Abstract
Purpose of Review
T cell prolymphocytic leukemia (T-PLL) is a rare mature T cell tumor. Available treatment options in this aggressive disease are largely inefficient and patient outcomes are highly dissatisfactory. Current therapeutic strategies mainly employ the CD52-antibody alemtuzumab as the most active single agent. However, sustained remissions after sole alemtuzumab-based induction are exceptions. Responses after available second-line strategies are even less durable. More profound disease control or rare curative outcomes can currently only be expected after a consolidating allogeneic hematopoietic stem cell transplantation (allo-HSCT) in best first response. However, only 30–50% of patients are eligible for this procedure. Major advances in the molecular characterization of T-PLL during recent years have stimulated translational studies on potential vulnerabilities of the T-PLL cell. We summarize here the current state of “classical” treatments and critically appraise novel (pre)clinical strategies.
Recent Findings
Alemtuzumab-induced first remissions, accomplished in ≈ 90% of patients, last at median ≈ 12 months. Series on allo-HSCT in T-PLL, although of very heterogeneous character, suggest a slight improvement in outcomes among transplanted patients within the past decade. Dual-action nucleosides such as bendamustine or cladribine show moderate clinical activity as single agents in the setting of relapsed or refractory disease. Induction of apoptosis via reactivation of p53 (e.g., by inhibitors of HDAC or MDM2) and targeting of its downstream pathways (i.e., BCL2 family antagonists, CDK inhibitors) are promising new approaches. Novel strategies also focus on inhibition of the JAK/STAT pathway with the first clinical data. Implementations of immune-checkpoint blockades or CAR-T cell therapy are at the stage of pre-clinical assessments of activity and feasibility.
Summary
The recommended treatment strategy in T-PLL remains a successful induction by infusional alemtuzumab followed by a consolidating allo-HSCT in eligible patients. Nevertheless, long-term survivors after this “standard” comprise only 10–20%. The increasingly revealed molecular make-up of T-PLL and the tremendous expansion of approved targeted compounds in oncology represent a “never-before” opportunity to successfully tackle the voids in T-PLL. Approaches, e.g., those reinstating deficient cell death execution, show encouraging pre-clinical and first-in-human results in T-PLL, and urgently have to be transferred to systematic clinical testing.
Keywords: T-PLL, T cell lymphoma, Alemtuzumab, p53 reactivation, HDAC, BCL2 antagonists, JAK/STAT inhibition
Introduction
T cell prolymphocytic leukemia (T-PLL) is an aggressive peripheral (post-thymic) T cell malignancy [1••]. With an incidence of ≈ 2.0/million/year, it is still the most common mature T cell leukemia in Western countries [2]. The median age at disease onset is ≈ 65 years [3]. T-PLL patients typically present with exponentially rising blood lymphocyte counts, bone marrow infiltration, splenomegaly, and small lymphadenopathy. Their dismal prognosis is reflected in a median overall survival (OS) from diagnosis of < 3 years [4–7].
T-PLL cells show a refractory behavior towards conventional chemotherapeutics like alkylating agents or CHOP polychemotherapy [8, 9]. Even after responses to the humanized CD52-antibody alemtuzumab, the most active single substance in T-PLL being effective in > 80% of patients, nearly all relapse at median within 12 months [3, 5, 10], with very limited options to salvage. Allogenic hematopoietic stem cell transplantation (allo-HSCT) is the only treatment of curative potential, however, most patients are ineligible, or experience critical side effects, or relapse within the first years from this intervention [11•]. There is currently no drug that carries FDA or EMA approval status for T-PLL. This applies to alemtuzumab as well and this antibody is currently only available through a named-patient program. These circumstances emphasize the need for new active treatments in this orphan disease.
Particularly in the past 5 years, modern profiling studies on sizable T-PLL cohorts and mechanistic validations have significantly advanced our disease concept. Activation of the T cell leukemia/lymphoma 1 (TCL1) proto-oncogenes and loss-of-function perturbations of the tumor suppressor ataxia telangiectasia mutated (ATM) are the most common genomic lesions of T-PLL [12•, 13••]. Both aberrations cooperate towards an aberrant DNA damage response [13••]. JAK/STAT-activation and epigenetic alterations have also emerged as hallmarks and further contribute to the genome-instability and cell-death resistant phenotype [13••, 14, 15•]. They provide new possibilities for targeting T-PLL [16].
The improved molecular understanding of T-PLL has resulted in encouraging preliminary results on the anti-leukemic activity of new substances with realistic potential to become part of our armentarium in this disease. In vitro drug screenings identified p53 reactivators, histone deacetylase (HDAC) inhibitors, B cell lymphoma 2 (BCL2) inhibitors, Janus kinase (JAK) inhibitors, and cyclin-dependent kinase inhibitors (CDK) as the most prominent categories [17, 18••]. The clinical activity of JAK/STAT inhibitors as well as of BCL2 inhibition was presented in first reports in relapsed T-PLL patients [19, 20].
Taken together, identification of actionable vulnerabilities and proof-of-principle preclinical data have initiated a dynamic era of clinical investigations of substances (re)purposed for targeting T-PLL. This systematic overview outlines the current state-of-the-art, summarizes advances in novel targeted approaches, and highlights promising directions in the treatment of T-PLL.
Current Treatment Options
A stable or slowly progressing disease can be referred to as “inactive” T-PLL, which is initially found in ≈ 20–30% of patients [1••]. For these, there is yet no evidence for a benefit of immediate treatment initiation. However, virtually all cases convert into an “active” T-PLL disease within 1–2 years, eventually requiring treatment [21]. Currently, the recommended first-line therapy is infusional alemtuzumab followed by an allo-HSCT, where possible [5]. For transplant-ineligible patients, there is no concept of consolidation after alemtuzumab-based induction. In the following, we discuss advances in the categories of chemo(immuno)therapy and HSCT in T-PLL. Table 1 summarizes the most important clinical studies therein. Overall, the rarity of T-PLL dictates the scarcity of systematic trials. Most of them conceptualized the use of alemtuzumab, as a single agent or in combination with a chemotherapy component.
Table 1.
Synopsis of important clinical trials that specifically addressed T-PLL
| Summary of most relevant clinical studies on chemo-/immunotherapy in T-PLL | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Regime | Study design | Treatment status | n | ORR | CR | PR | PFS | OS | Reference |
| [%] | [%] | [%] | [mo] | [mo] | |||||
| Pentostatin | Single center, retrospective | Pretreated | 56 | 45 | 9 | 36 | 6 | 9 | [9] |
| Alemtuzumab, iv | Single center, retrospective | Pretreated | 15 | 73 | 60 | 13 | 6 | 8 | [34] |
| Alemtuzumab, iv | Multicenter, prospective | Pretreated | 39 | 76 | 60 | 16 | 7 | 10 | [33] |
| Alemtuzumab, iv | Multicenter, retrospective | Untreated | 4 | 75 | 75 | 0 | 5 | 8.7 | [30] |
| Pretreated | 72 | 50 | 37.5 | 12.5 | 4.5 | 7.5 | |||
| Pentostatin + alemtuzumab, iv | Single center, prospective | Pretreated | 13 | 69 | 62 | 8 | 7.8 | 10.2 | [39] |
| Alemtuzumab, iv | Single center, prospective | Untreated | 32 | 91 | 81 | 10 | 12 | 48 | [10] |
| Pretreated | 45 | 74 | 60 | 14 | 12 | 48 | |||
| Alemtuzumab, sc | Untreated | 9 | 33 | 33 | 0 | 12 | 48 | ||
| FMC + alemtuzumab, iv | Multicenter, prospective | Untreated | 16 | 92 | 48 | 44 | 11.5 | 17.1 | [5] |
| Pretreated | 9 | ||||||||
| Bendamustine | Multicenter, retrospective | Untreated | 6 | 55.3 | 20 | 33.3 | 5 | 8.7 | [24] |
| Pretreated | 9 | ||||||||
| Alemtuzumab, iv | Single center, retrospective | Untreated | 13 | n.a. | n.a. | n.a. | n.a. | 40.5 | [32] |
| Alemtuzumab, sc | Single center, retrospective | Pretreated | 5 | n.a. | n.a. | n.a. | n.a. | 13.7 | [32] |
| Alemtuzumab, iv + cladribine +/− HDAC inhibition | Single center, retrospective | Untreated | 4 | 100 | 75 | 25 | 6.3 | 14.8 | [52] |
| Pretreated | 4 | 100 | 100 | 0 | 11.35 | 23.7 | |||
| Alemtuzumab, iv | Single center, retrospective | Untreated | 42 | 81 | 61 | 20 | 11 | 15 | [31•] |
| Pretreated | 15 | 46 | 46 | 0 | 3 | 15 | |||
| Alemtuzumab, iv + pentostatin | Untreated | 13 | 82 | 73 | 9 | 4.3 | 10.4 | ||
| Pretreated | 5 | 75 | 50 | 25 | 2.6 | 2.6 | |||
| FMC + alemtuzumab, sc | Multicenter, prospective | Untreated | 13 | 68.7 | 32.1 | 36.6 | 7.5 | 11.5 | [26•] |
| Pretreated | 5 | ||||||||
iv intravenous, sc subcutaneous, FMC fludarabine, mitoxantrone, cyclophosphamide, HDAC histone deacetylase
Conventional Cytostatics
Initial, mostly futile, attempts to treat T-PLL focused on alkylators, anthracyclines, and purine analogs or their combinations. CHOP (cyclophosphamide, doxorubicin, vincristine, prednisolone) or CHOP-like regimens induced responses in only 33% of previously untreated T-PLL without adding to the median overall survival (OS) of 7.5 months that patients faced during this era [8].
Treatment with the purine analogs pentostatin and nelarabine showed overall response rates (ORRs) in previously untreated T-PLL of 33–45% and 20%, respectively, with 63% for the combination of nelarabine with fludarabine. However, complete responses (CRs) were rarely accomplished in these studies and the remissions where short-lived (≈ 6 months) [9, 22, 23]. Bendamustine showed an ORR of 67% in treatment-naive T-PLL and of 53% in a mixed cohort (6 untreated and 9 previously treated), presenting the most promising results of a single chemotherapeutic with a milder reported toxicity profile compared to other cytostatics in T-PLL [24, 25•].
Polychemotherapy of fludarabine, mitoxantrone, and cyclophosphamide (FMC) induced high ORRs (68%; including 36% pre-treated patients) in a prospective phase-II trial of sequential FMC-plus-alemtuzumab by our study group [5]. However, an OS benefit after alemtuzumab consolidation over single-agent alemtuzumab (Table 1) was not accomplished.
In essence, chemotherapy is not recommended as a first-line treatment in T-PLL, unless there is well-documented severe intolerance towards alemtuzumab. It is rather an option in relapsed or primary alemtuzumab-refractory patients with the best clinical evidence for bendamustine. FMC is the most active first-line chemotherapy regimen, likely also to be active in a salvage situation [5, 26•]. Encouraging data on the nucleoside cladribine are discussed in “New rational-based approaches at conceptual stages and with first (pre)clinical evidence”.
Alemtuzumab Remains the Current Benchmark
A milestone in the treatment of T-PLL was the implementation of alemtuzumab (Campath-1H). It is a fully-humanized IgG1 antibody targeting the surface CD52 antigen. Virtually all T-PLL express CD52 and at a higher density than in other T cell and B cell malignancies [27]. Engagement of CD52 by alemtuzumab induces antibody-dependent cytolysis, activation of the complement system, and possibly direct apoptosis [28, 29].
In treatment-naïve T-PLL, alemtuzumab induces ORRs of 75–92% (CRs in 48–81%), with no major difference between its use as a single substance or in combination with a conventional cytostatic. The progression-free survival (PFS) ranged from 7 to 12 months in these series [5, 10, 26•, 30, 31•]. These data by far surpass those of sole chemotherapy-based inductions. Importantly, alemtuzumab should be administered intravenously; the subcutaneous route is inferior in terms of response rates and freedom from disease as demonstrated in three independent studies [10, 26•, 32].
Alemtuzumab is generally well-tolerated [5, 10]. Initial infusion reactions are the most common side effects. Hematotoxicity of grades 3/4 occurs in 10–20% during the recommended 12-week period of 3 × 30 mg i.v./week [33, 34]. A PJP and HSV/CMV prophylaxis (and regular CMV monitoring) has to be implemented during treatment with this highly immunosuppressive agent [35, 36]. CMV reactivations occur in 19–52%, of which around 2/3 are clinically relevant [5, 26•]. EBV-positive B cell lymphomas were reported as rare events under alemtuzumab in the context of multiple sclerosis and in 2 T-PLL patients [37, 38].
The combination of alemtuzumab with the FMC chemo-regimen did not prolong PFS in two studies [5, 26•], despite a higher rate of BM-confirmed CRs when intravenous alemtuzumab followed 4 cycles of FMC. These studies rather emphasized that the added toxicity by such a chemo-component can compromise the administration of effective dosages of alemtuzumab. Therefore, alemtuzumab is currently recommended as a single-agent first-line treatment. In scenarios of insufficient responses to alemtuzumab, the nucleoside analogs fludarabine or pentostatin are the most frequent chemotherapeutics to be added to this antibody.
To accomplish long-term disease-free survival is the main challenge after alemtuzumab induction. Although > 80% of patients demonstrate initial remissions, in virtually all of them the disease recurs (at median after ≈ 12 months) in the absence of a consolidation by an allo-HSCT. There is no data that would justify an alemtuzumab maintenance after an induction therapy [26•]. At relapse, expression of CD52 should be reassessed (not by BM-histochemistry, which is prone to false-negative results) as ≈ 50% of patients respond to alemtuzumab re-treatment, although with a shorter PFS and OS [10]. A combination of alemtuzumab with pentostatin showed ORRs of 69% in a mixed cohort (5 treatment-naive and 8 previously treated T-PLL) [39]. Alemtuzumab relapsed/refractory (r/r) T-PLL is currently the main target population of individual exploratory concepts and trials. Attempts to improve primary alemtuzumab responses and their durations, e.g., by targeted agents such as JAK inhibitors, are currently underway (e.g., NCT03989466).
Hematopoietic Stem Cell Transplantation
T-PLL patients, in which a CR can be achieved, need to be considered for allo-HSCT, the currently only treatment option to confer long-term disease control in T-PLL. In our experience, only 30–50% of T-PLL patients are eligible for an allo-HSCT, most commonly because of reduced performance status, relevant comorbidities, and age. A wash-out period between the last alemtuzumab administration and HSCT infusion is recommended to avoid related engraftment failures [40].
Retrospective studies showed the potential of allo-HSCT in inducing durable remissions [5, 41–46]. Therein, a 3–5-year post-HSCT survival was achieved in ≈ 20–30% of transplanted patients. Underlying reasons for these sobering results are high rates of early relapse (30–40%) and a considerable transplantation related mortality (TRM) of 30–40%.
A recently published prospective multi-center observational study emphasized the possibility of achieving a long-term disease-free survival in T-PLL patients after allo-HSCT (4-year PFS 30%, 4-year OS 42%) [47••]. By defining inclusion criteria in this registry, homogeneity of the analyzed cohort was accomplished and selection biases were reduced. While the overall relapse incidence was ≈ 38% after 4 years, this rate was significantly reduced in patients, who received conditioning regimens containing a total body irradiation of 6 Gy or more. Notably, an association of the time between alemtuzumab and allo-HSCT with disease control or non-relapse mortality, as previously described [41], was not observed. Furthermore, a graft-versus-leukemia (GvL) activity is described for T-PLL, as demonstrated by a reduction of minimal residual disease after immune modulations [48]. Overall, with the restrictions of sample size and study heterogeneity allowing no legitimate comparisons, outcomes in T-PLL patients after allo-HSCT seem to have improved within the last years (4-year OS 42% published in 2019 [47••] vs 2-year OS 21% published in 2012 [41], Table 2). Better patient selection (i.e. intent of allo-HSCT in first CR after alemtuzumab instead as a salvage attempt) and general advances in the allo-HSCT procedure may represent the main causes for such improvements.
Table 2.
Summary of clinical studies that evaluated hematopoietic stem cell transplantation in T-PLL
| Study design | n | Age [years] | Relapse rate [%] | TRM [%] | Pre-HSCT CR [%] | Post-HSCT CR [%] | PFS [mo] | OS | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Summary of clinical studies on auto-HSCT in T-PLL | |||||||||
| Multi-center, retrospective | 15 | 58 | 60 | 7 | 87 | 100 | n.a. | 52 mo | [42] |
| Summary of clinical studies on allo-HSCT in T-PLL | |||||||||
| Multicenter, retrospective | 13 | 51 | 33 | 31 | 69 | 92 | n.a. | 33mo | [42] |
| CIBMTR registry, retrospective | 21 | 54 | 39* | 28* | n.a. | n.a. | 5.1 | 11.2mo | [43] |
| EBMT registry, retrospective | 41 | 51 | 41** | 41** | 27 | n.a. | 10 | 21%** | [41] |
| Multicenter, prospective | 5 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | 24.8mo | [5] |
| French Society of SCT, retrospective | 27 | 53 | 47 | 31** | 52 | 78 | 26** | 36%** | [44] |
| Single-center, retrospective | 11 | 56 | 21*** | 34*** | 91 | 91 | 15 | 56mo | [45] |
| EBMT registry, prospective (a) | 37 | 56 | 38*** | 32*** | 62 | n.a. | 30*** | 42%*** | [47••] |
| TRUMP registry, retrospective | 20 | 54 | 69.6** | 20.9* | 30 | n.a. | 33.5%** | 40%** | [46] |
(a) Patients < 65 years, with progressive disease, with a mismatched unrelated donor or with cord blood were excluded
*at one year
**at three years
***at four years
EBMT: European Society for Blood and Marrow Transplantation; CIBMTR: Center for International Blood and Marrow Transplant Research; TRUMP: Transplant Registry Unified Management Program, Japan
Nevertheless, considering the still high relapse rates and above-average TRM, allo-HSCT in T-PLL requires profound optimizations: (i) robust strata that better identify who would benefit from an allo-HSCT, (ii) primary induction of more profound remissions without adding toxicity in patients that enter allo-HSCT, (iii) conditioning regimens that include specifically T-PLL-targeting components, (iv) better diagnostic and therapeutic tools to address residual T-PLL that causes post-transplant relapse, and (v) general strategies reducing the TRM and better directing the dichotomy of GvL vs GvHD.
When an allo-HSCT is not feasible (e.g., T-PLL patients without a donor), autologous HSCT (auto-HSCT) after high-dose chemotherapy can be considered. A post-induction auto-HSCT also achieved prolonged OS and PFS, but was not associated with long-term survival [42]. In addition, relapse rates are significantly higher, while TRM is lower compared to patients receiving an allo-HSCT. Table 2 provides a summary of studies that evaluated allo- and auto-HSCT in T-PLL.
New Rational-based Approaches at Conceptual Stages and with First (Pre)Clinical Evidence
Given that cures are only accomplished in a very small subset of T-PLL and that for the majority of patients the prognosis is dismal, there is an urgent need for new substances, especially in alemtuzumab r/r disease. Recent in vitro drug screening approaches revealed new compound classes (e.g., p53 reactivators, epigenetic modulators, JAK inhibitors, and CDK inhibitors) as potentially active in T-PLL [13••, 17, 18••]. Of note, these studies did not involve therapeutic antibodies, did not address T-PLL in the context of (immune)milieu components, and did not systematically address synergistic relationships. Nevertheless, their findings of identified pathway dependencies align well with a recently advanced mechanistic disease concept of a (epi)genetically defined phenotype of inefficient checkpoint induction (e.g., repair, cell-cycle arrest, apoptosis) after DNA-damage and stress induction [13••].
Importantly, heterogeneous responses across T-PLL patients in vitro and in vivo are reported for these promising drug categories. This calls for better integration with molecular data towards models of individual sensitivity prediction [49]. In the following, we will focus on those substance classes and principles that have been evaluated for T-PLL specifically. Publications on such novel strategies are summarized in Table 3.
Table 3.
Reference list summarizing the most important literature on new interventional strategies in T-PLL
| Novel therapeutic approaches | |
|---|---|
| Strategy | Reference |
| Epigenetic modulation | [13••, 17, 18••, 52] |
| P53 reactivation | [13••, 18••] |
| Inhibition of constitutive JAK/STAT signaling | [17, 18••, 19, 20] |
| Antagonists of BCL2 family molecules | [17, 18••, 59•, 60, 61, 64, 65] |
| Inhibitors of cyclin-dependent kinases | [18••] |
| Modulation of immune cell synapses | [76] |
| CAR-T cell therapy | [79••] |
Epigenetic Modulation
Recent genomic profiling series revealed high frequencies of mutations of genes being essential in histone modifications, e.g., mutations of the histone methyltransferases KMT2C, KMT2D, KMT5A, and EZH2 [12•, 13••, 16, 50]. In addition, the expression of genes encoding for components of epigenetic regulation is significantly altered in T-PLL [13••]. Because post-transcriptional modifications mediated by epigenetic regulators play an important role in DNA-damage repair via de-/acetylation of histones and of proteins like p53 or ATM [51], epigenetic dysregulations represent a targetable vulnerability in T-PLL.
In accordance with the high incidence of genomic alterations affecting epigenetic regulators in T-PLL, screening approaches identified inhibitors of HDACs as one of the most potent substance classes in T-PLL in vitro [13••, 17, 18••]. Importantly, HDAC inhibitors (vorinostat, belinostat, romidepsin) are FDA approved for the treatment of nodal and cutaneous peripheral T cell lymphomas (PTCL, CTCL). In a series of eight relapsed T-PLL patients, the combination of HDAC inhibitors with cladribine, a purine analog with epigenetic activity, enhanced the anti-leukemic activity of alemtuzumab and overcame previous treatment resistance towards this antibody as shown by responses in all treated patients (7 of 8 achieved a CR) [52]. Furthermore, an induction of CD30 expression after treatment with this combination was reported therein. Although our laboratory and others were not able to induce CD30 upon exposure to this combination (data not shown), these authors report that treatment with the anti-CD30 immunotoxin brentuximab vedotin led to a reduction of alemtuzumab refractory skin lesions after such epigenetic priming in two intensively pretreated T-PLL patients [52].
Other epigenetic approaches focus on the combination of HDAC inhibition with DNA-damage induction. We described a rational-based marked in vitro synergy in T-PLL by the pan-HDAC inhibitor panobinostat in combination with bendamustine [13••]. Moreover, tinostamustine (EDO-S101), a fusion molecule of vorinostat covalently linked to bendamustine, was granted FDA fast-track approval for T-PLL based on our pre-clinical data [53]. This novel deacetylating alkylator displayed promising in vitro and in-vivo anti-T-PLL activity and is likely to be investigated further in T-PLL patients and in other hematologic and solid-tumor entities.
Strategies of p53 Reactivation
In contrast to many other tumors, the TP53 gene in T-PLL is rarely the target of deletions or mutations [13••]. Instead, we demonstrated the marked inability of the T-PLL cell to evoke p53 activation due to deficient upstream signals through hypomorphic ATM [13••]. This led to a concept of functionally intact p53 to be arrested in an inactive state bound to its inhibitor mouse double minute 2 (MDM2) and being largely deacetylated [16]. We reasoned from this that deacetylase inhibitors (i.e., HDAC inhibitors) and MDM2/4 antagonists would act as anti-leukemic p53 derepressors in T-PLL. Indeed, treatment of T-PLL cells with the MDM2 inhibitor idasanutlin restored the functional capacity of p53 as demonstrated by its phosphorylation and acetylation, which was even more prominent in combination with the pan-HDAC inhibitor panobinostat [13••]. Moreover, in an independent screen of 301 drugs, the p53 reactivator Prima-1-Met was the second most efficient substance inducing cell death of T-PLL cells in vitro [18••]. In addition, the MDM2 antagonists serdemetan and nutlin-3 were among the 20 most potent drugs in this study. Another ex vivo drug profiling effort further underlined the synergism between p53 reactivation and HDAC inhibition [16]. Importantly, the presented MDM2 antagonists showed selectivity in killing T-PLL cells with nearly no cell death in normal T cells. MDM2 antagonists are currently tested for advanced solid and hematologic tumors in early-stage trials, however, their clinical applicability in T-PLL still has to be evaluated.
Of note, the efficiency of poly ADP-ribose polymerase (PARP) inhibition was reasoned based on the assumption of a synthetic lethal relationship with the mutated and deleted ATM recurrently found in T-PLL (> 85%). However, such a hyper-sensitivity was not observed [13••].
Inhibition of Constitutive JAK/STAT Signaling
Gain-of-function mutations in JAK and STAT genes have been described recently to be highly frequent in T-PLL, varying from 36% to 76%, although often found as sub-clonal lesions [15•]. This makes the JAK/STAT pathway, a cytokine-triggered mediator of proliferation, differentiation, and migration of T cells, an interesting target [54]. Predominantly, JAK1, JAK3, and STAT5B are affected, accompanied by a high prevalence of genomic losses of negative regulators (71%) [15•]. Such genomically determined JAK/STAT activation in 90% of T-PLL explains the elevated STAT5b phosphorylation we observed in virtually all cases [13••, 15•]. In the mentioned sensitivity screen by Andersson et al., JAK inhibitors were among the 25 most effective substances in inducing cell death in T-PLL [18••]. The frequently occurring STAT5B N642H mutation even predicted resistance towards JAK inhibition. These results were supported in another drug screen of a large panel of blood cancers, in which T-PLL showed the highest sensitivity towards JAK inhibitors [17]. JAK inhibitors are currently approved in autoimmune conditions and GvHD, while inhibitors of STAT proteins are still under pre-clinical development [55]. First case reports on the clinical use of JAK inhibitors in T-PLL presented moderate activity of tofacitinib (inhibition of JAK2/3) and ruxolitinib (inhibition of JAK1/2) [19, 20]. A phase-I trial investigating the safety and tolerability of the JAK1 inhibitor itacitinib in combination with alemtuzumab in T-PLL is currently commencing recruitment (NCT03989466). Therapeutic approaches targeting JAK/STAT signaling have to be expanded, including the development of new, SH2-selective or N-domain targeting STAT5 inhibitors [56].
Antagonists of BCL2 Family Molecules
P53 mediates apoptosis through direct effects at the mitochondrial membrane as well as through transcriptional activation of pro-apoptotic B cell lymphoma 2 (BCL2) family molecules. An equilibrium of the concentrations and affinities of pro- and anti-apoptotic BCL2 proteins (both multidomain), as well as BH3-only proteins hereby regulates apoptosis induction. Interaction between pro- and anti-apoptotic molecules and between the pro-apoptotic proteins and the effectors BCL2-associated X protein (BAX) and BCL2 homologous antagonist killer (Bak) takes place at the BH3 domain, which is therefore essential for apoptosis induction by modulation of the mitochondrial outer membrane permeability [57]. As p53 activation is deficient in T-PLL (see “Strategies of p53 Reactivation”), inducing apoptosis downstream of p53 by targeting the BH3 domain of anti-apoptotic BCL2 family proteins with BH3 mimetics is a reasonable strategy [16]. Mutations in BCL2 family genes are not described in T-PLL [12•, 13••, 58].
Ex vivo screens revealed high anti-leukemic activity of the BCL2 inhibitors navitoclax (targets BCL2 and BCL-XL) and venetoclax (BCL2 only) in T-PLL [17, 18••]. It is still not finally resolved whether the responses to venetoclax correlate with the expression of BCL2, or with the expression of other anti-apoptotic family members such as myeloid cell leukemia 1 (MCL1) or B cell lymphoma XL (BCL-XL)(own data, not shown and [59•]). In comparison to CLL, BCL2 dependence appears lower and cells were less primed towards apoptosis in T-PLL, while MCL1 dependences are comparable, as revealed by first BH3-profiling studies [60].
First clinical case reports showed partial responses (PRs) after treatment with single-agent venetoclax in 2 r/r T-PLL patients [59•]. The first patients responded rapidly but developed a tumor lysis syndrome during dose increments, while the ramp-up was completed in the second patient without any tumor lysis syndrome and a PR was achieved for 131 days. Induction of BCL2 and BCL-XL protein expression was observed in these patients upon venetoclax treatment, potentially explaining modes of venetoclax resistance.
Aiming at identifying potentially synergistic partners, a combination screen identified ibrutinib (inhibitor of IL-2 inducible T cell kinase, ITK) as a suitable co-treatment. This was underlined by an increase of BCL2 dependence after ibrutinib priming, the latter having no effect on T-PLL cell viability [61]. This corroborates data by us and others, in which single-agent ITK inhibitors led to a diminished activation upon T cell receptor (TCR) stimulation, but did not affect viability of T-PLL cells [62, 63]. Two r/r T-PLL patients treated with the combination of venetoclax and ibrutinib showed substantial clinical responses [61]. Based on these pilot data, an international study evaluating the efficiency of venetoclax plus ibrutinib in alemtuzumab r/r T-PLL was initiated and is currently recruiting (VIT trial, NCT03873493).
BCL2 dependence can obviously also be enhanced by co-treatment with JAK/STAT or HDAC inhibitors, leading to a pronounced in vitro anti-T-PLL effect of venetoclax [60]. Combination of venetoclax with the purine analog pentostatin was tested in one r/r T-PLL case, resulting in a CR [64]. Besides targeting BCL2, inhibition of the anti-apoptotic MCL1 represents another strategy to be further investigated in T-PLL [65].
Future research has to identify markers that detect the likely considerable number of T-PLL that are insensitive to BCL2 inhibition, has to elucidate mechanisms of resistance towards BH3 mimetics and how to overcome them, and has to determine the most ideal combination partners of this compound class.
Inhibitors of Cyclin-dependent Kinases
In the before-mentioned drug screen of 301 compounds, the CDK inhibitor SNS-032 was the top-scoring substance [18••]. SNS-032 particularly inhibits CDK-2, -7, and -9. Notably, sensitivity of T-PLL cases towards SNS-032 correlated with high MYC expression [18••]. Downregulation of MCL1 is described as one potential mechanism through which inhibitors of CDK9 work, leading to the hypothesis of a good synergism between specific CDK9 inhibitors and BH3 mimetics, which has to be evaluated in future research [66].
Potential Approaches Adopted from Other T Cell Lymphomas
Molecules under investigation for the treatment of other T cell lymphomas will likely also influence the field of T-PLL [67]. Important to mention is the inhibition of the phosphoinositide 3-kinase (PI3K, e.g., via Copanlisib, Duvelisib) or combined JAK/STAT-SYK inhibitors (e.g., Cerdulatinib) [67–69]. Ex vivo, blocking of PI3K led to a reduced growth of primary T-PLL cells [6]. Other strategies focus on targeting chemokine receptors via antibodies. Mogamulizumab (anti-C-C chemokine receptor type 4) currently enters the treatment of CTCL [70].
At the epigenetic level, besides HDAC inhibition, targeting of EZH1/2 appears as a reasonable strategy, as suggested by the high frequency of mutations of this histone methyltransferase in T-PLL [12•, 13••, 16, 50]. EZH2, which plays a role in T cell differentiation and malignant transformation, was previously described as highly expressed across most PTCL [71, 72]. GSK2816126, which inhibits wildtype and mutated EZH2, is currently tested in advanced solid and hematologic tumors, although with signals of considerable side effects [73].
Modulation of Immune Cell Synapses
Inhibitors of the T cell immune-checkpoints are being tested in PTCL [67]. However, there are several notes of caution to be stressed with respect to uncritical applications to any T cell tumor. T-PLL shows marked normal-T cell penia and tumor cells have drastically down-regulated checkpoint molecules, including PDL1, without knowing whether this is true for the hardly detectable non-malignant (effector T cells) [13••]. Furthermore, PD1 is a potent tumor-suppressor, and its blockade may lead to tumor progression as experimentally implicated [74]. Importantly, clinical hyper-progressions have already been described in PTCL after nivolumab [75].
Another approach of immunogenic cell death induction is to exploit the interaction of CD47 with its ligand signal regulatory protein α (SiRPα). By targeting tumor-cell CD47 through a decoy receptor (SiRPαFc), reverting the “do-not-eat-me” signal to bystander macrophages, a significant reduction of tumor load was observed in various hematologic malignancies, i.e., CTCL [76]. Perturbation of NK-cell tolerance, e.g., by anti-KIR3DL2 antibodies, is a further strategy of proven activity in other T cell tumors [76, 77]. The clinical utility of these concepts in T-PLL should be part of future research.
Outlook for CAR-T Cell Therapy
The emerging field of chimeric antigen receptor T cells (CAR-T cells) also raised interest in the field of T cell malignancies [78]. Antigens that are unique to the T cell malignancies are rare, an exception might be CD30. Therefore, CAR-T cell-based targeting of pan-T cell antigens would lead to severe T cell immunosuppression as well as CAR-T cell fratricide. An elegant study took advantage of the TCR beta-chain constant (TRBC) locus clonality. While normal T cell populations are a mixture of TRBC1 and TRBC2 positive cells, malignant Tcells only express one beta-chain. First in vitro data showed that CAR-T cells, selectively targeting the TRBC of the malignant clone, specifically killed T-PLL cells, while sparing healthy T cells expressing a different TRBC [79••]. Another possible target for personalized CAR-T cells is the complementarity-determining region 3 (CDR3), which is the hypervariable region of the TCR being responsible for binding of the antigen. Data on anti-CDR3 CAR-T cells have not been reported in T-PLL [80].
Conclusions
T-PLL remains a highly problematic disease with poor outcome data and very limited therapeutic options. Induction by infusional alemtuzumab followed by a consolidating allo-HSCT in the 30–50% eligible patients leads to a long-term survival in a < 50% fraction of transplanted patients, resulting in 5–10% of all T-PLL patients that would have such a benefit from this approach. The modalities in alemtuzumab r/r disease are of lesser efficacy and the responses are short-lived.
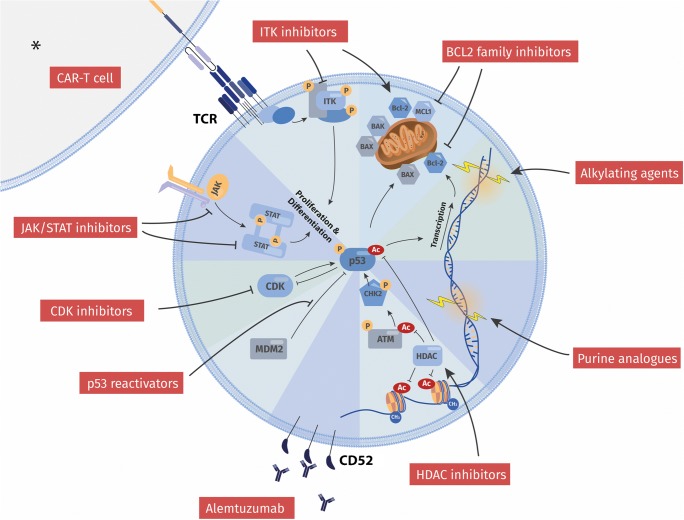
This review, however, shall stimulate optimism among physicians, researchers, and patients. The field of T-PLL has never been that active before. Academia and pharmaceutical companies gain increasing interest in T cell tumors, including T-PLL, for which we still lack approved drugs. We have arrived at a much better understanding of the molecular make-up of T-PLL and have identified key vulnerabilities [13••]. Consequently, novel therapeutic approaches are on the horizon, mainly represented by epigenetic modulators, p53 reactivators, JAK/STAT inhibitors, and BH3 mimetics, with the latter being closest to systematic clinical testing (Fig. 1). These will likely be supplemented by those that prove to be successful in other T cell malignancies. They will include in addition to repurposed cytostatics, so-called small molecules, novel antibodies, immune-synapse reshaping agents, or CAR-T-cells.
Fig. 1.
Overview of current and novel treatment strategies in T-PLL in relation to functional hallmarks of the tumor cell. Illustrated are categories of targets and modes of action of both established and most promising compound classes. Current treatment of T-PLL employs a (chemo)-immunotherapeutic approach based on alemtuzumab as well as on DNA-damaging alkylating agents and purine analogs. The inability of the T-PLL cell to evoke adequate p53-mediated responses to DNA-injuries, e.g., via enforced checkpoints or an apoptotic fate, stands at the center of its notorious therapy resistance. Novel strategies, however, revert the repressed state of functionally competent p53, or harness the apoptotically primed cellular state, or interrupt vital growth signal input. Respective examples are reactivation of p53 (e.g., via HDAC inhibitors, MDM2 inhibitors), targeting of BCL2 family members, inhibition of CDKs, or interception in JAK/STAT signal transduction. Efforts are also undertaken to utilize immunogenic cell death, e.g., by implementation of CAR-T cell therapies. * Generally, the role of cellular components of the tumor micromilieu is not established in T-PLL. Nevertheless, clinically proven GvL effects [48] and TCR-directed CAR-T cells in pre-clinical models [79••] implicate a therapeutic application of a T cell-mediated anti-T-PLL attack. Modulation of immune regulatory synapses, e.g., by perturbation of NK-cell tolerance (e.g., anti-KIR3DL2) or of macrophage inertia (e.g., SIRPαFc binding to CD47) represent interventional strategies of proven activity in other T cell tumors [76, 77], which have yet to be evaluated for their efficacy in T-PLL
We are looking forward to more-than-ever concerted efforts (i) to identify novel vulnerabilities in T-PLL, (ii) to describe optimal drug synergisms (including those with alemtuzumab or allo-HSCT protocols), (iii) to develop prediction tools for individual (pre)clinical responses, (iv) to devise strategies in dealing with resistance, and (v) to implement this in international clinical trials, overall to substantially improve the outcomes of T-PLL. Researchers in this orphan disease should also understand themselves as advocates for the multi-faceted needs of T-PLL patients, e.g., access to specialists, to off-label options, and to trial sites as well as in the promotion of fast-track drug approvals.
Acknowledgments
T.B. and L.W. are supported by the Köln Fortune program of the University of Cologne. M.H. is supported by the DFG Research Unit FOR1961 (Control-T; HE3553/4-2) and by the Fritz Thyssen Foundation (10.15.2.034MN).
Funding Information
Open Access funding provided by Projekt DEAL. This work was also supported by the EU Transcan-2 consortium “ERANET-PLL” and by the ERAPerMed consortium “JAKSTAT-TARGET.”
Compliance with Ethical Standards
Not applicable.
Conflict of Interest
T. Braun reports a stipend from the Köln Fortune program at Cologne University during the conduct of the study. J. von Jan has nothing to disclose. L. Wahnschaffe also receives support by the Köln Fortune program. Dr. Herling holds patents on TCL1 monoclonal antibodies (research and diagnostic use) with royalties paid.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by any of the authors.
Footnotes
Topical Collection on T-Cell and Other Lymphoproliferative Malignancies
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Staber PB, Herling M, Bellido M, Jacobsen ED, Davids MS, Kadia TM, et al. Consensus criteria for diagnosis, staging, and treatment response assessment of T-cell prolymphocytic leukemia. Blood. 2019;134:1132–1143. doi: 10.1182/blood.2019000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herling M, Khoury JD, Washington LT, Duvic M, Keating MJ, Jones D. A systematic approach to diagnosis of mature T-cell leukemias reveals heterogeneity among WHO categories. Blood. 2004;104:328–335. doi: 10.1182/blood-2004-01-0002. [DOI] [PubMed] [Google Scholar]
- 3.Dearden C. How I treat prolymphocytic leukemia. Blood. 2012;120:538–551. doi: 10.1182/blood-2012-01-380139. [DOI] [PubMed] [Google Scholar]
- 4.Cross M, Dearden C. B and T cell prolymphocytic leukaemia. Best Pract Res Clin Haematol. 2019;32:217–228. doi: 10.1016/J.BEHA.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Hopfinger G, Busch R, Pflug N, Weit N, Westermann A. Sequential chemoimmunotherapy of fludarabine, mitoxantrone, and cyclophosphamide induction followed by alemtuzumab consolidation is effective in T-cell Prolymphocytic leukemia. Cancer. 2013;119:2258–2267. doi: 10.1002/cncr.27972. [DOI] [PubMed] [Google Scholar]
- 6.Herling M, Patel KA, Teitell MA, Konopleva M, Ravandi F, Kobayashi R, et al. High TCL1 expression and intact T-cell receptor signaling define a hyperproliferative subset of T-cell prolymphocytic leukemia. Blood. 2008;111:328–37. 10.1182/blood-2007-07-101519. [DOI] [PMC free article] [PubMed]
- 7.Ravandi F, O’Brien S, Jones D, Lerner S, Faderl S, Ferrajoli A, et al. T-cell Prolymphocytic leukemia: a single-institution experience. Clin Lymphoma Myeloma. 2005;6:234–239. doi: 10.3816/CLM.2005.N.051. [DOI] [PubMed] [Google Scholar]
- 8.Matutes E, Brito-Babapulle V, Swansbury J, Ellis J, Morilla R, Dearden C, et al. Clinical and laboratory features of 78 cases of T-prolymphocytic leukemia. Blood. 1991;78:3269–74. [PubMed]
- 9.Mercieca J, Matutes E, Dearden C, MacLennan K, Catovsky D. The role of pentostatin in the treatment of T-cell malignancies: analysis of response rate in 145 patients according to disease subtype. J Clin Oncol. 1994;12:2588–2593. doi: 10.1200/JCO.1994.12.12.2588. [DOI] [PubMed] [Google Scholar]
- 10.Dearden CE, Khot A, Else M, Hamblin M, Grand E, Roy A, et al. Alemtuzumab therapy in T-cell prolymphocytic leukemia: comparing efficacy in a series treated intravenously and a study piloting the subcutaneous route. Blood. 2011;118:5799–802. 10.1182/blood-2011-08-372854. [DOI] [PubMed]
- 11.Herling M. Are we improving the outcome for patients with T-cell prolymphocytic leukemia by allogeneic stem cell transplantation? Eur J Haematol. 2015;94:191–192. doi: 10.1111/ejh.12462. [DOI] [PubMed] [Google Scholar]
- 12.Kiel MJ, Velusamy T, Rolland D, Sahasrabuddhe AA, Chung F, Bailey NG, et al. Integrated genomic sequencing reveals mutational landscape of T-cell prolymphocytic leukemia. Blood. 2014;124:1460–1472. doi: 10.1182/blood-2014-03-559542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schrader A, Crispatzu G, Oberbeck S, Mayer P, Pützer S, von Jan J, et al. Actionable perturbations of damage responses by TCL1/ATM and epigenetic lesions form the basis of T-PLL. Nat Commun. 2018;9:697. doi: 10.1038/s41467-017-02688-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johansson P, Klein-Hitpass L, Choidas A, Habenberger P, Mahboubi B, Kim B, et al. SAMHD1 is recurrently mutated in T-cell prolymphocytic leukemia. Blood Cancer J. 2018;8:11. 10.1038/s41408-017-0036-5. [DOI] [PMC free article] [PubMed]
- 15.Wahnschaffe L, Braun T, Timonen S, Giri AK, Schrader A, Wagle P, et al. JAK/STAT-activating genomic alterations are a hallmark of T-PLL. Cancers (Basel) 2019;11:1833. doi: 10.3390/cancers11121833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schrader A, Braun T, Herling M. The dawn of a new era in treating T-PLL. Oncotarget. 2019;10:626–628. doi: 10.18632/oncotarget.26595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dietrich S, Oleś M, Lu J, Sellner L, Anders S, Velten B, et al. Drug-perturbation-based stratification of blood cancer. J Clin Invest. 2018;128:427–45. 10.1172/JCI93801. [DOI] [PMC free article] [PubMed]
- 18.•• Andersson EI, Pützer S, Yadav B, Dufva O, Khan S, He L, et al. Discovery of novel drug sensitivities in T-PLL by high-throughput ex vivo drug testing and mutation profiling. Leukemia. 2017;32:774 Integrative high-throughputex vivodrug screen highlighting inhibition of HDAC, JAK/STAT, and CDK as well as reactivation of p53 as promising thereputic strategies in T-PLL. [DOI] [PubMed]
- 19.Gomez-Arteaga A, Margolskee E, Wei MT, van Besien K, Inghirami G, Horwitz S. Combined use of tofacitinib (pan-JAK inhibitor) and ruxolitinib (a JAK1/2 inhibitor) for refractory T-cell prolymphocytic leukemia (T-PLL) with a JAK3 mutation. Leuk Lymphoma. 2019;60:1626–1631. doi: 10.1080/10428194.2019.1594220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei M, Koshy N, van Besien K, Inghirami G, Horwitz SM. Refractory T-cell Prolymphocytic leukemia with JAK3 mutation: in vitro and clinical synergy of tofacitinib and ruxolitinib. Blood. 2015;126:5486. 10.1182/blood.V126.23.5486.5486
- 21.Garand R, Goasguen J, Brizard A, Buisine J, Charpentier A, FranCois Claisse J, et al. Indolent course as a relatively frequent presentation in T-prolymphocytic leukaemia. Br J Haematol. 1998;103:488–494. doi: 10.1046/j.1365-2141.1998.00977.x. [DOI] [PubMed] [Google Scholar]
- 22.Gandhi V, Tam C, O’Brien S, Jewell RC, Rodriguez CO, Lerner S, et al. Phase I trial of nelarabine in indolent leukemias. J Clin Oncol. 2008;26:1098–1105. doi: 10.1200/JCO.2007.14.1986. [DOI] [PubMed] [Google Scholar]
- 23.Dohner H, Ho AD, Thaler J, Stryckmans P, Sonneveld P, Witte T d, et al. Pentostatin in prolymphocytic leukemia: phase II trial of the European Organization for Research and Treatment of Cancer Leukemia Cooperative Study Group. J Natl Cancer Inst. 1993;85:658–662. doi: 10.1093/jnci/85.8.658. [DOI] [PubMed] [Google Scholar]
- 24.Herbaux C, Genet P, Bouabdallah K, Pignon J-M, Debarri H, Guidez S, et al. Bendamustine is effective in T-cell prolymphocytic leukaemia. Br J Haematol. 2015;168:916–919. doi: 10.1111/bjh.13175. [DOI] [PubMed] [Google Scholar]
- 25.• Zaja F, Baldini L, Ferreri AJM, Luminari S, Grossi A, Salvi F, et al. Bendamustine salvage therapy for T cell neoplasms. Ann Hematol. 2013;92:1249–54. 10.1007/s00277-013-1746-9Establishes Bendamustine as a clinical option in r/r T-PLL. [DOI] [PubMed]
- 26.Pflug N, Cramer P, Robrecht S, Bahlo J, Westermann A, Fink A-M, et al. New lessons learned in T-PLL: results from a prospective phase-II trial with fludarabine–mitoxantrone–cyclophosphamide–alemtuzumab induction followed by alemtuzumab maintenance. Leuk Lymphoma. 2019;60:649–657. doi: 10.1080/10428194.2018.1488253. [DOI] [PubMed] [Google Scholar]
- 27.Ginaldi L, De Martinis M, Matutes E, Farahat N, Morilla R, Dyer MJS, et al. Levels of expression of CD52 in normal and leukemic B and T cells: correlation with in vivo therapeutic responses to Campath-1H. Leuk Res. 1998;22:185–191. doi: 10.1016/S0145-2126(97)00158-6. [DOI] [PubMed] [Google Scholar]
- 28.Zhao Y, Su H, Shen X, Du J, Zhang X, Zhao Y. The immunological function of CD52 and its targeting in organ transplantation. Inflamm Res. 2017;66:571–578. doi: 10.1007/s00011-017-1032-8. [DOI] [PubMed] [Google Scholar]
- 29.Ruck T, Bittner S, Wiendl H, Meuth SG. Alemtuzumab in multiple sclerosis: mechanism of action and beyond. Int J Mol Sci. 2015;16:16414–16439. doi: 10.3390/ijms160716414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keating MJ, Cazin B, Coutré S, Birhiray R, Kovacsovics T, Langer W, et al. Campath-1H treatment of T-cell prolymphocytic leukemia in patients for whom at least one prior chemotherapy regimen has failed. J Clin Oncol. 2002;20:205–13. 10.1200/JCO.2002.20.1.205. [DOI] [PubMed]
- 31.Jain P, Aoki E, Keating M, Wierda WG, O’Brien S, Gonzalez GN, et al. Characteristics, outcomes, prognostic factors and treatment of patients with T-cell prolymphocytic leukemia (T-PLL) Ann Oncol. 2017;28:1554–1559. doi: 10.1093/annonc/mdx163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Damlaj M, Sulai NH, Oliveira JL, Ketterling RP, Hashmi S, Witzig T, et al. Impact of alemtuzumab therapy and route of administration in T-prolymphocytic leukemia: a single-center experience. Clin Lymphoma Myeloma Leuk. 2015;15:699–704. 10.1016/j.clml.2015.07.643. [DOI] [PubMed]
- 33.Dearden CE, Matutes E, Cazin B, Tjønnfjord GE, Parreira A, Nomdedeu B, et al. High remission rate in T-cell prolymphocytic leukemia with CAMPATH-1H. Blood. 2001;98:1721–6. 10.1182/blood.V98.6.1721. [DOI] [PubMed]
- 34.Pawson R, Dyer MJS, Barge R, Matutes E, Thornton PD, Emmett E, et al. Treatment of T-cell prolymphocytic leukemia with human CD52 antibody. J Clin Oncol. 1997;15:2667–2672. doi: 10.1200/JCO.1997.15.7.2667. [DOI] [PubMed] [Google Scholar]
- 35.O’Brien S, Ravandi F, Riehl T, Wierda W, Huang X, Tarrand J, et al. Valganciclovir prevents cytomegalovirus reactivation in patients receiving alemtuzumab-based therapy. Blood. 2008;111:1816–1819. doi: 10.1182/blood-2007-03-080010. [DOI] [PubMed] [Google Scholar]
- 36.Thursky KA, Worth LJ, Seymour JF, Miles Prince H, Slavin MA. Spectrum of infection, risk and recommendations for prophylaxis and screening among patients with lymphoproliferative disorders treated with alemtuzumab. Br J Haematol. 2006;132:3–12. doi: 10.1111/j.1365-2141.2005.05789.x. [DOI] [PubMed] [Google Scholar]
- 37.Sohani AR, Ferry JA, Chang PS, Abramson JS. Epstein-barr virus-positive diffuse large B-cell lymphoma during therapy with alemtuzumab for T-cell prolymphocytic leukemia. J Clin Oncol. 2010;28:e69–e72. doi: 10.1200/JCO.2009.24.4194. [DOI] [PubMed] [Google Scholar]
- 38.Alduaij A, Treaba DO, Winer ES. CD30-positive EBV–associated diffuse large B-cell lymphoma occurring after immunosuppressive therapy for T-cell prolymphocytic leukemia. Clin Lymphoma Myeloma Leuk. 2011;11:64–67. doi: 10.3816/CLML.2011.n.009. [DOI] [PubMed] [Google Scholar]
- 39.Ravandi F, Aribi A, O’Brien S, Faderl S, Jones D, Ferrajoli A, et al. Phase II study of alemtuzumab in combination with pentostatin in patients with T-cell neoplasms. J Clin Oncol. 2009;27:5425–5430. doi: 10.1200/JCO.2009.22.6688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Szuszies CJ, Hasenkamp J, Jung W, Koch R, Trümper L, Wulf GG. Loss of donor chimerism in remission after allogeneic stem cell transplantation of T-prolymphocytic leukemia patients following alemtuzumab induction therapy. Int J Hematol. 2014;100:425–428. doi: 10.1007/s12185-014-1678-8. [DOI] [PubMed] [Google Scholar]
- 41.Wiktor-Jedrzejczak W, Dearden C, de Wreede L, van Biezen A, Brinch L, Leblond V, et al. Hematopoietic stem cell transplantation in T-prolymphocytic leukemia: a retrospective study from the European Group for Blood and Marrow Transplantation and the Royal Marsden Consortium. Leukemia. 2012;26:972–976. doi: 10.1038/leu.2011.304. [DOI] [PubMed] [Google Scholar]
- 42.Krishnan B, Else M, Tjonnfjord GE, Cazin B, Carney D, Carter J, et al. Stem cell transplantation after alemtuzumab in T-cell prolymphocytic leukaemia results in longer survival than after alemtuzumab alone: a multicentre retrospective study. Br J Haematol. 2010;149:907–10. 10.1111/j.1365-2141.2010.08134.x. [DOI] [PubMed]
- 43.Kalaycio ME, Kukreja M, Woolfrey AE, Szer J, Cortes J, Maziarz RT, et al. Allogeneic hematopoietic cell transplant for prolymphocytic leukemia. Biol Blood Marrow Transplant. 2010;16:543–7. 10.1016/J.BBMT.2009.11.021. [DOI] [PMC free article] [PubMed]
- 44.Guillaume T, Beguin Y, Tabrizi R, Nguyen S, Blaise D, Deconinck E, et al. Allogeneic hematopoietic stem cell transplantation for T-prolymphocytic leukemia: a report from the French society for stem cell transplantation (SFGM-TC). Eur J Haematol. 2015;94:265–9. 10.1111/ejh.12430. [DOI] [PubMed]
- 45.Dholaria BR, Ayala E, Sokol L, Nishihori T, Chavez JC, Hussaini M, et al. Allogeneic hematopoietic cell transplantation in T-cell prolymphocytic leukemia: a single-center experience. Leuk Res. 2018;67:1–5. 10.1016/J.LEUKRES.2018.01.009. [DOI] [PubMed]
- 46.Yamasaki S, Nitta H, Kondo E, Uchida N, Miyazaki T, Ishiyama K, et al. Effect of allogeneic hematopoietic cell transplantation for patients with T-prolymphocytic leukemia: a retrospective study from the adult lymphoma working Group of the Japan Society for hematopoietic cell transplantation. Ann Hematol. 2019;98:2213–20. 10.1007/s00277-019-03759-y. [DOI] [PubMed]
- 47.Wiktor-Jedrzejczak W, Drozd-Sokolowska J, Eikema DJ, Hoek J, Potter M, Wulf G, et al. EBMT prospective observational study on allogeneic hematopoietic stem cell transplantation in T-prolymphocytic leukemia (T-PLL) Bone Marrow Transplant. 2019;54:1391–1398. doi: 10.1038/s41409-019-0448-x. [DOI] [PubMed] [Google Scholar]
- 48.Sellner L, Brüggemann M, Schlitt M, Knecht H, Herrmann D, Reigl T, et al. GvL effects in T-prolymphocytic leukemia: evidence from MRD kinetics and TCR repertoire analyses. Bone Marrow Transplant. 2017;52:544–51. 10.1038/bmt.2016.305. [DOI] [PubMed]
- 49.He L, Tang J, Andersson EI, Timonen S, Koschmieder S, Wennerberg K, et al. Patient-customized drug combination prediction and testing for T-cell prolymphocytic leukemia patients. Cancer Res. 2018;78:2407–2418. doi: 10.1158/0008-5472.CAN-17-3644. [DOI] [PubMed] [Google Scholar]
- 50.López C, Bergmann AK, Paul U, Murga Penas EM, Nagel I, Betts MJ, et al. Genes encoding members of the JAK-STAT pathway or epigenetic regulators are recurrently mutated in T-cell prolymphocytic leukaemia. Br J Haematol. 2016;173:265–73. 10.1111/bjh.13952. [DOI] [PubMed]
- 51.Tang Y, Zhao W, Chen Y, Zhao Y, Gu W. Acetylation is indispensable for p53 activation. Cell. 2008;133:612–626. doi: 10.1016/j.cell.2008.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hasanali ZS, Saroya BS, Stuart A, Shimko S, Evans J, Vinod Shah M, et al. Epigenetic therapy overcomes treatment resistance in T cell prolymphocytic leukemia. Sci Transl Med. 2015;7:293ra102. doi: 10.1126/scitranslmed.aaa5079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pützer S, Varghese L, von Jan J, Braun T, Giri A, Mayer P, et al. Reinstated p53 response and highanti-T-cell leukemia activity by the novel alkylating deacetylase inhibitortinostamustine. Leukemia 2020 (in press) [DOI] [PubMed]
- 54.Rawlings JS, Rosler KM, Harrison DA. The JAK/STAT signaling pathway. J Cell Sci. 2004;117:1281–1283. doi: 10.1242/jcs.00963. [DOI] [PubMed] [Google Scholar]
- 55.Wingelhofer B, Maurer B, Heyes EC, Cumaraswamy AA, Berger-Becvar A, de Araujo ED, et al. Pharmacologic inhibition of STAT5 in acute myeloid leukemia. Leukemia. 2018;32:1135–46. 10.1038/s41375-017-0005-9. [DOI] [PMC free article] [PubMed]
- 56.Orlova A, Wagner C, de Araujo ED, Bajusz D, Neubauer HA, Herling M, et al. Direct targeting options for STAT3 and STAT5 in cancer. Cancers. 2019;11:1930. 10.3390/cancers11121930 [DOI] [PMC free article] [PubMed]
- 57.Kale J, Osterlund EJ, Andrews DW. BCL-2 family proteins: changing partners in the dance towards death. Cell Death Differ. 2018;25:65–80. doi: 10.1038/cdd.2017.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johansson P, Klein-Hitpass L, Choidas A, Habenberger P, Mahboubi B, Kim B, et al. SAMHD1 is recurrently mutated in T-cell prolymphocytic leukemia. Blood Cancer J. 2018;8:1–16. 10.1038/s41408-017-0036-5. [DOI] [PMC free article] [PubMed]
- 59.• Boidol B, Kornauth C, van der Kouwe E, Prutsch N, Kazianka L, Gültekin S, et al. First-in-human response of BCL-2 inhibitor venetoclax in T-cell prolymphocytic leukemia. Blood. 2017;130:2499–503. 10.1182/blood-2017-05-785683Case reports of 2 r/r T-PLL patients with promising results after treatment with the BCL2 inhibitor venetoclax. [DOI] [PubMed]
- 60.Herbaux C, Kornauth C, Poulain S, Tournilhac O, Collins MC, Valentin R, et al. Characterizing the anti-apoptotic dependencies of T-cell prolymphocytic leukemia identifies HDAC and JAK/STAT pathway inhibitors as promising combination partners to augment Bcl-2 targeted killing by Venetoclax. Blood. 2019;134:807. doi: 10.1182/blood-2019-126773. [DOI] [Google Scholar]
- 61.Kornauth CF, Herbaux C, Boidol B, Guillemette C, Mayerhöfer ME, Jäger U, et al. The combination of venetoclax and ibrutinib is effective in relapsed/refractory T-prolymphocytic leukemia and influences BCL-2-family member dependencies. Hematol Oncol. 2019;37:482–484. doi: 10.1002/hon.161_2631. [DOI] [Google Scholar]
- 62.Dondorf S, Schrader A, Herling M. Interleukin-2-inducible T-cell kinase (ITK) targeting by BMS-509744 does not affect cell viability in T-cell prolymphocytic leukemia (T-PLL) J Biol Chem. 2015;290:10568–10569. doi: 10.1074/jbc.L115.644641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhong Y, Dong S, Strattan E, Ren L, Butchar JP, Thornton K, et al. Targeting interleukin-2-inducible T-cell kinase (ITK) and resting lymphocyte kinase (RLK) using a novel covalent inhibitor PRN694. J Biol Chem. 2015;290:5960–78. 10.1074/jbc.M114.614891. [DOI] [PMC free article] [PubMed]
- 64.Alfayez M, Thakral B, Jain P, Ravandi F, Ferrajoli A, Jain N, et al. First report of clinical response to venetoclax combination with pentostatin in T-cell-prolymphocytic leukemia (T-PLL). Leuk Lymphoma. 2019:1–5. 10.1080/10428194.2019.1660967. [DOI] [PMC free article] [PubMed]
- 65.Koch R, Christie AL, Crombie JL, Palmer AC, Plana D, Shigemori K, et al. Biomarker-driven strategy for MCL1 inhibition in T-cell lymphomas. Blood. 2019;133:566–75. 10.1182/blood-2018-07-865527. [DOI] [PMC free article] [PubMed]
- 66.Bose P, Gandhi V, Konopleva M. Pathways and mechanisms of venetoclax resistance. Leuk Lymphoma. 2017;58:1–17. doi: 10.1080/10428194.2017.1283032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ito Y, Makita S, Tobinai K. Development of new agents for peripheral T-cell lymphoma. Expert Opin Biol Ther. 2019;19:197–209. doi: 10.1080/14712598.2019.1572746. [DOI] [PubMed] [Google Scholar]
- 68.Horwitz SM, Koch R, Porcu P, Oki Y, Moskowitz A, Perez M, et al. Activity of the PI3K-δ,γ inhibitor duvelisib in a phase 1 trial and preclinical models of T-cell lymphoma. Blood. 2018;131:888–898. doi: 10.1182/blood-2017-08-802470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ng SY, Yoshida N, Christie AL, Ghandi M, Dharia NV, Dempster J, et al. Targetable vulnerabilities in T- and NK-cell lymphomas identified through preclinical models. Nat Commun. 2018;9:2024. 10.1038/s41467-018-04356-9. [DOI] [PMC free article] [PubMed]
- 70.Ollila TA, Sahin I, Olszewski AJ. Mogamulizumab: a new tool for management of cutaneous T-cell lymphoma. Onco Targets Ther. 2019;12:1085–1094. doi: 10.2147/OTT.S165615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gan L, Yang Y, Li Q, Feng Y, Liu T, Guo W. Epigenetic regulation of cancer progression by EZH2: from biological insights to therapeutic potential. Biomark Res. 2018;6:10. doi: 10.1186/s40364-018-0122-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang H, Lv H, Jia X, Hu G, Kong L, Zhang T, et al. Clinical significance of enhancer of zeste homolog 2 and histone deacetylases 1 and 2 expression in peripheral T-cell lymphoma. Oncol Lett. 2019;18:1415–23. 10.3892/ol.2019.10410. [DOI] [PMC free article] [PubMed]
- 73.Yap TA, Winter JN, Giulino-Roth L, Longley J, Lopez JS, Michot J-M, et al. Phase 1 study of the novel enhancer of zeste homolog 2 (EZH2) inhibitor GSK2816126 in patients with advanced hematological and solid tumors. Clin Cancer Res. 2019. 10.1158/1078-0432.CCR-18-4121. [DOI] [PMC free article] [PubMed]
- 74.Wartewig T, Kurgyis Z, Keppler S, Pechloff K, Hameister E, Öllinger R, et al. PD-1 is a haploinsufficient suppressor of T cell lymphomagenesis. Nature. 2017;552:121–5. 10.1038/nature24649. [DOI] [PMC free article] [PubMed]
- 75.Ratner L, Waldmann TA, Janakiram M, Brammer JE. Rapid progression of adult T-cell leukemia–lymphoma after PD-1 inhibitor therapy. N Engl J Med. 2018;378:1947–1948. doi: 10.1056/NEJMc1803181. [DOI] [PubMed] [Google Scholar]
- 76.Johnson LDS, Banerjee S, Kruglov O, Viller NN, Horwitz SM, Lesokhin A, et al. Targeting CD47 in Sézary syndrome with SIRPαFc. Blood Adv. 2019;3:1145–53. 10.1182/bloodadvances.2018030577. [DOI] [PMC free article] [PubMed]
- 77.Bagot M, Porcu P, Marie-Cardine A, Battistella M, William BM, Vermeer M, et al. IPH4102, a first-in-class anti-KIR3DL2 monoclonal antibody, in patients with relapsed or refractory cutaneous T-cell lymphoma: an international, first-in-human, open-label, phase 1 trial. Lancet Oncol. 2019;20:1160–70. 10.1016/S1470-2045(19)30320-1. [DOI] [PubMed]
- 78.Scherer LD, Brenner MK, Mamonkin M. Chimeric antigen receptors for T-cell malignancies. Front Oncol. 2019;9:126. doi: 10.3389/fonc.2019.00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maciocia PM, Wawrzyniecka PA, Philip B, Ricciardelli I, Akarca AU, Onuoha SC, et al. Targeting the T cell receptor β-chain constant region for immunotherapy of T cell malignancies. Nat Med. 2017;23:1416–1423. doi: 10.1038/nm.4444. [DOI] [PubMed] [Google Scholar]
- 80.Huang J, Alexey S, Li J, Jones T, Grande G, Douthit L, et al. Unique CDR3 epitope targeting by CAR-T cells is a viable approach for treating T-cell malignancies. Leukemia. 2019;33:2315–9. 10.1038/s41375-019-0455-3. [DOI] [PubMed]