Abstract
Acquired resistance to cyclin-dependent kinases 4 and 6 (CDK4/6) inhibition in estrogen receptor-positive (ER+) breast cancer remains a significant clinical challenge. Efforts to uncover the mechanisms underlying resistance are needed to establish clinically actionable targets effective against resistant tumors. In this study, we sought to identify differentially expressed genes (DEGs) associated with acquired resistance to palbociclib in ER+ breast cancer. We performed next-generation transcriptomic RNA sequencing (RNA-seq) and pathway analysis in ER+ MCF7 palbociclib-sensitive (MCF7/pS) and MCF7 palbociclib-resistant (MCF7/pR) cells. We identified 2183 up-regulated and 1548 down-regulated transcripts in MCF7/pR compared to MCF7/pS cells. Functional analysis of the DEGs using Gene Ontology (GO) and the Kyoto Encyclopedia of Genes and Genomes (KEGG) database identified several pathways associated with breast cancer, including ‘cell cycle’, ‘DNA replication’, ‘DNA repair’ and ‘autophagy’. Additionally, Ingenuity Pathway Analysis (IPA) revealed that resistance to palbociclib is closely associated with deregulation of several key canonical and metabolic pathways. Further studies are needed to determine the utility of these DEGs and pathways as therapeutics targets against ER+ palbociclib-resistant breast cancer.
Keywords: palbociclib, estrogen receptor, breast cancer, CDK4/6, CDK4/6 inhibitors, therapy resistance, DNA repair, metabolic rewiring
1. Introduction
Breast cancer is the most frequent malignancy among women, and approximately 60–70% of cases are estrogen receptor-positive (ER+). Selective inhibition of cyclin-dependent kinases 4 and 6 (CDK4/6) and ER signaling is now standard-of-care therapy for ER+ metastatic breast cancer [1]. Three CDK4/6 inhibitors, palbociclib, ribociclib and abemaciclib, are currently used in combination with endocrine therapy given their shown improvement in progression-free survival compared to endocrine therapy alone in the metastatic setting [2]. Despite the clear benefit of this combination, approximately 10% of patients remain insensitive, whereas nearly all patients become resistant within 12 to 36 months of therapy initiation [3]. Therefore, determining the underlying mechanisms of resistance is required to design novel treatment strategies that delay or overcome clinical resistance.
Previous studies have shown that resistance to palbociclib is commonly associated with cyclin E or CDK6 amplification, CDK2 activation and loss of the retinoblastoma (Rb) protein in ER+ breast cancer cells [4,5,6]. Analysis of circulating tumor DNA from patients enrolled in the PALOMA-3 trial (fulvestrant or fulvestrant + palbociclib) identified an enrichment of Rb mutations, although this only occurred in 4.5% of the palbociclib-treated cohort [7,8]. Importantly, acquired alterations in ESR and PIK3CA were also observed; however, these alterations occurred in both treatment arms indicating distinct events driving resistance to palbociclib versus fulvestrant [9]. Additional studies have implicated fibroblast growth factor receptor (FGFR) or aurora kinase A amplifications, enhanced MAPK or AKT signaling and decreased DNA repair as mechanisms of resistance against CDK4/6 inhibition [10,11,12,13]. Taken together, these studies have provided rationale for the testing of CDK4/6 inhibitors in combination with MEK or PI3K inhibitors [11,14].
The major goal of this study was to identify additional mechanisms of resistance to palbociclib in ER+ breast cancer cells through transcriptomic analyses. We previously demonstrated that ER+ palbociclib-resistant cells exhibit a marked decrease in the cellular antiviral interferon (IFN) response [6], and thus we expected that other drivers of resistance remained to be identified. Here, we determined the transcriptional landscape of ER+ MCF7 palbociclib-sensitive (MCF7/pS) and palbociclib-resistant (MCF7/pR) breast cancer cells via next-generation transcriptomic RNA sequencing (RNA-seq). Gene expression profile and pathway analysis identified significant canonical pathways associated with resistance to palbociclib including cell cycle regulation, immune responses and DNA damage repair (DDR) among others. Importantly, we identified several metabolic pathways uniquely enriched in palbociclib-resistant cells compared to palbociclib-sensitive cells. These studies provide a mechanistic base for the further validation of these pathways in mediating resistance to palbociclib.
2. Materials and Methods
2.1. Cell Culture, Generation of Palbociclib-Resistant Cells and Palbociclib Treatment
MCF7 (HTB-22) cells were purchased from the American Type Culture Collection (ATCC) and maintained at 37 °C with 5% CO2. MCF7 cells were cultured in IMEM (Corning) supplemented with 10% fetal bovine serum (FBS, Invitrogen). Drug-resistant MCF7 cells were established by culturing in media containing palbociclib (0.1–4 μM). Drug was replenished every 3 days. Cells were subcultured every 1–2 weeks with 25% increments in drug concentration. The resistant cells were established after 6 months and maintained in the presence of 1 μM palbociclib. Cells were authenticated by the short tandem repeat (STR) assay (Genetica).
2.2. RNA Extraction and Next-Generation Sequencing
MCF7/pS and MCF7/pR cells were seeded in 10 cm2 dishes at a density of 2 × 106 cells and allowed to incubate overnight prior to RNA extraction using the RNeasy kit (Qiagen) for a total of three independent replicates per cell line. Libraries were prepared simultaneously for all replicates and cell lines using the TruSeq Stranded mRNA LT Sample Prep Kit - Set A (Cat# RS-122-2101) with poly-A enrichment. Sequencing was performed on the University of Louisville Center for Genetics and Molecular Medicine’s (CGeMM) Illumina NextSeq 500 using the NextSeq 500/550 1 × 75 cycle High Output Kit v2 (Cat# FC-404-2005). A second run was performed on all samples to achieve an average of 45 million reads per sample.
2.3. DEG Analysis
The resulting samples were downloaded from Illumina’s BaseSpace [15] (https://basespace.illumina.com/). Sequences were directly aligned to the Homo sapiens hg38 reference genome assembly (hg38.fa) using tophat2 (version 2.0.13), generating alignment files in bam format. DEGs were identified for the pairwise comparison MCF7/pS versus MCF7/pR using the tuxedo suite programs including cufflinks-cuffdiff2 (VERSION2.2.1). A total of 60,603 ENSEMBL genes were considered. Of these, 26,837 showed no gene expression and were excluded. A q-value cutoff ≤ 0.05 with |log2FC| and gene expression greater than 1 in at least one replicate was used to determine differential expression. RNA-seq data are available (GEO accession number GSE130437). Gene Ontology Biological Processes (GO:BP) and KEGG pathway analysis was performed by using CategoryCompare [16].
2.4. In Silico Ingenuity Network Analysis
Pathway and biological processes analysis of all differentially expressed genes was performed using Ingenuity Pathway Analysis (Qiagen).
2.5. GFP-LC3 Visualization
Plasmid vector containing green fluorescent protein linked to microtubule-associated protein 1 LC3 was used to detect autophagosome formation in MCF7/pS and MCF7/pR cell lines [17]. Cells were treated with either vehicle control or palbociclib after 24 h of transfection. The expression of GFP was monitored by fluorescence microscopy 48 h after treatment. Cells were classified as having a predominantly diffuse GFP stain or having numerous punctate structures representing autophagosomes. Images were taken at 40× magnification with the EVOS FL Imaging System (Thermo Fisher Scientific, Waltham, MA, USA) under 357/44 and 447/60 nanometers (nm) excitation and emission visualization, respectively.
3. Results
3.1. RNA-Seq Profiling Reveals a Distinct Transcriptomic Profiling in Palbociclib-Resistant Cells
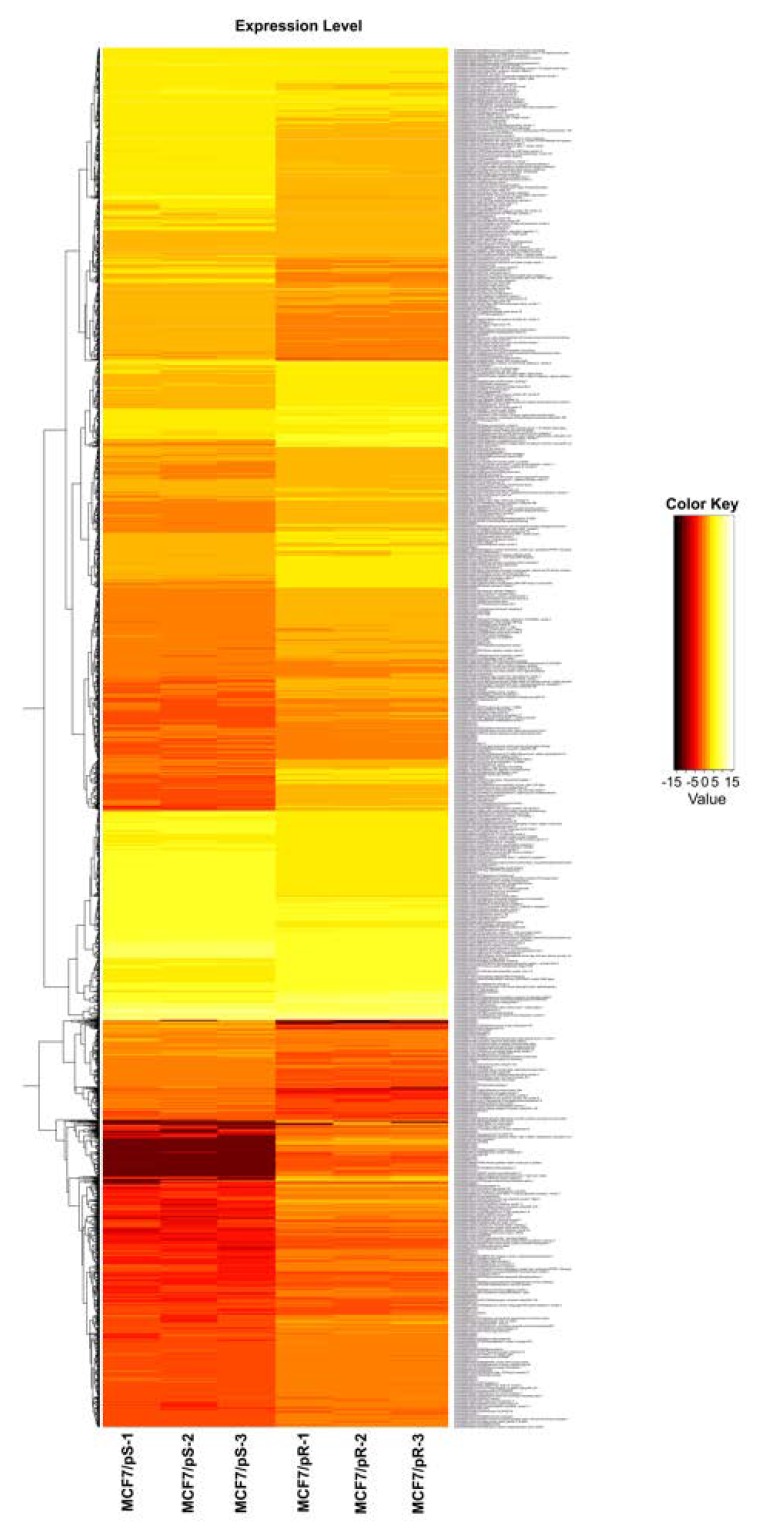
To characterize transcriptional alterations driven by acquired resistance to palbociclib, we performed gene expression profiling in MCF7/pS and MCF7/pR cells. These cells were developed by our group and were previously shown to be resistant to palbociclib [6]. Hierarchical clustering based on differentially expressed RNA transcripts revealed a distinct transcriptomic profile in MCF7/pR cells compared to MCF7/pS (Figure 1). Using a q-value cutoff ≤ 0.05 with |log2FC| , we identified 2183 up-regulated genes and 1548 down-regulated transcripts in MCF7/pR cells. Table 1 shows the top 20 up-regulated and down-regulated genes in MCF7/pR cells compared to MCF7/pS cells.
Figure 1.
Differential expression heatmap of estrogen receptor-positive (ER+) MCF7 palbociclib-sensitive (MCF7/pS) compared to MCF7 palbociclib-resistant (MCF7/pR) cells. Next-generation transcriptomic RNA sequencing (RNA-seq) was performed and the raw expression of genes is shown as a heatmap. Replicate samples are clustered. Red and yellow indicate lower and higher gene expression, respectively.
Table 1.
Top 20 up-regulated and down-regulated genes between MCF7/pS and MCF7/pR ranked by p-value (pval ≤ 0.05; qval ≤ 0.05; |log2FC| ≥ 1).
| Up-Regulated | Down-Regulated | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Ensembl ID | Gene Symbol|Description | Log2FC | p-Value | Q-value | Ensembl ID | Gene Symbol|Description | Log2FC | p-Value | Q-Value |
| ENSG00000011465 | DCN|decorin | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000211816 | TRAV38-1| | −16.6898 | 5 × 10−5 | 0.00026 |
| ENSG00000011677 | GABRA3|gamma-aminobutyric acid (GABA) A receptor, alpha 3 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000228340 | MIR646HG|MIR646 host gene | −16.6898 | 5 × 10−5 | 0.00026 |
| ENSG00000012223 | LTF|lactotransferrin | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000259761 | −16.6898 | 5 × 10−5 | 0.00026 | |
| ENSG00000070729 | CNGB1|cyclic nucleotide gated channel beta 1 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000082482 | KCNK2|potassium channel, two pore domain subfamily K, member 2 | −7.09413 | 5 × 10−5 | 0.00026 |
| ENSG00000079689 | SCGN|secretagogin, EF-hand calcium binding protein | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000182836 | PLCXD3|phosphatidylinositol-specific phospholipase C, X domain containing 3 | −6.53477 | 5 × 10−5 | 0.00026 |
| ENSG00000083782 | EPYC|epiphycan | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000253293 | HOXA10|homeobox A10 | −6.24454 | 5 × 10−5 | 0.00026 |
| ENSG00000086205 | FOLH1|folate hydrolase (prostate-specific membrane antigen) 1///FOLH1|folate hydrolase 1B | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000259527 | LINC00052|long intergenic non-protein coding RNA 52 | −6.17543 | 5 × 10−5 | 0.00026 |
| ENSG00000101441 | CST4|cystatin S | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000006747 | SCIN|scinderin | −5.91229 | 5 × 10−5 | 0.00026 |
| ENSG00000101460 | MAP1LC3A|microtubule-associated protein 1 light chain 3 alpha | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000110492 | MDK|midkine (neurite growth-promoting factor 2) | −5.60036 | 5 × 10−5 | 0.00026 |
| ENSG00000102854 | MSLN|mesothelin | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000140538 | NTRK3|neurotrophic tyrosine kinase, receptor, type 3 | −5.39223 | 5 × 10−5 | 0.00026 |
| ENSG00000104313 | EYA1|EYA transcriptional coactivator and phosphatase 1 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000102271 | KLHL4|kelch-like family member 4 | −5.2236 | 5 × 10−5 | 0.00026 |
| ENSG00000109846 | CRYAB|crystallin, alpha B | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000105974 | CAV1|caveolin 1, caveolae protein, 22kDa | −5.18256 | 5 × 10−5 | 0.00026 |
| ENSG00000111863 | ADTRP|androgen-dependent TFPI-regulating protein | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000112175 | BMP5|bone morphogenetic protein 5 | −5.08812 | 5 × 10−5 | 0.00026 |
| ENSG00000113805 | CNTN3|contactin 3 (plasmacytoma associated) | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000159618 | ADGRG5|adhesion G protein-coupled receptor G5 | −4.97744 | 5 × 10−5 | 0.00026 |
| ENSG00000115009 | CCL20|chemokine (C-C motif) ligand 20 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000174498 | IGDCC3|immunoglobulin superfamily, DCC subclass, member 3 | −4.96488 | 5 × 10−5 | 0.00026 |
| ENSG00000125788 | DEFB126|defensin, beta 126 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000168269 | FOXI1|forkhead box I1 | −4.95038 | 5 × 10−5 | 0.00026 |
| ENSG00000131095 | GFAP|glial fibrillary acidic protein | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000087077 | TRIP6|thyroid hormone receptor interactor 6 | −4.80366 | 5 × 10−5 | 0.00026 |
| ENSG00000139329 | LUM|lumican | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000134193 | REG4|regenerating islet-derived family, member 4 | −4.705 | 5 × 10−5 | 0.00026 |
| ENSG00000140287 | HDC|histidine decarboxylase | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000003436 | TFPI|tissue factor pathway inhibitor (lipoprotein-associated coagulation inhibitor) | −4.62227 | 5 × 10−5 | 0.00026 |
| ENSG00000146233 | CYP39A1|cytochrome P450, family 39, subfamily A, polypeptide 1 | 18.6778 | 5 × 10−5 | 0.00026 | ENSG00000064205 | WISP2|WNT1 inducible signaling pathway protein 2 | −4.57396 | 5 × 10−5 | 0.00026 |
3.2. KEGG Annotation of DEG and Enriched Biological Processes Analysis
To gain insight into the molecular mechanisms underlying palbociclib resistance, we performed KEGG pathway analysis of all DEGs identified using CategoryCompare [16]. Table 2 lists the enriched KEGG pathways identified in MCF7/pS vs. MCF7/pR cells (false discovery rate (FDR) ≤ 0.05 and p-value ≤ 0.001). The KEGG terms associated with resistance to palbociclib included ‘cell cycle’, ‘DNA replication’, ‘mismatch repair’ and ‘phagosome’. Subsequent analysis of GO:BP identified many enriched biological processes that correlated with palbociclib resistance (Figure 2). Importantly, we observed distinct groups of nodes such as DNA replication, cell cycle transition, mitosis, protein–DNA assembly and organization and response to virus revealing multiple functional ‘themes’ associated with resistance to palbociclib.
Table 2.
Top enriched KEGG terms between MCF7/pS and MCF7/pR ranked by p-value. (pval ≤ 0.05; qval ≤ 0.05; |log2FC| ≥ 1).
| KEGG ID | Description | p-value | FDR |
|---|---|---|---|
| 4110 | Cell cycle | 8.73 × 10−8 | 0 |
| 3030 | DNA replication | 1.20 × 10−7 | 0 |
| 4114 | Oocyte meiosis | 6.34 × 10−5 | 0 |
| 4914 | Progesterone-mediated oocyte maturation | 8.36 × 10−5 | 0 |
| 4360 | Axon guidance | 8.76 × 10−5 | 0 |
| 3430 | Mismatch repair | 5.20 × 10−4 | 0.01 |
| 4115 | p53 signaling pathway | 1.11 × 10−3 | 0.01143 |
| 4010 | MAPK signaling pathway | 2.91 × 10−3 | 0.03333 |
| 600 | Sphingolipid metabolism | 3.88 × 10−3 | 0.044 |
| 4145 | Phagosome | 4.78 × 10−3 | 0.05 |
Figure 2.
Enriched biological processes (BP) analysis of ER+ palbociclib-resistant breast cancer cells.
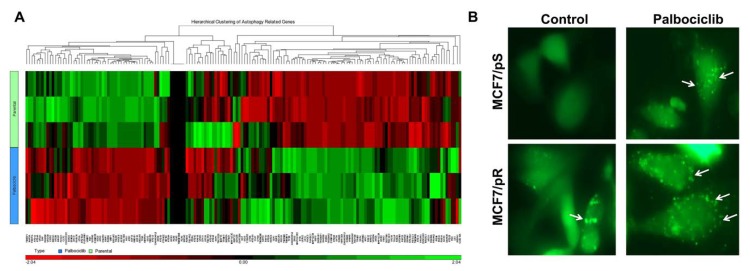
3.3. Resistance to Palbociclib Is Associated with Increased Autophagosome Formation
Characterization of MCF7/pR cells by KEGG pathway analysis revealed an enrichment in genes associated with phagosomes (Table 2). Given a previous observation suggesting a crosstalk between phagocytosis and autophagy, we sought to investigate autophagy levels in the context of resistance to palbociclib [18]. We performed hierarchical clustering of autophagy-related genes in MCF7/pS and MCF7/pR cells (Figure 3A). Using a p-value cutoff ≤ 0.05, we identified a significant number of autophagy-related genes differentially expressed in MCF7/pR compared to MCF7/pS cells. Next, we measured autophagosome formation by monitoring the conversion of cytoplasm-diffuse GFP-LC3-I to punctate forms of membrane-associated GFP-LC3-II, which indicates LC3-II incorporation into the autophagosomes. We observed that MCF7/pR cells displayed a significant increase in autophagosome formation compared to MCF7/pS and that the addition of palbociclib led to a marked increase in autophagosome formation in both MCF7/pS and MCF7/pR cells (Figure 3B). These results confirmed an increase in autophagy in MCF7/pR cells and are in line with previous studies [19]. Numerous studies have demonstrated that autophagy contributes to the resistance of breast cancer cells to targeted therapies by promoting tumor cell survival and blocking apoptosis [20,21,22]. Recently, it has been shown that autophagy inhibitors synergize with palbociclib in ER+ MCF7 and T47D breast cancer cells resulting in a significant increase in growth inhibition [19]. Our results provide rationale for the use of autophagy inhibitors to treat palbociclib-resistant cells in addition to palbociclib-sensitive cells. Future studies will test the efficacy of this combination against CDK4/6 inhibition in the resistance setting and determine the molecular mechanisms driving the increase in autophagy in resistant tumors.
Figure 3.
Increased autophagy is associated with palbociclib resistance in ER+ MCF7 cells. (A) Hierarchical clustering of autophagy-related genes performed by MetaCore analysis. (B) Cells were transfected with a pEGFP-LC3 plasmid and treated with either vehicle control (0.5% water) or 500 nM palbociclib for 24 h. Formation of autophagosomes is depicted by punctate structures (arrows). Images were taken at 40× magnification with an EVOS microscope.
3.4. Pathway Enrichment Analysis of DEG
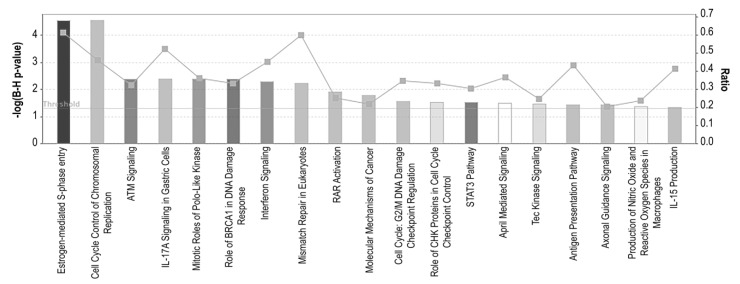
To identify potential targetable pathways, all altered transcripts were mapped to known pathways using Ingenuity Pathway Analysis (IPA). We observed significant enrichment of several canonical pathways including four pathways involved in cell cycle regulation (‘Estrogen-mediated S-phase entry’, ‘Cell cycle control of chromosomal replication’, ‘Mitotic roles of Polo-Like Kinase’ and ‘Role of CHK proteins in cell cycle checkpoint control’), four involved in DDR (‘ATM signaling’, ‘Role of BRCA in DNA damage response’, ‘Mismatch repair in eukaryotes’ and ‘G2/M DNA damage checkpoint regulation’), eight involved in immune responses (‘IL-17A signaling’, ‘Interferon signaling’, ‘STAT3 pathway’, ‘April mediated signaling’, ‘Tec Kinase signaling’, ‘Antigen presentation pathway’, ‘Production of nitric oxide and reactive oxygen species in macrophages’ and ‘IL-15 production’) among other pathways (Figure 4).
Figure 4.
Canonical pathway analysis of ER+ palbociclib-resistant breast cancer cells. A higher–log(B-H p-value) shown on the left Y axis represents more significant pathways. The ratio (right Y axis) refers to the number of genes from the data set that map to the pathway divided by the total number of genes that map the canonical pathway from the Ingenuity Pathway Analysis (IPA) database. pval ≤ 0.05; qval ≤ 0.05; |log2FC| ≥ 1.
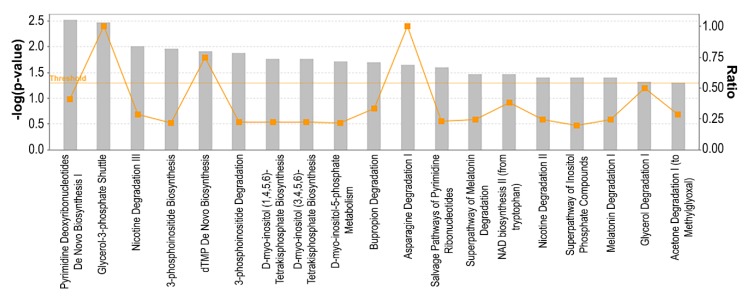
3.5. Metabolic Pathways Associated with Resistance to Palbociclib
Previous reports have indicated that cellular metabolism is a downstream target of CDK4/6 inhibition. Specifically, it has been shown that palbociclib administration increases glucose utilization in cancer, whereas cyclin D3-CDK6 can directly phosphorylate and inhibit the activity of two key enzymes in the glycolytic pathway [23,24]. To identify metabolic pathways associated with resistance to palbociclib, we performed metabolic pathway analysis of all DEGs using IPA (Figure 5). We observed an enrichment of several metabolic pathways including three pathways involved in ribonucleotides synthesis (‘Pyrimidine deoxyribonucleotides de novo biosynthesis I’, ‘dTMP de novo biosynthesis’ and ‘Salvage pathway of pyrimidine ribonucleotides’), six pathways involved in inositol metabolism (‘3-Phosphoinositide biosynthesis’, ‘3-Phosphoinositide degradation’, ‘D-myo-inositol(1,4,5,6)-tetrakisphosphate biosynthesis’, ‘D-myo-inositol-5-phosphate metabolism’ and ‘Superpathway of inositol phosphate compounds’). Among other pathways, we found ‘Glycerol-3-phosphate shuttle’, ‘Asparagine degradation’ and ‘NAD biosynthesis II (from tryptophan)’ to be enriched in our dataset. These results indicate that deregulated metabolism may play an essential role in mediating resistance to palbociclib.
Figure 5.
Metabolic pathway analysis of ER+ palbociclib-resistant breast cancer cells. A higher–log(p-value) shown on the left Y axis represents more significant pathways. The ratio (right Y axis) refers to the number of genes from the dataset that map to the pathway divided by the total number of genes that map the canonical pathway from the IPA database. pval ≤ 0.05; qval ≤ 0.05; |log2FC| ≥ 1.
4. Discussion
Three orally available inhibitors of CDK4/6 are currently used in combination with endocrine therapy (ET) as first-line therapy ER+ metastatic breast cancer patients [25]. Although initially beneficial, resistance to CDK4/6 inhibition arises in almost all patients within two years thus limiting durable responses. Currently, there are no biomarkers that can predict treatment response or early resistance [26]. Here, we identified a number of clinically relevant pathways that are associated with resistance to palbociclib, largely focusing on metabolic alterations and oncogenic signaling such as nucleotide metabolism, inositol metabolism, cell cycle, immune regulation and DDR.
Previous efforts to identify mechanisms of resistance to CDK4/6 inhibition have found that lack of Rb protein, increased cyclin E expression, IL6/STAT3 pathway activation and decreased DNA repair are some of the underlying mechanisms of resistance in ER+ breast cancer cells [6,13,19,27,28]. Analysis of ctDNA or tumor mRNA from patients enrolled in the PALOMA-3, NeoPalAna and MONALEESA-3 trials have identified Rb mutations, activating mutations in PIK3CA and ESR1, increased cyclin E1 and activation of the PDK1-AKT axis as some of the drivers of resistance [7,9,11]. Consistent with previous findings, we observed a significant enrichment in pathways involved in DDR [13]. Furthermore, we observed an increased in autophagy in MCF7/pR cells which is consistent with the previously described increase in autophagy driven by CDK4/6 inhibition in palbociclib-sensitive ER+ breast cancer cells [19]. Previous studies have shown that resistance to CDK4/6 inhibition is associated with a loss of ER/progesterone receptor (PR) expression in tumor biopsies of patients treated with the CDK4/6 inhibitor abemaciclib [5]. Notably, we observed a significant decrease in PR expression in palbociclib-resistant cells (Supplementary File 1). This finding is relevant given that unliganded PR sustains ER expression levels by maintaining a low methylation status of the ER gene [29]. Taken together, these observations suggest that PR loss may drive breast cancer cells to escape CDK4/6 inhibition by altering ER methylation thereby resulting in the down-regulation of ER expression. Additionally, our results highlight that ER methylation status can potentially be used to predict acquired resistance to CDK4/6 inhibition.
While our findings are in line with previously identified mechanisms of resistance, our analysis uncovered additional potential mechanisms of resistance such as deregulation of ‘Polo-Like Kinase (PLK)’, ‘April mediated signaling’ and ‘Tec Kinase signaling’. Of these, targeting PLK1 is of high relevance due to its role as a master regulator of the G2-M phase and DNA replication [30,31]. Importantly, PLK1 has been shown to play a role in mediating tamoxifen resistance in ER+ breast cancer cells, and thus we will conduct additional studies evaluating the role of PLK1 as a novel target for the ER+ breast cancer resistant to CDK4/6 inhibition [32]. Importantly, a potent PLK1 inhibitor, volasertib (BI6727), has been recently approved for the treatment of acute myeloid leukemia and would be a promising therapeutic agent against palbociclib-resistant breast cancer [33,34].
Close examination of the DEGs revealed significant expression changes in many genes involved in tumorigenesis and chemoresistance. For example, up-regulation of three of the small leucine-rich family of proteoglycans (SLRP), decorin, epiphycan and lumican, was observed in our dataset (Table 1). These proteoglycans are known for their ability to regulate cell signaling, adhesion, migration, proliferation and apoptosis in many types of cancer [35,36]. Notably, accumulated evidence supports a role for both decorin and lumican in mediating drug resistance, and thus our data suggest a potential role for these proteoglycans in mediating resistance to palbociclib [37,38,39,40,41]. Other promising genes that were shown to be up-regulated in our dataset were cystatin S and alpha B-crystallin. Elevated blood levels of cystatin-C have been detected in women with breast cancer and are shown to correlate with cancer progression [42,43]. Alpha B-crystallin expression has been associated with high metastatic potential, poor clinical outcome and drug resistance in breast cancer [44,45,46]. Our findings raise the possibility of the potential use of alpha B-crystallin and cystatin-C as biomarkers of sensitivity to CDK4/6 inhibition. Of the top 20 down-regulated genes, miR-646 host gene and homeobox A10 (HOXA10) are of great relevance given their emerging tumor suppressive functions. Expression of miR-646 has been shown to directly regulate CDK6 and FOXK1 expression in gastric cancer, suggesting its utility as a potential therapeutic target [47,48]. A lack of HOXA10 in breast cancer has been shown to decrease apoptosis and promote metastasis, and thus the role of HOXA10 in the context of palbociclib resistance warrants further investigation [49]. A limitation of our studies is the lack of validation of gene expression changes by real-time PCR; however, we believe that our initial profiling will help guide further efforts to better understand the molecular mechanisms driving drug resistance.
Metabolic reprograming is a well-established oncogenic driver that allows cells to support the increased bioenergetic and anabolic demands [50]. Importantly, CDK4/6 are key regulators of metabolic pathways, and therefore we anticipated that metabolic rewiring will be observed upon the development of resistance to palbociclib. While a previous study described an increase in glucose dependence in ER+/Her2- palbociclib-sensitive compared to palbociclib-resistant cells [51], to date little is known about global metabolic changes driving resistance to CDK4/6 inhibition. Our unbiased analysis of DEGs and metabolic pathways began to define metabolic hubs linked to palbociclib resistance. Specifically, we observed alterations in nucleotide metabolism in MCF7/pS vs. MCF7/pR cells. Importantly, these results are in line with previous reports indicating that increased expression of thymidine kinase-1 (TK1), an enzyme of the pyrimidine salvage pathway, correlates with poor prognosis in breast cancer patients treated with palbociclib [52,53,54,55].
Our findings indicate that inositol metabolism was altered in ER+ palbociclib-resistant cells. Given the role of inositols as essential membrane components crucial for the generation of secondary messengers, our results are of high biological significance and provide a direct link between signal transduction and metabolic alterations contributing to resistance. Future metabolomic profiling will be needed to confirm our initial findings and provide further evidence as to how inositol alteration contributes to resistance to palbociclib.
Collectively, our RNA-seq analysis uncovered key canonical and metabolic pathways altered in ER+ palbociclib-resistant cells and provided new insights into the molecular mechanisms and potential therapeutic targets underlying resistance to CDK4/6 inhibition.
Acknowledgments
We want to thank the University of Louisville’s Genomics Core facility and Nigel Cooper and Donald Miller for providing support for the Next-Gen RNA-seq studies.
Supplementary Materials
The following are available online at https://www.mdpi.com/2073-4425/11/4/467/s1, File S1: List of all DEG identified.
Author Contributions
Conceptualization, Y.I.-F.; methodology, L.L., C.O., N.L., J.G.G.-G., S.W.; software, E.R., X.L. and S.W.; validation, L.L., E.R., X.L. and Y.I.-F.; formal analysis, E.R., X.L., S.W. and Y.I.-F.; investigation, L.L., N.L. and Y.I.-F.; resources, E.R., X.L., S.W., J.C. and Y.I.-F.; data curation, E.R., X.L. and Y.I.-F.; writing—original draft preparation, Y.I.-F.; writing—review and editing, N.L., X.L., S.W., J.G.G.-G. and Y.I.-F.; visualization, J.G.G.-G. and Y.I.-F.; supervision, Y.I.-F.; project administration, Y.I.-F.; funding acquisition, J.C. and Y.I.-F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Twisted Pink (Yoannis Imbert-Fernandez, PI). Sequencing and bioinformatics support for this work was provided by the National Institutes of Health grants P20GM103436 (Nigel Cooper, PI) and P20GM106396 (Donald Miller, PI).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Rossi L., McCartney A., Risi E., De Santo I., Migliaccio I., Malorni L., Biganzoli L., Di Leo A. Cyclin-Dependent Kinase 4/6 Inhibitors in Neoadjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer. Clin. Breast Cancer. 2019;19:392–398. doi: 10.1016/j.clbc.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 2.Sobhani N., D’Angelo A., Pittacolo M., Roviello G., Miccoli A., Corona S.P., Bernocchi O., Generali D., Otto T. Updates on the CDK4/6 Inhibitory Strategy and Combinations in Breast Cancer. Cells. 2019;8:321. doi: 10.3390/cells8040321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang J., Wang Q., Wang Q., Cao J., Sun J., Zhu Z. Mechanisms of resistance to estrogen receptor modulators in ER+/HER2- advanced breast cancer. Cell. Mol. Life Sci. 2020;77:559–572. doi: 10.1007/s00018-019-03281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herrera-Abreu M.T., Palafox M., Asghar U., Rivas M.A., Cutts R.J., Garcia-Murillas I., Pearson A., Guzman M., Rodriguez O., Grueso J., et al. Early Adaptation and Acquired Resistance to CDK4/6 Inhibition in Estrogen Receptor-Positive Breast Cancer. Cancer Res. 2016;76:2301–2313. doi: 10.1158/0008-5472.CAN-15-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang C., Li Z., Bhatt T., Dickler M., Giri D., Scaltriti M., Baselga J., Rosen N., Chandarlapaty S. Acquired CDK6 amplification promotes breast cancer resistance to CDK4/6 inhibitors and loss of ER signaling and dependence. Oncogene. 2017;36:2255–2264. doi: 10.1038/onc.2016.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lypova N., Lanceta L., Gibson A., Vega S., Garza-Morales R., McMasters K.M., Chesney J., Gomez-Gutierrez J.G., Imbert-Fernandez Y. Targeting Palbociclib-Resistant Estrogen Receptor-Positive Breast Cancer Cells via Oncolytic Virotherapy. Cancers (Basel) 2019;11:684. doi: 10.3390/cancers11050684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Condorelli R., Spring L., O’Shaughnessy J., Lacroix L., Bailleux C., Scott V., Dubois J., Nagy R.J., Lanman R.B., Iafrate A.J., et al. Polyclonal RB1 mutations and acquired resistance to CDK 4/6 inhibitors in patients with metastatic breast cancer. Ann. Oncol. 2018;29:640–645. doi: 10.1093/annonc/mdx784. [DOI] [PubMed] [Google Scholar]
- 8.O’Leary B., Hrebien S., Morden J.P., Beaney M., Fribbens C., Huang X., Liu Y., Bartlett C.H., Koehler M., Cristofanilli M., et al. Early circulating tumor DNA dynamics and clonal selection with palbociclib and fulvestrant for breast cancer. Nat. Commun. 2018;9:896. doi: 10.1038/s41467-018-03215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Leary B., Cutts R.J., Liu Y., Hrebien S., Huang X., Fenwick K., Andre F., Loibl S., Loi S., Garcia-Murillas I., et al. The Genetic Landscape and Clonal Evolution of Breast Cancer Resistance to Palbociclib plus Fulvestrant in the PALOMA-3 Trial. Cancer Discov. 2018;8:1390–1403. doi: 10.1158/2159-8290.CD-18-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Formisano L., Lu Y., Servetto A., Hanker A.B., Jansen V.M., Bauer J.A., Sudhan D.R., Guerrero-Zotano A.L., Croessmann S., Guo Y., et al. Aberrant FGFR signaling mediates resistance to CDK4/6 inhibitors in ER+ breast cancer. Nat. Commun. 2019;10:1373. doi: 10.1038/s41467-019-09068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jansen V.M., Bhola N.E., Bauer J.A., Formisano L., Lee K.M., Hutchinson K.E., Witkiewicz A.K., Moore P.D., Estrada M.V., Sanchez V., et al. Kinome-Wide RNA Interference Screen Reveals a Role for PDK1 in Acquired Resistance to CDK4/6 Inhibition in ER-Positive Breast Cancer. Cancer Res. 2017;77:2488–2499. doi: 10.1158/0008-5472.CAN-16-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gong X., Du J., Parsons S.H., Merzoug F.F., Webster Y., Iversen P.W., Chio L.C., Van Horn R.D., Lin X., Blosser W., et al. Aurora A Kinase Inhibition Is Synthetic Lethal with Loss of the RB1 Tumor Suppressor Gene. Cancer Discov. 2019;9:248–263. doi: 10.1158/2159-8290.CD-18-0469. [DOI] [PubMed] [Google Scholar]
- 13.Kettner N.M., Vijayaraghavan S., Durak M.G., Bui T., Kohansal M., Ha M.J., Liu B., Rao X., Wang J., Yi M., et al. Combined Inhibition of STAT3 and DNA Repair in Palbociclib-Resistant ER-Positive Breast Cancer. Clin. Cancer Res. 2019;25:3996–4013. doi: 10.1158/1078-0432.CCR-18-3274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Leeuw R., McNair C., Schiewer M.J., Neupane N.P., Brand L.J., Augello M.A., Li Z., Cheng L.C., Yoshida A., Courtney S.M., et al. MAPK Reliance via Acquired CDK4/6 Inhibitor Resistance in Cancer. Clin. Cancer Res. 2018;24:4201–4214. doi: 10.1158/1078-0432.CCR-18-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Illumina I. BaseSpace User Guide. Ilumina; San Diego, CA, USA: 2014. pp. 1–98. Part # 15044182 Rev. E. [Google Scholar]
- 16.Flight R.M., Harrison B.J., Mohammad F., Bunge M.B., Moon L.D., Petruska J.C., Rouchka E.C. categoryCompare, an analytical tool based on feature annotations. Front. Genet. 2014;5:98. doi: 10.3389/fgene.2014.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kabeya Y., Mizushima N., Ueno T., Yamamoto A., Kirisako T., Noda T., Kominami E., Ohsumi Y., Yoshimori T. LC3, a mammalian homologue of yeast Apg8p, is localized in autophagosome membranes after processing. EMBO J. 2000;19:5720–5728. doi: 10.1093/emboj/19.21.5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shui W., Sheu L., Liu J., Smart B., Petzold C.J., Hsieh T.Y., Pitcher A., Keasling J.D., Bertozzi C.R. Membrane proteomics of phagosomes suggests a connection to autophagy. Proc. Natl. Acad. Sci. USA. 2008;105:16952–16957. doi: 10.1073/pnas.0809218105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vijayaraghavan S., Karakas C., Doostan I., Chen X., Bui T., Yi M., Raghavendra A.S., Zhao Y., Bashour S.I., Ibrahim N.K., et al. CDK4/6 and autophagy inhibitors synergistically induce senescence in Rb positive cytoplasmic cyclin E negative cancers. Nat. Commun. 2017;8:15916. doi: 10.1038/ncomms15916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chittaranjan S., Bortnik S., Dragowska W.H., Xu J., Abeysundara N., Leung A., Go N.E., DeVorkin L., Weppler S.A., Gelmon K., et al. Autophagy inhibition augments the anticancer effects of epirubicin treatment in anthracycline-sensitive and -resistant triple-negative breast cancer. Clin. Cancer Res. 2014;20:3159–3173. doi: 10.1158/1078-0432.CCR-13-2060. [DOI] [PubMed] [Google Scholar]
- 21.Chen S., Jiang Y.Z., Huang L., Zhou R.J., Yu K.D., Liu Y., Shao Z.M. The residual tumor autophagy marker LC3B serves as a prognostic marker in local advanced breast cancer after neoadjuvant chemotherapy. Clin. Cancer Res. 2013;19:6853–6862. doi: 10.1158/1078-0432.CCR-13-1617. [DOI] [PubMed] [Google Scholar]
- 22.Lefort S., Joffre C., Kieffer Y., Givel A.M., Bourachot B., Zago G., Bieche I., Dubois T., Meseure D., Vincent-Salomon A., et al. Inhibition of autophagy as a new means of improving chemotherapy efficiency in high-LC3B triple-negative breast cancers. Autophagy. 2014;10:2122–2142. doi: 10.4161/15548627.2014.981788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H., Nicolay B.N., Chick J.M., Gao X., Geng Y., Ren H., Gao H., Yang G., Williams J.A., Suski J.M., et al. The metabolic function of cyclin D3-CDK6 kinase in cancer cell survival. Nature. 2017;546:426–430. doi: 10.1038/nature22797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franco J., Balaji U., Freinkman E., Witkiewicz A.K., Knudsen E.S. Metabolic Reprogramming of Pancreatic Cancer Mediated by CDK4/6 Inhibition Elicits Unique Vulnerabilities. Cell Rep. 2016;14:979–990. doi: 10.1016/j.celrep.2015.12.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rozeboom B., Dey N., De P. ER+ metastatic breast cancer: Past, present, and a prescription for an apoptosis-targeted future. Am. J. Cancer Res. 2019;9:2821–2831. [PMC free article] [PubMed] [Google Scholar]
- 26.McCartney A., Migliaccio I., Bonechi M., Biagioni C., Romagnoli D., De Luca F., Galardi F., Risi E., De Santo I., Benelli M., et al. Mechanisms of Resistance to CDK4/6 Inhibitors: Potential Implications and Biomarkers for Clinical Practice. Front. Oncol. 2019;9:666. doi: 10.3389/fonc.2019.00666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fry D.W., Harvey P.J., Keller P.R., Elliott W.L., Meade M., Trachet E., Albassam M., Zheng X., Leopold W.R., Pryer N.K., et al. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol. Cancer Ther. 2004;3:1427–1438. [PubMed] [Google Scholar]
- 28.Finn R.S., Dering J., Conklin D., Kalous O., Cohen D.J., Desai A.J., Ginther C., Atefi M., Chen I., Fowst C., et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res. 2009;11:R77. doi: 10.1186/bcr2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Verde G., De Llobet L.I., Wright R.H.G., Quilez J., Peiro S., Le Dily F., Beato M. Unliganded Progesterone Receptor Governs Estrogen Receptor Gene Expression by Regulating DNA Methylation in Breast Cancer Cells. Cancers (Basel) 2018;10:371. doi: 10.3390/cancers10100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barr F.A., Sillje H.H., Nigg E.A. Polo-like kinases and the orchestration of cell division. Nat. Rev. Mol. Cell Biol. 2004;5:429–440. doi: 10.1038/nrm1401. [DOI] [PubMed] [Google Scholar]
- 31.Song B., Liu X.S., Liu X. Polo-like kinase 1 (Plk1): An Unexpected Player in DNA Replication. Cell Div. 2012;7:3. doi: 10.1186/1747-1028-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeong S.B., Im J.H., Yoon J.H., Bui Q.T., Lim S.C., Song J.M., Shim Y., Yun J., Hong J., Kang K.W. Essential Role of Polo-like Kinase 1 (Plk1) Oncogene in Tumor Growth and Metastasis of Tamoxifen-Resistant Breast Cancer. Mol. Cancer Ther. 2018;17:825–837. doi: 10.1158/1535-7163.MCT-17-0545. [DOI] [PubMed] [Google Scholar]
- 33.Shafer D., Grant S. Update on rational targeted therapy in AML. Blood Rev. 2016;30:275–283. doi: 10.1016/j.blre.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rudolph D., Steegmaier M., Hoffmann M., Grauert M., Baum A., Quant J., Haslinger C., Garin-Chesa P., Adolf G.R. BI 6727, a Polo-like kinase inhibitor with improved pharmacokinetic profile and broad antitumor activity. Clin. Cancer Res. 2009;15:3094–3102. doi: 10.1158/1078-0432.CCR-08-2445. [DOI] [PubMed] [Google Scholar]
- 35.Afratis N., Gialeli C., Nikitovic D., Tsegenidis T., Karousou E., Theocharis A.D., Pavao M.S., Tzanakakis G.N., Karamanos N.K. Glycosaminoglycans: Key players in cancer cell biology and treatment. FEBS J. 2012;279:1177–1197. doi: 10.1111/j.1742-4658.2012.08529.x. [DOI] [PubMed] [Google Scholar]
- 36.Nikitovic D., Kouvidi K., Voudouri K., Berdiaki A., Karousou E., Passi A., Tzanakakis G.N. The motile breast cancer phenotype roles of proteoglycans/glycosaminoglycans. Biomed. Res. Int. 2014;2014:124321. doi: 10.1155/2014/124321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kasamatsu A., Uzawa K., Minakawa Y., Ishige S., Kasama H., Endo-Sakamoto Y., Ogawara K., Shiiba M., Takiguchi Y., Tanzawa H. Decorin in human oral cancer: A promising predictive biomarker of S-1 neoadjuvant chemosensitivity. Biochem. Biophys. Res. Commun. 2015;457:71–76. doi: 10.1016/j.bbrc.2014.12.093. [DOI] [PubMed] [Google Scholar]
- 38.Pope W.B., Mirsadraei L., Lai A., Eskin A., Qiao J., Kim H.J., Ellingson B., Nghiemphu P.L., Kharbanda S., Soriano R.H., et al. Differential gene expression in glioblastoma defined by ADC histogram analysis: Relationship to extracellular matrix molecules and survival. AJNR Am. J. Neuroradiol. 2012;33:1059–1064. doi: 10.3174/ajnr.A2917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang Z.X., Lu C.Y., Yang Y.L., Dou K.F., Tao K.S. Lumican expression in pancreatic ductal adenocarcinoma. Hepatogastroenterology. 2013;60:349–353. doi: 10.5754/hge12642. [DOI] [PubMed] [Google Scholar]
- 40.Nikitovic D., Chalkiadaki G., Berdiaki A., Aggelidakis J., Katonis P., Karamanos N.K., Tzanakakis G.N. Lumican regulates osteosarcoma cell adhesion by modulating TGFbeta2 activity. Int. J. Biochem. Cell Biol. 2011;43:928–935. doi: 10.1016/j.biocel.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 41.Yamano Y., Uzawa K., Saito K., Nakashima D., Kasamatsu A., Koike H., Kouzu Y., Shinozuka K., Nakatani K., Negoro K., et al. Identification of cisplatin-resistance related genes in head and neck squamous cell carcinoma. Int. J. Cancer. 2010;126:437–449. doi: 10.1002/ijc.24704. [DOI] [PubMed] [Google Scholar]
- 42.Kwon W.S., Kim T.S., Nahm C.H., Moon Y., Kim J.J. Aberrant cystatin-C expression in blood from patients with breast cancer is a suitable marker for monitoring tumor burden. Oncol. Lett. 2018;16:5583–5590. doi: 10.3892/ol.2018.9380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Decock J., Obermajer N., Vozelj S., Hendrickx W., Paridaens R., Kos J. Cathepsin B, cathepsin H, cathepsin X and cystatin C in sera of patients with early-stage and inflammatory breast cancer. Int. J. Biol. Markers. 2008;23:161–168. doi: 10.1177/172460080802300305. [DOI] [PubMed] [Google Scholar]
- 44.Moyano J.V., Evans J.R., Chen F., Lu M., Werner M.E., Yehiely F., Diaz L.K., Turbin D., Karaca G., Wiley E., et al. AlphaB-crystallin is a novel oncoprotein that predicts poor clinical outcome in breast cancer. J. Clin. Investig. 2006;116:261–270. doi: 10.1172/JCI25888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chelouche-Lev D., Kluger H.M., Berger A.J., Rimm D.L., Price J.E. alphaB-crystallin as a marker of lymph node involvement in breast carcinoma. Cancer. 2004;100:2543–2548. doi: 10.1002/cncr.20304. [DOI] [PubMed] [Google Scholar]
- 46.Ivanov O., Chen F., Wiley E.L., Keswani A., Diaz L.K., Memmel H.C., Rademaker A., Gradishar W.J., Morrow M., Khan S.A., et al. alphaB-crystallin is a novel predictor of resistance to neoadjuvant chemotherapy in breast cancer. Breast Cancer Res. Treat. 2008;111:411–417. doi: 10.1007/s10549-007-9796-0. [DOI] [PubMed] [Google Scholar]
- 47.Zhang P., Tang W.M., Zhang H., Li Y.Q., Peng Y., Wang J., Liu G.N., Huang X.T., Zhao J.J., Li G., et al. MiR-646 inhibited cell proliferation and EMT-induced metastasis by targeting FOXK1 in gastric cancer. Br. J. Cancer. 2017;117:525–534. doi: 10.1038/bjc.2017.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xue M., Li G., Fang X., Wang L., Jin Y., Zhou Q. hsa_circ_0081143 promotes cisplatin resistance in gastric cancer by targeting miR-646/CDK6 pathway. Cancer Cell Int. 2019;19:25. doi: 10.1186/s12935-019-0737-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mustafa M., Lee J.Y., Kim M.H. CTCF negatively regulates HOXA10 expression in breast cancer cells. Biochem. Biophys. Res. Commun. 2015;467:828–834. doi: 10.1016/j.bbrc.2015.10.058. [DOI] [PubMed] [Google Scholar]
- 50.Ogrodzinski M.P., Bernard J.J., Lunt S.Y. Deciphering metabolic rewiring in breast cancer subtypes. Transl. Res. 2017;189:105–122. doi: 10.1016/j.trsl.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 51.Lorito N., Bacci M., Smiriglia A., Mannelli M., Parri M., Comito G., Ippolito L., Giannoni E., Bonechi M., Benelli M., et al. Glucose Metabolic Reprogramming of ER Breast Cancer in Acquired Resistance to the CDK4/6 Inhibitor Palbociclib+ Cells. 2020;9:668. doi: 10.3390/cells9030668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCartney A., Bonechi M., De Luca F., Biagioni C., Curigliano G., Moretti E., Minisini A.M., Bergqvist M., Benelli M., Migliaccio I., et al. Plasma thymidine kinase activity as a biomarker in patients with luminal metastatic breast cancer treated with palbociclib within the TREnd trial. Clin. Cancer Res. 2020 doi: 10.1158/1078-0432.CCR-19-3271. [DOI] [PubMed] [Google Scholar]
- 53.Romain S., Spyratos F., Descotes F., Daver A., Rostaing-Puissant B., Bougnoux P., Colonna M., Bolla M., Martin P.M. Prognostic of DNA-synthesizing enzyme activities (thymidine kinase and thymidylate synthase) in 908 T1-T2, N0-N1, M0 breast cancers: A retrospective multicenter study. Int. J. Cancer. 2000;87:860–868. doi: 10.1002/1097-0215(20000915)87:6<860::AID-IJC16>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 54.Broet P., Romain S., Daver A., Ricolleau G., Quillien V., Rallet A., Asselain B., Martin P.M., Spyratos F. Thymidine kinase as a proliferative marker: Clinical relevance in 1,692 primary breast cancer patients. J. Clin. Oncol. 2001;19:2778–2787. doi: 10.1200/JCO.2001.19.11.2778. [DOI] [PubMed] [Google Scholar]
- 55.Ma C.X., Gao F., Luo J., Northfelt D.W., Goetz M., Forero A., Hoog J., Naughton M., Ademuyiwa F., Suresh R., et al. NeoPalAna: Neoadjuvant Palbociclib, a Cyclin-Dependent Kinase 4/6 Inhibitor, and Anastrozole for Clinical Stage 2 or 3 Estrogen Receptor-Positive Breast Cancer. Clin. Cancer Res. 2017;23:4055–4065. doi: 10.1158/1078-0432.CCR-16-3206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.