Abstract
Background:
Gonorrhea and chlamydia are common among Chinese men who have sex with men (MSM), but testing rates are low. We developed a pay-it-forward program where men receive a free gonorrhea/chlamydia test and can then donate toward future participants’ tests. This study aims to investigate drivers of testing uptake and donation using a mixed methods approach.
Methods:
We used a sequential explanatory design to explore drivers of testing uptake and donation unique to pay-it-forward through a quantitative cross-sectional survey and a qualitative thematic analysis of semi-structured interviews. We collected data on socio-demographics and perceived benefits of pay-it-forward among men offered the pay-it-forward interventionand analyzed testing uptake and donations using descriptive statistics and logistic regression. We then conducted thirty semi-structured interviews with men and codedinterview data to identify themes.
Results:
301 MSM were offered pay-it-forward and 55% (165/301) received gonorrhea/chlamydia testing. 91% (150/165) donated any amount with a mean of 58.31±53.39 RMB ($8.61±7.88 USD), or 39% of the standard price of gonorrhea/chlamydia testing. Getting tested was not associated with income, but donations were higher in the highest income bracket (aOR = 7.12, 95% CI = 1.61-31.52). 58% (94/162) selected “more MSM can get tested” and 54% (88/162) selected “I can help someone else” as benefits of pay-it-forward. Qualitative themes for drivers of testing and donation included flexible pricing, generosity and reciprocity, and MSM community identity.
Conclusions:
Quantitative and qualitative results suggest that this pay-it-forward program may increase gonorrhea/chlamydia testing by reducing cost barriers, leveraging generosity and reciprocity, and mobilizing community altruism.
Keywords: gonorrhea, chlamydia, men who have sex with men, pay-it-forward, China
Short summary:
A mixed methods analysis found that drivers of a pay-it-forward gonorrhea/chlamydia testing program included flexible pricing, gift-giving and generosity, and community identity and collectivism.
Introduction
Gonorrhea and chlamydia infection are major risks factors for HIV transmission (1, 2), and may accelerate HIV transmission among men who have sex with men (MSM) (3). In China, gonorrhea and chlamydia are common among MSM (4, 5), but testing rates are as low as 30-40% (6, 7). There are multiple barriers to testing. There are no screening guidelines for gonorrhea and chlamydia among MSM in China (8, 9). This places the burden of testing squarely on the patient. However, knowledge about sexually transmitted diseases is limited across China (10). Further, patients must pay up to 100-150 RMB ($14.77-$22.15 USD) out-of-pocket. Additionally, due to persistent stigma, MSM are often distrustful of healthcare providers and reluctant to seek care (11).
To address these barriers, we partnered with several community-based organizations to implement a pay-it-forward gonorrhea/chlamydia testing program for MSM in China (12). Pay-it-forward is a system in which one person receives a gift, then passes on that gift to another person (13, 14) and has been used as a promotional strategy for goods and services (15, 16). We implemented a pay-it-forward program for gonorrhea/chlamydia testing to decrease barriers to testing and improve trust in health services.
In our pay-it-forward program, men were told that previous participants had already covered testing costs, so that they could receive a free test. Then they decide whether or not to donate toward testing for future participants. Donation was voluntary with no suggested amount (12).
We previously analyzed the pay-it-forward program through one quasi-experimental study from December 2017 to February 2018 at two sites in Guangzhou, China(12), and a three-armed randomized controlled trial from December 2018 to January 2019 at two sites in Guangzhou and one site in Beijing, China (17). In the quasi-experimental study, we found that the pay-it-forward program substantially increased testing uptake by compared to testing offered at the standard hospital price of 150 RMB ($22.15 USD) (cOR 18·65, 9·78–35·54; p<0·0001; aOR 19·73, 95% CI 10·02–38·85; p<0·0001)(12). In the RCT, we also found that the pay-it-forward program substantially increased testing uptake (estimated difference 38.4% , 95% CI lower bound: 28.4%) (17)
To implement pay-it-forward effectively and sustainably, it is important to understand how the model promotes test uptake and donation. Previous research has not evaluated pay-it-forward in the context of public health (14, 18). Pay-it-forward may be particularly useful in public health settings like STD clinics where user fees are common. The purpose of this study was to examine motivations for pay-it-forward testing and donation among MSM in China using a mixed methods approach.
Methods
This study is part of a community-based participatory research effort to improve gonorrhea/chlamydia testing among MSM in China through working with local community partners. We used a sequential explanatory design to identify and explore drivers for testing uptake and donation, with a quantitative cross-sectional survey analysis followed by a qualitative thematic analyses of semi-structured interviews. We collected quantitative data during two implementations of the pay-it-forward program. We then conducted semi-structured qualitative interviews with pay-it-forward participants based quantitative data findings.
Pay-it-forward program
A detailed methodological description is provided elsewhere (12). The pay-it-forward program was implemented, from December 2017 to February 2018 at two sites in Guangzhou, China, and from December 2018 to January 2019 at two sites in Guangzhou and one site in Beijing, China. The sites included two hospital-based STI clinic sites run by the same nonprofit organization (STI clinic), one community-based organization (CBO) site in Guangzhou, and one community-based site in Beijing run by Blued, the largest gay dating app in China. All sites offered free HIV rapid testing for MSM and were run by volunteers without physicians. Pay-it-forward was not advertised prior to the project. Inclusion criteria consisted of all men over the age of 18 who presented to the sites for free HIV testing. Men who participated in pay-it-forward but declined to fill out the quantitative survey were excluded. All men who arrived at the clinic were invited to participate. Briefly, men were told that the standard price of a gonorrhea/chlamydia test was 150 RMB ($22.15 USD), but that they could receive a free test because it was paid for by previous participants. Men could then donate money toward testing for future participants or choose not to donate. All men were given information about gonorrhea and chlamydia, and also shown postcards written by previous participants. Samples were processed at Southern Medical University Dermatology Hospital in Guangzhou, and men received test results via WeChat (a popular messaging app) after 1–2 weeks. Men who tested positive were counseled on where and how to obtain treatment. The name, logo, and other details of the pay-it-forward intervention were iteratively developed using crowdsourcing methods in a community-based participatory approach (19). Crowdsourcing relies on a group of non-expert individuals to solve a problem, then shares the solution with the public(20).
Quantitative methods
All men offered pay-it-forward were asked to fill out a survey with sociodemographic information, sexual behavior, previous testing behavior, and benefits and barriers of the pay-it-forward program (Supplement 1). Data were analyzed using descriptive statistics and logistic regression to evaluate factors associated with getting tested for gonorrhea and chlamydia. Among men who received testing through pay-it-forward, we used multinomial logistic regression to determine correlates of higher donations, with donations modeled as an ordinal variable with five groups. Results were reported as crude odds ratio (cOR) and adjusted odds ratio (aOR), with adjustment for age, nationality, marital status, education, income, and test site, and 95% confidence intervals (95% CI).
Qualitative methods
We conducted semi-structured interviews with participants of pay-it-forward. Main topics included (1) reasons for getting tested; (2) considerations for whether and how much to donate; (3) specific questions about income, community participation, and generosity motivated by initial quantitative results; and (4) the pay-it-forward concept (Supplement 2).
Recruitment was conducted by our community partners through a WeChat announcement or directly after testing, after sample collection and donation were complete. No participant names were collected. We recruited a voluntary response sample of MSM who participated in pay-it-forward and contacted participants via their preferred contact information to set up times for interviews.
All interviewees gave verbal informed consent. Interviews lasted 45-75 minutes and took place either in person or over the phone based on participant preference. Interviews were audio-recorded with consent, with personal information redacted. Participants were reimbursed 50 RMB ($7.38 USD).
All recorded interviews were transcribed, and transcripts were all checked by one research staff member. Coding was conducted by three researchers using NVivo version 12 (Nvivo, Columbus, OH), and data were analysed using thematic analysis. Quotations were translated into English by two researchers.
Ethics approval was obtained from the ethics review committees at Southern Medical University Dermatology Hospital and the University of North Carolina at Chapel Hill.
Results
Quantitative data were collected from December 2017 to February 2018 from 203 participants from the quasi-experimental study (12), and December 2018 to January 2019 from 104 participants from the pay-it-forward RCT. Three participants were excluded for failing to complete the survey. A total of 301 men were included for the quantitative analysis. Qualitative interviews were then conducted with 30 of these pay-it-forward participants from December 2018 through February 2019 (Fig 1)
Fig 1:
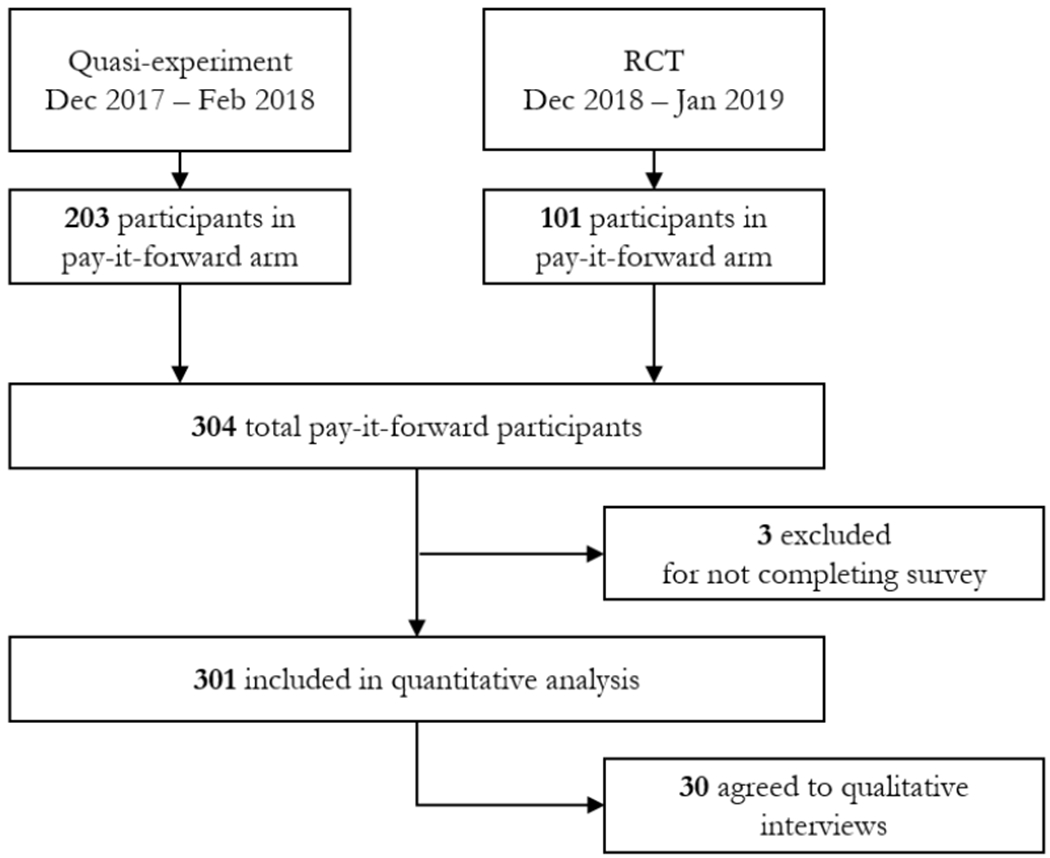
Study flow chart
Quantitative results
Correlates of testing
165/301(55%) men chose to get tested. Sociodemographic and behavioral characteristics of these participants are provided in Table 1. Multivariable logistic regression showed that getting tested was significantly associated with ever being married (aOR = 4.24, 95% CI 1.38-13.03), more male partners in the last three months (aOR = 1.20, 95% CI 1.02-1.40), and recent symptoms suggestive of an STD (aOR = 3.69, 95% CI 1.49-9.13) (Table 2). There was no significant association with income. In a subgroup analysis of 203 men from the first implementation of pay-it-forward from December 2017 to February 2018, who had monthly income categorized into four brackets, there was also no significant association with income (Supplement 3). Of all men who received testing, 94/162 (58%) who responded selected “more gay men in the community can get tested” as a benefit, and 88/162 (54%) selected “Someone has helped me, and I can help someone else” as a benefit (Fig 2).
Table 1:
Baseline characteristics of participants who completed the survey questionnaire (n = 301)
| Tested (n = 165) |
Did not test (n = 136) |
P-value* | |
|---|---|---|---|
| Age | 0.1071 | ||
| <= 30 | 115 (70%) | 106 (78%) | |
| > 30 | 50 (30%) | 30 (22%) | |
| Nationality | 0.1016 | ||
| Han Chinese | 155 (94%) | 133 (98%) | |
| Other | 10 (6%) | 3 (2%) | |
| Marital Status | 0.0013 | ||
| Never married | 135 (83%) | 129 (95%) | |
| Ever married | 28 (17%) | 7 (5%) | |
| Education | 0.3846 | ||
| Below Bachelors | 73 (44%) | 67 (49%) | |
| Bachelors and above | 92 (56%) | 69 (51%) | |
| Annual income (USD) | 0.9375 | ||
| <$8682 | 68 (41%) | 57 (42%) | |
| ≥$8283 | 96 (59%) | 79 (58%) | |
| Disclosure as MSM | 0.7206 | ||
| Never | 67 (41%) | 58 (43%) | |
| Ever | 98 (59%) | 78 (57%) | |
| Number of male partners in last 3 months^ | 2.26±2.40 | 1.59±1.41 | 0.0052 |
| Position w/ male partner | 0.6751 | ||
| Primarily receptive | 51 (32%) | 38 (30%) | |
| About half and half | 57 (36%) | 42 (33%) | |
| Primarily insertive | 52 (33%) | 48 (38%) | |
| Condomless anal sex in past 3 months | 0.4191 | ||
| No | 97 (62%) | 85 (66%) | |
| Yes | 60 (38%) | 43 (34%) | |
| Recent symptoms suspected due to STI | 0.0051 | ||
| No | 140 (85%) | 129 (95%) | |
| Yes | 25 (15%) | 7 (5%) | |
| Previously tested for HIV | 0.5837 | ||
| No | 31 (19%) | 29 (21%) | |
| Yes | 134 (81%) | 107 (79%) | |
| Site | 0.6813 | ||
| Guangzhou STI clinic site | 72 (44%) | 63 (46%) | |
| Guangzhou | 52 (32%) | 45 (33%) | |
| Community-based organization site | |||
| Beijing Blued organization site | 41 (25%) | 28 (21%) | |
| Attendance | 0.6591 | ||
| Alone | 83 (50%) | 63 (48%) | |
| With partner | 82 (50%) | 69 (52%) |
Chi-squared test
Shown as Mean±SD
Table 2:
Correlates of getting tested through pay-it-forward (n = 301)
| Univariable cOR (95% CI) |
Multivariable# aOR (95% CI) |
|
|---|---|---|
| Age | 1.04 (1.00-1.08) | 1.00 (0.95-1.05) |
| Nationality | ||
| Han Chinese | ||
| Other | 2.86 (0.77-10.61) | 2.19 (0.55-8.66) |
| Marital Status | ||
| Never married | ||
| Ever married | 3.82 (1.61-9.06)* | 4.24 (1.38-13.03)* |
| Education | ||
| Below Bachelors | ||
| Bachelors and above | 1.22 (0.78-1.93) | 1.55 (0.93-2.58) |
| Annual income (USD) | ||
| <$8682 | ||
| ≥$8283 | 1.02 (0.64-1.62) | 0.96 (0.57-1.62) |
| Disclosure as MSM | ||
| Never | ||
| Ever | 1.09 (0.69-1.72) | 1.16 (0.70-1.90) |
| No. male partners in last 3 months | 1.24 (1.06-1.45)* | 1.20 (1.02-1.40)* |
| Position | ||
| Primarily insertive | ||
| About half and half | 1.25 (0.72-2.19) | 1.16 (0.64-2.10) |
| Primarily receptive | 1.24 (0.70-2.20) | 1.21 (0.67-2.20) |
| Condomless anal sex in past 3 months | ||
| No | ||
| Yes | 1.22 (0.75-1.99) | 1.13 (0.67-1.90) |
| Recent symptoms suspected may be due to STI | ||
| No | ||
| Yes | 3.29 (1.38-7.87)* | 3.69 (1.49-9.13)* |
| Previously tested for HIV | ||
| No | ||
| Yes | 1.17 (0.67-2.06) | 1.15 (0.63-2.11) |
| Site | ||
| STI clinic | ||
| CBO | 1.01 (0.60-1.71) | 0.99 (0.56-1.75) |
| BlueD | 1.28 (0.71-2.31) | 1.70 (0.90-3.21) |
| Attendance | ||
| Alone | ||
| With Partner | 0.90 (0.57-1.43) | 0.72 (0.43-1.22) |
Multivariable analysis adjusted for age, nationality, marital status, education, income, and test site
p < 0.05.
Fig 2: Responses to “What are the benefits of pay-it-forward (select all that apply)” among men who received testing through pay-it-forward (n = 162, 3 blank).

*Includes I can experience warm glow from helping others, I can benefit from my community being healthier, and novel idea
Correlates of donation
Among the testers, 91% (150/165) donated any amount with a mean donation of 58.31±53.39 RMB ($8.61±7.88 USD). Two participants donated 200 RMB ($29.53 USD), greater than the price of one test. Four men donated without testing, with a mean donation of 125 RMB ($18.46 USD). All six of these participants had monthly income >10,000 RMB. Analysis of 203 participants from the first implementation of pay-it-forward from December 2017 to February 2018, who had monthly income categorized into four brackets, showed that a higher PIF contribution was associated with the highest income bracket of >10,000 RMB/month (aOR = 7.12, 95% CI = 1.61-31.52) (Supplement 3).
Higher contributions were associated with selecting “More gay men in the community can get tested” as a benefit (aOR = 2.61, 95% CI = 1.36-4.99) and marginally associated with “Someone has helped me, so I can help someone else too” as a benefit (aOR = 1.86, 95% CI = 0.98-3.53) (Table 3). Higher contributions were also associated with symptoms suggestive of STI (aOR = 2.42, 95% CI = 1.05-5.59) and marginally associated with condomless anal sex in the past three months (aOR = 1.87, 95% CI 0.98-3.58).
Table 3:
Correlates of pay-it-forward contribution amount^ (n = 165)
| Univariable cOR (95% CI) |
Multivariable# aOR (95% CI) |
|
|---|---|---|
| Age | 0.99 (0.95-1.04) | 0.98 (0.92-1.03) |
| Nationality | ||
| Han Chinese | ||
| Other | 1.40 (0.41-4.71) | 1.63 (0.44-6.02) |
| Marital Status | ||
| Never married | ||
| Ever married | 0.95 (0.43-2.10) | 1.29 (0.46-3.59) |
| Education | ||
| Below Bachelors | ||
| Bachelors and above | 1.46 (0.80-2.67) | 1.27 (0.65-2.48) |
| Annual income (USD) | ||
| <$8682 | ||
| ≥$8283 | 1.80 (0.97-3.34) | 1.79 (0.92-3.48) |
| Disclosure as MSM | ||
| Never | ||
| Ever | 1.49 (0.81-2.75) | 1.35 (0.71-2.57) |
| Number of male partners in last 3 months | 1.02 (0.90-1.15) | 1.02 (0.90-1.16) |
| Position | ||
| Primarily insertive | ||
| About half and half | 0.99 (0.48-2.06) | 1.16 (0.54-2.51) |
| Primarily receptive | 1.14 (0.54-2.41) | 1.33 (0.62-2.84) |
| Condomless anal sex in past 3 months | ||
| No | ||
| Yes | 1.91 (1.02-3.58)* | 1.87 (0.98-3.58)* |
| Recent symptoms suspected may be due to STI | ||
| No | ||
| Yes | 2.22 (0.99-4.95)* | 2.42 (1.05-5.59)* |
| Previously tested for HIV | ||
| No | ||
| Yes | 1.16 (0.54-2.48) | 0.98 (0.43-2.22) |
| Attendance | ||
| Alone | ||
| With Partner | 1.14 (0.63-2.06) | 1.44 (0.71-2.91) |
| Site | ||
| STI clinic | ||
| CBO | 1.35 (0.67-2.69) | 1.09 (0.52-2.28) |
| BlueD | 1.06 (0.50-2.25) | 1.04 (0.47-2.27) |
| Selected “more MSM can get tested” as a benefit | ||
| No | ||
| Yes | 2.63 (1.39-4.95)* | 2.61 (1.36-4.99)* |
| Selected “Someone helped me and I can help someone else” as a benefit | ||
| No | ||
| Yes | 1.77 (0.97-3.25) | 1.86 (0.98-3.53)* |
| Selected “Others can help pay for me” as a benefit | ||
| No | ||
| Yes | 0.67 (0.34-1.31) | 0.64 (0.32-1.28) |
Multivariable analysis adjusted for age, nationality, marital status, education, income, and test site
p < 0.05.
Categorized as: 0 RMB (USD $0), 1-50 RMB (USD $0.15-$7.24), 51-100 RMB (USD $7.25-$14.47), 101-150 RMB (USD $14.48-$21.71), and > 150 RMB (USD $21.71).
Qualitative results
A total of 30 men were interviewed: 9 from the STI clinic site, 8 from the Guangzhou CBO site, and 13 from the Beijing Blued site. The average age was 28 years old. Donations ranged from 0-150 RMB ($0-22.15 USD), with a mean of 45.0±44.4 RMB ($6.65±6.56 USD). Major themes that emerged as unique drivers of testing and donating included flexible pricing; gift-giving and reciprocity; community identity and collectivism; and norms and peer influence.
Flexible pricing
The flexible pricing component of pay-it-forward was a strong motivator of testing: “If you told me I had to pay, I probably wouldn’t have tested from the beginning,” (29, Beijing).
For some men, flexible pricing removed financial barriers to testing: “When I realized, you can either pay or not pay, then I thought okay…at the time, I truly didn’t have much money,” (20, Beijing).
As a result, men could determine how much to donate based on their own finances. Those with less means could pay less: “I didn’t have an income, so I just donated a little…at that time, I could donate 20-30. Now that [I’m employed], I might donate 50-60,” (25, CBO site); and those who could afford more could pay more: “I just paid the standard price…because I’m not lacking in money…I have the means, so I paid it,” (30, Beijing).
Gift-giving, generosity, and reciprocity
Many men mentioned that receiving a generous gift encouraged them to participate. Framing the test as a gift made it attractive “I think because somebody gifted me this free test…it’s a very joyful thing – who doesn’t like free things?…But if you told me from the beginning that I had to pay for myself…I might feel some resistance instead, like forget it, in that case I won’t test.” (27, STI clinic).
Many said that this act of generosity motivated them to be generous in turn: “When you see someone else’s heartwarming message, you feel that others want to help you, so then you want to help others, and pass down the love like this, everyone altogether” (38, CBO) Others said that donation was more motivated by reciprocity and obligation: “At the very least you should cover your own [cost], why should someone else pay for you, they don’t owe you anything.” (20, Beijing)
A few individuals talked about reciprocity between each tester and the service provider: “You guys are completely providing a service, and of course this service costs money, you didn’t ask for payment, so I should initiate donation, that’s no problem.” (20, Beijing); and “This is a type of passing forward of trust…normally when you buy something, it’s a market exchange, one hand pays and one hand takes. But this has sentiment,” (30, Beijing).
Only one individual explicitly mentioned profiting from the generosity of others: “Originally the price is 150, I donated 10, just took advantage.” (29, STI clinic).
Community identity and collectivism
Most participants also discussed how pay-it-forward enhanced community identity and desire to help the community. Some said that pay-it-forward was attractive because it created a sense of belonging: “First it’s a project for the [gay] community, I feel like it can very much evoke the concept of community…helps one feel like he’s not alone, he is a part of this community,” (20, Beijing).
Others said that getting tested and then donating through pay-it-forward provided the opportunity to help the MSM community: “Normally…if you want to provide a helping hand specifically for LGBTQ health, there aren’t many opportunities, so this provided a great chance” (20, Beijing). A few men did not think that pay-it-forward increased their connection with the community: “Everyone getting tested is an individual, he doesn’t care about the previous person or the next person, he only cares about his own test…there isn’t a very apparent sense of connection in the project,” (29, Beijing).
Social norms and peer influence
Men also said that pay-it-forward helped normalize gonorrhea/chlamydia testing by conveying the fact that others have already participated: “When you see a message from the previous person, you think, I’m not the first person to [try something new], or I’m not the first to take this risk, this puts people at ease,” (26, CBO site). Some men felt that this was particularly important in the context of STI testing: “Some people…feel awkward or fear other people’s judgment, and they’re afraid to get tested…this can help those people have more courage” (26, Beijing).
At the same time, for a few participants, perceived social pressure also created anxiety over how much to donate despite reassurance that donation amount would be confidential: “We’ll always worry, if you can pay whatever you want, whether it’s too little…I have to donate something, I can’t donate nothing, I think no one else would donate nothing. I didn’t want to donate too little, and let everyone feel contempt,” (31, STI clinic). Some men pointed specifically to Chinese cultural norms: “Most Chinese people tend toward conformity. Because I’m not a big boss, I might not have as much as some…but I want to donate about the same as others…it’s shameful otherwise.” (28, Beijing).
Discussion
We conducted a mixed methods analysis to identify drivers of test uptake and donation to a pay-it-forward program. Quantitative and qualitative data both supported three main drivers unique to a pay-it-forward model of testing: flexible pricing; gift-giving, generosity and reciprocity; and community identity and collectivism. Qualitative results also identified the additional driver of norms and peer influence. This study expands the literature by evaluating a pay-it-forward program in a public health context, specifically STD testing among Chinese MSM.
We found that flexible pricing was a major driver of pay-it-forward. Quantitative analysis showed that income was not associated with getting tested, but the highest income category was associated with higher donations. Qualitative results showed that many men found flexible pricing to be an attractive component of the program, and further revealed that several participants only tested because the cost was covered by others. Taken together, these results suggest that the standard cost of 150 RMB is a barrier to some men, and that the flexible pricing model of pay-it-forward removed barriers which one might expect to be associated with income. Effectively, donations from higher-income individuals subsidized the cost of testing for lower-income individuals. Prior research suggests that cross-subsidization across income categories is a promising, acceptable financing mechanism for delivering health services to low-income populations (21, 22). Our program relies on a mix of participant incomes to help provide STI testing to MSM for whom cost may be a barrier.
Generosity and reciprocity also appeared to drive the pay-it-forward program. More than half of all testers selected “Someone has helped me and I can help someone else” as a benefit of pay-it-forward. Participants highlighted the attractiveness of framing the test as a gift, suggesting that gift marketing and promotional gifts, which are common sales strategies (23), may be applicable to health services. Moreover, this gift was an act of kindness from a previous participant, which was a key motivator for many men. This is consistent with previous work showing that generosity can spread through networks of unrelated individuals (14, 24). Some men were also motivated to donate by reciprocity with the organization providing testing out of obligation or because they believed “it is the right thing to do” (25). Our results suggest that concepts of gift-giving can be applied to STI testing, and that both generosity between testers and reciprocity between individuals and the testing organization can motivate contributions to public health programs.
We also found that community identity and collectivism were important components of pay-it-forward. More than half of all testers selected “More MSM can get tested” as a benefit of pay-it-forward, and selecting this option was associated with a higher donation. Qualitative results showed that men were attracted by the sense of belonging and agency that this program created. This is consistent with previous work showing that community engagement can positively influence HIV testing (26). Some were specifically motivated to test because of the opportunity to help the MSM community. Historically, many advances in HIV and STI testing among MSM have been catalyzed by community initiative (27, 28), and pay-it-forward provides a simple, tangible way to for MSM to engage with their health services. These results suggest that pay-it-forward may be particularly effective for MSM due to shared community identity. Future research should investigate pay-it-forward in other populations with shared identity.
Finally, social norms and peer influence also emerged as a driver of testing and donation in our qualitative results. Research has shown that peer influence can positively influence sexual health behavior and decrease stigma(29), consistent with our qualitative results. Social norms and the anticipated judgment of peers also generated social pressure to donate a certain amount. While this pressure encouraged donation among participants we interviewed, donation-based programs can sometimes fail due to too much anxiety over how much to pay (30), and selection bias inherently limits our ability to capture the role that this may have played. Future iterations of the program should attempt to balance the social pressure to donate without generating excessive anxiety and thus turning away potential participants.
To better understand a pay-it-forward gonorrhea/chlamydia testing program, we evaluated unique motivators of testing and donation to the program. Further research should also investigate operational and implementation facilitators and barriers of pay-it-forward. Since two main drivers include free/flexible pricing and generosity and reciprocity, pay-it-forward could potentially be useful for any public program that requires patients to pay a small fee. The drivers of community identity and social norms suggest that pay-it-forward could be particularly useful in groups with shared identity, or communities with shared social norms.
Our study has several limitations. First, pay-it-forward has only been implemented on a small scale, limiting our quantitative analysis. In particular, it was only implemented across three sites in Guangzhou and Beijing, some of the most economically developed cities in China. More research is required to determine whether these trends are found across larger populations, or in other regions.Our participants came from a wide range of income categories (Table 1). Second, our qualitative sample only consisted of men who who participated in pay-it-forward and were willing to express their thoughts about the program. This may have biased our sample toward men who were more enthusiastic about the program. We also did not extend interviews to men who chose not to participate in pay-it-forward and who may not have found the above drivers of testing and donating to be compelling.Third, the reimbursement for qualitative interviews was monetary, so it is also possible that our interview sample is more sensitive to financial reward than the general MSM population. Finally, because the questions we asked were related to finances, generosity, and MSM identity, it is possible that some participants were reluctant to disclose their true motivations. We emphasized that all data would be confidential and de-identified.
Conclusion
In a pay-it-forward model of gonorrhea and chlamydia testing for men who have sex with men in China, we found four drivers unique to pay-it-forward: flexible pricing, generosity and reciprocity, community identity and collectivism, and norms and peer influence. Pay-it-forward is a promising model for expanding sexual health services and other public programs which may cost a fee, particularly those involving communities with shared identity.
Supplementary Material
Acknowledgments:
We would like to thank our community partners at Zhitong and Lingnan Partners in Guangzhou, and at Blued in Beijing, as well as all study participants for their valuable input.
This study received support from the National Key Research and Development Program of China (2017YFE0103800), the National Institutes of Health (NIAID K24AI143471, NIA P30 AG034420), UNC Center for AIDS Research (NIAID 5P30AI050410), Doris Duke Charitable Foundation, and SESH (Social Entrepreneurship to Spur Health) Global. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript. The authors thank all people who contributed to this study.
Sources of support: This study was supported by the Doris Duke Charitable Foundation, the Weill Cornell Health Equity Fund, the Weill Cornell Center for Global Health, the Milton B. Rosenbluth Foundation, and US NIH.
Footnotes
Conflict of interest: The authors declare that they have no competing interests.
Patient consent: Obtained
Ethics approval: This study was approved by the institutional review boards at the University of North Carolina at Chapel Hill and Southern Medical University Dermatology Hospital.
References
- 1.Zetola NM, Bernstein KT, Wong E, et al. Exploring the relationship between sexually transmitted diseases and HIV acquisition by using different study designs. J Acquir Immune Defic Syndr. 2009;50(5):546–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernstein KT, Marcus JL, Nieri G, et al. Rectal gonorrhea and chlamydia reinfection is associated with increased risk of HIV seroconversion. J Acquir Immune Defic Syndr. 2010;53(4):537–43. [DOI] [PubMed] [Google Scholar]
- 3.Jones J, Weiss K, Mermin J, et al. Proportion of Incident HIV Cases among Men Who Have Sex with Men Attributable to Gonorrhea and Chlamydia: A Modeling Analysis. Sex Transm Dis. 2019; 46(6):357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X-S, Peeling RW, Yin Y-P, et al. The epidemic of sexually transmitted infections in China: implications for control and future perspectives. BMC Med. 2011;9(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang L-G, Zhang X-H, Zhao P-Z, et al. Gonorrhea and chlamydia prevalence in different anatomical sites among men who have sex with men: a cross-sectional study in Guangzhou, China. BMC Infect Dis. 2018;18(1):675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin L, Nehl EJ, Tran A, et al. Sexually transmitted infection testing practices among ‘money boys’ and general men who have sex with men in Shanghai, China: objective versus self-reported status. Sex Health. 2014;11(1):94–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu D, Li KT, Tang W, et al. Low Chlamydia and Gonorrhea Testing Rates Among Men Who Have Sex With Men in Guangdong and Shandong Provinces, China. Sex Transm Dis. 2019;46(4):260–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.China Centers for Disease Control and Prevention 2005. Website. Available at http://www.chinacdc.cn/jkzt/crb/zl/lb/zstd/200509/t20050922_24839.html Accessed February 21 2020.
- 9.Chen S, Li J, van den Hoek A. Universal Screening or Prophylactic Treatment for Chlamydia trachomatis Infection Among Women Seeking Induced Abortions: Which Strategy Is More Cost-Effective? Sex Transm Dis. 2007;34(4):230–6. [DOI] [PubMed] [Google Scholar]
- 10.Tang S, Tang W, Meyers K, et al. HIV epidemiology and responses among men who have sex with men and transgender individuals in China: a scoping review. BMC Infect Dis. 2016;16(1):588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng Y, Wu Z, Detels R. Evolution of MSM community and experienced stigma among MSM in Chengdu, China. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li KT, Tang W, Wu D, et al. Pay-it-forward strategy to enhance uptake of dual gonorrhea and chlamydia testing among men who have sex with men in China: a pragmatic, quasi-experimental study. Lancet Infect Dis. 2019;19(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hyde CR. Pay It Forward. New York, NY: Simon & Schuster; 1999. [Google Scholar]
- 14.Gray K, Ward AF, Norton MI. Paying it forward: generalized reciprocity and the limits of generosity. J Exp Psychol Gen. 2014;143(1):247–54. [DOI] [PubMed] [Google Scholar]
- 15.Cueva M. Thanks, au lait: 750 pay it forward at Starbucks location. CNN, 2014. Available from: https://edition.cnn.com/2014/08/21/us/starbucks-pay-it-forward-chain/index.html Accessed February 21st, 2020.
- 16.Wegert T. JetBlue Pays It Forward Through a Social Storytelling Campaign With No End in Sight. The Content Strategist; 2014. Available from: https://contently.com/2014/11/13/jetblue-pays-it-forward-through-a-social-storytelling-campaign-with-no-end-in-sight/ Accessed February 21st, 2020. [Google Scholar]
- 17.Yang F, Zhang T, Tang W., et al. Pay-it-Forward Gonorrhea and Chlamydia Testing Among Men Who Have Sex With Men in China: A Randomized Controlled Trial. Oral Presentation. University of North Carolina at Chapel Hill; August 15, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung MH, Nelson LD, Gneezy A, et al. Paying more when paying for others. J Pers Soc Psychol. 2014;107(3):414–31. [DOI] [PubMed] [Google Scholar]
- 19.WHO/TDR/SESH/SIHI. Crowdsourcing in Health and Health Research: A Practical Guide. Social Innovation in Health Initiative. Geneva: WHO/TDR; 2018. Available from: https://www.who.int/tdr/publications/year/2018/crowdsourcing-practical-guide/en/ Accessed February 21st 2020. [Google Scholar]
- 20.Tucker JD, Day S, Tang W, et al. Crowdsourcing in medical research: concepts and applications. PeerJ 2019;6:e6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goudge J, Akazili J, Ataguba J, et al. Social solidarity and willingness to tolerate risk- and income-related cross-subsidies within health insurance: experiences from Ghana, Tanzania and South Africa. Health Policy Plan. 2012;27 Suppl 1:i55–63. [DOI] [PubMed] [Google Scholar]
- 22.Bhattacharyya O, Khor S, McGahan A, et al. Innovative health service delivery models in low and middle income countries - what can we learn from the private sector? Health Res Policy and Syst. 2010;8(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taschetta J (Website) 2012. Accessed at https://www.clickz.com/why-gift-marketing-is-the-next-big-thing/42824/.
- 24.Fowler JH, Christakis NA. Cooperative behavior cascades in human social networks. Proc Natl Acad Sci USA. 2010;107(12):5334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riener G, Traxler C. Norms, moods, and free lunch: Longitudinal evidence on payments from a Pay-What-You-Want restaurant. J Socio Econ. 2012;41(4):476–83. [Google Scholar]
- 26.Zhang TP, Liu C, Han L, et al. Community engagement in sexual health and uptake of HIV testing and syphilis testing among MSM in China: a cross-sectional online survey. J Int AIDS Soc. 2017;20(1):21372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheng W, Cai Y, Tang W, et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016;94(3):222–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Trapence G, Collins C, Avrett S, et al. From personal survival to public health: community leadership by men who have sex with men in the response to HIV. Lancet. 2012;380(9839):400–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young SD, Konda K, Caceres C, et al. Effect of a community popular opinion leader HIV/STI intervention on stigma in urban, coastal Peru. AIDS and Behavior. 2011;15(5):930–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gneezy A, Gneezy U, Riener G, et al. Pay-what-you-want, identity, and self-signaling in markets. Proc Natl Acad Sci USA. 2012;109(19):7236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


