Abstract
Background:
Medicaid expansion substantially increased health insurance coverage, but its effect on the delivery of preventative health care is unclear.
Objectives:
To assess the impact of Medicaid expansion on the receipt of 15 different measures of preventive care including cancer screening, cardiovascular risk reduction, diabetes care, and other primary care measures.
Research Design:
We performed a serial cross-sectional analysis of BRFSS survey data from 2012 to 2017. We used a quasi‐experimental design with difference‐in‐differences (DiD) analyses to examine changes in preventative health care delivery over three time periods in Medicaid expansion compared with non-expansion states.
Subjects:
We included low-income (<138% FPL) non-elderly (age<65) adults residing in 46 U.S. states.
Measures:
Our predictor was residing in a Medicaid expansion state (24 states) versus non-expansion state (19 states). Our primary outcomes were preventative health care services, which we categorized as cancer screening (breast cancer, cervical cancer, and colorectal cancer); cardiovascular risk reduction (serum cholesterol screening in low-risk groups, serum cholesterol monitoring in high-risk groups, and aspirin use); diabetes care (serum cholesterol monitoring, Hemoglobin A1c monitoring, foot examination, eye examination, and influenza vaccination, and pneumonia vaccination), and other primary care measures (influenza vaccination, alcohol use screening, and HIV screening).
Results:
Survey responses from 500,495 low-income non-elderly adults from 2012 to 2017 were included in the analysis, representing 68.2 million U.S. adults per year. Of the 15 outcomes evaluated, we did not detect statistically significant differences in cancer screening (3 outcomes), cholesterol screening or monitoring (2 outcomes), diabetes care (6 outcomes), or alcohol use screening (1 outcome) in expansion compared to non-expansion states. Aspirin use (DiD 8.8%, p<0.001), influenza vaccination (DiD 1.4%, p = 0.016), and HIV screening (DiD 1.9%, p = 0.004) increased in expansion states compared to non-expansion states.
Conclusions:
Medicaid expansion was associated with an increase in aspirin use, influenza vaccination, and HIV screening in expansion states. Despite improvements in access to care, including health insurance, having a primary care doctor, and routine visits, Medicaid expansion was not associated with improvements in cancer screening, cholesterol monitoring, diabetes care, or alcohol use screening. Our findings highlight implementation challenges in delivering high quality primary care to low-income populations.
Keywords: Medicaid Expansion, Health Care Reform, Insurance Access, Primary Care, Quality of Care, Affordable Care Act
Introduction
State and national policies to increase health insurance coverage aim to improve access to health care services, including primary care and preventative health. Delivery of optimal preventative care has been demonstrated to prevent the development of chronic disease, reduce health care utilization, and improve life expectancy.(Oster, 2003 #3)(Macinko, 2003 #4) However, efforts to expand health insurance coverage have had inconsistent success in improving the delivery of preventative health services. The Oregon Health Insurance Experiment, which provided Medicaid coverage to low-income non-elderly adults via a randomized lottery, increased diabetes diagnosis and management and cancer screening, but did not show improvements in the diagnosis or treatment of hypertension or hyperlipidemia in the first two years.1 More recently, the Patient Protection and Affordable Care Act resulted in the expansion of Medicaid coverage to adults with an income <138% of the Federal Poverty Level (FPL) in participating states. Medicaid expansion substantially increased health insurance coverage: the number of Medicaid-covered persons in the U.S. increased by over 7 million from 2013 to 2016.(Berchick ER, #50) Several analyses have confirmed that insurance coverage and having a primary care physician improved in Medicaid expansion states compared with non-expansion states under the Affordable Care Act.3–10
Although Medicaid expansion has been associated with increased access to care and self-reported health, an increase in the delivery of preventative care services after Medicaid expansion has not yet been consistently demonstrated.11–13 Analyses of pent-up demand in new Medicaid enrollees in Minnesota saw an increase in outpatient visits, suggesting that improvements in preventative care delivery may be expected after Medicaid expansion.(Fertig, 2018 #51) However, successfully obtaining preventative health care has been shown to require additional factors beyond solely visit attendance, including trust, continuity, and awareness of the importance of prevention.(Messina, 2017 #53) Accordingly, analyses of National Health Interview Survey data from 2014 and 2015 failed to show increases in cancer screening in low-income non-elderly adults who were targeted by the policy.14 Several studies using data from the Behavioral Risk Factor Surveillance System (BRFSS), a national telephone-based survey, showed no change in the receipt of preventive care measures including clinical diabetes care, influenza vaccinations, or cancer screening, but each study examined only a limited number of measures.13,15–17
The unclear effect of Medicaid expansion on the receipt of preventative health care points to the need for ongoing evaluation over longer time intervals. Thus, analyses of many preventative measures using the most recent data will improve the assessment of this pivotal national policy. In this study, we evaluated multiple domains of primary care to determine the effect of Medicaid expansion on the delivery of preventative health services. We update prior analyses using data from the 2017 BRFSS. Understanding the role of insurance expansion in improving provision of evidence-based primary care will gauge the need for additional targeted interventions.
Methods
Study Design and Population
We performed a serial cross-sectional analysis of the BRFSS survey. The BRFSS is a federally funded nationally representative telephone survey conducted annually since 1984 by the Centers for Disease Control in collaboration with state health departments. It collects state-level prevalence data on participant and household characteristics, health behaviors, and health services. The questionnaire is comprised of an annual standard core, a biannual rotating core, optional modules, and state-added questions. Further details about BRFSS can be found on the CDC website.17
Our sample included low-income (<138% FPL) non-elderly (age<65) adults who participated in the BRFSS survey from 2012 to 2017. We included low-income non-elderly adults as this was the population targeted by Medicaid expansion as part of the Affordable Care Act. We included participants residing in 46 U.S. states. Participants residing in Delaware, District of Columbia, Massachusetts, New York, and Vermont were excluded because they expanded Medicaid before 2014. Using household size from BRFSS data, we estimated 138% of the FPL based on the poverty guidelines in the Federal Register by the U.S. Department of Health and Human Services for program eligibility.18 Because income is a categorical variable in BRFSS, we chose the income threshold that was closest to the poverty guideline value. For example, $33,948 was 138% of the poverty guideline for a household of four in 2017, which was closest to an income threshold of less than $35,000 in BRFSS.
Predictors
Our predictor was residing in a Medicaid expansion state versus non-expansion state. We classified 24 states as expansion states and 19 as non-expansion states similar to prior analyses.14 Alaska, Louisiana, and Montana were classified as non-expansion states for the immediate 2014–2015 time period and expansion states for the late 2016–2017 time period, because they expanded Medicaid in late 2015 or 2016. We assessed three different time periods: pre-expansion (2012–2013), immediate post-expansion (2014–2015), and late post-expansion (2016–2017) to evaluate differences over time.
Outcomes
We first examined outcomes related to health care access to verify the effects of Medicaid expansion on measures of coverage and access. These included having health insurance coverage, as assessed by the question “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?” We also assessed having a primary care clinician, which was asked “Do you have one person you think of as your personal doctor or health care provider?” and getting a routine checkup within the past year.
We then assessed preventative health care services, which we categorized as cancer screening (breast cancer, cervical cancer, and colorectal cancer); cardiovascular risk reduction (serum cholesterol screening in low-risk groups, serum cholesterol monitoring in high-risk groups, and aspirin use); diabetes care (serum cholesterol monitoring, Hemoglobin A1c monitoring, foot examination, eye examination, and influenza vaccination, and pneumonia vaccination); and other primary care measures (influenza vaccination, alcohol use screening, and HIV screening). Outcomes were chosen from United States Preventative Services Task Force (USPSTF) recommendations, the CDC, and professional society guidelines, as defined in Table 1. We chose guideline recommendations that were published before or near the start of our study period in 2012.
Table 1.
Definitions of Preventative Health Services
| Preventative Health Service | Numerator | Denominator | Guideline | Strength of Recommendation | Questions in BRFSS |
|---|---|---|---|---|---|
| Cancer Screening | |||||
| Breast cancer screening | Mammogram in the past 2 years | Women age 50 to 74 | USPSTF19 | B† | “Have you ever had a mammogram?” “How long has it been since you had your last mammogram?” |
| Cervical cancer screening | Pap test in the past 3 years | Women age 21 to 65 | USPSTF20 | A* | “Have you ever had a Pap test?” “How long has it been since you had your last Pap test?” |
| Colorectal cancer screening | Colonoscopy in the past 10 years Blood stool test in the past year |
Participants age 50 to 75 | USPSTF21 | A* | “How long has it been since you had your last sigmoidoscopy or colonoscopy?” “How long has it been since you had your last blood stool test using a home kit?” |
| Cardiovascular Risk Reduction | |||||
| Serum cholesterol screening | Cholesterol checked in the past 5 years | Men age ≥35 and women age ≥45 | USPSTF22 | A* | About how long has it been since you last had your blood cholesterol checked? |
| Serum cholesterol monitoring | Cholesterol checked in the past 5 years | History of HTN, HLD, or CVD | AACE37 | C¶ | About how long has it been since you last had your blood cholesterol checked? |
| Aspirin use | Regular aspirin use | Men age 45 to 79 and woman age 55 to 79 excluding taking aspirin is unsafe | USPSTF23 | A* | Do you take aspirin daily or every other day? Do you have a health problem or condition that makes taking aspirin unsafe for you? |
| Diabetes care | |||||
| Serum cholesterol monitoring | Cholesterol checked in the past 5 years | History of DM | ADA24 | E∬ | About how long has it been since you last had your blood cholesterol checked? |
| HbA1c monitoring | HbA1c measurement in the past year | History of DM | ADA24 | E∬ | About how many times in the past 12 months has a doctor, nurse, or other health professional checked you for “A one C”? |
| Foot examination | Foot examination in the past year | History of DM | ADA24 | B† | About how many times in the past 12 months has a health professional checked your feet for any sores or irritations? |
| Eye examination | Dilated eye examination in the past year | History of DM | ADA24 | B† | When was the last time you had an eye exam in which the pupils were dilated? |
| Influenza vaccination | Flu shot in the past year | History of DM | ADA24 | C¶ | During the past 12 months, have you had either a flu shot or a flu vaccine that was sprayed in your nose? |
| Pneumonia vaccination | Pneumonia vaccination ever | History of DM | ADA24 | C¶ | A pneumonia shot or pneumococcal vaccine is usually given only once or twice in a person’s lifetime and is different from the flu shot. Have you ever had a pneumonia shot? |
| Other Primary Care | |||||
| Influenza vaccination | Flu shot in the past year | All participants | CDC ACIP25 | -- | During the past 12 months, have you had either a flu shot or a flu vaccine that was sprayed in your nose? |
| Alcohol use screening | Asked if you drink alcohol during checkup | All participants | USPSTF26 | B† | At that checkup, were you asked in person or on a form if you drink alcohol? |
| HIV screening | Ever tested for HIV | Participants age 18 to 65 | USPSTF27 | A* | Have you ever been tested for HIV? |
A - “The USPSTF recommends the service. There is high certainty that the net benefit is substantial” or “Clear evidence from well-conducted, generalizable, RCTs that are adequately powered or Supportive evidence from well-conducted randomized controlled trials that are adequately powered or Compelling nonexperimental evidence” (ADA)
B - “The USPSTF recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial” or “Supportive evidence from well-conducted cohort studies or Supportive evidence from a well-conducted case-control study” (ADA)
C - “The USPSTF recommends selectively offering or providing this service to individual patients based on professional judgment and patient preferences. There is at least moderate certainty that the net benefit is small” or “Supportive evidence from poorly controlled or uncontrolled studies or Conflicting evidence with the weight of evidence supporting the recommendation” or Recommendation grade weak (AACE).
E - “Expert consensus or clinical experience” (ADA)
BRFSS – Behavioral Risk Factor Surveillance System; USPSTF – United States Preventative Services Task Force; HTN – hypertension; HLD – hyperlipidemia; CVD – cardiovascular disease; AACE – American Association of Clinical Endocrinologists; DM – diabetes mellitus; ADA – American Diabetes Association; HbA1c – Hemoglobin A1c; CDC ACIP – Centers for Disease Control Advisory Committee on Immunization Practices; HIV – Human Immunodeficiency Virus
Breast cancer screening was assessed by the questions “Have you ever had a mammogram?” and “How long has it been since you had your last mammogram?” in women age 50 to 74.19 Cervical cancer screening was assessed by the questions “Have you ever had a Pap test?” and “How long has it been since you had your last Pap test?”20 Similarly, colorectal screening was assessed by the questions “How long has it been since you had your last sigmoidoscopy or colonoscopy?” and “How long has it been since you had your last blood stool test using a home kit?”21 Serum cholesterol screening in low-risk groups was defined as checking cholesterol in men age ≥35 and women age ≥45, whereas cholesterol monitoring in high-risk groups was defined as those with a history of hypertension, hyperlipidemia, or cardiovascular disease, according to USPSTF guidelines.22 Aspirin use was assessed in men age 45 to 79 and women age 55 to 79 according to prior USPSTF guidelines, excluding participants who reported having a health condition that makes taking aspirin unsafe.23 We included six measures of diabetes care from the American Diabetes Association guidelines: serum cholesterol monitoring, Hemoglobin A1c monitoring, foot examination, eye examination, and influenza vaccination, and pneumonia vaccination.24 Other primary care measures included influenza vaccination within the past year, alcohol use screening, and being ever tested for HIV.25–27
Statistical Analysis
We reported participant characteristics in expansion versus non-expansion states over time. We examined the unadjusted prevalences of the reported receipt of preventative health services in expansion versus non-expansion states over time. We then used a quasi‐experimental design with difference‐in‐differences (DiD) analyses to examine the change in preventative health services over the three time periods in Medicaid expansion compared with non-expansion states. We performed two comparisons: the immediate period to the baseline period, and the late period to the baseline period. We performed multivariable linear regression adjusting for patient age and sex. The outcome of aspirin use was additionally adjusted for atherosclerotic cardiovascular disease risk factors. As DiD analyses assume that the difference between the treatment and comparison groups is constant over time, we checked the parallel trend assumption by visually inspecting graphs of the outcomes over time.
In additional analyses, we examined the unadjusted change in measures of health care access per year in low-income non-elderly adults in expansion states and non-expansion states using linear regression. We then determined the change in preventative health services per year in expansion states and non-expansion states using linear regression. All analyses took into account the complex survey design and weighted sampling probabilities of the data source.
Results
Sociodemographic and Clinical Characteristics
Survey responses from 500,495 low-income non-elderly adults from 2012 to 2017 were included in the analysis, representing 68.2 million U.S. adults per year. Participants in expansion states (N = 270,067) were less likely to be black (12.5% vs. 21.5%), but were similar in age (25.3% vs. 25.8% age 50 to 64) and sex (48.9% vs. 48.6% male) compared with those in non-expansion states (N = 230,428). The prevalence of hypertension (25.3% vs. 27.7%, p<0.001), diabetes (9.0% vs. 9.5%, p<0.001), and cardiovascular disease (6.5% vs. 7.5%, p<0.001) was lower in expansion compared with non-expansion states.
Health Care Access
Health care coverage, having a personal doctor, and routine checkups increased in expansion and non-expansion states over time (Supplemental Table 1). In difference-in-differences analysis, health care coverage increased over time in expansion compared to non-expansion states (baseline 64.1%, late DiD estimate 4.7%, p<0.001). The percentage of participants that had a personal doctor increased in expansion states compared to non-expansion states (baseline 60.9%, late DiD estimate 2.7%, p<0.001), as did the prevalence of having a routine checkup within the past year (baseline 56.8%, late DiD estimate 1.9%, p = 0.004, Table 3).
Table 3. Changes in health care access for low-income non-elderly adults in pre-expansion, immediate post-expansion, and late post-expansion periods.
Difference‐in‐differences estimate for expansion states.∬
| Baseline 2012–2013 (Mean % in expansion states) | Immediate Post-expansion 2014–2015 Difference-in-Differences Estimate (%, 95% CI) | p-value | Late Post-expansion 2016–2017 Difference-in-Differences Estimate (%, 95% CI) | p-value | |
|---|---|---|---|---|---|
| Healthcare access | |||||
| Have health care coverage (N = 498,627) | 64.1 | 4.3* (3.1 to 5.6) | <0.001 | 4.7* (3.4 to 5.9) | <0.001 |
| Have a personal doctor (N = 498,540) | 60.9 | 2.0* (0.7 to 3.3) | 0.002 | 2.7* (1.4 to 4.0) | <0.001 |
| Routine checkup within past year (N = 484,470) | 56.8 | 1.7* (0.4 to 3.0) | 0.010 | 1.9* (0.6 to 3.2) | 0.004 |
Expansion states (n = 24) were Arizona, Arkansas, California, Colorado, Connecticut, Hawaii, Illinois, Indiana, Iowa, Kentucky, Maryland, Michigan, Minnesota, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Washington, West Virginia
Non-expansion states (n = 19) were Alabama, Florida, Georgia, Idaho, Kansas, Maine, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, and Wyoming.
Alaska, Louisiana, and Montana were included as non-expansion states for the immediate 2014–2015 time period, and expansion states for the late 2016–2017 time period.
Delaware, District of Columbia, Massachusetts, New York, and Vermont were excluded.
Significant at the level p<0.05.
Cancer Screening and Cardiovascular Risk Reduction
The prevalence of breast cancer screening, colorectal cancer screening, and cholesterol screening and monitoring increased over time in unadjusted analyses of expansion and non-expansion states, while cervical cancer screening and aspirin use decreased (Supplemental Table 2). We did not detect a statistically significant difference in breast cancer screening (baseline 66.6%, late DiD estimate 0.6%, p = 0.78), cervical cancer screening (baseline 74.0%, late DiD estimate 0.4%, p = 0.75), or colorectal cancer screening (baseline 47.4%, late DiD estimate 0.2%, p = 0.91) in expansion compared to non-expansion states (Table 4, Figure 1).
Table 4. Changes in preventative health services for low-income non-elderly adults in pre-expansion, immediate post-expansion, and late post-expansion periods.
Difference‐in‐differences estimate for expansion states.∬
| Preventative Health Service (Unweighted N) | Baseline 2012–2013 (Mean % in expansion states*) | Immediate Post-expansion 2014–2015 Difference-in-Differences Estimate^ (%, 95% CI) | p-value | Late Post-expansion 2016–2017 Difference-in-Differences Estimate^ (%, 95% CI) | p-value |
|---|---|---|---|---|---|
| Cancer Screening | |||||
| Breast cancer screening (N = 54,094) | 66.6 | −0.3 (−4.0 to 3.5) | 0.89 | 0.6 (−3.4 to 4.5) | 0.78 |
| Cervical cancer screening (N = 142,917) | 74.0 | −0.5 (−2.7 to 1.6) | 0.63 | 0.4 (−1.9 to 2.7) | 0.75 |
| Colorectal cancer screening (N = 99,170) | 47.4 | −1.2 (−4.2 to 1.7) | 0.42 | 0.2 (−3.0 to 3.4) | 0.91 |
| Cardiovascular Risk Reduction | |||||
| Serum cholesterol screening (N = 272,004) | 72.8 | 1.4 (−0.9 to 3.8) | 0.24 | 0.6 (−1.7 to 2.8) | 0.63 |
| Serum cholesterol monitoring (N = 133,609) | 80.6 | 1.3 (−1.0 to 3.5) | 0.27 | 2.0 (−0.1 to 4.1) | 0.064 |
| Aspirin use (N = 171,900) | 5.5 | 8.7* (7.1 to 10.4) | <0.001 | 8.8* (7.2 to 10.5) | <0.001 |
| Diabetes Care | |||||
| Serum cholesterol monitoring (N = 58,150) | 91.0 | −3.6* (−7.3 to 0) | 0.048 | −3.1 (−6.5 to 0.3) | 0.071 |
| HbA1c monitoring (N = 27,623) | 76.8 | −1.2 (−5.4 to 3.0) | 0.57 | −3.6 (−7.7 to 0.6) | 0.095 |
| Foot examination (N = 27,424) | 67.8 | 1.8 (−2.9 to 6.5) | 0.44 | −0.2 (−5.3 to 5.0) | 0.95 |
| Eye examination (N = 27,622) | 54.2 | 0.4 (−4.5 to 5.3) | 0.88 | 0.6 (−4.7 to 5.8) | 0.84 |
| Influenza vaccination (N = 58,150) | 40.7 | 1.0 (−2.9 to 4.9) | 0.61 | 0.7 (−3.3 to 4.7) | 0.73 |
| Pneumonia vaccination (N = 58,150) | 38.0 | 2.1 (−1.7 to 5.9) | 0.29 | 1.6 (−2.3 to 5.5) | 0.41 |
| Other Primary Care | |||||
| Influenza vaccination (N = 463,262) | 26.0 | −0.1 (−1.3 to 1.0) | 0.86 | 1.4* (0.3 to 2.6) | 0.016 |
| Alcohol use screening (N = 22,871) | 77.1 | -- | -- | 1.1 (−1.7 to 3.8) | 0.45 |
| HIV screening (N = 461,088) | 43.6 | 0.5 (−0.8 to 1.8) | 0.46 | 1.9* (0.6 to 3.3) | 0.004 |
Difference-in-differences estimates compared immediate period to baseline, and late period to baseline. All estimates are adjusted for patient age and sex.
Breast cancer screening and cervical cancer screening were adjusted for age only.
Aspirin use was additionally adjusted for race/ethnicity, smoking status, hypertension, hyperlipidemia, diabetes, coronary heart disease or angina, stroke, and myocardial infarction.
Expansion states (n = 24) were Arizona, Arkansas, California, Colorado, Connecticut, Hawaii, Illinois, Indiana, Iowa, Kentucky, Maryland, Michigan, Minnesota, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Washington, West Virginia
Non-expansion states (n = 19) were Alabama, Florida, Georgia, Idaho, Kansas, Maine, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, and Wyoming.
Alaska, Louisiana, and Montana were included as non-expansion states for the immediate 2014–2015 time period, and expansion states for the late 2016–2017 time period.
Delaware, District of Columbia, Massachusetts, New York, and Vermont were excluded.
Significant at the level p<0.05.
Figure 1.
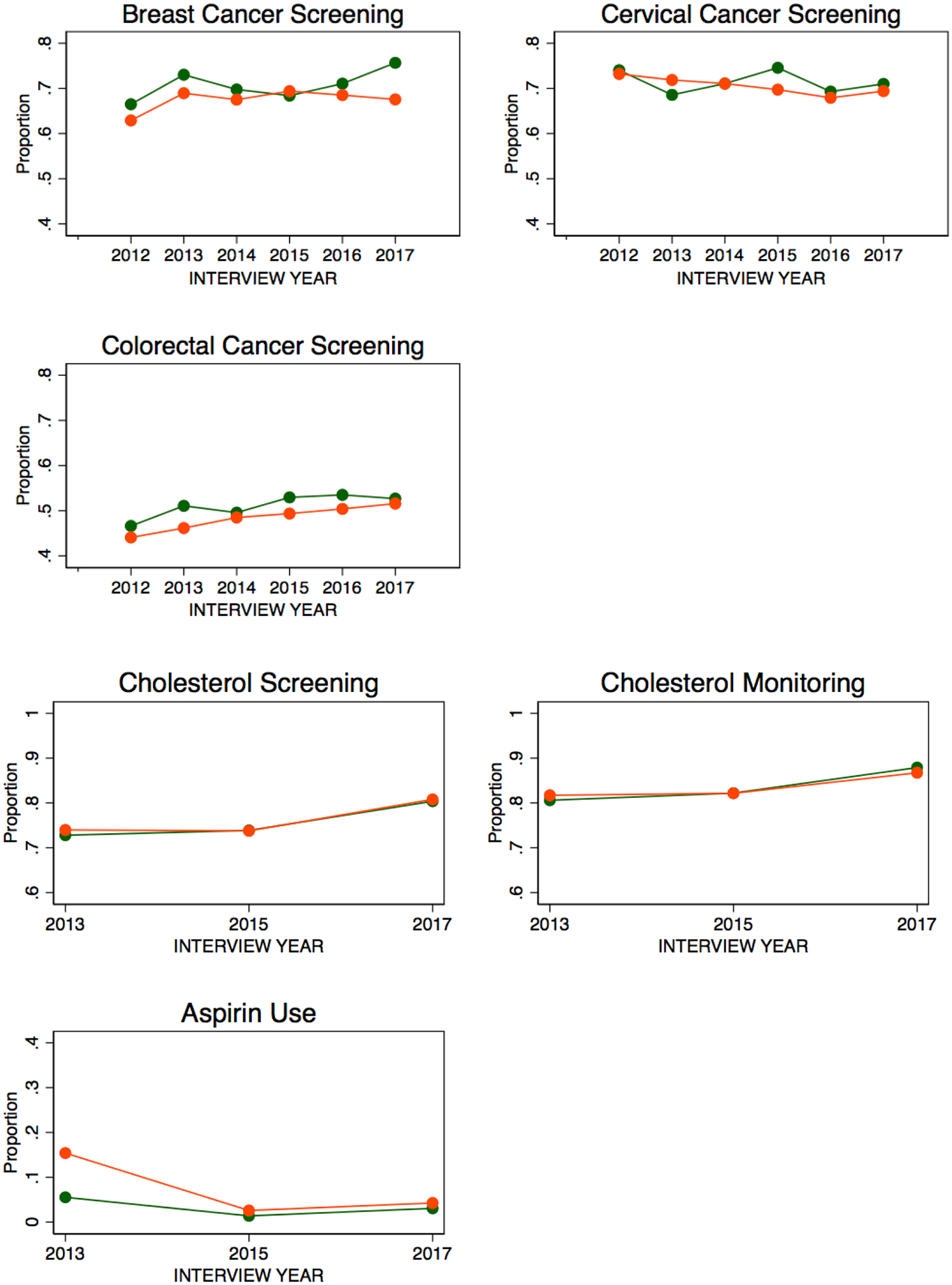
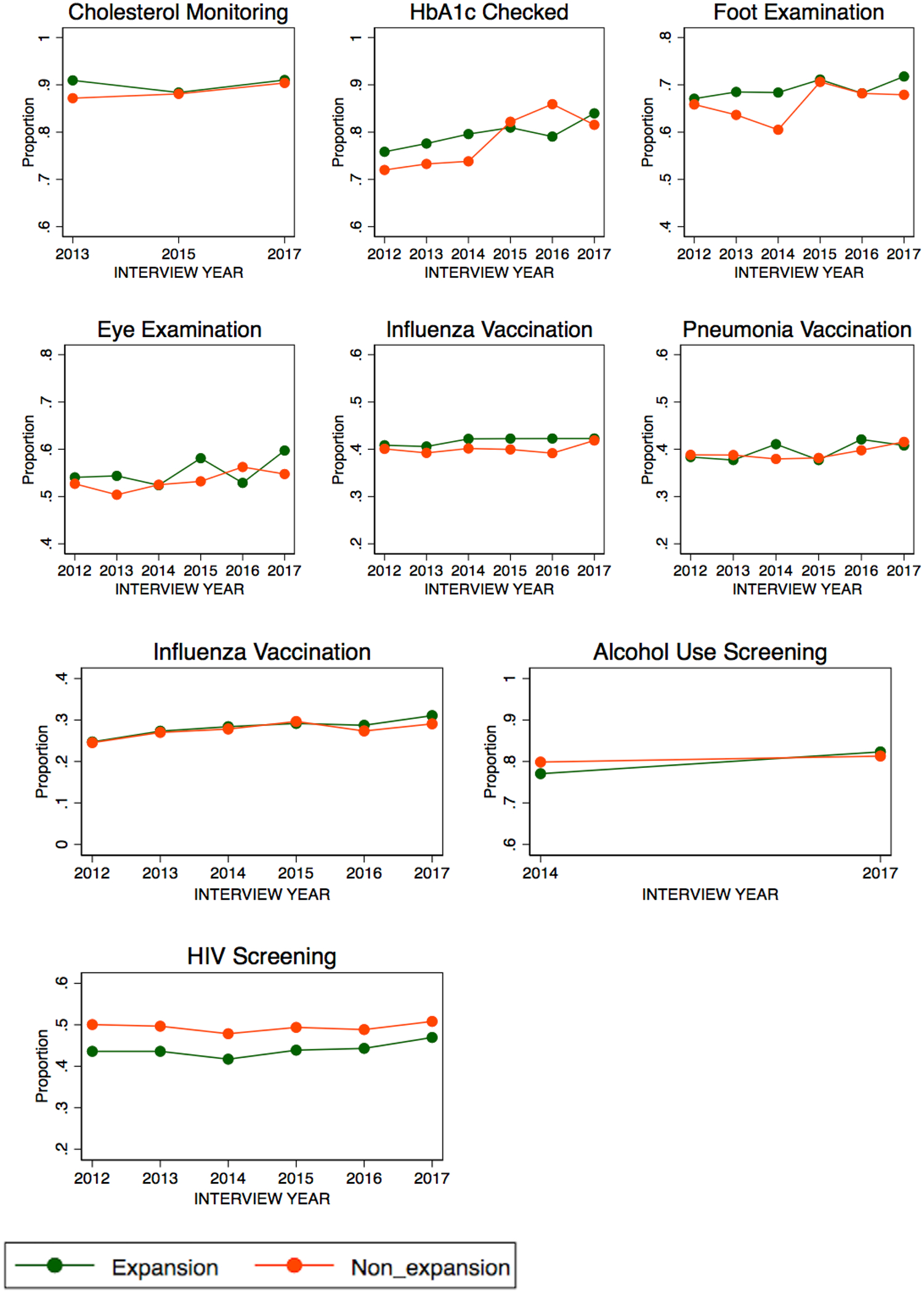
Cancer screening, cardiovascular risk reduction, diabetes care, and other primary care measures in Medicaid expansion and non-expansion states, unadjusted.
Similarly, there were no differences that met statistical significance for cholesterol screening in low-risk groups (baseline 72.8%, late DiD estimate 0.6%, p = 0.63) or monitoring in high-risk patients with a history of hypertension, hyperlipidemia, or cardiovascular disease (baseline 80.6%, late DiD estimate 2.0%, p = 0.064) in expansion versus non-expansion states. Aspirin use increased over time in expansion compared to non-expansion states, but violated the parallel trend assumption (baseline 5.5%, late DiD estimate 8.8%, p<0.001, Table 4).
Diabetes and Other Primary Care Measures
HbA1c monitoring and influenza vaccination increased over time in expansion and non-expansion states in unadjusted analyses (Supplemental Table 2). Expansion states did not demonstrate greater provision of diabetes care services compared to non-expansion states, including cholesterol monitoring (baseline 91.0%, late DiD estimate −3.1%, p = 0.071), Hemoglobin A1c monitoring (baseline 76.8%, late DiD estimate −3.6%, p = 0.095), foot examinations (baseline 67.8%, late DiD estimate −0.2%, p = 0.95), eye examinations (baseline 54.2%, late DiD estimate 0.6%, p = 0.84), influenza vaccination (baseline 40.7%, late DiD estimate 0.7%, p = 0.73), or pneumococcal vaccinations (baseline 38.0%, late DiD estimate 1.6%, p = 0.41, Table 4).
No statistically significant differences in alcohol use screening (baseline 77.1%, late DiD estimate 1.1%, p = 0.45) were detected between expansion versus non-expansion states. Influenza vaccination (baseline 26.0%, late DiD estimate 1.4%, p = 0.016) and HIV screening (baseline 43.6%, late DiD estimate 1.9%, p = 0.004) increased in expansion states compared to non-expansion states (Table 4).
Discussion
In this nationally representative sample of low-income non-elderly adults, states with Medicaid expansion demonstrated an increase in aspirin use, influenza vaccination, and HIV screening compared with non-expansion states. Despite improvements in access to care, including health insurance, having a primary care doctor, and routine visits, Medicaid expansion was not associated with improvements in cancer screening, cholesterol monitoring, diabetes care, or alcohol use screening.
Our study analyzes several widely accepted primary care measures, including cancer screening, laboratory testing, and vaccination rates, and adds to the literature by assessing a broad range of preventative health services using updated data from the fourth year after Medicaid expansion. Previous studies using less recent BRFSS data also showed an increase in HIV testing and no statistically significant change in cancer screening or diabetes care, similar to our results.13,15,16 An analysis of the Medicare Expenditure Panel Survey also found that Medicaid expansion was not associated with an increase in mammography or cervical cancer screening.28 However, another study in BRFSS comparing 2016 to 2012 data showed an increase in cervical and colorectal cancer screening in expansion states, but not mammography, that met statistical significance, which may have been due to differences in covariate adjustment in their model.29 We chose not to adjust for patient characteristics in assessing performance rates for health services, as the benchmark for quality care is high regardless of the underlying patient population. Thus, our results were largely consistent with prior analyses, but also showed an improvement in two other measures suggesting some modest effects from Medicaid expansion.
While there have been limited improvements in preventative care, which are largely process measures, several analyses have found early evidence of improved health outcomes after Medicaid expansion. An analysis of federally funded community centers showed improvements in hypertension control.30 Among non-elderly adults with diabetes, Medicaid expansion was associated with decreased hospitalizations for diabetes complications.31 Ongoing analyses will be crucial to assess how Medicaid expansion has affected other critical health outcomes.32
The modest effect of Medicaid expansion on receipt of preventative health care (improvement in 3 out of 15 measures assessed) points to several possible challenges along the across the cascade of care implementation. Upon insurance expansion there was an increase in routine checkups, but during these visits, clinicians may not have ordered recommended care. Alternatively, for certain preventative care services, clinicians may have ordered the testing, but patients may have faced barriers in following up with recommended care, related to difficulties navigating the health care system or patient factors. Distinguishing between these possibilities is difficult from the available data sources; for example, an analysis of electronic health record data from community health centers could not assess whether clinicians did not prescribe cervical and colorectal cancer screening, or if it was prescribed but patients did not obtain the screening, due to limitations of the data source.33 Lastly, Medicaid patients may have suboptimal access to timely specialty care, which is necessary for certain preventative health services, such as colonoscopies and ophthalmologic exams, and may contribute to a lack of improvement in those domains.34
Several additional explanations should be considered for why preventative health care delivery has improved differentially in Medicaid expansion states for only a few measures thusfar. One possibility is that four years is not enough time for the policy to take effect. While this may apply to the effect of insurance expansion on health outcomes, we find this explanation for process measures of care to be unlikely. In the Oregon Health Experiment, improvements in diabetes detection, receipt of medication for diabetes, cholesterol screening, breast cancer screening, and cervical cancer screening were seen within two years of randomization to Medicaid coverage.1 Second is the consideration that many of the screening rates were “topped-out,” and meaningful improvements could no longer be made. This may have been a contributing factor; the three quality measures that had improvements that met statistical significance all had baseline performance rates of less than 50%. Third, we found that many outcomes improved over time in both expansion and non-expansion states, including breast cancer screening, colorectal cancer screening, cholesterol screening and monitoring, HbA1c monitoring, and influenza vaccination (Supplemental Tables 1 and 2). Other sources of increased health care coverage, such as the Affordable Care Act individual mandate and insurance exchanges, in non-Medicaid expansion states could have diminished the differential effect of Medicaid in expansion states on the receipt of preventative health services. Lastly, validity of self-reporting in the BRFSS is crucial for assessing the outcomes. Low participant awareness of health services being performed, such as cholesterol testing, would have biased results towards no effect. An analysis of a managed care population in Colorado found high agreement between self-report and the medical record for breast and cervical cancer screening, indicating accuracy of self-reporting is relatively high for those outcomes, however validity is less clear for other outcomes such as laboratory testing which may involve less patient education and participation.35
The limited improvements in preventative care services after Medicaid expansion raises the need for a thorough evaluation of quality of care monitoring and reimbursement in the Medicaid population. While the Quality Payment Program for Medicare beneficiaries has been the topic of considerable discussion, quality measurement for Medicaid patients receives less attention. The Medicaid Adult Health Care Quality Measures introduced in January 2012 encourage voluntary reporting of quality measures by states in multiple domains of care. The core measures set includes breast cancer screening, cervical cancer screening, and HbA1c testing, which we included in our analysis, but the impact of this public reporting mechanism on quality of care performance has not been rigorously assessed. CMS has sponsored Adult Medicaid Quality Grants to support state reporting, data analysis, and quality improvement efforts, and further efforts are necessary to improve preventative health care in the Medicaid population. Furthermore, low reimbursement for Medicaid visits may undermine quality of care; one study found that higher reimbursement for Medicaid office visits was associated with an increased likelihood of cancer screening.36
The main strength of our analysis is the use of a quasi-experimental design to assess the effect of Medicaid expansion on an expansive set of preventative health services. The BRFSS surveys a large sample of participants, so our analysis was well powered to detect an effect. Several limitations should be noted. BRFSS data is self-reported, so we are unable to confirm receipt of preventative health services in the medical record, but we expect this to affect both expansion and non-expansion states. We examined differences over time at the state level and the BRFSS contains serial cross-sectional data, so we were unable to follow individuals over time. The BRFSS does not contain laboratory data or data on health outcomes, which is a limitation of the study.
Our results show some improvement in the receipt of evidence-based preventative health services four years after Medicaid expansion as part of the Affordable Care Act, a monumental national policy. While we find that Medicaid expansion had a limited effect on primary care delivery, this may be at least in part due to the positive effects of the Affordable Care Act on receipt of needed care in non-expansion states. Our results suggest that expanding health insurance coverage alone is not sufficient to improve the use of recommended preventative health services. Our findings highlight implementation challenges in delivering high quality primary care to low-income adults.
Supplementary Material
Table 2.
Sociodemographic and clinical characteristics of low-income non-elderly adults in expansion and non-expansion states across the study period 2012–2017.
| Expansion States∬ (%, n = 270,067) |
Non-expansion States (%, n = 230,428) |
p-value | |
|---|---|---|---|
| Sociodemographics | |||
| Age | |||
| 18–29 | 34.0 | 33.1 | 0.003 |
| 30–49 | 40.7 | 41.1 | |
| 50–64 | 25.3 | 25.8 | |
| Sex | |||
| Male | 48.9 | 48.6 | 0.28 |
| Female | 51.1 | 51.4 | |
| Race/Ethnicity | |||
| Non-Hispanic White | 47.4 | 47.2 | <0.001 |
| Non-Hispanic Black | 12.5 | 21.5 | |
| Hispanic | 30.5 | 25.5 | |
| Asian, Native Hawaiian, or Pacific Islander | 5.7 | 2.4 | |
| Other | 3.9 | 3.4 | |
| Employment | |||
| Employed for wages | 47.7 | 49.6 | <0.001 |
| Self-employed | 8.8 | 9.1 | |
| Unemployed | 11.4 | 10.7 | |
| Not in labor force | 32.1 | 30.6 | |
| Education Level | |||
| < High school graduate | 24.8 | 23.4 | <0.001 |
| High school graduate | 32.7 | 33.9 | |
| 1–3 yrs of college | 30.9 | 31.2 | |
| ≥4 yrs of college | 11.6 | 11.6 | |
| Marital Status | |||
| Married | 31.7 | 34.1 | <0.001 |
| Divorced, separated, or widowed | 21.1 | 23.5 | |
| Never married | 47.2 | 42.5 | |
| Clinical Characteristics and Medical History | |||
| Current smoker | 27.0 | 28.0 | <0.001 |
| Obesity (BMI ≥30) | 31.6 | 34.2 | <0.001 |
| Hypertension | 25.3 | 27.7 | <0.001 |
| Hyperlipidemia | 29.6 | 30.8 | 0.004 |
| Diabetes | 9.0 | 9.5 | <0.001 |
| Cardiovascular disease† | 6.5 | 7.5 | <0.001 |
Expansion states (n = 24) were Arizona, Arkansas, California, Colorado, Connecticut, Hawaii, Illinois, Indiana, Iowa, Kentucky, Maryland, Michigan, Minnesota, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Washington, West Virginia
Non-expansion states (n = 19) were Alabama, Florida, Georgia, Idaho, Kansas, Maine, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, and Wyoming.
Alaska, Louisiana, and Montana were included as non-expansion states for the immediate 2014–2015 time period, and expansion states for the late 2016–2017 time period.
Delaware, District of Columbia, Massachusetts, New York, and Vermont were excluded.
Includes coronary heart disease or angina, stroke, or myocardial infarction.
Acknowledgements:
Dr. Tummalapalli is supported by the ASN Foundation for Kidney Research Ben J. Lipps Research Fellowship Program (Sharon Anderson Research Fellowship) and the Jonathan A. Showstack Career Advancement Award in Health Policy/Health Services Research at the UCSF Philip R. Lee Institute for Health Policy Studies.
Footnotes
Poster Presentation: Academy Health Annual Research Meeting, June 2–4, 2019, Washington, DC
Disclosures: The authors have nothing to disclose.
References
- 1.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. The New England journal of medicine 2013;368:1713–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaiser Family Foundation analysis of 2013 and 2016 American Community Survey (ACS) -YE.
- 3.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act. Jama 2015;314:366–74. [DOI] [PubMed] [Google Scholar]
- 4.Griffith K, Evans L, Bor J. The Affordable Care Act Reduced Socioeconomic Disparities In Health Care Access. Health affairs (Project Hope) 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi S, Lee S, Matejkowski J. The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling. Population health management 2018;21:235–44. [DOI] [PubMed] [Google Scholar]
- 6.Benitez JA, Seiber EE. US Health Care Reform and Rural America: Results From the ACA’s Medicaid Expansions. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association 2018;34:213–22. [DOI] [PubMed] [Google Scholar]
- 7.Yue D, Rasmussen PW, Ponce NA. Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access. Health services research 2018;53:3640–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wherry LR, Miller S. Early Coverage, Access, Utilization, and Health Effects Associated With the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study. Annals of internal medicine 2016;164:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Effects of the Affordable Care Act on Health Care Access and Self-Assessed Health After 3 Years. Inquiry : a journal of medical care organization, provision and financing 2018;55:46958018796361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soni A, Hendryx M, Simon K. Medicaid Expansion Under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association 2017;33:217–26. [DOI] [PubMed] [Google Scholar]
- 11.Antonisse L, G R, Rudowitz R, Artiga S. The effects of Medicaid expansion under the ACA: updated findings from a literature review [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2018. March [cited 2018 Apr 3].(Issue Brief). [Google Scholar]
- 12.Mazurenko O, Balio CP, Agarwal R, Carroll AE, Menachemi N. The Effects Of Medicaid Expansion Under The ACA: A Systematic Review. Health affairs (Project Hope) 2018;37:944–50. [DOI] [PubMed] [Google Scholar]
- 13.Cawley J, Soni A, Simon K. Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S. Journal of general internal medicine 2018;33:1495–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller S, Wherry LR. Health and Access to Care during the First 2 Years of the ACA Medicaid Expansions. The New England journal of medicine 2017;376:947–56. [DOI] [PubMed] [Google Scholar]
- 15.Luo H, Chen ZA, Xu L, Bell RA. Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS. Journal of public health management and practice : JPHMP 2018. [DOI] [PubMed] [Google Scholar]
- 16.Simon K, Soni A, Cawley J. The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions. Journal of policy analysis and management : [the journal of the Association for Public Policy Analysis and Management] 2017;36:390–417. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control. The BRFSS Data User Guide. August 15 hwcgbddpUp.
- 18.US Department of Health and Human Services. Prior HHS poverty guidelines and federal register references. Washington: Dhahgpf-f-rs. [Google Scholar]
- 19.Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine 2009;151:716–26, w-236. [DOI] [PubMed] [Google Scholar]
- 20.Moyer VA. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine 2012;156:880–91, w312. [DOI] [PubMed] [Google Scholar]
- 21.Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine 2008;149:627–37. [DOI] [PubMed] [Google Scholar]
- 22.Final Recommendation Statement: Lipid Disorders in Adults (Cholesterol DSUSPSTFJ, https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/lipid-disorders-in-adults-cholesterol-dyslipidemia-screening. [Google Scholar]
- 23.Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine 2009;150:396–404. [DOI] [PubMed] [Google Scholar]
- 24.Standards of medical care in diabetes--2012. Diabetes care 2012;35 Suppl 1:S11–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)--United States, 2012–13 influenza season. MMWR Morbidity and mortality weekly report 2012;61:613–8. [PubMed] [Google Scholar]
- 26.Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Annals of internal medicine 2004;140:554–6. [DOI] [PubMed] [Google Scholar]
- 27.Moyer VA. Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement. Annals of internal medicine 2013;159:51–60. [DOI] [PubMed] [Google Scholar]
- 28.Alharbi AG, Khan MM, Horner R, Brandt H, Chapman C. Impact of Medicaid coverage expansion under the Affordable Care Act on mammography and pap tests utilization among low-income women. PloS one 2019;14:e0214886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hendryx M, Luo J. Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion. Medical care 2018;56:944–9. [DOI] [PubMed] [Google Scholar]
- 30.Cole MB, Galarraga O, Wilson IB, Wright B, Trivedi AN. At Federally Funded Health Centers, Medicaid Expansion Was Associated With Improved Quality Of Care. Health affairs (Project Hope) 2017;36:40–8. [DOI] [PubMed] [Google Scholar]
- 31.Mondesir FL, Kilgore ML, Shelley JP, et al. Medicaid Expansion and Hospitalization for Ambulatory Care-Sensitive Conditions Among Nonelderly Adults With Diabetes. The Journal of ambulatory care management 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Angier H, Huguet N, Marino M, et al. Observational study protocol for evaluating control of hypertension and the effects of social determinants. BMJ open 2019;9:e025975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huguet N, Angier H, Rdesinski R, et al. Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Preventive medicine 2019;124:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Timbie JW, Kranz AM, Mahmud A, Damberg CL. Specialty care access for Medicaid enrollees in expansion states. The American journal of managed care 2019;25:e83–e7. [PMC free article] [PubMed] [Google Scholar]
- 35.Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women’s self-reports of cancer screening test utilization in a managed care population. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 2003;12:1182–7. [PubMed] [Google Scholar]
- 36.Halpern MT, Romaire MA, Haber SG, Tangka FK, Sabatino SA, Howard DH. Impact of state-specific Medicaid reimbursement and eligibility policies on receipt of cancer screening. Cancer 2014;120:3016–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jellinger PS, Dickey RA, Ganda OP, et al. AACE medical guidelines for clinical practice for the diagnosis and treatment of dyslipidemia and prevention of atherogenesis. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists 2000;6:162–213. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


