Abstract
Objective
The coronavirus disease 2019 (COVID-19) pandemic has had significant economic impact on radiology with markedly decreased imaging case volumes. The purpose of this study was to quantify the imaging volumes during the COVID-19 pandemic across patient service locations and imaging modality types.
Methods
Imaging case volumes in a large health care system were retrospectively studied, analyzing weekly imaging volumes by patient service locations (emergency department, inpatient, outpatient) and modality types (x-ray, mammography, CT, MRI, ultrasound, interventional radiology, nuclear medicine) in years 2020 and 2019. The data set was split to compare pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods. Independent-samples t tests compared the mean weekly volumes in 2020 and 2019.
Results
Total imaging volume in 2020 (weeks 1-16) declined by 12.29% (from 522,645 to 458,438) compared with 2019. Post-COVID-19 (weeks 10-16) revealed a greater decrease (28.10%) in imaging volumes across all patient service locations (range 13.60%-56.59%) and modality types (range 14.22%-58.42%). Total mean weekly volume in 2020 post-COVID-19 (24,383 [95% confidence interval 19,478-29,288]) was statistically reduced (P = .003) compared with 33,913 [95% confidence interval 33,429-34,396] in 2019 across all patient service locations and modality types. The greatest decline in 2020 was seen at week 16 specifically for outpatient imaging (88%) affecting all modality types: mammography (94%), nuclear medicine (85%), MRI (74%), ultrasound (64%), interventional (56%), CT (46%), and x-ray (22%).
Discussion
Because the duration of the COVID-19 pandemic remains uncertain, these results may assist in guiding short- and long-term practice decisions based on the magnitude of imaging volume decline across different patient service locations and specific imaging modality types.
Key Words: COVID-19, imaging volume, patient service locations, modality types
Introduction
In a short time, the coronavirus disease 2019 (COVID-19) pandemic has had a devastating global impact on the health of the population with an overwhelming demand for health care resources. As of May 3, 2020, a total of 3,502,956 cases have been reported worldwide with 245,081 deaths [1]. With 210 countries battling the pandemic, the United States has quickly become most severely affected with 1,160,996 cases and 67,448 deaths reported [1]. Within the United States, New York State has become the epicenter of COVID-19, representing over one-fourth of the cases (319,213) and over one-third of the deaths (24,368) reported in the country [1]. Community spread of the virus in an environment without pre-existing immunity continues to pose a serious health risk to the population.
Although social isolation policies have been successful in slowing the spread of COVID-19 [2], it has also led to a significant downturn of the US economy with stock market declines [3] and continuous rise in unemployment [4]. The economic impact has affected both small and large companies struggling to survive in almost every business sector, including health care. During this period, health care institutions and providers have been instructed to stop performing elective surgical procedures to slow the spread of disease and conserve health care resources for COVID-19 patients. Furthermore, ACR has endorsed guidance from the Centers for Disease Control and Prevention to reschedule nonurgent outpatient visits [5].
As a consequence of public policy, financial hardship, and patient fear, many radiology departments have experienced a rapid decline in imaging case volumes. This has important implications on the short- and long-term economic stability of radiology departments across all practice settings. However, only anecdotal evidence currently exists without a clear understanding of the magnitude of reduced imaging case volumes across different patient service locations (emergency department, inpatient, outpatient) and specific imaging modality types (x-ray, mammography, CT, MRI, ultrasound, interventional radiology, nuclear medicine).
The purpose of this study was to evaluate the impact of the COVID-19 pandemic on imaging case volumes using real-world data from a large health care institution. We analyzed the weekly imaging volumes during the COVID-19 pandemic stratified by patient service locations and imaging modality types.
Methods
A retrospective review of the imaging case volumes in a large health care system was performed from January 1, 2019, to April 18, 2020, to evaluate the impact of the COVID-19 pandemic on the imaging volumes by patient service locations and imaging modality types. Our institution is the largest health care system in New York State, consisting of 23 hospitals (academic, community, and specialty), 52 urgent care centers, and 17 imaging centers, serving a highly diverse mix of racial, ethnic, and socioeconomic groups. The imaging case volumes were provided as aggregate data for each week (Sunday to Saturday) in 2019 and 2020 stratified by patient service locations (emergency department, inpatient, outpatient) and imaging modality types (x-ray, mammography, CT, MRI, ultrasound, interventional radiology, nuclear medicine). Our health care system had no overall changes in the number of imaging scanners available for x-ray, mammography, CT, MRI, ultrasound, interventional procedures, and nuclear medicine examinations between 2019 and 2020 that would have affected the expected imaging case volumes during the COVID-19 pandemic. The institutional review board approved a waiver to use the retrospective aggregate data.
COVID-19 History in New York City
In New York City, the first confirmed patient tested positive for COVID-19 on March 1, 2020 (week 10, day 1). The first confirmed patient in our health care system tested positive on March 8, 2020 (week 11, day 1). Due to the rapid growth in COVID-19–positive cases, New York City quickly became the epicenter of the pandemic in the United States.
To lower the risk of exposure and transmission to health care providers, staff, and patients and to minimize contamination of equipment during the transportation and scanning of COVID-19 patients, careful review of the need for imaging in all patients was performed. On March 27, 2020 (week 13, day 6), our Department of Radiology issued guidelines for appropriate use of imaging in the emergency, inpatient, and outpatient settings. All nonurgent imaging was avoided in patients with confirmed or suspected COVID-19, if possible. The guidelines also recommended avoiding imaging procedures, when possible, that required health care providers to be in close contact with patients with COVID-19, such as ultrasound and interventional procedures. In the inpatient setting, the guidelines emphasized limiting imaging to those procedures that could not safely be performed in an outpatient setting after discharge. In particular, the judicious use of chest CT imaging in patients with COVID-19 was suggested for hospitalized symptomatic patients with specific clinical indications (ie, concern for bacterial superinfection, intubation-related barotrauma, etc).
Statistical Analysis
The imaging case volumes were provided for each imaging modality type (x-ray, mammography, CT, MRI, ultrasound, interventional radiology, nuclear medicine) in aggregate sum data according to the patient service locations (emergency department, inpatient, outpatient) for each week 1 to 16 in both 2020 and 2019 calendar years. The data set was split for analysis to compare the pre-COVID-19 period (weeks 1-9) and post-COVID-19 period (weeks 10-16). In the 2019 data, week 1 was adjusted to match 4 days of imaging volume data in 2020 for adequate comparison by eliminating January 1, 2019, imaging volumes from the data analysis.
The frequency data for each week were summed for the total weeks 1 to 16 pre-COVID-19 and post-COVID-19 periods according to patient service locations and imaging modality types. Descriptive frequency data were plotted separately to demonstrate the trend in the weekly imaging case volumes in 2020 from weeks 1 to 16 according to patient service locations and imaging modality types. The percent difference in the 2020 imaging case volumes was calculated by week for the total weeks 1 to 16 and pre-COVID-19 and post-COVID-19 periods, compared with the 2019 imaging volumes, stratified by patient service locations and imaging modality types. The difference in the imaging volumes in the 2020 calendar year were compared with the same weeks in 2019 to assess the degree of change accounting for monthly or seasonal variation within the same calendar year. The trend in the percentage of the 2020 weekly imaging case volumes, relative to 2019, was plotted from weeks 1 to 16 according to the patient service locations.
The mean weekly imaging volumes were calculated for each imaging modality type stratified by patient service locations for the total weeks 1 to 16 and pre-COVID-19 and post-COVID-19 periods. Independent-samples t tests were performed comparing the mean weekly imaging case volumes in years 2020 and 2019 for each imaging modality type stratified by patient service locations for the total weeks 1 to 16 and pre-COVID-19 and post-COVID-19 periods. Statistical significance was considered for P values < .05. All statistical analyses were performed using SAS v9.4 (SAS, North Carolina).
Results
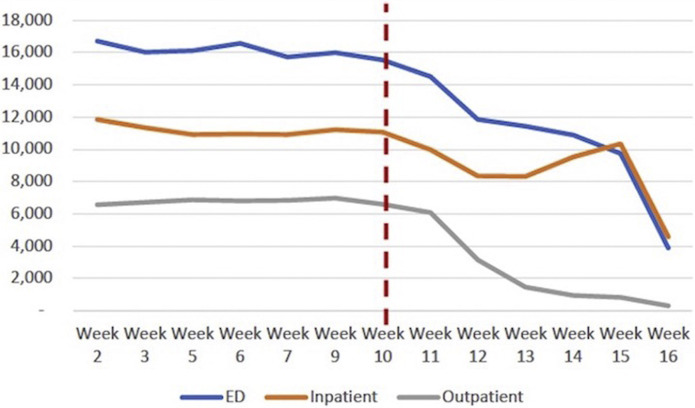
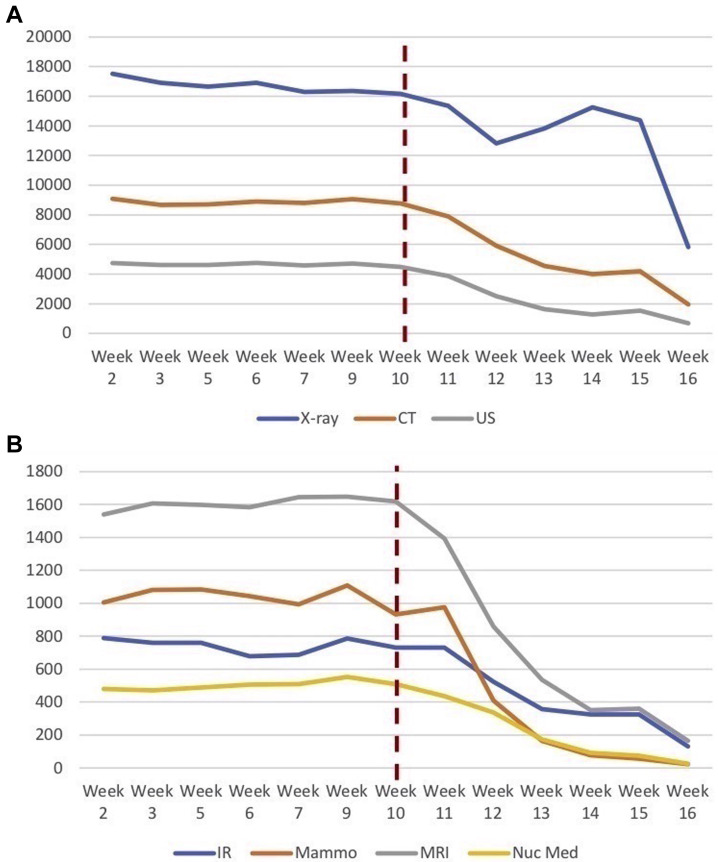
The total imaging case volume performed at our institution in year 2020 from weeks 1 to 16 was 458,438 examinations, compared with 522,645 examinations in 2019 during the same period (weeks 1-16). Table 1 displays the imaging case volumes according to patient service locations and imaging modality types for the total weeks 1 to 16 and pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods in 2020 and 2019. Figure 1 demonstrates the trend in the imaging case volumes in 2020 across weeks 1 to 16 stratified by patient service locations. Figure 2 reveals the trend in the imaging case volumes in 2020 across weeks 1 to 16 stratified by imaging modality types. Imaging case volumes in 2020 began to decline in week 10 (when the first confirmed patient tested positive for COVID-19 in New York City).
Table 1.
Imaging case volumes in 2020 and 2019 for the total (weeks 1-16) and pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods stratified by patient service locations and imaging modality types
| 2020 Year |
2019 Year |
|||||
|---|---|---|---|---|---|---|
| Imaging Volumes | Total (Weeks 1-16) | Pre-COVID-19 (Weeks 1-9) | Post-COVID-19 (Weeks 10-16) | Total (Weeks 1-16) | Weeks 1-9 | Weeks 10-16 |
| Total volume | 458,438 | 287,759 | 170,679 | 522,645 | 285,257 | 237,388 |
| Patient location | ||||||
| Emergency | 221,151 | 138,570 | 82,581 | 247,639 | 135,060 | 112,579 |
| Inpatient | 162,470 | 94,302 | 68,168 | 175,511 | 96,609 | 78,902 |
| Outpatient | 74,817 | 54,887 | 19,930 | 99,495 | 53,588 | 45,907 |
| Modality type | ||||||
| X-ray | 241,965 | 141,303 | 100,662 | 259,804 | 142,460 | 117,344 |
| Mammography | 11,232 | 8,557 | 2,675 | 14,320 | 7,887 | 6,433 |
| Ultrasound | 55,918 | 38,992 | 16,926 | 69,561 | 37,701 | 31,860 |
| CT | 115,315 | 75,485 | 39,830 | 134,494 | 73,284 | 61,210 |
| MRI | 18,858 | 13,321 | 5,537 | 24,399 | 13,065 | 11,334 |
| Nuclear medicine | 5,747 | 4,050 | 1,697 | 7,912 | 4,274 | 3,638 |
| Interventional | 9,403 | 6,051 | 3,352 | 12,155 | 6,586 | 5,569 |
COVID-19 = coronavirus disease 2019.
Fig 1.
The 2020 imaging case volume trend across weeks 1 to 16 stratified by patient service locations. The vertical red line at week 10 indicates when the first patient in New York City tested positive for coronavirus disease 2019. Calendar weeks are presented on the x axis and number of imaging examinations on the y axis. ED = emergency department.
Fig 2.
The 2020 imaging case volume trend across weeks 1 to 16 stratified by imaging modality types. The vertical red line at week 10 indicates when the first patient in New York City tested positive for coronavirus disease 2019. (A) Imaging volume data for x-ray, CT, and ultrasound (US) examinations. (B) Imaging volume data for interventional radiology (IR), mammography (Mammo), MRI, and nuclear medicine (Nuc Med) examinations. Calendar weeks are presented on the x axis and number of imaging examinations on the y axis.
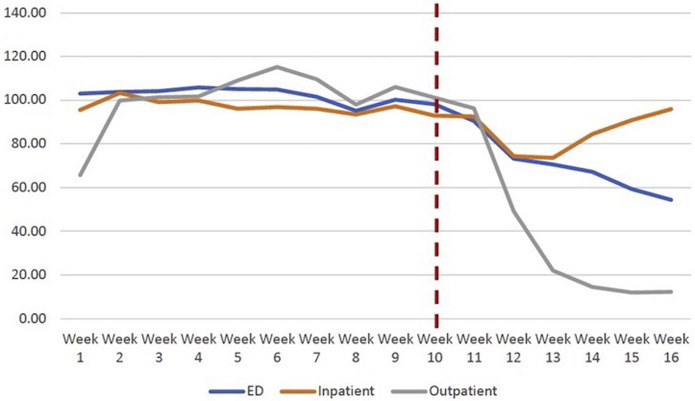
Table 2 reveals the percent difference in the imaging case volumes between 2020 and 2019 for the total weeks 1 to 16 and pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods, according to patient service locations and imaging modality types. In weeks 1 to 16, the total imaging volume decreased by 12.29% compared with the same period in 2019. However, when separating the total weeks into the pre-COVID-19 and post-COVID-19 periods, the total imaging volume increased by 0.88% in the pre-COVID-19 (weeks 1-9) period and decreased by 28.10% in the post-COVID-19 (weeks 10-16) period in year 2020 compared with the same weeks in 2019. In year 2020, the imaging case volumes declined in the post-COVID-19 period across all patient service locations (range 13.60%-56.59%) and imaging modality types (range 14.22%-58.42%). By week 16, the 2020 imaging case volumes declined by 45.56%, 4.15%, and 87.55% for emergency department, inpatient, and outpatient imaging, respectively. We also observed a shift in imaging volume with increased use of x-ray relative to cross-sectional imaging. When excluding x-ray, the decline in volume at week 16 was 54.96%, 37.80%, and 87.20% for emergency department, inpatient, and outpatient imaging, respectively. Figure 3 demonstrates the trend in the percentage of the 2020 imaging case volumes relative to 2019 across weeks 1 to 16 by patient service locations, with declines observed after week 10 in the post-COVID-19 period. At week 16, the 2020 imaging case volumes represented 54.44%, 95.85%, and 12.45% of the imaging volume in 2019 for the emergency department, inpatient, and outpatient settings, respectively.
Table 2.
Percent change in the 2020 imaging volumes, compared with 2019, for the total (weeks 1-16) and pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods, and week 16 stratified by patient service locations and imaging modality types
| Percent Change in 2020 Imaging Volumes Compared With 2019 |
||||
|---|---|---|---|---|
| Imaging Volumes | Weeks 1-16 | Weeks 1-9 | Weeks 10-16 | Week 16 |
| Total volume | −12.29 | +0.88 | −28.10 | −40.14 |
| Patient location | ||||
| Emergency | −10.70 | +2.60 | −26.65 | −45.56 |
| Inpatient | −7.43 | −2.39 | −13.60 | −4.15 |
| Outpatient | −24.80 | +2.42 | −56.59 | −87.55 |
| Modality type | ||||
| X-ray | −6.87 | −0.81 | −14.22 | −22.16 |
| Mammography | −21.56 | +8.49 | −58.42 | −93.58 |
| Ultrasound | −19.61 | +3.42 | −46.87 | −63.69 |
| CT | −14.26 | +3.00 | −34.93 | −46.46 |
| MRI | −22.71 | +1.96 | −51.15 | −73.57 |
| Nuclear medicine | −27.36 | −5.24 | −53.35 | −85.03 |
| Interventional | −22.64 | −8.12 | −39.81 | −55.57 |
COVID-19 = coronavirus disease 2019.
Fig 3.
The trend in the percentage of the 2020 imaging case volumes relative to 2019 across weeks 1 to 16 stratified by patient service locations. The vertical red line at week 10 indicates when the first patient in New York City tested positive for coronavirus disease 2019. Calendar weeks are presented on the x axis and the imaging volume percentage on the y axis. At week 16, the 2020 imaging case volumes represented 54.44%, 95.85%, and 12.45% of the imaging volume in 2019 for the emergency department (ED), inpatient, and outpatient settings, respectively.
Table 3 shows the comparison of the 2020 and 2019 mean weekly imaging case volumes in the post-COVID-19 period (weeks 10-16) for the imaging modality types stratified by patient service locations. In the pre-COVID-19 period, there was no statistical difference (P = .905) in the mean weekly imaging volumes in 2020 (31,973 [95% confidence interval 27,978-35,967]) compared with 2019 (31,695 [95% confidence interval 28,194-35,195]). However, statistically significant differences (P = .003) were seen in the mean weekly imaging case volumes in the post-COVID-19 period with total volume decreased to 24,383 (95% confidence interval 19,478-29,288) in 2020 compared with 33,913 (95% confidence interval 33,429-34,396) in 2019 and across all patient service locations and imaging modality types.
Table 3.
Comparison of years 2020 and 2019 mean weekly imaging volumes and 95% CIs for the post-COVID-19 (weeks 10-16) period according to imaging modality types stratified by patient service locations
| 2020 Year |
2019 Year |
P value | |||
|---|---|---|---|---|---|
| Imaging Volumes | Mean | 95% CI | Mean | 95% CI | |
| Emergency department | |||||
| CT | 3,866.9 | 2,668.3-5,065.4 | 5,961.1 | 5,823.7-6,098.6 | .005∗ |
| Interventional | 8.7 | 5.1-12.3 | 11.9 | 7.1-16.6 | .219 |
| MRI | 70.0 | 34.8-105.2 | 165.9 | 149.7-182.0 | <.001∗ |
| Nuclear medicine | 11.9 | 2.0-21.7 | 24.9 | 20.2-29.6 | .018∗ |
| Ultrasound | 834.0 | 425.2-1,242.8 | 1,772.6 | 1,743.8-1,801.4 | .001∗ |
| X-ray | 7,005.9 | 6,097.5-7,914.3 | 8,146.4 | 7,980.0-8,312.9 | .022∗ |
| Total | 11,797.3 | 9,498.2-14,096.3 | 16,082.7 | 15,867.8-16,297.7 | .004∗ |
| Inpatient | |||||
| CT | 1,502.1 | 1,139.2-1,865.1 | 2,070.7 | 1,992.1-2,149.3 | .008∗ |
| Interventional | 307.7 | 211.3-404.1 | 503.0 | 486.5-519.5 | .002∗ |
| MRI | 402.4 | 186.5-618.3 | 792.7 | 753.5-831.9 | .004∗ |
| Nuclear medicine | 75.7 | 29.2-122.3 | 191.9 | 173.1-210.6 | <.001∗ |
| Ultrasound | 1,002.6 | 692.5-1,312.6 | 1,490.0 | 1,439.3-1,540.7 | .008∗ |
| X-ray | 6,447.7 | 5,459.5-7,436.0 | 6,223.4 | 5,988.4-6,458.5 | .599 |
| Total | 9,738.3 | 87,49.2-10,727.4 | 11,271.7 | 10,952.6-11,590.9 | .008∗ |
| Outpatient | |||||
| CT | 321.0 | 66.8-575.2 | 712.4 | 692.9-732.0 | .009∗ |
| Interventional | 162.4 | 86.8-238.0 | 280.7 | 260.9-300.5 | .008∗ |
| Mammography | 382.1 | 4.5-759.8 | 919.0 | 829.6-1,008.4 | .013∗ |
| MRI | 318.6 | 79.6-557.6 | 660.6 | 644.6-676.6 | .013∗ |
| Nuclear medicine | 154.9 | 39.4-270.3 | 303.0 | 284.9-321.1 | .020∗ |
| Ultrasound | 581.4 | 107.4-1,055.5 | 1,288.9 | 1,240.1-1,337.6 | .011∗ |
| X-ray | 926.7 | 107.6-1,745.9 | 2,393.6 | 2,321.6-2,465.5 | .005∗ |
| Total | 2,847.1 | 504.3-5,190.0 | 6,558.1 | 6,403.9-6,712.4 | .008∗ |
| All patient service locations | |||||
| CT | 5,690.0 | 3,909.6-7,470.4 | 8,744.3 | 8,557.2-8,931.4 | .006∗ |
| Interventional | 478.9 | 307.7-650.0 | 795.6 | 783.3-807.9 | .004∗ |
| Ultrasound | 2,418.0 | 1,242.3-3,593.7 | 4,551.4 | 4,477.5-4,625.4 | .004∗ |
| MRI | 791.0 | 306.9-1,275.1 | 1,619.1 | 1,569.2-1,669.1 | .006∗ |
| Nuclear medicine | 242.4 | 72.7-412.2 | 519.7 | 498.4-541.1 | .007∗ |
| X-ray | 14,380.3 | 13,193.6-15,567.0 | 16,763.4 | 16,431.2-17,095.7 | .002∗ |
| Total | 24,382.7 | 19,477.7-29,287.7 | 33,912.6 | 33,429.3-34,395.9 | .003∗ |
CI = confidence interval; COVID-19 = coronavirus disease 2019.
P ≤ .05.
Discussion
The COVID-19 pandemic has given rise to unprecedented and unpredictable circumstances for radiology practices. Anecdotal experience suggests that radiology practices should anticipate 50% to 70% decreases in imaging volume that will last a minimum of 3 to 4 months, depending on the location of practice and the severity of the COVID-19 pandemic in each region [6]. To prepare a short-term and long-term response to the COVID-19 crisis, the need for real-world data is essential to understand the magnitude of reduced imaging case volumes across the different patient service locations and specific imaging modality types.
The results from this study have revealed an overall 28% decline in the total imaging volume over a 7-week period during the COVID-19 pandemic (weeks 10-16) compared with 2019, including all patient service locations and imaging modality types. Even though this decline in imaging volumes seems less than the anecdotal evidence suggesting a 50% to 70% decline [6], the trend data have shown a transition period with a steep decline rate observed from weeks 10 to 13. Thus, we have observed the greatest percent difference in the 2020 imaging case volumes after the transition period at week 16 (40%). Furthermore, this study has demonstrated that the imaging volume deterioration has varied by location, with the greatest declines observed at week 16 in the outpatient setting (maximum year-over-year decline of 88%) followed by the emergency department (46%) and inpatient (4%) settings. Imaging volume deterioration also varied by modality type, with the greatest declines observed at week 16 in mammography (94%), followed in descending order by nuclear medicine (85%), MRI (74%), ultrasound (64%), interventional radiology (56%), CT (46%), and x-ray (22%).
To our knowledge, there is no published study describing the magnitude of the decline in imaging case volumes during the COVID-19 pandemic stratified by both patient service locations and imaging modality types. Importantly, this study used the prior year 2019 weekly data for comparison to account for potential bias from monthly and seasonal variation. In addition, our health care system had no overall changes in the number of imaging scanners available for x-ray, mammography, CT, MRI, ultrasound, interventional procedures, and nuclear medicine examinations between 2019 and 2020 that would have affected the expected imaging case volumes during the COVID-19 pandemic. Given that our health care institution is comprised of different practice settings, the stratified data may be applicable to other radiology practices that are comprised mainly of either outpatient or inpatient settings.
There are significant economic implications on radiology groups and health care systems mainly due to the resultant combined lost revenue and staffing needs [6] during the pandemic. Several policy changes have been enacted to limit the transmission of COVID-19. Federal and state governments have mandated nonessential business closures and “stay-at-home” orders. In addition, health care policies have recommended the pause of elective and routine medical services, particularly surgical procedures and imaging examinations. However, individual behavior and actions have also contributed to the decline in imaging case volumes. The general public is hesitant to visit any health care facility for fear of being exposed to the coronavirus (SARS-CoV-2), in particular the emergency department [7]. This has raised concerns regarding the potential adverse health outcomes in patients delaying care for emergent conditions, such as acute stroke, myocardial infarction, appendicitis, and so on.
Even though health care institutions can apply for interim funding relief from a variety of government remedies including the CARES Act [8], Treasury’s Exchange Stabilization Fund [9], and Medicare [10], more radiology practices will be challenged to survive in a constrained economic environment as the pandemic ensues. Thus, many practices will need to make short-term changes to survive this period and permanent changes to the radiology practice model may be necessary in the long term [6]. In particular, radiology groups that are mainly comprised of outpatient imaging will be most severely affected according to anecdotal evidence [6] and the real-world data presented in this study.
The main limitation of this study is the retrospective design using aggregate data, thus limiting more detailed analyses evaluating the potential decline of imaging case volumes by CPT codes (ie, brain MRI, chest CT, abdominal x-ray) or clinical indications (International Classification of Diseases, 10th rev codes). It is possible that imaging case volumes for some CPT codes or clinical indications changed more than others. Another limitation is that our health care institution is located in the epicenter of the COVID-19 pandemic, potentially limiting the generalizability of these results. With nationwide spread of COVID-19, it is likely that almost every region will directly or indirectly experience the impact of this pandemic. Even though these results may serve as a worst-case scenario, specific analyses of imaging case volumes in less severely affected regions would be warranted for comprehensive evaluation.
In summary, as radiology practices prepare to minimize the impact of the COVID-19 pandemic on imaging case volumes and begin to formulate transition plans in the recovery period, the results from this study provide real-world data to inform radiology practices toward evidence-based decisions. Because the duration of the COVID-19 pandemic remains uncertain, this study may assist in guiding short-term and long-term practice decisions based on the magnitude of imaging volume decline across different patient service locations and specific imaging modality types during the COVID-19 pandemic. Importantly, these data may play a vital role in demonstrating the impact on radiology practices to support requests for funding relief from the government COVID-19 recovery plans.
Take-Home Points
-
▪
This study reveals an overall 28% decline in the total imaging volume during the COVID-19 pandemic (7 weeks) including all patient service locations and imaging modality types.
-
▪
Imaging volume deterioration varied by location, with the greatest decline observed by week 16 in the outpatient setting (88%) followed by the emergency department (46%) and inpatient (4%) settings.
-
▪
Imaging volume deterioration also varied by modality type, with the greatest decline observed by week 16 in mammography (94%), followed in descending order by nuclear medicine (85%), MRI (74%), ultrasound (64%), interventional radiology (56%), CT (46%), and x-ray (22%).
-
▪
As radiology practices prepare to minimize the impact of the COVID-19 pandemic on imaging case volumes and begin to formulate transition plans in the recovery period, the results from this study provide real-world data to inform radiology practices toward evidence-based decisions.
Acknowledgments
Funding support was received from the Harvey L. Neiman Health Policy Institute through a research partnership. We acknowledge Frank Rizzo, Morgan O’Hare, and Chen (Shirley) Liu from the finance department at our institution for contributing the aggregated data used in the analyses in this study. We acknowledge the Northwell COVID-19 Research Consortium.
Footnotes
Dr Boltyenkov reports personal fees from Siemens Medical Solutions USA, Inc, outside the submitted work, and is a shareholder of Siemens Healthineers. Dr Hughes reports grants from Harvey L. Neiman Health Policy Institute, outside the submitted work. Dr Sanelli reports grants from Harvey L. Neiman Health Policy Institute, during the conduct of the study, and grants and nonfinancial support from Siemens Healthineers, Inc, outside the submitted work. The other authors state that they have no conflict of interest related to the material discussed in this article. All authors are nonpartnership track employees.
References
- 1.Worldometer United States. https://www.worldometers.info/coronavirus/country/us/ Available at: Updated May 3, 2020. Accessed 2020 May 3, 2020.
- 2.NYC Health COVID-19 data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Available at: Updated April 18, 2020. Accessed April 25, 2020.
- 3.Federal Reserve Bank of St. Louis, Economic Research. S&P 500. https://fred.stlouisfed.org/series/SP500 Updated May 1, 2020. Accessed May 3, 2020.
- 4.Federal Reserve Bank of St. Louis, Economic Research. Unemployment rate. https://fred.stlouisfed.org/series/UNRATE Available at: Updated April 3, 2020. Accessed May 3, 2020.
- 5.ACR ACR COVID-19 clinical resources for radiologists. https://www.acr.org/Clinical-Resources/COVID-19-Radiology-Resources Available at: Updated April 28, 2020. Accessed May 3, 2020.
- 6.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices [E-pub ahead of print] Radiology. 2020:201495. doi: 10.1148/radiol.2020201495. PubMed PMID: 32293225. Published online April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krumholz H.M. Where have all the heart attacks gone? New York Times. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html Available at: Published April 6, 2020. Accessed April 25, 2020.
- 8.Capital Associates, Inc Summary of CARES Act supplemental appropriations/summary of CARES Act Healthcare Provisions. AHRA Resources. https://link.ahra.org/2020/03/27/summary-of-cares-act-supplemental-appropriations/ Available at: Published March 27, 2020. Accessed April 25, 202.
- 9.ACR CARES Act offers loans and tax relief to radiology practices. (VA): American College of Radiology; c2004-2020. https://www.acr.org/Advocacy-and-Economics/Advocacy-News/Advocacy-News-Issues/In-the-April-4-2020-Issue/CARES-Act-Offers-Loans-and-Tax-Relief-to-Radiology-Practices Available at: Published April 1, 2020. Accessed April 25, 2020.
- 10.AMA CARES Act: Medicare advance payments for COVID-19 emergency. https://www.ama-assn.org/delivering-care/public-health/cares-act-medicare-advance-payments-covid-19-emergency Available at: Updated April 6, 2020. Accessed April 25, 2020.