Abstract
Background.
The YMCA of USA has adopted Healthy Eating and Physical Activity (HEPA) Standards for its afterschool programs (ASPs). Little is known about strategies YMCA ASPs are implementing to achieve Standards and these strategies’ effectiveness.
Aims.
(1) Identify strategies implemented in YMCA ASPs and (2) evaluate the relationship between strategy implementation and meeting Standards.
Method.
HEPA was measured via accelerometer (moderate-to-vigorous-physical-activity [MVPA]) and direct observation (snacks served) in 20 ASPs. Strategies were identified and mapped onto a capacity building framework (Strategies To Enhance Practice [STEPs]). Mixed-effects regression estimated increases in HEPA outcomes as implementation increased. Model-implied estimates were calculated for high (i.e., highest implementation score achieved), moderate (median implementation score across programs), and low (lowest implementation score achieved) implementation for both HEPA separately.
Results.
Programs implemented a variety of strategies identified in STEPs. For every 1-point increase in implementation score 1.45% (95% confidence interval = 0.33% to 2.55%, p ≤ .001) more girls accumulated 30 min/day of MVPA and fruits and/or vegetables were served on 0.11 more days (95% confidence interval = 0.11-0.45, p ≤ .01). Relationships between implementation and other HEPA outcomes did not reach statistical significance. Still regression estimates indicated that desserts are served on 1.94 fewer days (i.e., 0.40 vs. 2.34) in the highest implementing program than the lowest implementing program and water is served 0.73 more days (i.e., 2.37 vs. 1.64).
Conclusions.
Adopting HEPA Standards at the national level does not lead to changes in routine practice in all programs. Practical strategies that programs could adopt to more fully comply with the HEPA Standards are identified.
Keywords: child health, health policy, out of school time, physical activity/exercise, youth
Childhood obesity has reached epidemic proportions in the United States, with 1 in every 5 elementary-aged child (i.e., 6-11 years) considered obese (Ogden et al., 2016). Thus, identifying effective strategies to combat childhood obesity is an important public health goal. Recognizing the tremendous potential of their programming to contribute to the fight against childhood obesity, the YMCA of USA adopted Healthy Eating and Physical Activity (HEPA) Standards for all of its afterschool programs in November of 2011. This step is substantial because the YMCA of USA operates afterschool programs for children from all walks of life in more than 10,000 communities around the country, and these HEPA Standards have the potential to positively affect the health of the 9 million youth served by these programs.1 The Standards call for YMCA afterschool programs to provide 30 minutes of physical activity (interpreted as moderate-to-vigorous-physical-activity [MVPA] for the purpose of this study) to all children, and to serve a fruit or vegetable and water daily while eliminating sugar-sweetened foods and beverages, fried foods, and foods with trans-fat.2 Standards also indicate that programs should serve whole grains when grains are served and low (1%) to no fat milk if milk is offered. Additionally, Standards provide guidelines for programs to follow in order to create a HEPA friendly environment. These guidelines include restricting access to vending machines, reducing screen time, staff role modeling, and getting families involved through informational materials.
However, the adoption of standards does not always lead to changes in routine practice. How standards are communicated to programs and local priorities that conflict with national standards play a role in whether standards are achieved at the local level (Amis, Wright, Dyson, Vardaman, & Ferry, 2012; Barroso et al., 2009; Beets, Webster, Saunders, & Huberty, 2013). Thus, identifying practices adopted by practitioners to achieve the HEPA Standards is important as afterschool programs must identify appropriate strategies and implement these strategies with minimal outside assistance or resources. In many cases, this laissez-faire approach to policy adoption may lead to some period of trial and error before settling on strategies that work. Moreover, evaluating strategies in terms of their degree of efficacy for achieving the HEPA Standards can help identify strategies that are more likely to be effective at influencing children’s HEPA. These strategies can then be packaged and disseminated to other programs as a guide. The purposes of this study are to (1) identify the strategies for the achieving the HEPA Standards implemented in YMCA afterschool programs in one southeastern state and (2) evaluate if implementing more strategies leads to higher Standards achievement.
Method
Description of the Study
All protocols and procedures were approved by the institutional review board of the University of South Carolina. Data represent baseline from a single southeastern state’s initiative to achieve the YMCA HEPA Standards. A total of 21 YMCA associations operate independently across the state. YMCA associations were located within specific geographic regions and operated under a centralized organizational structure. One association did not operate an afterschool program and, therefore, was not included in the sample. The remaining 20 associations collectively operated 102 programs, with a median of 4 programs per association (range 1-13 programs). Based on fall 2014 enrollment, these programs served 5,244 children aged 5 to 12 years. Afterschool programs were operated in YMCA facilities (25%), schools (64%), and community locations (11%). The sample for this study was drawn from YMCA and school settings exclusively, due to the small number of programs operating in community locations (i.e., churches or apartment complexes).
Sampling for this study was designed to ensure variability of afterschool program characteristics (size, socioeconomic status, etc.) across the state run by different YMCA associations (see Figure 1). A two-stage process was followed to select a sample of participant afterschool programs. First, a single program from each of the 20 YMCA partner associations was included. This was deliberate given differences in organizational structure and capacity across the associations, the need to ensure representativeness of afterschool programs dispersed geographically throughout the state, and to include all YMCA associations in the state. Second, to ensure sufficient sample size at the child level and representativeness of programs of all sizes, programs were grouped by association and, then, stratified by enrollment. For associations that operated a single program (n = 5), that program was selected. For associations that operated two or more programs (n = 15), the following sampling strategy was adopted. Where all programs within an association enrolled fewer than 50 children (n = 3), the largest program was selected. For associations (n = 12) that operated programs with more than 50 children enrolled, a single program was randomly selected.
Figure 1.
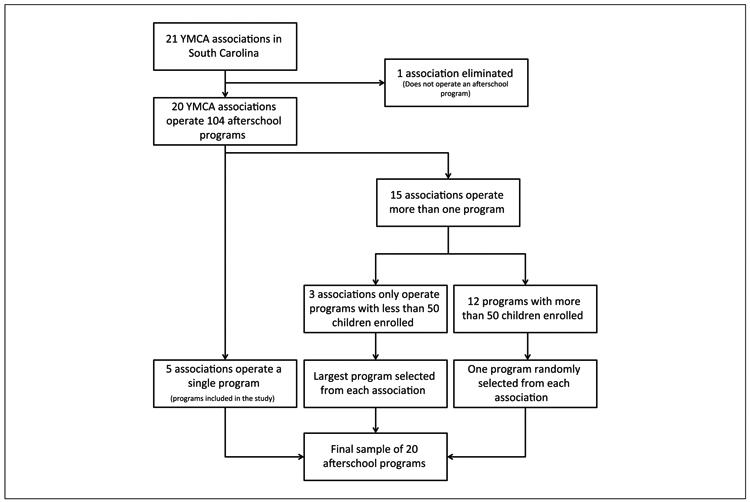
Flow chart of sampling process.
Strategy Implementation Data Collection
Strategy implementation data were collected concurrently with HEPA data (i.e., physical activity via accelerometry and snacks served via direct observation) during spring 2015 using established protocols (Beets, Weaver, Turner-McGrievy, Huberty, Ward, Freedman, et al., 2015; Weaver, Beets, Huberty, et al., 2015). Implementation data collection was guided by Strategies to Enhance Practice (STEPs) for HEPA. STEPs is a multicomponent framework for identifying program components to create HEPA-friendly environments (Beets et al., 2014; Beets, Weaver, Turner-McGrievy, Huberty, Ward, Freedman, et al., 2015; Beets, Weaver, Turner-McGrievy, Huberty, Ward, Pate, et al., 2015). STEPs includes characteristics of programs that are under the control of program leaders and staff, easily modifiable, and low-to-no cost to modify. Characteristics included in STEPs were selected based on a systematic review of theory, “best practices” position statements, literature on competencies for school-wide and out-of-school time physical activity promotion, policy documents, and empirical evidence collected within afterschool programs. STEPs has been used in interventions to identify and modify afterschool program components to increase children’s MVPA, and the quality of snacks served (Weaver, Beets, Hutto, et al., 2015). STEPs data were collected via document review, observation, the System-for-Observing-Staff-Promotion-of-Activity-and-Nutrition (Weaver, Beets, Webster, & Huberty, 2014), and the Healthy Afterschool Activity and Nutrition Documentation instrument (Ajja, Beets, Huberty, Kaczynski, & Ward, 2012). For a complete list of implementation variables included in the STEPs framework and their operational definitions, see Table 1. The STEPs framework is founded on the notion that programs with more of the capacity building components in place will also be closer to attaining the benchmarks set forth in the YMCA HEPA Standards.
Table 1.
Framework for Mapping, Data Source, Definition, and Index Coding Procedures for the STEPs for Physical Activity Promotion Variables.
| Index score coding procedure |
|||||
|---|---|---|---|---|---|
| Variable | Data source | Definition | Green (full implementation) |
Yellow (partial implementation) |
Red (no implementation) |
| STEPs physical activity foundational index score | |||||
| Schedule level of detail | Document review of schedule | Detailed schedules define activity type (snack, homework, physical activity), location, staff roles, and materials. Limited detail schedules define at least one of the items above and none indicates the site has no schedule. | Detailed schedule | Limited detail | None |
| Scheduled activity time | Document review of schedule | Total number of minutes dedicated to physical activity opportunities on the afterschool programs’ schedule | More than 60 minutes | 60 minutes | Less than 60 minutes |
| Physical activity is the only option | Document review of schedule | Total number of minutes dedicated exclusively to physical activity (i.e., children must choose a physical activity) | More than 60 minutes | 60 minutes | Less than 60 minutes |
| Number of days all staff wore physically active clothing | Direct observation | Active clothing defined as clothes that would not restrict staff from participating in activity with children (e.g., tennis shoes) | Every day | Some days | No days |
| Days a schedule was posted | Direct observation | Schedule posted in plain sight of parents at the program | Every day | Some days | No days |
| Quantity of staff physical activity trainings | HAAND | More than 1 hour/year | Less than 1 hour/year | No training for HE promotion | |
| STEPs physical activity quality index score | |||||
| Staff giving instructions | SOSPAN | Staff are giving instructions (i.e., other than PA instructions) to children | Observed rarelya | Observed sometimesa | Observed mosta |
| Staff disciplining children | SOSPAN | Children are being disciplined by staff | Observed rarelya | Observed sometimesa | Observed mosta |
| Idle time | SOSPAN | Children are not engaged in any specific activity and are awaiting instructions from staff | Observed rarelya | Observed sometimesa | Observed mosta |
| Staff withholding PA | SOSPAN | Staff member removes a child from physical activity (i.e., present or future) or threatens to remove a child from physical activity (i.e., present or future) as a consequence for behavior | Observed rarelya | Observed sometimesa | Observed mosta |
| Children wait for their turn | SOSPAN | Children waiting their turn to play/participate | Observed rarelya | Observed sometimesa | Observed mosta |
| Elimination games | SOSPAN | Physical activity eliminates children from physical activity opportunities as it progresses | Observed rarelya | Observed sometimesa | Observed mosta |
| Small team games | SOSPAN | Children are divided into several small games (no more than 5 per team) instead of one large game | Observed mosta | Observed sometimesa | Observed rarelya |
| Staff playing with children | SOSPAN | Staff member is participating in physical activity with the children | Observed mosta | Observed sometimesa | Observed rarelya |
| Staff verbally encouraging children | SOSPAN | Staff member verbally promotes physical activity (e.g., keep going, awesome job, good effort) | Observed mosta | Observed sometimesa | Observed rarelya |
| Choice provided | SOSPAN | Children have a choice of PAs in which to participate (i.e., NOT do this or sit) | Observed mosta | Observed sometimesa | Observed rarelya |
| Outside time | SOSPAN | Percent of program time spent outside | Observed mosta | Observed sometimesa | Observed rarelya |
| Girls-only physical activity option | SOSPAN | There is a physical activity opportunity in which only girls participate | Observed mosta | Observed sometimesa | Observed rarelya |
| STEPs healthy eating foundational index score | |||||
| Schedule of daily snack offerings (snack menu) | Direct observation | The site has a snack menu for the week that the observation took place | Every day | Some days | No days |
| Days a snack menu was posted | Direct observation | Snack menu posted in plain sight of parents at the program | Every day | Some days | No days |
| Following schedule of daily snack offerings | Direct observation | The site served what was on the menu the day of the observation | Every day | Some days | No days |
| Snack cost | Document review of program receipts | The program leader is aware of the snack budget | Clear snack budget | N/A | Unclear/no snack budget |
| Location of snack purchases | Document review of program receipts | The program purchases snacks from one or several vendors on a regular basis | One or several vendors | N/A | No consistent vendor |
| Quantity of staff healthy eating trainings | HAAND | More than 1 hour/year | Less than 1 hour/year | No training for HE promotion | |
| STEPs healthy eating quality index score | |||||
| Staff eat snacks with children | SOSPAN | Staff eat provided snack with the children during snack time | Every day | Some days | No days |
| Staff verbally promote healthy eating | SOSPAN | Staff verbally encourage children to eat the healthy snack | Every day | Some days | No days |
| Staff refrain from eating inappropriate foods in front of children | SOSPAN | Staff do not eat other foods in front of children during program time | Every day | Some days | No days |
| Staff refrain from drinking inappropriate drinks in front of children | SOSPAN | Staff drink only water in front of children during program time | Every day | Some days | No days |
| Staff deliver healthy eating education | SOSPAN | Staff deliver healthy eating education (e.g., healthy eating coloring sheets/crosswords/word searches, trivia, etc.) to children | More than one observation day | One observation day | No days |
| Snack is served family style | SOSPAN | Children serve themselves from a common container | Every day | Some days | No days |
| Vending access | Direct observation | Children have access to buy foods from a vending machine during program time | No days | Some days | Every day |
Note. STEP = Strategies To Enhance Practice program; HAAND = Healthy Afterschool Activity and Nutrition Documentation Instrument; HE = health education; SOSPAN = System for Observing Staff Promotion of Physical Activity and Nutrition; PA = physical activity.
Observed rarely defined as program is in the lower tertile—lower 33% in relation to other programs at baseline, observed sometimes defined as program in the middle tertile—middle 33% in relation to other programs at baseline, and observed most is defined as program in upper tertile—upper 33% in relation to other programs at baseline.
HEPA Data Collection
Consistent with established protocols (Beets, Beighle, & Bottai, 2012; Beets, Tilley, Kim, & Webster, 2011; Beets, Wallner, & Beighle, 2010; Beets, Weaver, Turner-McGrievy, Huberty, Ward, Freedman, et al., 2015; Beets, Weaver, Turner-McGrievy, Huberty, Ward, Pate, et al., 2015; Mozaffarian et al., 2010), HEPA data were collected by trained data collectors on four unannounced nonconsecutive days in the spring of 2015. During data collection, all snack options were recorded and categorized as fruit or vegetables, water, desserts, grains (whole or non-whole grain), sugar sweetened beverages, foods with trans-fat, and fried or prefried foods (Beets et al., 2011; Beets, Weaver, Turner-McGrievy, Huberty, Ward, Freedman, et al., 2015).
Children’s physical activity levels were estimated via ActiGraph GT3X+ accelerometers (Shalimar, FL). As children arrived to the program, an accelerometer was affixed to their waist via an elastic belt. Children participated in the regularly scheduled afterschool program activities while research staff monitored children for wear compliance. Prior to departing from the program, research staff retrieved the accelerometer from children. A valid day of accelerometer data was defined as wear time ≥60 minutes (Beets et al., 2010; Beets, Huberty, & Beighle, 2012; Trost, Rosenkranz, & Dzewaltowski, 2008). A total of 1,125 children wore an accelerometer for at least 1 day with an average of 2.7 days of wear and 127.6 minutes of wear time. To account for the transitive (Baquet, Stratton, Van Praagh, & Berthoin, 2007; Vale, Santos, Silva, Soares-Miranda, & Mota, 2009) and sporadic (Bailey et al., 1995) nature of children’s activity, accelerometer data were distilled using 5-second epochs. Cutpoint thresholds related to children’s MVPA were applied to estimate activity intensity (Evenson, Catellier, Gill, Ondrak, & McMurray, 2008).
Creation of STEPs Implementation Scores
Strategies observed were compiled by program and then mapped onto the STEPs framework. To identify strategies implemented by programs, at what level these strategies were implemented, and which programs were implementing more strategies, implementation scores, as outlined in Table 1, were assigned to all afterschool programs by following a two-stage process:
Programs were assigned a score and color code for each STEPs component by implementation level. Programs were assigned red (implementation score = 0) for no implementation, yellow for partial implementation (implementation score = 1), and green for full implementation (implementation score = 2). Each afterschool program was assigned an implementation score for each of the 17 physical activity and 13 healthy eating STEPs components.
Each program received an overall implementation score for HEPA, separately; by summing all STEPs components’ implementation scores from Stage 1. For healthy eating, the possible range of scores for a single program was 0 to 26 (0 = red on all elements, 26 = green on all components). For physical activity the possible range of scores was 0 to 36 for girls and 0 to 34 for boys (one STEPs component was girl specific).
This process is consistent with previous research (Weaver, Beets, Hutto, et al., 2015; Weaver et al., 2016).
Statistical Analysis
All analyses were run using STATA version 14.0 (College Station, TX). The relationship between implementation and HEPA outcomes was evaluated using two modeling approaches. First, for physical activity, MVPA minutes accumulated by children during afterschool program time was dichotomized to represent children who achieved (i.e., ≥30 minutes MVPA/day) and failed to achieve (i.e., <30 minutes MVPA/day) the YMCA Physical Activity Standard. Multilevel mixed effect linear regression models accounting for children, nested within program estimated relationships between overall implementation score (i.e., DV) and percentage of children accumulating 30 minutes/day of MVPA (IV). Full information maximum likelihood estimators were used to account for missing data. Separate models were estimated for boys and girls. Location of operation (school vs. YMCA), percentage of households in poverty, operating revenue of the program, and number of children enrolled were included as fixed effects covariates. Second, the relationship between healthy eating outcomes and implementation was estimated using multilevel mixed effect linear regression models accounting for days nested, within programs. Number of days that fruits or vegetables, water, milk, desserts, sugar sweetened beverages, and whole grains were served were the dependent variables, while overall implementation score was the independent variable. Separate models were estimated for each healthy eating outcome and the same covariates as the physical activity models were included. Models were not estimated for fried foods or foods with trans-fat because they were never observed. For all analyses, alpha levels were set at p < .05.
Following estimation of the analytical models, outcomes by high, moderate, and low implementation were calculated based on model estimates to illustrate the relationship between implementation and standard achievement. It was hypothesized that higher implementation would lead to higher achievement of HEPA outcomes. High implementation was considered the maximum overall implementation score received by a program for healthy eating (i.e., 16) and physical activity (i.e., 27). Low was considered the minimum overall implementation score received by a program for healthy eating (i.e., 5) and physical activity (i.e., 11), while moderate implementation was considered the median implementation score across programs for healthy eating (i.e., 11) and physical activity (i.e., 19).
Results
STEPs Strategy Implementation
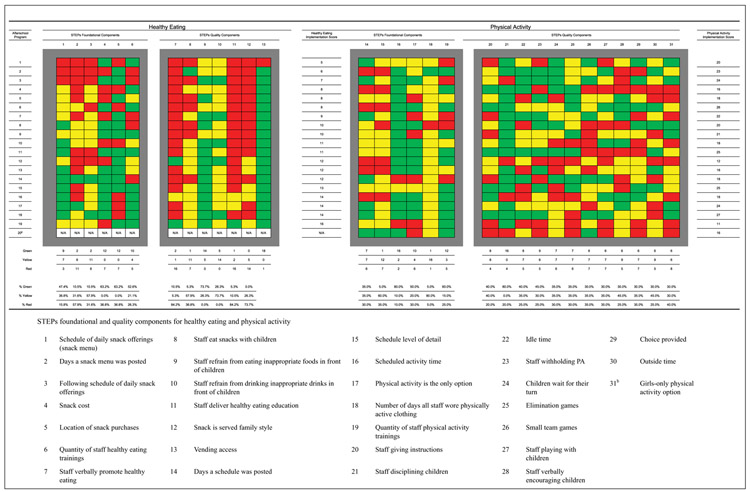
Child- and program-level characteristics of participant programs are presented in Table 2. Strategies to increase HEPA were mapped onto the STEPs framework in Figure 2. For the healthy eating, overall implementation scores ranged from 5 to 16, with a median score of 11. The most common fully implemented strategy (GREEN) was restricting children’s access to vending machines during program time (18 of 19 programs). This was followed closely by staff refraining from eating inappropriate foods in front of children (14 of 19 programs) and program leaders establishing a snack budget (n = 12). The most common partially used strategies (YELLOW) included staff refraining from drinking inappropriate beverages in front of children (n = 14), program leaders identifying a single snack vendor (n = 12), staff eating snack with children (n = 11), and following the snack menu (n = 11). The most common strategies that were not implemented included (RED) staff verbally promoting healthy eating (n = 16), delivering healthy eating education (n = 16), serving snacks family style (n = 14), and posting the snack menu in the program (n = 11).
Table 2.
Child and Program Characteristics of Participant Programs.
| Characteristics | Evaluation programs (n = 20) |
|---|---|
| Child characteristics | |
| Gender (% male) | 66 |
| Age (years; M, SD) | 7.6 (1.7) |
| Race/ethnicity (%) | |
| White non-Hispanic | 55.3 |
| African American | 31.5 |
| Other | 13.2 |
| Afterschool program characteristics | |
| Average number of children enrolled (M, SD) | 70 (39) |
| Average percent of population in poverty (M, SD) | 13.6 (6.0) |
| Average number of staff (M, SD) | 8.3 (5.0) |
| Average available indoor space sq ft (M, SD) | 9,128 (4,386) |
| Average available outdoor space sq ft (M, SD) | 137,755 (87,095) |
| Programs located at YMCAs | 44% |
| Programs located at schools | 56% |
| Amount of physical activity training for staff | |
| Staff receive no training | 25% |
| Staff receive less than 1 hour of training | 15% |
| Staff receive 1 to 4 hours of training | 50% |
| Staff receive more than 4 hours of training | 10% |
| Amount of healthy eating training for staff | |
| Staff receive no training | 25% |
| Staff receive less than 1 hour of training | 25% |
| Staff receive 1 to 4 hours of training | 35% |
| Staff receive more than 4 hours of training | 15% |
| Programs with full-time site leader | 47% |
| Programs with part-time site leader | 53% |
| Program leader educational attainment | |
| High school diploma | 11% |
| Some college | 37% |
| Bachelor’s degree | 32% |
| Graduate degree | 20% |
Figure 2.
STEPs implementation scores for healthy eating and physical activity graphically represented. Note. PA = physical activity.
aProgram did not serve snack so no STEPs implementation score for healthy eating assigned. bGirls only included in girls STEPs implementation score exclusive.
For physical activity, the median overall implementation score was 19, with a range of 11 to 27. The most common fully implemented physical activity strategies were minimizing discipline time and scheduling 60 minutes or more of physical activity with 16 programs implementing these strategies. The next most common strategy was providing staff with 1 hour or more of physical activity training annually (n = 12). Staff wearing physically active clothing (n = 18) and creating a detailed schedule of programming (n = 12) were the most common partially implemented STEPs components. Providing outdoor activity time (n = 8), a girls only physical activity opportunity (n = 7), playing small sided games (n = 7), providing physical activity choices (n = 7), and creating a detailed schedule of programming (n = 7) were the most common STEPs components that were not implemented.
Relationship of STEPs Strategy Implementation to HEPA
The relationship between STEPs implementation and HEPA is presented in Table 3. For healthy eating, all relationships were in the hypothesized direction and there was a clear stair stepping pattern from the lowest implementer to the highest implementer in relation to the number of days foods and beverages were served. The relationship between overall implementation score and days fruits or vegetables were served (0.28 day increase for every 1-point increase in overall implementation score, 95% confidence interval [CI; 0.11 to 0.45], p = .001) was statistically significant. Relationships between overall implementation score and number of days water (0.07 day increase for every 1-point increase in overall implementation score, 95% CI [−0.17 to 0.30], p = .59), whole grains (0.03 day increase for every 1-point increase in overall implementation score, 95% CI [−0.05 to 0.12], p = .43), low or non-fat milk (0.10 day increase for every 1-point increase in overall implementation score, 95% CI [−0.07 to 0.27], p = .24), desserts (0.18 day decrease for every 1-point increase in overall implementation score, 95% CI [−0.37 to 0.02], p = .08), and sugar-sweetened beverages (0.05 day decrease for every 1-point increase in overall implementation score, 95% CI [−0.17 to 0.06], p = .38) did not reach statistical significance. For physical activity, the relationship between overall implementation score and the percentage of girls and boys accumulating 30 minutes/day of MVPA was in the hypothesized direction and there was a clear stair stepping pattern from the lowest implementer to the highest implementer. However, the relationship between implementation and the percentage of boys accumulating 30 minutes/day of MVPA did not reach statistical significance (0.78% increase for every 1-point increase in overall implementation score, 95% CI [−0.83% to 2.39%], p = .34), while it did for girls (1.45% increase for every 1- point increase in overall implementation score, 95% CI [0.33% to 2.55%], p = .01).
Table 3.
Differences in Healthy Eating and Physical Activity by Level of Implementation.
| Variable | Low implementation (minimum implementation score recorded) |
Moderate implementation (median implementation score recorded) |
High implementation (maximum implementation score recorded) |
Change for every 1 point increase in overall implementation scorea |
95% CI | p |
|---|---|---|---|---|---|---|
| Healthy eating | ||||||
| Fruit or vegetableb (e.g., fresh, frozen, or dried) | 0.59 | 2.26 | 3.64 | 0.28 | [0.11, 0.45] | .001 |
| Waterb (e.g., plain unflavored) | 1.64 | 2.04 | 2.37 | 0.07 | [−0.17, 0.30] | .59 |
| Whole grains (e.g., breads where whole grain is the first ingredient on the package) | 0.56 | 0.76 | 0.93 | 0.03 | [−0.05, 0.12] | .43 |
| Milk (e.g., 1% or nonfat milk) | 0.41 | 1.02 | 1.52 | 0.10 | [−0.07, 0.27] | .24 |
| Dessertsb (e.g., Trix yogurt, cookies, Pop-Tarts, chocolate, frozen treats) | 2.34 | 1.28 | 0.40 | −0.18 | [−0.37, 0.02] | .08 |
| Sugar-sweetened beveragesb (e.g., soda, powered drink mixed, sport drinks, chocolate milk) | 0.64 | 0.33 | 0.07 | −0.05 | [−0.17, 0.06] | .38 |
| Foods with trans-fatb,c | 0.00 | 0.00 | 0.00 | — | — | — |
| Fried or prefried foodsb,c | 0.00 | 0.00 | 0.00 | — | — | — |
| Physical activity | ||||||
| Boys accumulating 30 minutes/day of MVPAd | 37.47% | 43.72% | 49.96% | 0.78% | [−0.83%, 2.39%] | .34 |
| Girls accumulating 30 minutes/day of MVPAd | 7.27% | 18.84% | 30.41% | 1.45% | [0.33%, 2.55%] | .01 |
Note. CI = confidence interval; MVPA = moderate-to-vigorous physical activity. Statistically significant differences at <.05 are bolded.
Based on linear regression models.
Number of days per week item served.
Regression analyses not estimated because items were never observed.
Percentage of children accumulating 30 minutes/day of MVPA.
Discussion
This study investigated the implementation of strategies by YMCA afterschool programs to achieve YMCA HEPA Standards 4 years following initial adoption of the Standards. Afterschool programs used a variety of strategies identified in the STEPs framework and high implementation was related to serving fruits or vegetables on more days, and higher levels of physical activity for girls.
STEPs Strategy Implementation
For healthy eating, the majority of programs with high implementation scores had a snack menu every day and a snack budget, while few programs with low implementation had a snack menu or a snack budget. Planning a menu of snacks to serve and budgeting for snack purchases seems to be related to serving healthier snacks. This is not surprising as it logically follows that programs that plan a snack menu are consciously choosing snacks to be served and, in turn, are more likely to comply with the HEPA Standards. Creating a snack menu and budget are simple inexpensive strategies for programs to achieve the YMCA HEPA Standards.
Staff at few programs verbally promoted healthy eating, delivered healthy eating education, served snacks family style, or refrained from drinking inappropriate beverages in front of children. Why programs struggled to model healthy eating is unclear as the majority of programs provided at least some training on healthy eating (i.e., 14 programs). However, these trainings may not have included content on encouraging and modeling healthy eating. Incorporating training on verbal promotion, delivering healthy eating education, and serving snack family style into existing training opportunities could help staff integrate these strategies into routine practice. Additionally, there are a variety of healthy eating curricula that could be adopted by afterschool programs looking to increase healthy eating promotion and healthy eating education. Curricula like Food and Fun3 and Commit to Health4 are freely available online and have been developed specifically for afterschool programs. Training staff to incorporate these curricula into their programs may lead to increase healthy eating promotion, education, and role modeling.
For physical activity, the majority of programs provided ample time (i.e., 60 minutes or more) for physical activity opportunities (Brazendale et al., 2014). However, there is evidence that this time was not used effectively. For instance, programs did not provide detailed schedules for staff and many programs allowed children to choose sedentary activities during scheduled activity time. Less detailed schedules can lead to increased idle time as staff decide what games to play, gather appropriate equipment, and explain rules to children (Weaver, Beets, Saunders, & Beighle, 2014). Furthermore, allowing children to choose sedentary activities during scheduled activity time leads to lower activity levels for some children and is contrary to the YMCA Standard of providing “all” children with 30 minutes/day of activity during program time (i.e., some children may choose not to participate in physical activity).
Relationship of STEPs Implementation to HEPA
Implementation of a greater number of strategies included in the STEPs framework during routine practice was associated with higher levels of MVPA for both boys and girls. However, the relationship between the percentage of boys accumulating 30 minutes/day of MVPA and implementation level was not statistically significant. It is unclear what physical activity promotion strategies included in STEPs would affect girls’ and not boys’ MVPA. One possible explanation for the muted effect on boys’ MVPA is the manner in which afterschool programs scheduled activity opportunities. Most programs in this study scheduled 60 minutes or more for activity time daily (n = 16 programs). However, half of the programs included sedentary options during activity opportunities (n = 10 programs). For example, children could choose to play an active game in the gym or participate in arts and crafts in a classroom. Boys may be more likely than girls to choose active opportunities. This is consistent with the finding that boys are more active than girls in all settings (Troiano et al., 2008) including afterschool programs (Trost et al., 2008). Thus, simply providing ample time for physical activity may be sufficient to get boys more active, while ensuring that physical activity is the only option may be important for increasing girls’ activity. For instance, programs in this study that had at least 40% of boys accumulating 30 minutes/day of MVPA (n = 10) scheduled 34 more minutes of activity opportunities than programs that did not have 40% of boys accumulating 30 minutes/day of MVPA (113.5 minutes vs. 79.5 minutes).
It is important to note that not all programs with high levels of implementation also demonstrated high levels of MVPA. For instance, the program with the second highest implementation score (i.e., 26) only had the 13th highest percentage of boys accumulating 30 minutes/day of MVPA (i.e., 23.4%). The reason that high implementers are not all achieving the 30 minutes/day of MVPA guideline at a high level is unclear. One explanation is that the some key STEPs components may need to be in place prior to implementing other STEPs components. For example, a program may provide training to all staff for promoting MVPA, but might fail to provide adequate time for physical activity in the program schedule. The opposite is also true; programs may adopt one key strategy that leads to higher levels of physical activity while neglecting other strategies. Understanding why strategies included in STEPs are more effective in some programs and if there are certain key “active ingredients” that drive achievement of the HEPA Standards is crucially important. Identifying these strategies can help in the design of more effective interventions for achieving the HEPA Standards across all YMCA afterschool programs (Craig et al., 2008). Unfortunately, answering this question would take a larger and more diverse sample than the one included in the current study. Nonetheless, it does appear that, on average, if programs are implementing more physical activity promotion strategies they are more likely to experience increases in the percentage of girls accumulating 30 minutes/day of MVPA.
For healthy eating, high implementation was related to serving more fruits and/or vegetables, water, whole grains, and low or non-fat milk on more days and desserts and sugar-sweetened beverages on fewer days per week. No programs were ever observed serving foods with trans-fat or fried foods. Days per week a fruit or vegetable was served was the only statistically significant difference. However, the differences between the highest and lowest implementers appear to be meaningful. For instance, the highest implementer served milk one more day per week and desserts almost 2 fewer days per week. While these differences are not statistically significant an additional serving of milk and 2 fewer servings of desserts per week are meaningful changes in children’s diets. Furthermore, these changes have been shown to increase important micro- and macronutrients along with changing the nutrient profile of snacks (Beets, Turner-McGrievy, et al., 2015). These findings suggest that programs that implement healthy eating promotion strategies consistent with the STEPs framework will see meaningful changes in the nutritional quality of snacks served. This finding is also consistent with previous research (Beets, Weaver, Turner-McGrievy, Huberty, Ward, Freedman, et al., 2015; Weaver, Beets, Hutto, et al., 2015).
This study provides important low to no cost strategies that practitioners can adopt should they want to increase compliance with the YMCA HEPA Standards. The first strategy identified herein is developing a snack menu. This may lead to increased awareness of the snacks being served and in turn increased compliance with the YMCA HEPA Standards. Second, providing 60 minutes of physical activity opportunities appears to be a simple strategy for getting boys to be physically active. However, this is not the case for girls. Ensuring that other nonactive opportunities (i.e., enrichment, computer time) are not offered alongside physical activity opportunities may be important for increasing girls’ physical activity. These are simple, commonsense strategies that practitioners can adopt with limited to no added cost.
This study has several strengths, including using objective process and outcome measures, statistical modeling to test the STEPs framework’s relationship to HEPA achievement, and the diversity of programs included (small and large enrollments, varying physical space/amenities, varying program locations). This study also has limitations. First the generalizability of these findings to other states and regions across the country may be limited, especially given the limited number of programs included in the sample (N = 20). Modeling relationships of STEPs to program-level outcomes limits the study’s power to detect statistically significant relationships. Furthermore, all relationships are cross-sectional; therefore, cause and effect between STEPs components and HEPA cannot be established. Finally, the act of observing staff may have influenced staff behaviors. However, observation days were unannounced limiting the ability of staff to prepare for observations and change the program drastically. Visits by research staff prior to data collection and conducting observation on four program days also familiarized staff with and acclimated staff to observation.
In conclusion, this study found that the adoption of the Standards alone does not always lead to changes in routine practice. Four years after the adoption of the YMCA HEPA Standards, there is still large variability in compliance. This study used a capacity building framework (STEPs) to identify low-cost and effective strategies programs can adopt to more closely align routine practice with HEPA Standards. Programs that implemented more STEPs components in this study showed increased MVPA for girls and quality of snacks, suggesting that the strategies contained within STEPs can be used for identifying and modifying key program components for HEPA interventions. If the HEPA Standards are to have the desired effect of increasing children’s MVPA and the quality of snacks served during program time, future research needs to continue to identify resources to help programs achieve the HEPA Standards as well as strategies to ensure that these resources are accessed.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this article was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number RO1HD079422.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ajja R, Beets MW, Huberty J, Kaczynski AT, & Ward DS (2012). The healthy afterschool activity and nutrition documentation instrument. American Journal of Preventive Medicine, 43, 263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amis JM, Wright PM, Dyson B, Vardaman JM, & Ferry H (2012). Implementing childhood obesity policy in a new educational environment: The cases of Mississippi and Tennessee. American Journal of Public Health, 102, 1406–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey RC, Olson J, Pepper SL, Porszaz J, Barstow TJ, & Cooper DM (1995). The level and tempo of children’s physical activities: An observational study. Medicine & Science in Sports & Exercise, 27, 1033–1041. [DOI] [PubMed] [Google Scholar]
- Baquet G, Stratton G, Van Praagh E, & Berthoin S (2007). Improving physical activity assessment in prepubertal children with high-frequency accelerometry monitoring: A methodological issue. Preventive Medicine, 44, 143–147. [DOI] [PubMed] [Google Scholar]
- Barroso CS, Kelder SH, Springer AE, Smith CL, Ranjit N, Ledingham C, & Hoelscher DM (2009). Senate Bill 42: Implementation and impact on physical activity in middle schools. Journal of Adolescent Health, 45(3), S82–S90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Beighle A, & Bottai M (2012). Pedometer-determined step count guidelines for afterschool programs. Journal of Physical Activity and Health, 9, 71–77. [DOI] [PubMed] [Google Scholar]
- Beets MW, Huberty J, & Beighle A (2012). Physical activity of children attending afterschool programs research- and practice-based implications. American Journal of Preventive Medicine, 42, 180–184. doi: 10.1016/j.amepre.2011.10.007 [DOI] [PubMed] [Google Scholar]
- Beets MW, Tilley F, Kim Y, & Webster C (2011). Nutritional policies and standards for snacks served in after-school programmes: A review. Public Health Nutrition, 14, 1882–1890. doi: 10.1017/S1368980011001145 [DOI] [PubMed] [Google Scholar]
- Beets MW, Turner-McGrievy B, Weaver RG, Huberty J, Moore JB, Ward DS, & Freedman DA (2015). Intervention leads to improvements in the nutrient profile of snacks served in afterschool programs: A group randomized controlled trial. Translational Behavioral Medicine, 6, 329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Wallner M, & Beighle A (2010). Defining standards and policies for promoting physical activity in afterschool programs. Journal of School Health, 80, 411–417. doi: 10.1111/j.1746-1561.2010.00521.x [DOI] [PubMed] [Google Scholar]
- Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward D, Freedman DA, … Moore JB (2014). Making healthy eating and physical activity policy practice: The design and overview of a group randomized controlled trial in afterschool programs. Contemporary Clinical Trials, 38, 291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward DS, Freedman D, … Beighle A (2015). Making healthy eating policy practice: A group randomized controlled trial on changes in snack quality, costs, and consumption in afterschool programs. American Journal of Health Promotion, 48, 694–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward DS, Pate RR, … Beighle A (2015). Making physical activity policy practice: A group randomized controlled trial on changes in moderate-to-vigorous physical activity in afterschool programs. American Journal of Preventive Medicine, 48, 694–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Webster C, Saunders R, & Huberty JL (2013). Translating policies into practice: A framework to prevent childhood obesity in afterschool programs. Health Promotion Practice, 14, 228–237. [DOI] [PubMed] [Google Scholar]
- Brazendale K, Beets MW, Weaver RG, Huberty J, Beighle AE, & Pate RR (2014). Wasting our time? Allocated versus accumulated physical activity in afterschool programs. Journal of Physical Activity & Health, 12, 1061–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, & Petticrew M (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance. British Medical Journal, 337, a2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, & McMurray RG (2008). Calibration of two objective measures of physical activity for children. Journal of Sports Science, 26, 1557–1565. [DOI] [PubMed] [Google Scholar]
- Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, & Gortmaker SL (2010). Impact of an organizational intervention designed to improve snack and beverage quality in YMCA after-school programs. American Journal of Public Health, 100, 925–932. doi: 10.2105/ajph.2008.158907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, & Flegal KM (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. Journal of the American Medical Association, 315, 2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, MÂSse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40, 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Trost SG, Rosenkranz RR, & Dzewaltowski D (2008). Physical activity levels among children attending after-school programs. Medicine & Science in Sports & Exercise, 40, 622–629. doi: 10.1249/MSS.0b013e318161eaa5 [DOI] [PubMed] [Google Scholar]
- Vale S, Santos R, Silva P, Soares-Miranda L, & Mota J (2009). Preschool children physical activity measurement: Importance of epoch length choice. Pediatric Exercise Science, 21, 413–420. [DOI] [PubMed] [Google Scholar]
- Weaver R, Beets M, Webster C, & Huberty J (2014). System for Observing Staff Promotion of Activity and Nutrition (SOSPAN). Journal of Physical Activity & Health, 11, 173–185. [DOI] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Huberty J, Freedman D, Turner-Mcgrievy G, & Ward D (2015). Physical activity opportunities in afterschool programs. Health Promotion Practice, 16, 371–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Hutto B, Saunders R, Moore JB, Turner-McGrievy G, … Freedman D (2015). Making healthy eating and physical activity policy practice: Process evaluation of a group randomized controlled intervention in afterschool programs. Health Education Research, 30, 849–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Saunders RP, & Beighle A (2014). A coordinated comprehensive professional development training’s effect on summer day camp staff healthy eating and physical activity promoting behaviors. Journal of Physical Activity & Health, 11, 1170–1178. [DOI] [PubMed] [Google Scholar]
- Weaver RG, Moore JB, Huberty J, Freedman D, Turner-McGrievy G, Beighle A, … Beets MW (2016). Process evaluation of making HEPA policy practice: A group randomized trial. Health Promotion Practice, 17, 631–647. [DOI] [PMC free article] [PubMed] [Google Scholar]