Abstract
Objective
There is a coronavirus disease 2019 (COVID-19) pandemic. We aimed to describe the characteristics of patients transported by the Royal Flying Doctor Service (RFDS) for confirmed or suspected COVID-19 and to investigate the surge capacity of and operational implications for the RFDS in dealing with COVID-19.
Methods
This was a prospective cohort study. To determine the characteristics of patients transported for confirmed or suspected COVID-19, we included patient data from February 2, 2020, to May 6, 2020. To investigate the surge capacity and operational implications for the RFDS in dealing with COVID-19, we built and validated an interactive operations area-level discrete event simulation decision support model underpinned by RFDS air medical activity data from 2015 to 2019 (4 years). This model was subsequently used in a factorial in silico experiment to systematically investigate both the supply of RFDS air medical services and the increased rates of demand for these services for diseases of the respiratory system.
Results
The RFDS conducted 291 patient episodes of care for confirmed or suspected COVID-19. This included 288 separate patients, including 136 men and 119 women (sex missing = 33), with a median age of 62.0 years (interquartile range, 43.5-74.9 years). The simulation decision support model we developed is capable of providing dynamic and real-time support for RFDS decision makers in understanding the system's performance under uncertain COVID-19 demand. With increased COVID-19–related demand, the ability of the RFDS to cope will be driven by the number of aircraft available. The simulation model provided each aviation section with estimated numbers of aircraft required to meet a range of anticipated demands.
Conclusion
Despite the lack of certainty in the actual level of COVID-19–related demand for RFDS services, modeling demonstrates that the robustness of meeting such demand increases with the number of operational and medically staffed aircraft.
There is a coronavirus disease 2019 (COVID-19) pandemic, which originated in Hubei Province in China. There is evidence of community transmission throughout the world, including Australia. Infection can cause severe acute respiratory illness, but there is a spectrum of disease ranging from mild to severe symptoms.1
To help reduce the incidence of COVID-19, quarantine measures have been implemented in Australia. These measures are changing rapidly. People who have been in contact with a person with a confirmed case of COVID-19 and people who have traveled from or who have transited through affected areas are required to quarantine for 14 days. People who are tested for COVID-19 include those who have symptoms of the disease, such as fever, or acute respiratory infection (eg, shortness of breath or cough), with or without fever, and have either traveled or transited through a country considered to pose a risk of transmission in the 14 days before illness onset or have had contact with a confirmed case of COVID-19 in the 14 days before illness onset.2 Routine population screening is currently being conducted in some areas; however, it has not been mandated by the Commonwealth. The Australian Commonwealth Government has recently announced Australian border closures, with some state governments also shutting borders to domestic travelers. This is in addition to new social distancing measures and the closure of nonessential services3 in response to the continued growth of COVID-19 within the community.4
The Royal Flying Doctor Service (RFDS) is 1 of the largest air medical services in the world,5 , 6 with 77 aircraft and 140 health care vehicles located across its 23 Australian bases.7 In 2018/2019, 370,706 patient contacts were made through RFDS clinics, air medical transports, and telehealth consultations. At the same time, there were 82,081 road transfers.7
The RFDS deals with respiratory and infectious diseases routinely. However, COVID-19 presents challenges in terms of potential volumes of patients needing care and the impacts it has on organizational capacity. Since the identification of COVID-19 within Australia, the RFDS has been transporting patients with confirmed COVID-19 and those who have developed symptoms after being in a high-risk situation. This has included cases from the cruise ship The Diamond Princess and the transfer of patients for ongoing isolation and hospital care.
Despite the containment measures implemented in Australia, COVID-19 cases are expected to increase in the coming weeks. As a provider of air medical retrieval services and road transport services for a range of illnesses, it is important for the RFDS to understand the potential impact of COVID-19 on the populations it serves. Predicting what medical resources may need to be deployed to provide appropriate patient care ahead of time will assist the RFDS in being well prepared to provide this care. In addition to undertaking air medical retrievals for a variety of acute illnesses, the RFDS needed to understand its surge capacity and ability to rapidly deploy additional aircraft if the COVID-19 pandemic worsened.
The objectives of this study were to describe the characteristics of patients transported by either an air medical retrieval or road transport by the RFDS for confirmed or suspected COVID-19 and to investigate the surge capacity of and operational implications for the RFDS in dealing with air medical retrievals for COVID-19.
Methods
Setting
The RFDS traditionally provides air medical retrievals, road transports, and primary health care to rural and remote populations who are unable to access traditional services through the Medicare Benefits Schedule. However, with the COVID-19 pandemic, the RFDS has been called on to expand its scope of practice and provide services across all geographic areas, including inner regional and major city areas.
RFDS air medical retrievals include primary evacuations and interhospital transfers (IHTs). A primary evacuation describes the provision of emergency medical services to people affected by illness or accident who are in a serious or potentially life-threatening condition and are beyond the normal medical infrastructure. An IHT describes the transfer of patients between hospitals designated as normal medical infrastructure, often to access a higher level of care, such as specialist treatment or lifesaving surgery. However, an IHT can also include the transfer of a patient from a large to a smaller community hospital to receive ongoing care closer to the patient's home.
Nonemergency road transports are undertaken by the RFDS. For these transports, the RFDS is tasked by an ambulance service (eg, Ambulance Victoria) to transport a patient to the hospital or to receive specialist care.
Patients
Since tasking to retrieve COVID-19 patients, the RFDS has been recording cases. Each COVID-19 case has been coded under chapter 10 (Diseases of the Respiratory System) of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification.8 A suspected case was defined in accordance with the World Health Organization global surveillance for human infection with COVID-19 guidelines.2 A confirmed case was defined as those who have been confirmed as being positive for COVID-19 via a laboratory pathology test. Patient data were collected within flight, and road transport data were collected during transport using either paper-based or electronic methods according to the usual practice of the specific RFDS section and operation.9
Statistical Analysis and Simulation Modeling
To describe the characteristics of patients transported by the RFDS for confirmed or suspected COVID-19 from February 2, 2020, to May 7, 2020, means (standard deviations) and medians (interquartile ranges) were used for continuous characteristics and counts (proportions) for count characteristics.
To investigate the surge capacity of and operational implications for the RFDS in dealing with air medical retrievals for COVID-19, we built and validated an interactive discrete event simulation (DES) decision support model based on RFDS activity data from July 1, 2015, to June 30, 2019 (4 years). DES is focused on improving the design and operation of the systems under investigation10 and is widely used in health systems research.11 The fundamental building blocks of the DES model include individual patients who flow through the system, queues where patients are waiting to be cared for, activities performed by the system as part of the care process, and resources required to provide successful patient care activities.
DES modeling began by creating a conceptual model for the RFDS process of care for an air medical retrieval consisting of the following activities: flight authorization, resource mobilization, flight to the scene, patient care at the scene, flight to the receiving hospital airstrip, and return to base. Every activity requires appropriate resources in the form of an aircraft and crew capable and ready to perform this activity and may require patients queueing for service based on the predetermined category of priority. The model followed the following 3-tiered priority classification: category 1, the patient is classified as high acuity/severity; category 2, the patient is classified as moderate acuity/severity; and category 3, the patient is classified as low acuity/severity.
We also divided patients into 2 categories based on whether their primary diagnosis was related to the respiratory system (which includes novel coronaviruses, such as COVID-19) or another disease so that the characteristics of the respiratory system disease patients could be used to subsequently model increased demand because of COVID-19.
The following outcomes of immediate interest for the DES were identified: 1) the percentage of time the RFDS does not have spare aircraft capacity to respond to the next call for service, 2) the median time from the first call to aircraft mobilization by priority category, and 3) the median time from the first call to aircraft arrival by priority category.
The conceptual model was validated with representatives (n = 20) of the individual RFDS operational area commands (including Western Operations, Central Operations [CO], the Queensland Section, the South Eastern Section, the Victorian Section, and the Tasmanian Section). After this, the computational DES models for individual RFDS operational areas were created and calibrated for the base case scenario using historic data on air medical retrievals for respiratory and nonrespiratory diseases. This included data on all patients who underwent an air medical retrieval for diseases of the respiratory system (coded in chapter 10 of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification) between July 1, 2015, and June 30, 2019 (4 years). Patient data were collected within flight and included the patient's sex, age, and self-reported indigenous status (Table 1 ) using either paper-based or electronic methods according to the usual practice of the specific RFDS section and operation.8 The computational DES model was subsequently iteratively validated using the base case scenario with the representatives of the individual RFDS operational area commands until all the stakeholders were satisfied with the model's performance. The computational DES model was created using AnyLogic 8.5.1 (former XJ Technologies), Oakbrook Terrace, IL 60181 USA, simulation modeling software.
Table 1.
Characteristics of Patients Air Medically Retrieved for Respiratory Disease for 2015 to 2019 Financial Years
| ICD-10 Code Description Respiratory System Disease | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| J18 Pneumonia, organism unspecified | 1,022 (18.9) | 866 (20.5) | 1,888 (19.6) |
| J21 Acute bronchiolitis | 552 (10.2) | 414 (9.8) | 966 (10.0) |
| J44 Other chronic obstructive pulmonary disease | 295 (5.5) | 271 (6.4) | 566 (5.9) |
| J22 Unspecified acute lower respiratory infection | 176 (3.3) | 192 (4.5) | 368 (3.8) |
| J45 Asthma | 126 (2.3) | 195 (4.6) | 321 (3.3) |
| J93 Pneumothorax | 202 (3.7) | 68 (1.6) | 270 (2.8) |
| J81 Pulmonary oedema | 136 (2.5) | 132 (3.1) | 268 (2.8) |
| J90 Pleural effusion, not elsewhere classified | 148 (2.7) | 116 (2.7) | 264 (2.7) |
| J96 Respiratory failure, not elsewhere classified | 113 (2.1) | 83 (2.0) | 196 (2.0) |
| J36 Peritonsillar abscess | 112 (2.1) | 72 (1.7) | 184 (1.9) |
| J15 Bacterial pneumonia, not elsewhere classified | 89 (1.6) | 86 (2.0) | 175 (1.8) |
| J98 Other respiratory disorders | 101 (1.9) | 74 (1.8) | 175 (1.8) |
| J16 Pneumonia due to other infectious organisms, not elsewhere classified | 81 (1.5) | 69 (1.6) | 150 (1.6) |
| J06 Acute upper respiratory infections of multiple and unspecified sites | 61 (1.1) | 66 (1.6) | 127 (1.3) |
| J39 Other diseases of upper respiratory tract | 68 (1.3) | 52 (1.2) | 120 (1.2) |
| J47 Bronchiectasis | 55 (1.0) | 38 (0.9) | 93 (1.0) |
| J80 Adult respiratory distress syndrome | 49 (0.9) | 39 (0.9) | 88 (0.9) |
| J05 Acute obstructive laryngitis (croup) and epiglottitis | 61 (1.1) | 26 (0.6) | 87 (0.9) |
| J03 Acute tonsillitis | 46 (0.9) | 38 (0.9) | 84 (0.9) |
| J12 Viral pneumonia, not elsewhere classified | 37 90.7) | 32 (0.8) | 69 (0.9) |
| Leading 20 diagnoses | 3,530 (65.4) | 2,929 (69.3) | 6,459 (67.1) |
| All other respiratory system diseases | 1,869 (34.6) | 1,296 (30.7) | 3,165 (32.9) |
| Total | 5,399 | 4,225 | 9,624 |
ICD-10 = International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
The designed and validated DES model was subsequently used in a full factorial in silico experiment to systematically investigate the system's performance under various scenarios, combining individual levels of supply of RFDS services and the potential COVID-19–related demand. The factors included in the experimental design were the number of aircraft available within the operational command area as well as the daily rates of potential additional COVID-19–related demand in patients with respiratory system disease for different priority categories.
Overall, 520 individual DES simulation runs were conducted, with every run including 1 month of “warm-up” simulated activity to achieve the steady state followed by a 6-month period of simulated activity to estimate the system's performance.
Results
RFDS COVID-19 Transfer Number and Results
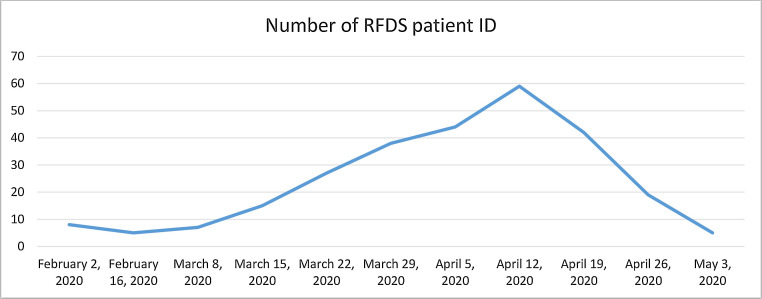
The RFDS conducted 291 patient episodes of care for confirmed or suspected COVID-19. This included 288 separate patients, including 136 men and 119 women (sex missing = 33), with a median age of 62.0 years (interquartile range, 43.5-74.9 years). Episodes included 262 interhospital transfers, 25 primary evacuations, and 1 repatriation. All patients were either confirmed (n = 20) or strongly suspected (n = 268) of having COVID-19. Figure 1 demonstrates the RFDS COVID-19 activity since the 2 Febraury 2020.
Figure 1.
Confirmed and Suspected COVID-19 Weekly Retrieval Trends.
Interactive DES Decision Support Tool
To assist in planning the RFDS’ air medical response related to a potential surge in COVID-19, we designed and validated an interactive surge capacity planning decision support tool. This tool is capable of providing dynamic and real-time support for RFDS decision makers in understanding the system's performance under uncertain COVID-19 demand through exploring various demand scenarios.Figure 2 demonstrates the interactive decision support tool interface.
Figure 2.
The COVID-19 Activity Modeling Visual Dashboard.
Levels of RFDS Service Provision for a Range of Hypothetical Increases in COVID-19 Demand
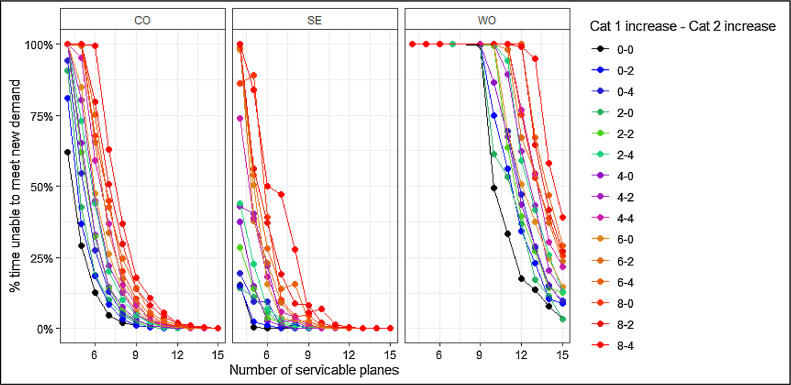
The RFDS is able to meet demand on current activity; however, as the numbers of priority 1 and 2 cases increase because of COVID-19, the percentage of time when the RFDS is able to meet demand is driven by the number of aircraft available per section and operation. For example, when CO, which provides services to South Australia and the Northern Territory, has 6 operational aircraft, it is able to meet demand 87.5% of the time at benchmark. However, if COVID-19 cases were to increase by 8 priority 1 and 4 priority 2 patients per day, CO would need to increase its serviceable aircraft to 8 to 15 to meet demand. This is consistent throughout the RFDS sections and operations (Fig. 3 ).
Figure 3.
The Percentage of Time the RFDS Area Does Not Have Spare Aircraft Capacity to Respond to the Next Call for Service.
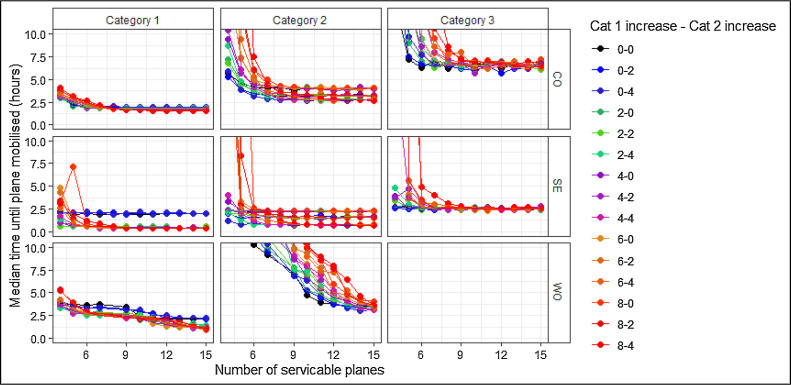
Figure 4 indicates that under most scenarios, priority 1 patient demand is met under 6 hours; however, this is at the expense of priority 2 to 3 patients (because they are prioritized after priority 1 patients). Note that the bottom right panel in this figure is blank; as in all tested scenarios, the time to mobilization for priority 3 patients is greater than 10 hours. The impact of COVID-19 on the ability to meet patient demand in a timely manner is reflected in the overall patient wait times (Fig. 5 ).
Figure 4.
The Median Time From the First Call to Aircraft Mobilization by Urgency Category.
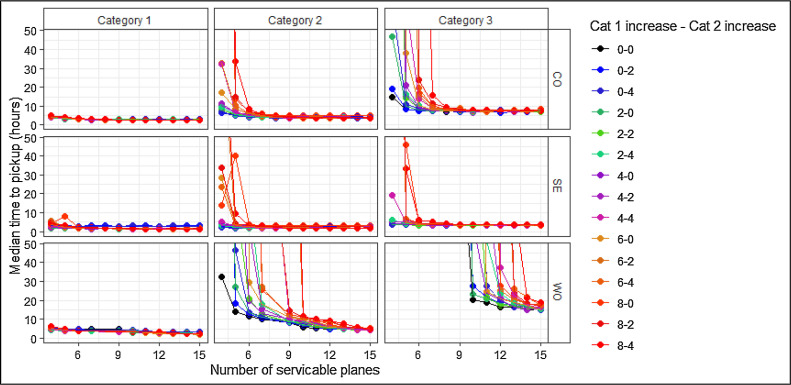
Figure 5.
The Median Time From the First Call to Aircraft Arrival by Urgency Category.
For all considered outcomes, the impact of COVID-19 demand on RFDS operations is mitigated by an increase in aircraft capacity. As the number of aircraft is increased, all of the outcomes improve in each tested demand scenario, resulting in shorter waiting times and a greater ability to respond to additional demand. Furthermore, the spread of outcomes between the largest and smallest levels of COVID-19 demand is reduced as aircraft capacity is improved, indicating that despite the lack of certainty in the actual level of COVID-19–related demand, the degree of robustness in meeting such demand increases with resource availability.
Discussion
The RFDS has conducted 291 transfers for COVID-19, increasing from 3 on February 2, 2020, to 291 on May 7, 2020. These trends appear to be consistent with Australia data, with 12 confirmed cases on February 2, 2020, increasing to 6,849 as of 15:00 on May 7, 2020.4 The trajectory of the epidemic in Australia appears to be lagging behind many European and North American countries by several weeks, in part because of the travel bans introduced early in the epidemic. However, it is important to be prepared for a significant increase in COVID-19 cases, especially in rural and remote Australia.
In order to be prepared, the RFDS has identified likely barriers and enablers for the provision of adequate level of RFDS services under a range of different COVID-19 demand scenarios. Our modeling indicates that at most thresholds, we can provide air medical retrievals for increased COVID-19 activity. It appears that the availability of aircraft is unlikely to be a major barrier. However, the potential lack of workforce (ie, pilots/engineers/clinical staff) has been identified as the major barrier to getting aircraft into the air. Without the appropriately skilled and available workforce, the RFDS is unlikely to be able to transfer category 3 patients to the hospital, who would then require patient care within their communities.
Our modeling indicated that above a certain activity level, we would not be able to transfer mild COVID-19 patients within a reasonable time frame and that providing transportation is dependent on workforce being able to staff and provide maintenance on aircraft. Rural and remote areas (especially remote areas) have significant workforce shortages.12 This includes limitations in recruiting and retaining general practitioners, nurses, and allied health professionals.12 During this pandemic, we have had volunteer pilots offer their services. However, our most significant barrier to providing additional services is a lack of engineers to maintain the aircraft and clinical staff to provide services. In the event of mass infection and current staff potentially becoming unwell, we will need more staff to provide coverage. This could include having nursing and medical students providing paid (covered by insurance) support to senior clinicians, as recently recommended.13 Alternatively, the Australian Defence Force could provide engineering and clinical support, as recently seen in the Australian bushfires.
In addition to constraints on RFDS air medical retrievals for priority 3 patients, it is likely that hospitals would be overwhelmed in the case of mass infection in rural and remote Australia, further necessitating the need for local solutions for the treatment of less severe cases.
Rural and remote areas also have significantly lower health care service provision than their major city counterparts, with the RFDS and Aboriginal Medical Services being the only service provider in many areas.14 , 15 It is of concern that our modeling predicted that at high activity levels, we would not be able to transport priority 3 patients. This is worrying because mild COVID-19 patients would need to be treated within their community until transfer is possible. Having patients remain within their community without adequate treatment could result in further community transmission.
Mass infection of COVID-19 has overwhelmed hospitals in Italy because of severe cases requiring intensive care unit (ICU) services, such as ventilators and a specialized workforce. Because of shortfalls in ICU beds, Italy has seen a spike in otherwise preventable deaths.16 Within Australia, we may not have enough ICU beds to match the potential demand.16 The current Australian government strategy is to mitigate transmission risk factors within the general public.17 However, it is unclear how a mass infection would affect rural and remote Australia because of the vast distances between communities. If mass infection occurred in rural and remote towns, it could have dire outcomes. This is due to rural and remote populations having higher rates of respiratory disease than their major city counterparts, as well as higher rates of other chronic diseases.12 , 18 Specifically, rural and remote populations are also more likely to suffer poorer outcomes of respiratory disease, including bronchiectasis.14 COVID-19 directly affects the lungs and patients’ ability to breathe, with severe cases requiring oxygen therapy via a respirator.18
Furthermore, many remote communities have high proportions of indigenous Australians15 , 19 and higher levels of socioeconomic disadvantage.20 The life expectancy of indigenous Australians is significantly lower than nonindigenous Australians, with indigenous Australians more likely to suffer from many chronic diseases at a younger age, including type 2 diabetes, cardiovascular disease, and renal disease.21
As such, in the event of mass infection, it is vitally important that we develop care strategies for mild COVID-19 patients in rural and remote areas, including dedicated COVID-19 clinics or in situ field hospitals (or similar). Another strategy would be to increase the use of RFDS telehealth platforms.
Conclusion
The RFDS has been conducting extensive air medical retrievals and road transports for patients with or suspected of having COVID-19 throughout Australia. Modeling indicates that as COVID-19 activity increases, the RFDS will need to use more aircraft in the transportation of patients to inner regional and major city hospitals. However, if COVID-19 activity was to increase to 10 patients per day per RFDS area of operations, many of the mild cases would need to remain within their communities for an extended period of time, potentially increasing the risk of community transfer. As such, it is important to ensure that the RFDS has adequate funding, workforce, and equipment to allow it to respond in the event of increased COVID-19 activity.
References
- 1.Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global surveillance for human infection with coronavirus disease (COVID-19). Available at: https://www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel-coronavirus-(2019-ncov). Published 2020. Accessed March 18, 2020.
- 3.Department of Health . Australian Government; Published 2020. Update from the Prime Minister on social distancing and other measures to combat coronavirus (COVID-19)https://www.health.gov.au/news/update-from-the-prime-minister-on-social-distancing-and-other-measures-to-combat-coronavirus-covid-19 Available at: [Google Scholar]
- 4.Department of Health . Australian Government; Published 2020. Coronavirus (COVID-19) current situation and case numbers.https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-current-situation-and-case-numbers Available at: [Google Scholar]
- 5.Margolis SA, Ypinazar VA. Aeromedical retrieval for critical clinical conditions: 12 years of experience with the Royal Flying Doctor Service, Queensland, Australia. J Emerg Med. 2009;36:363–368. doi: 10.1016/j.jemermed.2008.02.057. [DOI] [PubMed] [Google Scholar]
- 6.Le Cong M, Gynther B, Hunter E, Schuller P. Ketamine sedation for patients with acute agitation and psychiatric illness requiring aeromedical retrieval. Emerg Med J. 2012;29:335. doi: 10.1136/emj.2010.107946. [DOI] [PubMed] [Google Scholar]
- 7.Royal Flying Doctor Service Victoria. Annual report. Royal Flying Doctor ServiceVictoria. Available at: https://rfds-media.s3.amazonaws.com/documents/RFDS_Annual_Report_2018_VICTORIA_web_2.pdf?AWSAccessKeyId=AKIA57J6V557HP5WJ6WZ&Expires=1580944769&Signature=5IPwHq4s8clhm%2BbOlKKYu5R6rvo%3D. Published 2018. Accessed February 6, 2020.
- 8.International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Available at: https://icd.who.int/browse10/2016/en. Published 2016. Accessed July 1, 2019.
- 9.Gardiner FW, Bishop L, Gale L, et al. Poor access to kidney disease management services in susceptible patient populations in rural Australia is associated with increased aeromedical retrievals for acute renal care [epub ahead of print]. Intern Med J. doi: 10.1016/j.amj.2020.03.001. Accessed. [DOI] [PubMed]
- 10.Brailsford S, Churilov L, Dangerfield B. John Wiley & Sons, Ltd; Hoboken, NJ: 2014. Discrete‐Event Simulation and System Dynamics for Management Decision Making. [Google Scholar]
- 11.Zhang X. Application of discrete event simulation in health care: a systematic review. BMC Health Serv Res. 2018;18:687. doi: 10.1186/s12913-018-3456-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gardiner F, Gale L, Ransom A, Laverty M. The Royal Flying Doctor Service; Published 2018. Looking ahead: responding to the health needs of country Australians in 2028- the centenary year of the RFDS.https://rfds-media.s3.amazonaws.com/documents/RN064_Looking_Ahead_Report_D3.pdf?Signature=3Z60TPlMc%2F8BwsdLpC7qIfezZX4%3D&AWSAccessKeyId=AKIAJJRKZ3AFU5ZOK5FQ&Expires=1571113335 Available at: Accessed February 2 2020. [Google Scholar]
- 13.Wang JH-S, Tan S, Raubenheimer K. Rethinking the role of senior medical students in the COVID-19 response [epub ahead of print]. Med J Aust. doi: 10.1016/j.amj.2020.03.001. Accessed April 1 2020. [DOI] [PMC free article] [PubMed]
- 14.Chang AB, Grimwood K, Maguire G, King PT, Morris PS, Torzillo PJ. Management of bronchiectasis and chronic suppurative lung disease in Indigenous children and adults from rural and remote Australian communities. Med J Aust. 2008;189:386–393. doi: 10.5694/j.1326-5377.2008.tb02085.x. [DOI] [PubMed] [Google Scholar]
- 15.Australian Institute of Health and Welfare . AIHW; Canberra, Australia: 2019. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2015. [Google Scholar]
- 16.Fox GJ, Trauer JM, McBryde E. Modelling the impact of COVID-19 upon intensive care services in New South Wales [epub ahead of print]. Med J Aust. doi: 10.1016/j.amj.2020.03.001. Accessed April 3 2020. [DOI] [PMC free article] [PubMed]
- 17.Hunter P. The spread of the COVID-19 coronavirus: health agencies worldwide prepare for the seemingly inevitability of the COVID-19 coronavirus becoming endemic. EMBO Rep. 2020;21:e50334. doi: 10.15252/embr.202050334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health. 2020;25:278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Australian Institute of Health and Welfare . AIHW; Canberra, Australia: 2018. Australia's Health 2018. [Google Scholar]
- 20.Al-Yaman F. The Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people, 2011. Public Health Res Pract. 2017;27 doi: 10.17061/phrp2741732. [DOI] [PubMed] [Google Scholar]
- 21.Gardiner FW, Bishop L, Gale L, et al. Poor access to kidney disease management services in susceptible patient populations in rural Australia is associated with increased aeromedical retrievals for acute renal care [epub ahead of print]. Intern Med J. doi: 10.1016/j.amj.2020.03.001. Accessed April 3 2020. [DOI] [PubMed]