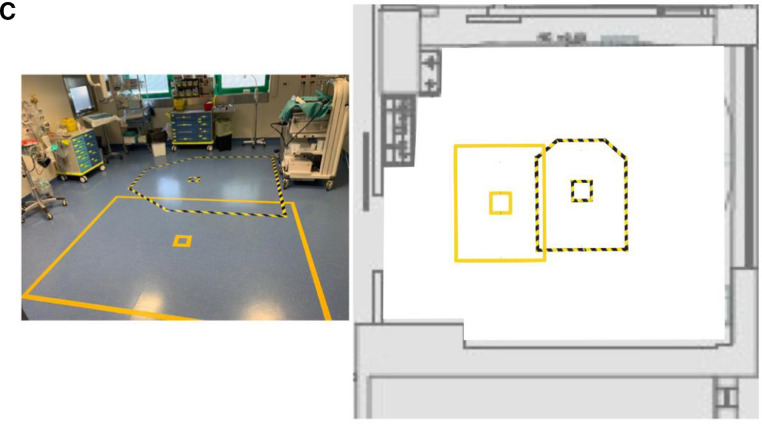
Two different droplet areas have been estimated according to the maximum known distance for large droplet diffusion and the maximum feasible distance for medical instruments during lower and upper gastrointestinal (GI) procedures. Therefore, we have paid attention to the position of the patient's head on the bed, because the head is the source of droplet emission. So, we estimated the possible head excursion (about 35cm) during both the aforementioned procedures; in fact, while in both types of procedure the patient's head could be in left lateral or supine decubitus, during colonoscopy a right lateral decubitus may sometimes be necessary (Fig. 4 A-B).
Figure 4.
(A-B) Calculation of “droplet safety distance” in accordance with the position of the patient's head on the operating table and the possible movements that can be performed during the procedure. (C) Taping with markers of the lower (yellow tape) and upper GI (black/yellow tape) procedures droplet areas.
Figure 4C depicts the floor markings collocation for droplet safety distance and the position of the patient's head in bed, in the two possible scenarios: upper and lower GI endoscopy procedures. Yellow tape marks are for the operating table collocation in case of lower GI, while black & yellow striped tape mark is used in case of upper GI procedures.
The purpose of these markers is to remind the HWs to keep distant from this area when their direct contact with the patient is not needed. These are also helpful in order to adequately position the instrumentation (i.e. Light source, processor) at least out from the droplet area line or, when the procedure allows it, far from the line, in order to minimize the risk of surface contamination.
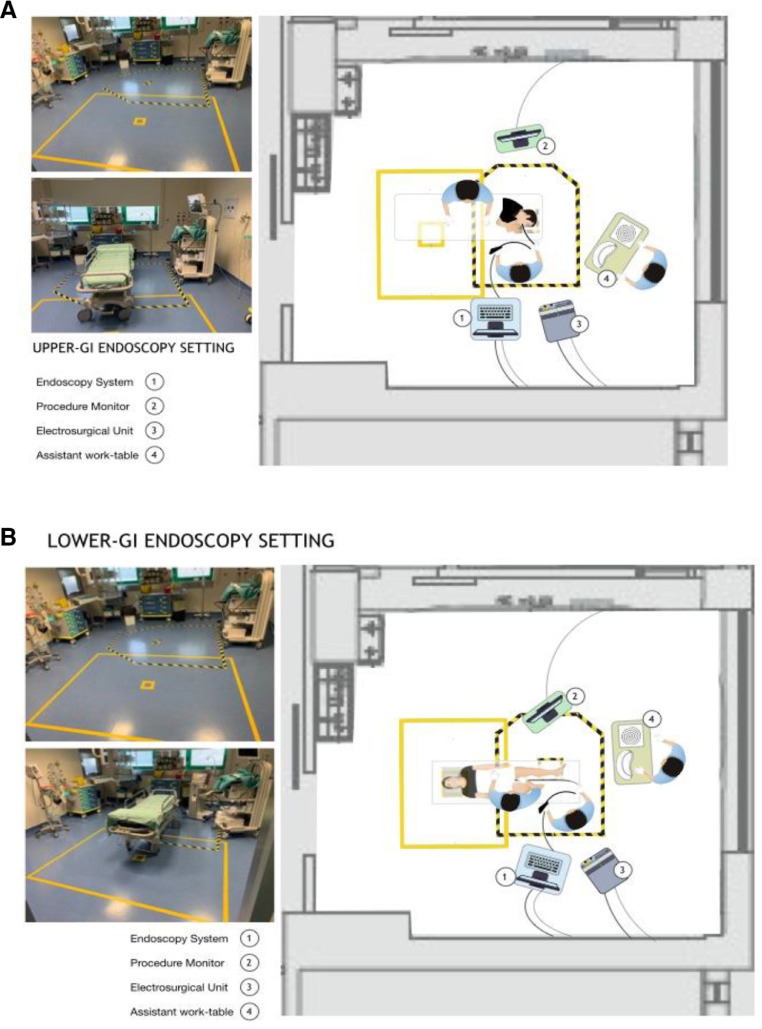
Figures 5 A-D shows how different types of endoscopic equipment should be placed during endoscopic procedures (gastroscopy and colonoscopy, EUS and ERCP).
Figure 5.
(A-D). Different endoscopic equipment positions during procedures (gastroscopy, colonoscopy, ERCP, EUS).
5. Create separate pathways and processes
Thanks to the new color-code design separate and completely independent patient pathways have been defined for suspected or confirmed COVID-19 patients and non-suspected patients.
Key points for directing the patients to pathways and workflow are the following:
-
1)
Keep the social distance required by local health recommendations throughout the duration of the patient's visit, from arrival to discharge.
-
2)
Avoid direct and indirect contacts through environmental surfaces between low risk, intermediate risk, high risk patients and COVID-19 positive patients.
-
3)
Avoid surfaces contact by suspected or confirmed COVID-19 patients in the endoscopy unit.
-
4)
Limit transport and movement in the different endoscopic department areas avoiding unnecessary transit or stay.
Depending on the color-coded risk, patients are placed in the respective waiting areas and called for different pathways as described below. Although there are four risk categories for patients (low risk, intermediate risk, high risk patients and COVID-19 positive patients), this distinction is maintained for waiting areas and recovery rooms, only, in a scheme that matches the risk classes of patients with the procedures risk and adapts the PPE kit to this combination, grouping the operational risk of the activity in endoscopy rooms in only two types, marked by color code (green room: low risk patients; red room: intermediate/high risk and COVID-19 positive patients) (Fig. 3).
5.1. Low risk patients paths
5.1.1. Inpatients
5.1.1.1. Upper and Lower Endoscopic procedures in low risk inpatients
Low risk inpatients access the endoscopy unit with their hospital bed. Depending on room availability, they may be welcomed directly into the green endoscopy room or, alternatively, placed in the recovery room green area. They are then taken to the green endoscopy room to undergo the examination and, once the procedure is completed, they return to the green area and are then discharged, transported with bed.
5.1.2. Outpatients
5.1.2.2. Upper and Lower Endoscopic procedures in low risk outpatients
Low risk outpatients (green area), are called by the check-point staff, enter the corridor of the current preparation area (external to the endoscopic block), wear the usual clothing and shoe covers, and are accompanied to the endoscopy room to perform the examination. If sedation has not been performed, they are then taken directly to the external green area and discharged. If sedation has been carried out, they are taken by stretcher to the green area of the recovery room and then taken out avoiding transit through the red areas
5.2. Intermediate/ high risk patients and COVID-19 positive patients paths
5.2.1. Inpatients
5.2.1.3. Upper and Lower Endoscopic procedures in intermediate/high risk patients (COVID-19 suspected) and COVID-19 positive inpatients
Inpatients at intermediate/high risk (COVID-19 suspected) or with confirmed COVID-19 access the endoscopy unit with their hospital bed, and, whenever possible, depending on red room availability, are transported directly inside the red endoscopic room and, after the procedure, directly transported to their ward, without being temporarily placed in the recovery room. Alternatively, they are previously allocated to the red or yellow area of the recovery room corresponding to their color code, then they are taken to the red room to perform the examination. At the end of the procedure, they are directly transported to their ward or, when further postprocedural patient evaluation and monitoring are needed, return to the red or yellow area of recovery room corresponding to their color code before being returned to their ward.
5.2.2. Outpatients
5.2.2.4. Upper and Lower endoscopy procedures in intermediate/high risk patients (COVID-19 suspected) and COVID-19 positive outpatients
Intermediate/high risk patients (COVID-19 suspected) and COVID-19 positive outpatients are taken to the appropriate yellow/red area in the waiting room. Once called for the examination, they enter the yellow/red area of the recovery room through a dedicated and separated entrance and are prepared by wearing the appropriate gown and shoe covers and placed on a stretcher. Then they are accompanied to the red room to carry out the examination. Both in case of sedation and in case of absence of sedation, after the examination, they are transported on a stretcher to the yellow or red area of the recovery room (depending on the respective color code) and then discharged following the transit route through the aforementioned separated entrance.
Notably, the abovementioned paths allow to avoid, from the arrival and for all the duration of the patient's visit, any potential droplet diffusion or surface contact of suspected or known COVID-19 patient in the endoscopic block and/or in areas other than those assigned to them in respect of their color-code risk classification.
Remarkably, inside the endoscopy unit, all patient's transports directed to the red endoscopic room, for both suspected or confirmed COVID-19 patients, either from the recovery room or the ward, are operated by bed or stretcher, preventing the patients to walk and thus obviating the potential risk of surface contamination.
Transported patients are asked to wear a surgical mask and covered with a clean sheet during transport. A protocol is in place to ensure that, if the patient is being transported outside the room, HWs of the receiving area are notified in advance.
5.3. Endoscopic suite workflow
The room worklist is defined according to risk-based criteria and may be subject to change in relation to the identification of patients at risk of COVID-19 or positive COVID-19 by the checkpoint. Since the risk class determines a sequence of access and specific room allocation, the recovery room manager will be responsible for the assignment of the examinations in the endoscopic unit.
Therefore, the daily worklist, integrated for each patient with a specific color code, will be placed in the recovery room and the flow in the endoscopic rooms will be managed by the recovery room nurse (identified by the nursing coordinator).
5.4. Red room workflow
Intermediate/high risk patients and COVID-19 positive patients undergo endoscopic examinations in the red room suite according to a specific scheduling order based upon the risk classification of patient and procedure.
Although whether endoscopy is an aerosol generating procedure is still debated, our healthcare local institution considered upper GI endoscopies as aerosol-generating procedures; on the other hand, lower GI endoscopy has not been included in the list of procedures in this risk class.
Therefore, a priority access to the red room suite has been defined with the aim of performing procedures in the following order:
-
1)
Lower GI endoscopy for intermediate risk patients
-
2)
Upper GI endoscopy for intermediate risk patients
-
3)
Lower GI endoscopy for high risk patients
-
4)
Upper GI endoscopy for high risk patients
-
5)
Upper GI endoscopy for COVID-19 positive patients
-
6)
Lower GI endoscopy for COVID-19 positive patients
Adequate time and air changes are warranted between different procedures [12].
6. Layout and pathway set-up
Implementation of this practical model of redesign of a digestive disease endoscopy unit during the COVID-19 emergency requires a pre-interventional multidisciplinary meetings to define a specific plan taking into account the current endoscopy unit layout, evaluating the general feasibility and identifying areas and paths.
Furthermore, the contribution of graphic designers and technicians is needed to design and set-up new signals and markers in outdoor areas and in the endoscopic rooms, including signs, infographics, wall and floor color markers, and stickers marking printed or floor marking tapes. Signals are posted on the walls and doors of areas according to the color code to allow an easy recognition.
Table 2 shows the suggested changes and Fig. 6 depicts the new layout of our endoscopy unit.
Table 2.
New signals and markers proposed.
| Signals and markers | |
|---|---|
| Checkpoint | • Sign with “Endoscopy Checkpoint – do not enter: wait for the Health Worker” • Warning tape for safety distance limit from the check point. • Safety distance warning tape between users to avoid crowding of people. |
| Waiting room | • Specific color markings on the available chairs. • Wall sign with area/waiting room color code definition. • Signs with the words “DO NOT SIT” to be affixed on the seats not to be used to guarantee the safety distances as per regulations |
| Endoscopic room hallway | • Warning tape to delimit the dirty/clean filter area. • Wall sign with room color code definition • Wall sign with the name " PPE donning and doffing area " • Signs with standards and instructions on dressing and undressing related to the respective risk class. |
| Recovery room | • Signal tape to delimit the dirty/clean filter area • Wall sign with area color code definition • Wall sign with the name " PPE donning and doffing area " • Signs with standards and dress code and dressing instructions for the respective risk class |
Figure 6.
Layout of our endoscopy unit modified with new signals and markers.
Practically, our department reconversion requested a few markers, tapes and signals, two technicians and two multidisciplinary meetings before the set-up, which, in our experience, took no more than 3 hours.
The use of these signals and markers could avoid mistakes that could lead to the diffusion of the infection in each step of the permanence of both patients and HWs in the endoscopy unit. All workers should learn the codes of each area and be familiar with the system. Indeed, as observed with the use of color code in the industrial environment, a color-coding system increases the safety of employees [14].
7. Conclusions
Our redesigning model of the digestive endoscopy unit is based on the stratification of patient and procedure risks and on the creation of dedicated areas and pathways aimed at minimizing the risk of spread of infection both between HWs and patients but also between different patients.
Despite the work involved, many proponents agree that a concrete and well-organized color-coding system can make any workplace safer and more effective.
Since a color-coding system has been shown to be effective in some industrial environments to identify hazard zones, it could also be useful in the current need for a rapid reorganization of endoscopic departments because of the COVID-19 pandemic. Such a model could contribute to minimizing the risk of contamination and reduce or eliminate wasted time by allowing a fast adherence to new protocols and tasks. Indeed, this operating procedure establishes and identifies the use of colors, signs and signals which should allow for quick recognition of information and hazards in the various work areas. A color code system together with the implementation of new areas and the use of clear visual markers allows a speedy visual search, emphasizes information, shows associations with specific actions and transmits important messages. Furthermore, our method has been shown to be easy to implement, cheap and fast.
Declaration of Competing Interest
All authors disclosed no financial relationships.
References
- 1.Chatterjee P. The 2019 novel coronavirus disease (COVID-19) pandemic: A review of the current evidence. Indian J. Med. Res. mar. 2020;151(2):147–159. doi: 10.4103/ijmr.IJMR_519_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations(Accessed apr. 13, 2020).
- 3.Ong S.W.X. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. mar. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Doremalen N. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. mar. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gu J., Han B., Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology. mar. 2020;158(6):1518–1519. doi: 10.1053/j.gastro.2020.02.054. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125(Accessed apr. 18, 2020).
- 7.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19)(Accessed apr. 19, 2020).
- 8.Wang X., Pan Z., Cheng Z. Association between 2019-nCoV transmission and N95 respirator use. J. Hosp. Infect. mar. 2020;105(1):104–105. doi: 10.1016/j.jhin.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. mar. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnston E.R. Risk of bacterial exposure to the endoscopist's face during endoscopy. Gastrointestinal Endoscopy. apr. 2019;89(4):818–824. doi: 10.1016/j.gie.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 11.ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic – European Society of Gastrointestinal Endoscopy (ESGE). https://www.esge.com/esge-and-esgena-position-statement-on-gastrointestinal-endoscopy-and-the-covid-19-pandemic/(Accessed apr. 13, 2020). [DOI] [PMC free article] [PubMed]
- 12.Repici A. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest. Endosc. mar. 2020;92(1):192–197. doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silently Guiding Safety: American National Standards for Safety Signs and Colors, www.ansi.org.https://www.ansi.org/news_publications/news_story?menuid=7&articleid=724b7e4d-6e66-4a00-af99-6791da1e5018(Accessed apr. 23, 2020).
- 14.NASD - Color Coding. https://nasdonline.org/131/d001678/color-coding.html(Accessed apr. 23, 2020).