Abstract
The outcome of patients with hepatocellular carcinoma (HCC) is still poor. Decorin is a small leucine-rich proteoglycan, which exerts antiproliferative and antiangiogenic properties in vitro. We aimed to investigate the associations of decorin with physical function and prognosis in patients with HCC. We enrolled 65 patients with HCC treated with transcatheter arterial chemoembolization (median age, 75 years; female/male, 25/40). Serum decorin levels were measured using enzyme-linked immunosorbent assays; patients were classified into the High or Low decorin groups by median levels. Associations of decorin with physical function and prognosis were evaluated by multivariate correlation and Cox regression analyses, respectively. Age and skeletal muscle indices were not significantly different between the High and Low decorin groups. In the High decorin group, the 6-min walking distance was significantly longer than the Low decorin group and was significantly correlated with serum decorin levels (r = 0.2927, p = 0.0353). In multivariate analysis, the High decorin group was independently associated with overall survival (hazard ratio 2.808, 95% confidence interval 1.016–8.018, p = 0.0498). In the High decorin group, overall survival rate was significantly higher than in the Low decorin group (median 732 days vs. 463 days, p = 0.010). In conclusion, decorin may be associated with physical function and prognosis in patients with HCC.
Keywords: hepatoma, myokine, decorin, walking distance, survival
1. Introduction
Hepatocellular carcinoma (HCC) is a common cancer and the fourth leading cause of death due to cancer worldwide [1]. The incidence of HCC is predicted to continuously increase in both sexes and all age groups, since risk factors for HCC such as obesity, non-alcoholic steatohepatitis, and type 2 diabetes mellitus have become more prevalent worldwide [2]. In addition, the mortality rate of HCC has increased since 2000 [3], although there has been remarkable progresses in treatment for HCC, including the use of tyrosine kinase inhibitors [4]. The age-adjusted incidence and mortality rates of HCC are reported to be the highest in Eastern Asia [2]. The average 5-year survival rate is less than 15% in patients with HCC [5]. Thus, the prognosis of patients with HCC remains poor.
Skeletal muscle mass is known to be associated with the prognosis of patients with HCC [6]. Muscle atrophy is an independent factor associated with poor prognosis in patients with HCC treated with surgical resection and radiofrequency ablation [7]. Muscle atrophy is also a prognostic factor in patients with HCC treated with transarterial chemoembolization (TACE) and sorafenib [8,9]. In addition, muscle atrophy is associated with treatment tolerability and additional or subsequent therapies in patients with HCC treated with sorafenib [10]. In contrast, physical activity is associated with a reduced risk of HCC [11]. Moreover, exercise is reported to improve the prognosis of patients with HCC, regardless of changes in skeletal muscle mass [12].
Skeletal muscle is known as an endocrine organ [13]. By muscle contraction, myocytes release small peptides and cytokines, called myokines, and regulate muscle mass [13]. Myostatin is a myokine, which suppresses skeletal muscle growth and causes muscle atrophy [14]. Meanwhile, decorin is an exercise-induced myokine that suppresses muscle atrophy via inhibition of myostatin [15]. We previously reported that serum decorin levels are positively correlated with skeletal muscle mass in patients with HCC [16]. Decorin is also reported to interact with transforming growth factor-β and receptors of tyrosine kinase such as epidermal and insulin-like growth factors [17], leading to suppression of proliferation of various tumor cell lines, including HCC cell lines [18,19,20]. In addition, decorin is known to be expressed in various tissues including intestinal tissue, cardiac tissue, and adipose tissue and is known to regulate autophagy, inflammation, and glucose homeostasis [21,22,23,24]. Thus, accumulated evidence from basic studies suggests that decorin has an impact on the prognosis of patients with HCC. However, there has been no clinical study investigating the prognostic impact of decorin in patients with HCC.
The aim of this study was to investigate the association of serum decorin levels with physical function and prognosis in patients with HCC.
2. Materials and Methods
2.1. Study Design
This was a retrospective study to investigate the impact of serum decorin levels on the physical function and prognosis of patients with HCC.
2.2. Ethics
The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the institutional review board of Kurume University. We employed an opt-out approach to obtain informed consent from patients.
2.3. Subjects
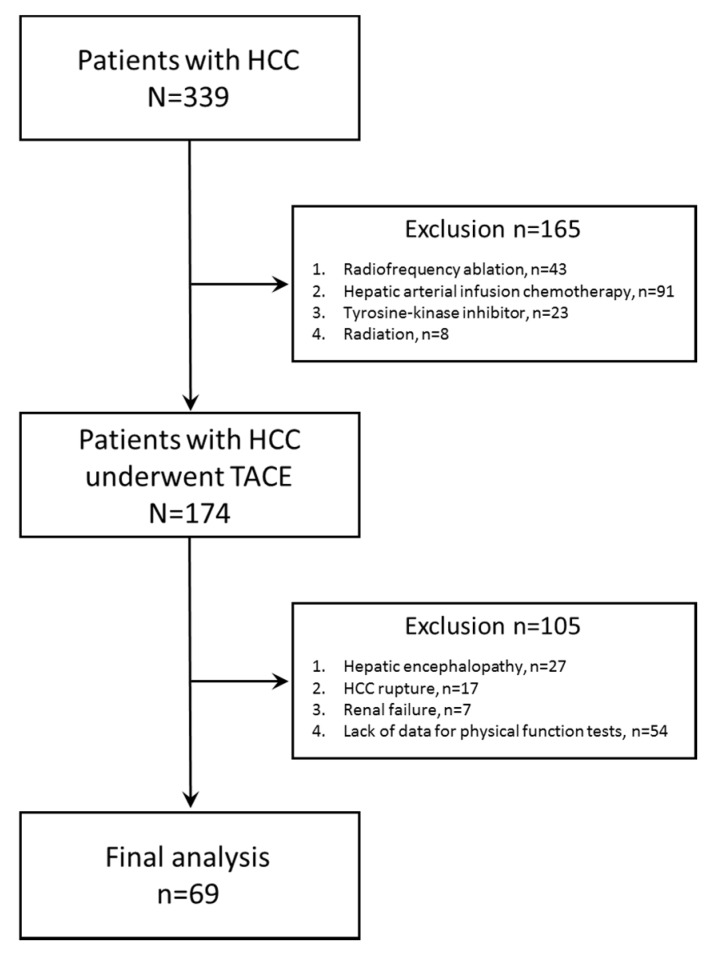
We registered 339 consecutive patients with HCC between November 2014 and March 2018. Of these patients, 165 patients were excluded because of radiofrequency ablation (n = 43), hepatic arterial infusion chemotherapy (n = 91), tyrosine-kinase inhibitor (n = 23), or radiation (n = 8), and the remaining 174 patients with HCC who underwent TACE were selected. Of the 174 patients with HCC who underwent TACE, 105 patients were excluded because of hepatic encephalopathy (n = 27), HCC rupture (n = 17), renal failure (n = 7), or lack of data for physical function tests (n = 54). Finally, a total of 69 patients with HCC were analyzed in this study (Figure 1). We classified all patients into the High or Low decorin group per the median decorin level.
Figure 1.
A flow diagram of analyzed subjects.
2.4. Diagnosis, Barcelona Clinic Liver Cancer (BCLC) Staging, and Treatment of HCC
HCC was diagnosed and treated according to the guidelines for HCC of the Japan Society of Hepatology [25]. The clinical stage of HCC was evaluated using the BCLC staging system [26].
2.5. Measurement of Skeletal Muscle Index (SMI) and Visceral Fat Area
The SMI was evaluated using computed tomography (CT) images obtained at the diagnosis of HCC as previously described [27,28]. The skeletal muscle mass was measured by manual tracings on CT images, and their sum was calculated using ImageJ Version 1.50 software (National Institutes of Health, Bethesda, MD, USA) [29]. The skeletal muscle mass was evaluated by the SMI.
2.6. Measurement of Physical Function
Grip strength and the 6-min walking distance were evaluated by qualified physical therapists. Handgrip was measured on the non-dominant hand using a dynamometer (TKK5401; Takei Scientific Instruments Co., Ltd., Niigata, Japan) [6]. The 6-minute walking distance was measured by evaluating the total ambulated distance [30].
2.7. Diagnosis of Sarcopenia
The diagnosis of sarcopenia was based on the Japan Society of Hepatology diagnostic criteria for sarcopenia in patients with liver disease [6]. Patients who showed both a decrease in grip strength (the cut-off value is 26 kg for men and 18 kg for women) and a decrease in skeletal muscle mass (the cut-off value of SMI is 42 cm2/m2 for men and 38 cm2/m2 for women) were diagnosed with sarcopenia. The other patients were classified as non-sarcopenia [6].
2.8. Biochemical Tests
Blood samples were obtained at the baseline in the early morning after an overnight fast. The blood biochemical tests performed were for serum levels of alpha-fetoprotein, des-γ-carboxy prothrombin, liver function tests, renal function tests, total cholesterol, creatine kinase, and hemoglobin A1c. We also measured the complete blood cell count.
2.9. Measurement of Serum Levels of Myostatin, FGF-21 and Decorin
Serum levels of myostatin, FGF-21, and decorin were measured using a Myostatin Quantikine enzyme-linked immunosorbent assay (ELISA) Kit (R&D Systems, Inc., Minneapolis, MN, USA), Human FGF-21 ELISA Kit (BioVendor—Laboratorni medicina a.s., Brno, Czech Republic), and Human Decorin ELISA Kit (Abcam plc., Cambridge, UK) according to the manufacturers’ instructions, respectively.
2.10. Follow-Up and Definition of Survival Term
After treatment with TACE, patients were followed up until death or the study censor date through routine physical examinations, biochemical tests, and abdominal imaging including ultrasonography, CT, or magnetic resonance imaging according to the HCC guidelines of the Japan Society of Hepatology [25]. The median observational period was 617 days (range, 52–2068 days). The survival term was defined as the period from the diagnosis of HCC to death or the study censor date.
2.11. Statistical Analysis
Data are expressed as the median (interquartile range), range, or number. The differences between the High and Low decorin groups were analyzed using Wilcoxon rank sum tests. Factors correlated with serum decorin levels were evaluated by pairwise correlations [31]. In addition, independent factors associated with survival were analyzed using Cox regression analysis, as previously described [27]. The overall survival in the High and Low decorin groups was estimated using the Kaplan–Meier method, and differences in survival between the groups were analyzed using the log-rank test. All the statistical analyses were performed using JMP Pro® 14 (SAS Institute Inc., Cary, NC, USA). Values of p < 0.05 were considered to indicate statistically significant differences.
3. Results
3.1. Patient Characteristics
The patient characteristics are summarized in Table 1. There was no significant difference in age and body mass index. The prevalence of men was significantly higher in the High decorin group than that in the Low decorin group. There was no significant difference in the hospitalization period between the two groups.
Table 1.
Patients’ characteristics.
| All Subjects | High Decorin | Low Decorin | |||||
|---|---|---|---|---|---|---|---|
| Median (IQR) | Range (min–max) |
Median (IQR) | Range (min–max) |
Median (IQR) | Range (min–max) |
p | |
| Number (n) | 65 | N/A | 33 | N/A | 32 | N/A | N/A |
| Age (years) | 75 (71–80) | 60–90 | 76 (72–80) | 60–89 | 75 (71–80) | 63–90 | 0.9528 |
| Sex (women/men) | 38.5%/61.5% (25/40) |
N/A | 54.5%/45.5% (18/15) | N/A | 21.9%/78.1% (7/25) | N/A | 0.0068 |
| Body mass index (kg/m2) | 23.9 (21.2–26.0) |
16.7–37.8 | 23.0 (21.5–26.3) |
19.6–30.3 | 24.1 (20.5–25.8) |
16.7–37.8 | 0.6227 |
| Hospitalization period (days) | 14 (11–21) | 7–55 | 13 (11.5–17.5) | 7–55 | 17 (11–21) | 7–34 | 0.3076 |
| Grip strength (kg) | 24.2 (20.3–31.3) |
13.3–42.8 | 24.1 (19.25–30.63) |
13.3–42.8 | 25.0 (21.5–32.1) |
14.9–39 | 0.8045 |
| Skeletal muscle index (cm2/m2) | 29.69 (23.94–35.20) | 11.85–51.18 | 28.50 (23.21–34.22) |
11.85–41.79 | 31.53 (24.33–36.82) |
12.45–51.18 | 0.3758 |
| Sarcopenia (Presence/Absence) | 18.5%/81.5% (12/53) |
N/A | 6.1%/93.9% (2/31) |
N/A | 31.3%/68.7% (10/22) |
N/A | 0.0089 |
| Visceral fat area (cm2) | 61.7 (39.8–84.6) | 4.4–240.8 | 59.2 (39.8–78.1) | 24.2–240.8 | 61.9 (36.5–95.9) | 4.4–197.8 | 0.7578 |
| Serum creatine kinase (U/L) | 95 (70.5–132.5) |
17–374 | 99 (77–133) |
44–246 | 90.5 (63.75–129.5) |
17–374 | 0.3558 |
| 6-minute walking distance (m) | 379 (302–420) |
26–621 | 391 (365–433) |
228–621 | 334 (255–407) |
26–501 | 0.0093 |
| Decorin (pg/mL) | 17,322 (13,499–21,866) |
7400–32,102 | 21,799 (18,990–27,033) |
17,322–32,102 | 13,499 (11,939–14,726) |
7400–16,838 | <0.0001 |
| Myostatin (pg/mL) | 1699 (1180–3658) |
245–7788 | 3056 (1313–4610) |
501–6350 | 1500 (1154–3214) |
246–7788 | 0.0426 |
| FGF-21 (pg/mL) | 160 (116–344) | 13–2150 | 174 (140–340) | 39–2150 | 156 (96–357) | 13–1328 | 0.4197 |
| BCLC stage (A/B) | 10.8%/89.2% (7/58) | N/A | 15.2%/84.8%(5/28) | N/A | 6.2%/93.8%(2/30) | N/A | 0.2471 |
| AFP (ng/mL) | 32.75 (6.83–275.18) |
1.4–67,036 | 20 (8.25–72.27) |
3.9–1594 | 93 (5.5–1613) |
1.4–67,036 | 0.2318 |
| DCP (mAU/mL) | 76 (28–888.5) | 9–30,844 | 36 (24–211.5) | 12–17,353 | 144 (43–6753) | 9–30,844 | 0.0253 |
| Child–Pugh class (A/B) | 69.2%/30.8% (45/20) |
N/A | 75.8%/24.2% (25/8) |
N/A | 62.5%/37.5% (20/12) |
N/A | 0.2469 |
| BCAA supplementation (With/Without) | 52.3%/47.7% (34/31) |
N/A | 51.5%/48.5% (17/16) |
N/A | 53.1%/46.9% (17/15) |
N/A | 0.8966 |
| AST (IU/L) | 43 (32–55.5) | 19–158 | 45 (40–65.5) | 23–158 | 34 (26–48) | 19–99 | 0.0009 |
| ALT (IU/L) | 28 (21–37.5) | 7–186 | 32 (24.5–41) | 20–186 | 23 (17.5–32.5) | 7–87 | 0.0031 |
| ALP (IU/L) | 351 (291–479) | 180–854 | 356 (309.5–541.5) | 200–854 | 325 (275.75–455) | 180–659 | 0.2299 |
| GGT (IU/L) | 44 (26–73.5) | 9–551 | 45 (26.5–79.5) | 15–551 | 42 (26–66.5) | 9–252 | 0.6088 |
| Total protein (g/dL) | 7.28 (6.72–7.78) | 5.94–8.89 | 7.36 (6.62–7.81) | 5.94–8.15 | 7.28 (6.82–7.62) | 6.04–8.89 | 0.9477 |
| Albumin (g/dL) | 3.5 (3.1–3.7) | 2.5–4.3 | 3.4 (3.1–3.7) | 2.5–4.3 | 3.5 (3.0–3.8) | 2.8–4.2 | 1.0000 |
| Total bilirubin (mg/dL) | 0.9 (0.6–1.3) | 0.3–2.8 | 0.9 (0.6–1.3) | 0.4–2.8 | 0.9 (0.6–1.2) | 0.3–1.6 | 0.5996 |
| Prothrombin activity (%) | 80 (68–88) | 38–117 | 81 (65.5–90) | 42–117 | 79 (69–85.5) | 38–108 | 0.6365 |
| Blood urea nitrogen (mg/dL) | 17 (14–19.6) | 5.9–47.6 | 14.9 (13–18.9) | 5.9–28.1 | 17.45 (15–20.18) | 11.5–47.6 | 0.0253 |
| Creatinine (mg/dL) | 0.74 (0.61–0.92) | 0.43–1.91 | 0.66 (0.55–0.77) | 0.43–1.52 | 0.81 (0.66–1.03) | 0.56–1.91 | 0.0013 |
| eGFR (mL/min/1.73 m2) | 73.2 (54.3–84.85) | 27.3–121.3 | 78.6 (62.15–89.95) | 34.3–121.3 | 65.7 (52.63–75.8) | 27.3–102.4 | 0.0107 |
| Total cholesterol (mg/dL) | 144 (126–162) | 79–233 | 138 (121–156) | 84–197 | 147 (128–163) | 79–233 | 0.3154 |
| Triglyceride (mg/dL) | 82 (70–108) | 28–249 | 75 (64–94) | 28–249 | 91 (78–130) | 54–179 | 0.0237 |
| HbA1c (%) | 5.8 (5.5–6.4) | 4.3–13.4 | 5.7 (5.25–6.1) | 4.3–8.3 | 6.1 (5.7–6.8) | 4.7–13.4 | 0.0268 |
| Red blood cell count (×104/µL) | 389 (355–420) | 249–615 | 385 (356–416) | 310–455 | 393 (347–442) | 249–615 | 0.7528 |
| Hemoglobin (g/dL) | 11.9 (10.4–12.75) | 7.3–15.4 | 11.9 (10.6–12.8) | 7.3–15.4 | 11.9 (9.8–12.7) | 7.3–14.9 | 0.7083 |
| White blood cell count (/µL) | 3800 (3100–5050) |
1800–7900 | 3700 (3050–5560) |
1900–6600 | 4150 (3125–5525) |
1800–7900 | 0.2270 |
| Platelet count (×103/mm3) | 10.9 (8.35–15.1) | 3.2–31.8 | 9.4 (7.8–13.0) | 3.2–22.6 | 11.8 (8.6–16.1) | 4.0–31.8 | 0.0881 |
Note: Data are expressed as median (interquartile range (IQR)), range, or number. Abbreviations: AFP, alpha-fetoprotein; ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BCAA, branched-chain amino acid; BCLC, Barcelona Clinic Liver Cancer; DCP, des-γ-carboxy prothrombin; eGFR, estimated glomerular filtration rate; FGF-21, fibroblast growth factor-21; GGT, gamma-glutamyl transpeptidase; HbA1c, hemoglobin A1c; N/A, not applicable
In the High decorin group, the prevalence of sarcopenia was significantly lower than that in the Low decorin group. Although no significant differences were noted in the SMI and serum creatine kinase level between the two groups, the 6-min walking distance in the High decorin group was significantly longer than that in the Low decorin group (Table 1).
Although there was no significant difference in the serum fibroblast growth factor (FGF)-21 level between the two groups, the serum level of myostatin was significantly higher in the High decorin group than that in the Low decorin group (Table 1).
There was no significant difference in the BCLC classification between the High and Low decorin groups. No significant difference in the serum alpha-fetoprotein level was also observed between the two groups; however, in the High decorin group, the serum des-γ-carboxy prothrombin level was significantly lower than that in the Low decorin group (Table 1).
There was no significant difference in the prevalence of Child–Pugh class B and use of branched-chain amino acid supplementation between the two groups. Serum levels of aspartate aminotransferase, alanine aminotransferase, and estimated glomerular filtration rate were significantly higher in the High decorin group than those in the Low decorin group. In the High decorin group, serum levels of blood urea nitrogen, creatinine, and triglycerides and the hemoglobin A1c value were significantly lower than those in the Low decorin group (Table 1).
3.2. Multivariate Correlation Analysis Between Serum Decorin Levels and Each Variable
No significant correlation was seen between serum decorin levels and age, body mass index, grip strength, SMI, levels of alpha-fetoprotein, albumin, total bilirubin, creatine kinase, hemoglobin A1c, and estimated glomerular filtration rate. Serum decorin levels showed a significant negative correlation with serum des-γ-carboxy prothrombin levels. Serum decorin levels demonstrated a significant positive correlation between the 6-min walking distance and serum myostatin levels (Table 2).
Table 2.
Multivariate correlation analysis between serum decorin levels and each variable.
| Variable | Correlation Coefficient | p |
|---|---|---|
| Age | −0.0250 | 0.8750 |
| Body mass index | 0.0415 | 0.7942 |
| Grip strength | −0.0532 | 0.7380 |
| Skeletal muscle index | −0.1362 | 0.3898 |
| Visceral fat area | 0.0278 | 0.861 |
| 6-min walking distance | 0.2927 | 0.0353 |
| Creatine kinase | −0.0062 | 0.9690 |
| Myostatin | 0.3200 | 0.0389 |
| FGF-21 | −0.0352 | 0.8249 |
| AFP | −0.2270 | 0.1482 |
| DCP | −0.3476 | 0.0241 |
| AST | 0.2453 | 0.0992 |
| ALT | 0.2734 | 0.0798 |
| ALP | 0.1260 | 0.4266 |
| GGT | 0.0042 | 0.979 |
| Total protein | −0.0197 | 0.9015 |
| Albumin | −0.1754 | 0.2664 |
| Total bilirubin | 0.1054 | 0.5063 |
| Prothrombin activity | 0.1078 | 0.4968 |
| Blood urea nitrogen | −0.1606 | 0.3095 |
| Creatinine | −0.1650 | 0.2965 |
| eGFR | 0.0695 | 0.6617 |
| Total cholesterol | −0.0914 | 0.5650 |
| Triglyceride | −0.0594 | 0.7089 |
| HbA1c | −0.2748 | 0.0782 |
| Red blood cell count | −0.1337 | 0.3984 |
| Hemoglobin | −0.0384 | 0.8091 |
| White blood cell count | −0.233 | 0.1376 |
| Platelet count | −0.2261 | 0.15 |
Abbreviations: FGF-21, fibroblast growth factor-21; AFP, alpha-fetoprotein; DCP, des-γ-carboxy prothrombin; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; GGT, gamma-glutamyl transpeptidase; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c.
3.3. Independent Factors Associated with Survival
We examined independent factors associated with survival and found that high decorin levels were identified as an independent factor of better overall survival. Meanwhile, the BCLC stage and Child–Pugh class were not identified as independent factors associated with overall survival (Table 3).
Table 3.
Multivariate Cox regression analysis for overall survival.
| Factors | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Decorin (High/Low) | 2.808 | 1.016–8.018 | 0.0498 |
| BCLC stage (A/B–C) | 6.720 | 0.707–73.877 | 0.0553 |
| Child–Pugh class (A/B) | 1.436 | 0.461–4.473 | 0.5308 |
Abbreviations: BCLC, Barcelona Clinic Liver Cancer.
3.4. Kaplan–Meier Analysis for Survival
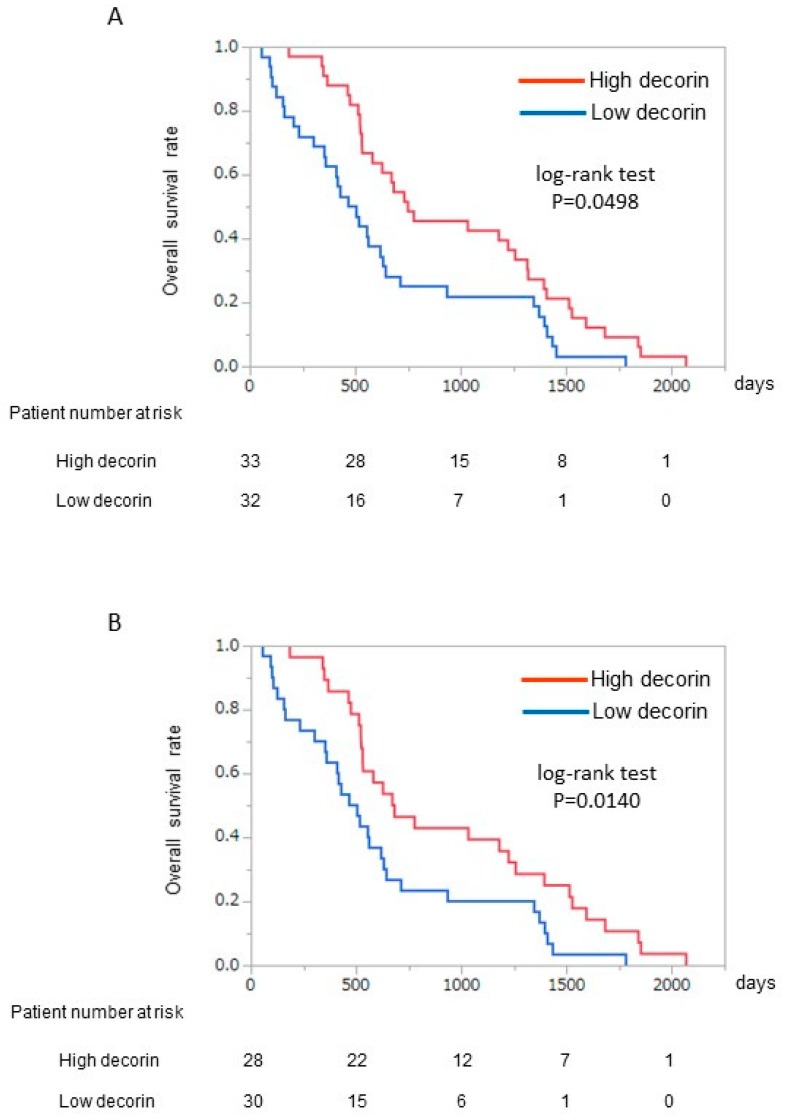
In the High decorin group, the overall survival rate was significantly higher compared to that in the Low decorin group (median 732 days vs. 463 days; log-rank test p = 0.0498) (Figure 2A). In the subgroup analysis of BCLC stage B, the difference in overall survival rates between the High and Low decorin groups became more significant than that in the analysis in all subjects (BCLC stages A and B) (Figure 2B).
Figure 2.
Kaplan–Meier analysis between the High decorin and Low decorin groups. (A) All patients; (B) Patients with BCLC stage B HCC. BCLC, Barcelona Clinic Liver Cancer; HCC, hepatocellular carcinoma.
4. Discussion
In this study, we demonstrated that serum decorin levels were positively correlated with the 6-min walking distance, an index of cardiopulmonary function in patients with HCC. In addition, we found that serum decorin levels were an independent prognostic factor in patients with HCC. Although more research is needed and our data are preliminary in essence, these data suggest that decorin may be associated with physical function and prognosis in patients with HCC.
TACE is a standard treatment for intermediate-stage HCC [26,32]. In this study, we enrolled patients with HCC treated with TACE, and the median survival period was 617 days, which is comparable to that reported previously [26,33]. The prognosis of patients with HCC is dependent on the BCLC stage [26]. However, the BCLC stage was not identified as an independent prognostic factor in this study, and the reason for this remains unclear. However, all enrolled patients with HCC were treated with TACE, and patients with the BCLC stage B accounted for about 90% of the enrolled patients. Therefore, the narrow distribution of the BCLC stage may be a possible explanation.
Although myostatin and FGF-21 are myokines, the levels of these myokines were not identified as independent prognostic factors in patients with HCC. Nishikawa et al. reported that elevated serum myostatin levels are associated with worse survival in patients with liver cirrhosis [34]. Hyperammonemia has been reported to transcriptionally upregulate myostatin through nuclear transport of p65 nuclear factor-ƙB, resulting in sarcopenia and poor prognosis [35]. Meanwhile, patients with hepatic encephalopathy (West Haven criteria grade II–IV) were excluded, and the prevalence of hyperammonemia was thought to be low in this study. Therefore, myostatin may not be identified as a prognostic factor. Deficiency of FGF-21 is reported to promote HCC in mice receiving a long-term obesogenic diet [36]. Long-term administration of FGF-21 prevents chemically induced hepatocarcinogenesis in mice [37]. However, FGF-21 is known to be expressed in several tissues, including those of the liver, fat, and pancreas [38]. Serum FGF-21 levels are affected by various tissues expressing FGF-21, and, therefore, FGF-21 was not identified as an independent prognostic factor in patients with HCC.
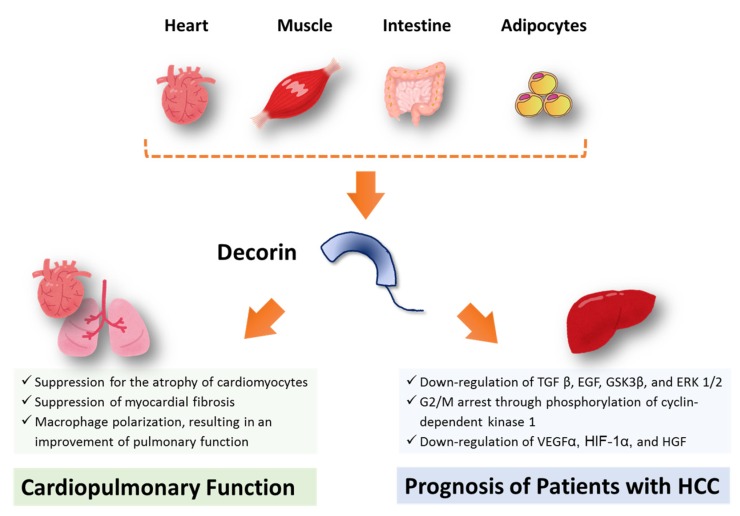
Serum decorin levels were positively correlated with the 6-min walking distance, an index of cardiopulmonary function in patients with HCC. Overexpression of decorin is reported to ameliorate diabetic cardiomyopathy and cardiac function in rats [39]. N-terminal cleavage of decorin confers an inhibitory effect against myostatin, suppressing the atrophy of cardiomyocytes [40]. In fact, serum decorin level was positively correlated with serum myostatin level in this study. One would think that decorin may be up regulated to suppress muscle atrophy in response to an increase in serum myostatin level. In addition, C-terminal truncation of decorin interacts with the connective tissue growth factor, leading to suppression of myocardial fibrosis through down-regulation of cardiac extracellular matrix production [40]. Furthermore, Kwon et al. reported that decorin causes macrophage polarization via cluster of differentiation-44, resulting in an amelioration of pulmonary function in a rat model of hypertoxic lung damage [41]. These previous basic studies, along with our results, may suggest that decorin may be associated with cardiopulmonary function in patients with HCC (Figure 3). However, the correlation between serum decorin level and the 6-min walking distance could not lead to the conclusion that the high decorin level is a cause of high cardiovascular fitness, in such a small number of subjects.
Figure 3.
A scheme for the proposed hypothesis of this study. Decorin is expressed in various tissues including skeletal muscle, heart, intestine, and adipocytes. In this study, it remains unclear where decorin comes from. Decorin may be associated with cardiopulmonary function, because decorin suppresses the atrophy of cardiomyocytes, myocardial fibrosis, and causes macrophage polarization. In addition, decorin may be associated with prognosis of patients with HCC, because decorin downregulates transforming growth factor-β1, epidermal growth factor receptor, glycogen synthase kinase 3β, and extracellular signal-regulated kinase 1/2, G2/M arrest through phosphorylation of cyclin-dependent kinase 1, downregulation of vascular endothelial growth factor A, hypoxia-inducible factor 1-α, and hepatocyte growth factor. Abbreviations: TGF β, transforming growth factor-β1; EGF, epidermal growth factor receptor; GSK3β, glycogen synthase kinase 3β; and ERK, extracellular signal-regulated kinase; VEGF, vascular endothelial growth factor; HIF-1α, hypoxia-inducible factor 1-α; HGF, hepatocyte growth factor.
In this study, we first examined the impact of the serum decorin level in patients with HCC and found that serum decorin levels were identified as an independent prognostic factor in patients with HCC. Moreover, in the stratification analysis according to the BCLC stage, the prognostic impact of decorin was more evident in patients with HCC with the BCLC stage B. Horváth et al. reported that genetic ablation of decorin leads to enhanced hepatocarcinogenesis compared to that in wild-type animals [42]. Meanwhile, recombinant human decorin inhibits the proliferation of HepG2 cells [43,44]. Several mechanisms for decorin-induced inhibition of cell proliferation have been reported. Decorin is reported to reduce the secretion of transforming growth factor-β1 in HCC cell lines [20]. Decorin is also reported to downregulate the phosphorylation of epidermal growth factor receptor, glycogen synthase kinase 3β, and extracellular signal-regulated kinase 1/2 [20]. In addition, decorin suppresses the ATR/Chk1/Wee1 axis, leading to inhibition of the cell cycle in the G2/M phase via phosphorylation of cyclin-dependent kinase 1 [20]. Moreover, decorin is known to decrease the expression of pro-angiogenic factors, vascular endothelial growth factor A, and hypoxia-inducible factor 1-α, resulting in downregulation of the hepatocyte growth factor and epidermal growth factor receptor signaling axes [45]. In fact, the serum decorin level was negatively correlated with the serum des-γ-carboxy prothrombin level, which is a tumor maker for HCC in this study. Thus, decorin may suppress the proliferation of HCC through direct and indirect tumor inhibitory effects and may be associated with prognosis in patients with HCC (Figure 3). However, decorin is known to be expressed not only in skeletal muscle [15], but also in various tissues including intestinal tissue, cardiac tissue, and adipose tissue [21,22,23,24]. Accordingly, it remains unclear where decorin comes from in the present study (Figure 3). In addition, we have to be cautious of the interpretation of our data. Expression of decorin is recently reported to be seen in the tumor cell such as glioblastoma and is negatively associated with the overall survival rate of patients with glioblastoma multiforme [46]. Thus, further research is required to investigate the expression of decorin in HCC tissue and a causal relationship between decorin and prognosis of the patients with HCC.
Limitations of this study are the following: First, this was a retrospective study conducted in a single center. Second, the number of enrolled subjects is very limited to examine independent prognostic factors. Third, we enrolled patients with HCC treated with TACE. It remains unclear if serum decorin levels have a prognostic impact in patients with HCC treated with hepatic resection or tyrosine kinase inhibitors. Fourth, no patient underwent liver transplantation during the observation period, suggesting the selection bias. Thus, a multicenter prospective cohort study should be conducted with various HCC stages and treatments for HCC including liver transplantation.
5. Conclusions
In conclusion, we demonstrated that serum decorin levels were positively correlated with cardiopulmonary function in patients with HCC. In addition, serum decorin levels were an independent prognostic factor in patients with HCC. Although more research is needed and our data are preliminary in essence, the results of this study may suggest that decorin may be associated with physical function and prognosis in patients with HCC.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
Author Contributions: T.K., S.Y. (Sachiyo Yoshio), and R.H. participated in the study conception and design, data acquisition and interpretation, and manuscript drafting. Y.S. participated in data analysis and manuscript drafting. S.K., K.H., D.N., S.Y. (Sakura Yamamura), and T.N. participated in data acquisition and interpretation and manuscript drafting. H.M. and T.T. participated in the study conception and design, interpretation, and critical revision. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Program for Basic and Clinical Research on Hepatitis (AMED) under JP19fk0210045.
Conflicts of Interest
T.K. received lecture fees from MSD K.K., Mitsubishi Tanabe Pharma Corporation and Otsuka Pharmaceutical Co., Ltd. The other authors have no conflicts of interest.
References
- 1.Weinmann A., Koch S., Niederle I.M., Schulze-Bergkamen H., Konig J., Hoppe-Lotichius M., Hansen T., Pitton M.B., Duber C., Otto G., et al. Trends in epidemiology, treatment, and survival of hepatocellular carcinoma patients between 1998 and 2009: An analysis of 1066 cases of a German HCC Registry. J. Clin. Gastroenterol. 2014;48:279–289. doi: 10.1097/MCG.0b013e3182a8a793. [DOI] [PubMed] [Google Scholar]
- 2.Younossi Z.M., Golabi P., de Avila L., Paik J.M., Srishord M., Fukui N., Qiu Y., Burns L., Afendy A., Nader F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J. Hepatol. 2019;71:793–801. doi: 10.1016/j.jhep.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 3.Xu J. Trends in Liver Cancer Mortality among Adults Aged 25 and Over in the United States, 2000–2016. NCHS Data Brief. 2018;314:1–8. [PubMed] [Google Scholar]
- 4.Ikeda K. Recent advances in medical management of hepatocellular carcinoma. Hepatol. Res. 2019;49:14–32. doi: 10.1111/hepr.13259. [DOI] [PubMed] [Google Scholar]
- 5.El-Serag H.B. Hepatocellular carcinoma. N. Engl. J. Med. 2011;365:1118–1127. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- 6.Nishikawa H., Shiraki M., Hiramatsu A., Moriya K., Hino K., Nishiguchi S. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol. Res. 2016;46:951–963. doi: 10.1111/hepr.12774. [DOI] [PubMed] [Google Scholar]
- 7.Hiraoka A., Otsuka Y., Kawasaki H., Izumoto H., Ueki H., Kitahata S., Aibiki T., Okudaira T., Yamago H., Miyamoto Y., et al. Impact of muscle volume and muscle function decline in patients undergoing surgical resection for hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2018;33:1271–1276. doi: 10.1111/jgh.14058. [DOI] [PubMed] [Google Scholar]
- 8.Fujita M., Takahashi A., Hayashi M., Okai K., Abe K., Ohira H. Skeletal muscle volume loss during transarterial chemoembolization predicts poor prognosis in patients with hepatocellular carcinoma. Hepatol. Res. 2019;49:778–786. doi: 10.1111/hepr.13331. [DOI] [PubMed] [Google Scholar]
- 9.Takada H., Kurosaki M., Nakanishi H., Takahashi Y., Itakura J., Tsuchiya K., Yasui Y., Tamaki N., Takaura K., Komiyama Y., et al. Impact of pre-sarcopenia in sorafenib treatment for advanced hepatocellular carcinoma. PLoS ONE. 2018;13:e0198812. doi: 10.1371/journal.pone.0198812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawada K., Saitho Y., Hayashi H., Hasebe T., Nakajima S., Ikuta K., Fujiya M., Okumura T. Skeletal muscle mass is associated with toxicity, treatment tolerability, and additional or subsequent therapies in patients with hepatocellular carcinoma receiving sorafenib treatment. JGH Open. 2019;3:329–337. doi: 10.1002/jgh3.12167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baumeister S.E., Schlesinger S., Aleksandrova K., Jochem C., Jenab M., Gunter M.J., Overvad K., Tjonneland A., Boutron-Ruault M.C., Carbonnel F., et al. Association between physical activity and risk of hepatobiliary cancers: A multinational cohort study. J. Hepatol. 2019;70:885–892. doi: 10.1016/j.jhep.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Hashida R., Kawaguchi T., Koya S., Hirota K., Goshima N., Yoshiyama T., Otsuka T., Bekki M., Iwanaga S., Nakano D., et al. Impact of Cancer Rehabilitation on the Prognosis of Patients with Hepatocellular Carcinoma. Oncol. Lett. 2020 doi: 10.3892/ol.2020.11345. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pedersen B.K., Febbraio M.A. Muscles, exercise and obesity: Skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 2012;8:457–465. doi: 10.1038/nrendo.2012.49. [DOI] [PubMed] [Google Scholar]
- 14.Dasarathy S., Dodig M., Muc S.M., Kalhan S.C., McCullough A.J. Skeletal muscle atrophy is associated with an increased expression of myostatin and impaired satellite cell function in the portacaval anastamosis rat. Am. J. Physiol. Gastrointest Liver Physiol. 2004;287:G1124–G1130. doi: 10.1152/ajpgi.00202.2004. [DOI] [PubMed] [Google Scholar]
- 15.Kanzleiter T., Rath M., Gorgens S.W., Jensen J., Tangen D.S., Kolnes A.J., Kolnes K.J., Lee S., Eckel J., Schurmann A., et al. The myokine decorin is regulated by contraction and involved in muscle hypertrophy. Biochem. Biophys. Res. Commun. 2014;450:1089–1094. doi: 10.1016/j.bbrc.2014.06.123. [DOI] [PubMed] [Google Scholar]
- 16.Bekki M., Hashida R., Kawaguchi T., Goshima N., Yoshiyama T., Otsuka T., Koya S., Hirota K., Matsuse H., Niizeki T., et al. The association between sarcopenia and decorin, an exercise-induced myokine, in patients with liver cirrhosis: A pilot study. J. Cachexia Sarcopenia Muscle Rapid Commun. 2018;1:e00068. doi: 10.1002/j.2617-1619.2018.tb00009.x. [DOI] [Google Scholar]
- 17.Tanaka Y., Tateishi R., Koike K. Proteoglycans Are Attractive Biomarkers and Therapeutic Targets in Hepatocellular Carcinoma. Int. J. Mol. Sci. 2018;19:E3070. doi: 10.3390/ijms19103070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi X., Liang W., Yang W., Xia R., Song Y. Decorin is responsible for progression of non-small-cell lung cancer by promoting cell proliferation and metastasis. Tumour Biol. 2015;36:3345–3354. doi: 10.1007/s13277-014-2968-8. [DOI] [PubMed] [Google Scholar]
- 19.Dawoody Nejad L., Biglari A., Annese T., Ribatti D. Recombinant fibromodulin and decorin effects on NF-kappaB and TGFbeta1 in the 4T1 breast cancer cell line. Oncol. Lett. 2017;13:4475–4480. doi: 10.3892/ol.2017.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horvath Z., Reszegi A., Szilak L., Danko T., Kovalszky I., Baghy K. Tumor-specific inhibitory action of decorin on different hepatoma cell lines. Cell Signal. 2019;62:109354. doi: 10.1016/j.cellsig.2019.109354. [DOI] [PubMed] [Google Scholar]
- 21.Svard J., Rost T.H., Sommervoll C.E.N., Haugen C., Gudbrandsen O.A., Mellgren A.E., Rodahl E., Ferno J., Dankel S.N., Sagen J.V., et al. Absence of the proteoglycan decorin reduces glucose tolerance in overfed male mice. Sci. Rep. 2019;9:4614. doi: 10.1038/s41598-018-37501-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao H., Xi H., Wei B., Cai A., Wang T., Wang Y., Zhao X., Song Y., Chen L. Expression of decorin in intestinal tissues of mice with inflammatory bowel disease and its correlation with autophagy. Exp. Ther. Med. 2016;12:3885–3892. doi: 10.3892/etm.2016.3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gubbiotti M.A., Neill T., Frey H., Schaefer L., Iozzo R.V. Decorin is an autophagy-inducible proteoglycan and is required for proper in vivo autophagy. Matrix Biol. 2015;48:14–25. doi: 10.1016/j.matbio.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pohle T., Altenburger M., Shahin M., Konturek J.W., Kresse H., Domschke W. Expression of decorin and biglycan in rat gastric tissue: Effects of ulceration and basic fibroblast growth factor. Scand. J. Gastroenterol. 2001;36:683–689. doi: 10.1080/003655201300191932. [DOI] [PubMed] [Google Scholar]
- 25.Arii S., Sata M., Sakamoto M., Shimada M., Kumada T., Shiina S., Yamashita T., Kokudo N., Tanaka M., Takayama T., et al. Management of hepatocellular carcinoma: Report of Consensus Meeting in the 45th Annual Meeting of the Japan Society of Hepatology (2009) Hepatol. Res. 2010;40:667–685. doi: 10.1111/j.1872-034X.2010.00673.x. [DOI] [PubMed] [Google Scholar]
- 26.European Association for the Study of the Liver Electronic address, e.e.e., European Association for the Study of the, L. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Koya S., Kawaguchi T., Hashida R., Goto E., Matsuse H., Saito H., Hirota K., Taira R., Matsushita Y., Imanaga M., et al. Effects of in-hospital exercise on liver function, physical ability, and muscle mass during treatment of hepatoma in patients with chronic liver disease. Hepatol. Res. 2017;47:E22–E34. doi: 10.1111/hepr.12718. [DOI] [PubMed] [Google Scholar]
- 28.Hirota K., Kawaguchi T., Koya S., Nagamatsu A., Tomita M., Hashida R., Nakano D., Niizeki T., Matsuse H., Shiba N., et al. Clinical utility of the Liver Frailty Index for predicting muscle atrophy in chronic liver disease patients with hepatocellular carcinoma. Hepatol. Res. 2019;50:330–341. doi: 10.1111/hepr.13453. [DOI] [PubMed] [Google Scholar]
- 29.Schneider C.A., Rasband W.S., Eliceiri K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brooks D., Solway S., Gibbons W.J. ATS statement on six-minute walk test. Am. J. Respir Crit. Care Med. 2003;167:1287. doi: 10.1164/ajrccm.167.9.950. [DOI] [PubMed] [Google Scholar]
- 31.Chong C.D., Dumkrieger G.M., Schwedt T.J. Structural Co-Variance Patterns in Migraine: A Cross-Sectional Study Exploring the Role of the Hippocampus. Headache. 2017;57:1522–1531. doi: 10.1111/head.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forner A., Gilabert M., Bruix J., Raoul J.L. Treatment of intermediate-stage hepatocellular carcinoma. Nat. Rev. Clin. Oncol. 2014;11:525–535. doi: 10.1038/nrclinonc.2014.122. [DOI] [PubMed] [Google Scholar]
- 33.Shimose S., Tanaka M., Iwamoto H., Niizeki T., Shirono T., Aino H., Noda Y., Kamachi N., Okamura S., Nakano M., et al. Prognostic impact of transcatheter arterial chemoembolization (TACE) combined with radiofrequency ablation in patients with unresectable hepatocellular carcinoma: Comparison with TACE alone using decision-tree analysis after propensity score matching. Hepatol. Res. 2019;49:919–928. doi: 10.1111/hepr.13348. [DOI] [PubMed] [Google Scholar]
- 34.Nishikawa H., Enomoto H., Ishii A., Iwata Y., Miyamoto Y., Ishii N., Yuri Y., Hasegawa K., Nakano C., Nishimura T., et al. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J. Cachexia Sarcopenia Muscle. 2017;8:915–925. doi: 10.1002/jcsm.12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dasarathy S., Merli M. Sarcopenia from mechanism to diagnosis and treatment in liver disease. J. Hepatol. 2016;65:1232–1244. doi: 10.1016/j.jhep.2016.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singhal G., Kumar G., Chan S., Fisher F.M., Ma Y., Vardeh H.G., Nasser I.A., Flier J.S., Maratos-Flier E. Deficiency of fibroblast growth factor 21 (FGF21) promotes hepatocellular carcinoma (HCC) in mice on a long term obesogenic diet. Mol. Metab. 2018;13:56–66. doi: 10.1016/j.molmet.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu P., Zhang Y., Wang W., Yuan Q., Liu Z., Rasoul L.M., Wu Q., Liu M., Ye X., Li D., et al. Long-Term Administration of Fibroblast Growth Factor 21 Prevents Chemically-Induced Hepatocarcinogenesis in Mice. Dig. Dis. Sci. 2015;60:3032–3043. doi: 10.1007/s10620-015-3711-z. [DOI] [PubMed] [Google Scholar]
- 38.Watanabe M., Singhal G., Fisher F.M., Beck T.C., Morgan D.A., Socciarelli F., Mather M.L., Risi R., Bourke J., Rahmouni K., et al. Liver-derived FGF21 is essential for full adaptation to ketogenic diet but does not regulate glucose homeostasis. Endocrine. 2020;67:95–108. doi: 10.1007/s12020-019-02124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai J., Chen F., Chen J., Ruan G., He M., Chen C., Tang J., Wang D.W. Overexpression of decorin promoted angiogenesis in diabetic cardiomyopathy via IGF1R-AKT-VEGF signaling. Sci. Rep. 2017;7:44473. doi: 10.1038/srep44473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barallobre-Barreiro J., Gupta S.K., Zoccarato A., Kitazume-Taneike R., Fava M., Yin X., Werner T., Hirt M.N., Zampetaki A., Viviano A., et al. Glycoproteomics Reveals Decorin Peptides With Anti-Myostatin Activity in Human Atrial Fibrillation. Circulation. 2016;134:817–832. doi: 10.1161/CIRCULATIONAHA.115.016423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwon J.H., Kim M., Bae Y.K., Kim G.H., Choi S.J., Oh W., Um S., Jin H.J. Decorin Secreted by Human Umbilical Cord Blood-Derived Mesenchymal Stem Cells Induces Macrophage Polarization via CD44 to Repair Hyperoxic Lung Injury. Int. J. Mol. Sci. 2019;20:E4815. doi: 10.3390/ijms20194815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horvath Z., Kovalszky I., Fullar A., Kiss K., Schaff Z., Iozzo R.V., Baghy K. Decorin deficiency promotes hepatic carcinogenesis. Matrix Biol. 2014;35:194–205. doi: 10.1016/j.matbio.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Y., Wang Y., Du Z., Wang Q., Wu M., Wang X., Wang L., Cao L., Hamid A.S., Zhang G. Recombinant human decorin suppresses liver HepG2 carcinoma cells by p21 upregulation. Onco Targets Ther. 2012;5:143–152. doi: 10.2147/OTT.S32918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamid A.S., Li J., Wang Y., Wu X., Ali H.A., Du Z., Bo L., Zhang Y., Zhang G. Recombinant human decorin upregulates p57KIP (2) expression in HepG2 hepatoma cell lines. Mol. Med. Rep. 2013;8:511–516. doi: 10.3892/mmr.2013.1510. [DOI] [PubMed] [Google Scholar]
- 45.Appunni S., Anand V., Khandelwal M., Gupta N., Rubens M., Sharma A. Small Leucine Rich Proteoglycans (decorin, biglycan and lumican) in cancer. Clin. Chim. Acta. 2019;491:1–7. doi: 10.1016/j.cca.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Tsidulko A.Y., Kazanskaya G.M., Volkov A.M., Suhovskih A.V., Kiselev R.S., Kobozev V.V., Gaytan A.S., Krivoshapkin A.L., Aidagulova S.V., Grigorieva E.V. Chondroitin sulfate content and decorin expression in glioblastoma are associated with proliferative activity of glioma cells and disease prognosis. Cell Tissue Res. 2020;379:147–155. doi: 10.1007/s00441-019-03127-2. [DOI] [PubMed] [Google Scholar]