Abstract
Nonalcoholic fatty liver disease (NAFLD) emerges as an important global burden and Helicobacter pylori infection (Hp-I) has been suggested as a risk factor of NAFLD, although controversy exists. This retrospective study aimed to investigate a potential impact of active Hp-I on NAFLD severity in morbidly obese patients, subjected to bariatric surgery and gastric biopsy for documentation of Hp-I. Of 64 eligible participants, 15 (23.4%) were diagnosed with active Hp-I, showing higher rates of nonalcoholic steatohepatitis (NASH) than those without Hp-I (86.7% vs. 26.5%, respectively; p < 0.001). Concerning histological lesions, steatosis grade (p = 0.027), ballooning (p < 0.001), lobular inflammation (p = 0.003), and fibrosis stage (p < 0.001) were also more severe in Hp-I positive patients. Likewise, liver function tests, insulin resistance, dyslipidemia, and arterial hypertension were significantly higher in Hp-I positive patients. Hp-I was independently positively associated with NASH (beta = 3.27; p = 0.002), severe NASH (beta = 2.37; p = 0.018), and the presence of fibrosis (beta = 3.86; p = 0.001) in a binary regression model, after adjustment for potential confounders. In conclusion, active Hp-Ι was independently associated with NASH and fibrosis, findings offering potential clinical implication.
Keywords: nonalcoholic steatohepatitis, NASH, NAFLD, nonalcoholic fatty liver disease, Helicobacter pylori, Hp, metabolic syndrome, MetS
1. Introduction
Nonalcoholic fatty liver disease (NAFLD), as the hepatic component of the metabolic syndrome (MetS), represents a leading cause of chronic liver disease; its estimated global prevalence is about 25% of the general population [1] whereas in morbidly obese individuals its prevalence might rise up to 90% [1,2]. NAFLD is bidirectionally linked to MetS and insulin resistance (IR) [3]. The general term NAFLD encompasses a spectrum of distinct pathologies; simple steatosis (nonalcoholic fatty liver, NAFL) represents a reportedly benign entity, but might progress in a percentage of patients after the effect of “multiple hits” [2,3,4], to nonalcoholic steatohepatitis (NASH), which may also progress to fibrosis, liver cirrhosis, and hepatocellular carcinoma [3].
One of the potential pathogenetic “multiple hits, is regarded to be Helicobacter pylori infection (Hp-I) [1], with an estimated prevalence of 58% (varying from 39.9%–91.7%) worldwide [5]. Hp-I exhibits pleiotropic local and systematic manifestations. Peptic ulcer, nonulcer dyspepsia, gastric adenocarcinoma, gastric mucosa-associated lymphoid tissue lymphoma, and colorectal cancer belong to its classical pathogenicity [6,7]. Beyond its established local pathologies, Hp-I has been associated with systematic entities, including MetS, IR, diabetes mellitus type 2 (T2DM), coronary artery disease, and neurodegenerative diseases [1,8]. In addition, there is accumulating evidence, that Hp-I might contribute to the development and progression of NAFLD, as concluded in several studies [9,10,11,12,13], although controversy still exists [14,15,16], as we have previously systematically reviewed [1]. Notably, meta-analyses, having been conducted on the association between Hp-I and NAFLD, showed higher rates of NAFLD in Hp infected individuals, as we have also reviewed [5].
Together with the aforementioned high prevalence of NAFLD in morbidly obese individuals, the prevalence of Hp seropositivity in these patients is also higher (a 1.7-fold increased probability of having Hp-I) compared with nonobese controls [17]. However, the serological test does not discriminate between active and past infection. Beyond serological testing for Hp-I, there are further diagnostic modalities used for the investigation of a possible association between Hp-I and NAFLD: Urea breath test [18,19,20,21,22,23] and the detection of Hp antigen in patients’ stool [24] for the diagnosis of Hp-I, as well as sonography [10,19,23,24,25,26], and liver function tests and various noninvasive indices [10,11,22,27] for the diagnosis of NAFLD. Nevertheless, 13C urea breath and Hp antigen fecal tests are also not sufficient to substitute the histological diagnostic “gold standard” for detection of active Hp-I; the gold standards for the diagnosis of Hp-I and NAFLD are currently histological examination after gastric and liver biopsies, respectively [28,29,30,31]. However, studies with gastric and liver biopsies are currently scarce [14].
The aim of this study was to investigate a potential association of active Hp-I with NAFLD and its histological severity in morbidly obese patients subjected to bariatric surgery, gastric, and liver biopsy.
2. Methods
2.1. Study Design
The study was performed retrospectively, using an electronic database with 94,304 case records of patients who have been presented to the emergency department (ED) of Inselspital Bern from 1 January 2017 to 30 November 2018. This academic hospital offers its medical services to an area of approximately 2,000,000 citizens.
2.2. Ethical Considerations
The last revision of the principles of the Declaration of Helsinki was fulfilled. The study was approved by the cantonal (district) ethics committee in Berne, (Kantonale Ethikkommission Bern, Ref. No. KEK-BE: 010/2016) and since our patients were fully anonymized prior to analysis, according to Swiss law, informed consent was not mandatory.
2.3. Inclusion and Exclusion Criteria
Eligible were morbidly obese patients older than 16 years having been subjected to bariatric surgery, as well as to liver and gastric biopsy for documentation of NAFLD and active Hp-I, respectively. Exclusion criteria were: Ethanol consumption (>20 g/day); previous Hp eradication treatment; known history of other active or past hepatobiliary disease; history of gastrectomy; malignancies; inappropriate thyroid or adrenal function; kidney disease; pregnancy or lactation; use of glucocorticoids, insulin, orlistat, methotrexate, amiodarone, vitamin E, pioglitazone, intravenous glucose, or parenteral nutrition administration; any drug addiction; type 1 DM; pancreatitis; thrombotic disorders. Patients with T2DM were excluded if they were on thiazolidinediones or insulin treatment.
2.4. Data Collection and Extraction
Morbidly obese patients undergoing an elective bariatric operation were recruited. Specifically, the Hp-I status was evaluated by the diagnostic “gold standard” histology from gastric biopsies, obtained either preoperatively (in terms of a routine esophagogastroduodenoscopy) or intraoperatively. Histological diagnosis of Hp gastritis was made on 5 μm formalin-fixed, paraffin-embedded tissue sections by means of Hematoxylin and Eosin staining. A modified Giemsa stain was also used to highlight the Hp bacteria.
Liver specimens were obtained intraoperatively during laparoscopic bariatric surgery, from liver segment II or, less commonly, segment III. Grading and staging of NAFLD was based on the NASH Clinical Research Network scoring system [32]; for the discrimination between NAFL and NASH, both NAFLD activity score (NAS) [32] and fatty liver inhibition of progression (FLIP) were used, the latter introduced in morbidly obese populations [29]. Severe NASH was defined as steatosis, activity, and fibrosis (SAF) scoring system ≥3 and/or F ≥ 3, as elsewhere recommended [33].
Patients’ records at the time of admission to the ED were stored in the clinical application E.care for Windows (E.care BVBA, ED 2.1.3.0, Turnhout, Belgium). E.care offers the advantage of instantaneous recall of medical reports, and other relevant data, while multiple filters of E.care application can be applied. Patients’ records from ED were extracted to an Excel sheet (Microsoft® Excel for Mac 2019, Microsoft Corporation, Redmond, WA, USA) with the use of appropriate filters. Eligibility of the retrieved patients was evaluated by two investigators (M.D. and S.S.), following the inclusion and exclusion criteria. Selected data were validated by D.S.S. In cases of conflict, a consensus was met by the intervention of a senior author (A.Ε.). The following parameters were extracted: (a) Demographics and anthropometric (age, gender, body-mass index (BMI)); (b) histological findings of gastric and liver biopsies: Hp-I positivity, steatosis grade, lobular inflammation, ballooning degeneration, and fibrosis; (c) MetS components, i.e., IR, dyslipidemia, hypertension, and T2DM, as recommended by the Expert Committee on the Diagnosis and Classification of Diabetes [34]; in this regard, dyslipidemia was defined as triglyceride levels ≥150 mg/dL (1.7 mmol/L) or LDL-C levels ≥ 100–160 mg/dl (2.58–4.13 mmol/L, depending on other risk factors) or HDL-C levels < 40 and 50 mg/dl (1.03 and 1.29 mmol/L) in men and women, respectively, or treatment with hypolipidemic medication(s); arterial hypertension was defined as systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg or treatment with antihypertensive medication(s); (d) laboratory tests: Fasting glucose and fasting insulin (for the calculation of IR, using the homeostasis model assessment IR (HOMA-IR) [35]), glycated hemoglobin A1c (Hba1c), liver function tests (aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), bilirubin).
2.5. Statistical Analysis
Data are presented as mean ± standard deviation (SD) and percentages, for continuous and categorical variables, respectively. The normality of distributions of continuous variables was tested with the Kolmogorov–Smirnov test. The comparisons of continuous and categorical variables were performed with the Mann–Whitney test and chi-square test (or the Fischer exact test), respectively. Binary logistic regression analysis was performed to investigate whether Hp-I was independently associated with NASH, severe NASH and fibrosis, because they are considered the main histological endpoints. As independent variables, we entered parameters related to MetS (BMI, hypertension, dyslipidemia, HOMA-IR), as well as age and gender. Statistical analysis was performed with SPSS 21.0 for Macintosh (IBM Corp., Armonk, NY, USA). Significance was set at p < 0.05 (two tailed).
3. Results
Sixty-four patients (47 women), subjected to both gastric and liver biopsy, were recruited in this study. Fifteen (23.4%) patients were positive for Hp-I. According to the FLIP algorithm, nine (14.1%) patients were classified as “No NAFLD”, 29 (45.3%) as NAFL, and 26 (40.6%) as NASH. Severe NASH was observed in 13 (20.3%) patients. According to NAS, eight (12.5%) patients were classified as “No NAFLD”, 25 (39.0%) as NAFL, 17 (26.6%) as borderline NASH, and 14 (21.9%) as definite NASH. Regarding fibrosis stage, 39 (61.0%) patients were at F0, 18 (28.1%) at F1, 5 (7.8%) at F2, 2 (3.1%) at F3, whereas none were at F4; due to the small number of patients at F3, categories F2 and F3 were merged for the analysis (F2/3: 7 (10.9%) patients).
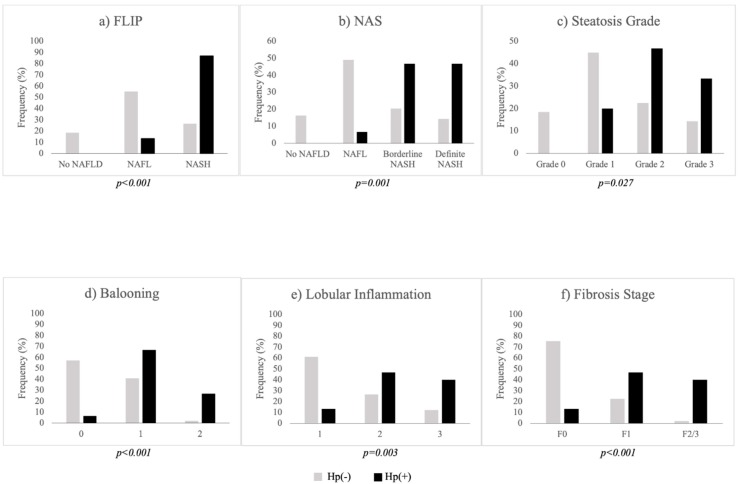
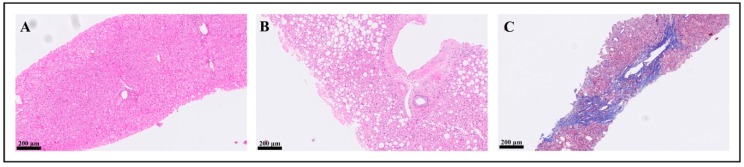
Comparative data between Hp-I positive [Hp(+)] and negative [Hp(−)] patients are presented in Table 1. Hp(+) and Hp(−) groups were of similar gender age, and BMI. AST, ALT, GGT, bilirubin, triglycerides, and HOMA-IR were higher in Hp(+) than in Hp(−) group, whereas total cholesterol, HDL-C, and LDL-C were not statistically different between groups. Higher rates of hypertension (p = 0.041) and triglyceridemia (p = 0.039), but not prediabetes/diabetes, were observed in Hp(+) than Hp(−) group. Regarding both FLIP and NASH classifications, higher rates of NASH were observed in Hp(+) than in Hp(−) group (Table 1). Likewise, higher rates of severe NASH were observed in Hp(+) than in Hp(−) group. Concerning separate histological lesions, histological severity was more prominent in Hp(+) than Hp(−) patients in steatosis grade, ballooning, lobular inflammation, and fibrosis (Table 1, Figure 1). Representative histological images from the included patients are illustrated in Figure 2. When the analysis was repeated in women (n = 47), the results remained essentially unchanged. However, the analysis in men was avoided, mainly owing to the small sample of men (n = 17), which might have led to insecure conclusions.
Table 1.
Comparative data between Hp(+) and Hp(−) patients.
|
Hp(−) N = 49 (76.6%) |
Hp(+) N = 15 (23.4%) |
p-Value * | |
|---|---|---|---|
| Women [N (%)] | 37 (75.5) | 10 (66.7) | 0.52 |
| Age (years) | 46.7 ± 13.3 | 49.1 ± 12.4 | 0.51 |
| BMI (kg/m2) | 45.5 ± 10.2 | 42.6 ± 5.9 | 0.70 |
| AST (U/L) | 24.5 ± 9.0 | 42.7 ± 18.9 | 0.001 |
| ALT (U/L) | 28.6 ± 20.5 | 51.6 ± 24.5 | <0.001 |
| GGT (U/L) | 35.7 ± 43.9 | 86.3 ± 60.2 | <0.001 |
| Bilirubin (μmol/L) | 7.8 ± 5.2 | 12.2 ± 8.3 | 0.013 |
| Triglycerides (mmol/L) | 1.48 ± 1.58 | 2.02 ± 0.98 | 0.003 |
| Total cholesterol (mmol/L) | 4.39 ± 1.14 | 4.79 ± 0.46 | 0.10 |
| HDL-C (mmol/L) | 1.29 ± 0.37 | 1.23 ± 0.46 | 0.55 |
| LDL-C (mmol/L) | 2.48 ± 0.85 | 2.72 ± 0.64 | 0.20 |
| HbA1c (%) | 5.7 ± 0.6 | 6.0 ± 1.3 | 0.33 |
| HOMA-IR | 4.3 ± 3.9 | 10.1 ± 6.8 | <0.001 |
| Prediabetes/Diabetes [N (%)] | 24 (49.0) | 9 (60.0) | 0.46 |
| Arterial hypertension [N (%)] | 18 (36.7) | 10 (66.7) | 0.041 |
| FLIP [N (%)] | <0.001 | ||
| No NAFLD | 9 (18.4) | 0 (0.0) | |
| NAFL | 27 (55.1) | 2 (13.3) | |
| NASH | 13 (26.5) | 13 (86.7) | |
| Severe NAFLD [N (%)] | 6 (12.2) | 7 (46.7) | 0.008 |
| NAS [N (%)] | 0.001 | ||
| No NAFLD | 8 (16.3) | 0 (0.0) | |
| NAFL | 24 (49.0) | 1 (6.6) | |
| Borderline NASH | 10 (20.4) | 7 (46.7) | |
| Definite NASH | 7 (14.3) | 7 (46.7) | |
| Steatosis [N (%)] | 0.027 | ||
| Grade 0 | 9 (18.4) | 0 (0.0) | |
| Grade 1 | 22 (44.9) | 3 (20.0) | |
| Grade 2 | 11 (22.4) | 7 (46.7) | |
| Grade 3 | 7 (14.3) | 5 (33.3) | |
| Ballooning [N (%)] | <0.001 | ||
| 0 | 28 (57.1) | 1 (6.6) | |
| 1 | 20 (40.8) | 10 (66.7) | |
| 2 | 1 (2.0) | 4 (26.7) | |
| Lobular inflammation [N (%)] | 0.003 | ||
| 0 | 30 (61.2) | 2 (13.3) | |
| 1 | 13 (26.5) | 7 (46.7) | |
| 2 | 6 (12.2) | 6 (40.0) | |
| Fibrosis stage [N (%)] | <0.001 | ||
| F0 | 37 (75.5) | 2 (13.3) | |
| F1 | 11 (22.4) | 7 (46.7) | |
| F2/3 | 1 (2.0) | 6 (40.0) |
Data are presented as mean ± standard deviation (SD) for continuous, and frequencies (percentage) for categorical variables. * Between group comparisons (Mann–Whitney test for continuous and chi-square or Fischer exact test for categorical variables). Abbreviations: ALT: Alanine transaminase; AST: Aspartate transaminase; BMI: Body mass index; FLIP: Fatty liver inhibition of progression; GGT: Gamma-glutamyl transferase; HbA1: Glycated hemoglobin; HDL: High density lipoprotein; HOMA-IR: Homeostatic model of assessment insulin resistance; LDL: Low density lipoprotein; NAFLD: Nonalcoholic fatty liver disease; NAS: Nonalcoholic fatty liver disease activity score; NASH: Nonalcoholic steatohepatitis.
Figure 1.
Bar grams depicting the histological endpoints: (a) FLIP; (b) NAS; (c) steatosis grade; (d) ballooning; (e) lobular inflammation; (f) fibrosis stage. The rates of Hp infection were increased with the severity of all presenting histological lesions and composite scores (FLIP and NAS). Hp(+): Black bars; Hp(−): Grey bars. Abbreviations: F: Fibrosis stage; FLIP: Fatty liver inhibition of progression; Hp(+): Helicobacter pylori positive; Hp(−): Helicobacter pylori negative; NAFLD: Nonalcoholic fatty liver disease; NAS: Nonalcoholic fatty liver disease activity score; NASH: Nonalcoholic steatohepatitis.
Figure 2.
Liver microphotographs of patients with the most representing stages of nonalcoholic fatty liver disease. (A) Formalin fixed, paraffin embedded histological section (hematoxylin and eosin staining) of liver with normal architecture. (B) Formalin fixed, paraffin embedded histological section (hematoxylin and eosin staining) of liver with prominent steatosis without activity or fibrosis. (C) Formalin fixed, paraffin embedded histological section (Masson trichrome staining) of liver with bridging fibrosis.
Binary regression analysis was performed with FLIP as dependent variable in a subset of patients (NALF vs. NASH; n = 55), after the exclusion of those without NAFLD (n = 9). The results of this analysis are presented in Table 2. NASH remained independently positively associated with Hp-I (p = 0.002) after adjusting for potential confounding. Next, regression analysis was performed with severe NASH as dependent variable (No vs. Yes) in the sum of patients. Again, severe NASH remained independently positively associated with Hp-I (p = 0.018; Table 3). In this model, age and BMI were also independently positively associated with severe NASH. Likewise, when fibrosis (F0 vs. F1-3) in the sum of patients was selected as dependent variable, the presence of fibrosis remained independently positively associated with Hp-I (p = 0.001; Table 4). In this model gender was also independently associated with the presence of fibrosis (i.e., men had independently higher risk of fibrosis).
Table 2.
Independent associates of NASH (NAFL vs. NASH), according to FLIP classification in binary logistic regression analysis.
| Independent Variables | Beta | Exp(Beta) | p-Value | 95% CI for Exp(Beta) |
|---|---|---|---|---|
|
Hp-I diagnosis
(0: Negative; 1: Positive) |
3.27 | 26.32 | 0.002 | 3.36–206.23 |
|
Gender
(0: Women; 1: Men) |
1.30 | 3.68 | 0.14 | 0.65–20.73 |
|
Hypertension
(0: No; 1: Yes) |
−1.17 | 0.31 | 0.19 | 0.05–1.80 |
|
Hyperglyceridemia
(0: No; 1: Yes) |
−0.33 | 0.72 | 0.70 | 0.14–3.75 |
| Age (years) | 0.03 | 1.03 | 0.40 | 0.97–1.09 |
| BMI (kg/m2) | 0.05 | 1.06 | 0.15 | 0.98–1.14 |
| HOMA-IR | 0.15 | 1.17 | 0.12 | 0.96–1.41 |
Abbreviations: BMI: Body mass index; FLIP: Fatty liver inhibition of progression; HOMA-IR: Homeostatic model of assessment insulin resistance; Hp-I: Helicobacter pylori infection; NAFL: Nonalcoholic fatty liver; NASH: Nonalcoholic steatohepatitis.
Table 3.
Independent associates of severe NASH (No vs. Yes), according to FLIP classification in binary logistic regression analysis.
| Independent Variables | Beta | Exp(Beta) | p-Value | 95% CI for Exp(Beta) |
|---|---|---|---|---|
|
Hp-I diagnosis
(0: Negative; 1: Positive) |
2.37 | 10.73 | 0.018 | 1.50–76.46 |
|
Gender
(0: Women; 1: Men) |
0.06 | 1.06 | 0.95 | 0.17–6.58 |
|
Hypertension
(0: No; 1: Yes) |
0.06 | 1.07 | 0.94 | 0.20–5.74 |
|
Hyperglyceridemia
(0: No; 1: Yes) |
0.44 | 1.56 | 0.62 | 0.27–9.09 |
| Age (years) | 0.09 | 1.10 | 0.028 | 1.01–1.19 |
| BMI (kg/m2) | 0.10 | 1.10 | 0.035 | 1.01–1.21 |
| HOMA-IR | 0.02 | 1.02 | 0.82 | 0.88–1.17 |
Abbreviations: BMI: Body mass index; FLIP: Fatty liver inhibition of progression; HOMA-IR: Homeostatic model of assessment insulin resistance; Hp–I: Helicobacter pylori infection; NAFL: Nonalcoholic fatty liver; NASH: Nonalcoholic steatohepatitis.
Table 4.
Independent associates of fibrosis (F0 vs. F1-3) in binary logistic regression analysis.
| Independent Variables | Beta | Exp(Beta) | p-value | 95% CI for Exp(Beta) |
|---|---|---|---|---|
|
Hp-I diagnosis
(0: Negative; 1: Positive) |
3.86 | 47.28 | 0.001 | 4.76–469.5 |
|
Gender
(0: Women; 1: Men) |
1.95 | 7.00 | 0.026 | 1.26–39.02 |
|
Hypertension
(0: No; 1: Yes) |
−0.18 | 0.84 | 0.82 | 0.18–3.90 |
|
Hyperglyceridemia
(0: No; 1: Yes) |
−0.20 | 0.82 | 0.81 | 0.16–4.11 |
| Age (years) | 0.05 | 1.05 | 0.08 | 0.99–1.12 |
| BMI (kg/m2) | −0.05 | 0.95 | 0.37 | 0.86–1.06 |
| HOMA-IR | −0.04 | 0.96 | 0.56 | 0.83–1.11 |
Abbreviations: BMI: Body mass index; FLI: Fatty liver inhibition of progression; HOMA-IR: Homeostatic model of assessment insulin resistance; Hp-I: Helicobacter pylori infection; NAFL: Nonalcoholic fatty liver; NASH: Nonalcoholic steatohepatitis.
4. Discussion
This study favors an association between active Hp-I and histological severity of NAFLD in morbidly obese patients subjected to bariatric surgery. Specifically, higher rates of NASH, as well as hepatic steatosis, inflammation, and fibrosis were observed in Hp(+) than Hp(−) patients, findings warranting further investigation. Notably, Hp-I was independently positively associated with NASH, severe NASH, and hepatic fibrosis, the latter considered as the main histological prognostic factor [36].
Importantly, the histological diagnostic “gold standard” for both main variables of interest (active Hp-I and NAFLD) were used, which is scarce in the literature. More specifically, this is the second study, after the study of Lecube et al. [14] investigating the association between Hp-I and NAFLD by using both gastric and liver biopsies, in which liver biopsy was performed in a subset of patients (22% of patients subjected to gastric biopsy). In that study, higher steatosis rates were observed in Hp(+) patients, as in our study, but, unexpectedly rates of NASH were higher in Hp(−) patients. Moreover, contrary to our finding, the authors reported similar overall NAFLD rates between Hp(+) and Hp(−) patients [14]. There is no secure conclusion about the controversy of our with Lecube et al. [14] study; population and/or methodological differences may exist, thus warranting more studies, specifically designed to this aim.
Noteworthy, we were the first to show an association between Hp-I and NAFLD in a case-control study of biopsy-proven NAFLD patients [37]. Subsequently, other studies reported a positive association between Hp-I and NAFLD, including those of Yu et al. [19], Sumida et al. [38], Okushin et al. [18], Kim et al. [10,27], Zhang et al. [21], Chen et al. [26], Dogan et al. [25], Abdel-Razik et al. [24], and Kang et al. [11]. Noteworthy, there have been five systematic reviews performed with meta-analysis, all of which revealed a positive association between the pathologies of interest [39,40,41,42,43]. Nonetheless, there are studies showing no association between Hp-I and NAFLD [14,15,19,20,22].
The association between Hp-I and components related to IR or MetS were also investigated in this study as secondary aims. Higher liver function tests, triglycerides, HOMA-IR, and higher rates of arterial hypertension were observed in Hp(+) compared with Hp(−) patients. In a systematic review we performed almost 10 years ago, we have proposed a positive association between Hp-I and IR, in terms of HOMA-IR [44]. Although controversy still exists, similar results to this study have provided a meta-analysis between Hp-I, MetS, and MetS-related comorbidities [45].
The observational nature of this study cannot show causality or direction of the relationship, i.e., to answer the question whether Hp-I is another pathogenetic factor of NAFLD or, inversely, NAFLD makes affected individuals more susceptible to Hp-I. However, pathogenetic mechanisms between Hp-I and NAFLD may be hypothesized. Hp-I related gastrointestinal epithelium disruption, microbiota, and their metabolites translocation into portal circulation, activation of inflammation via toll-like receptors signaling in hepatocytes, may be some contributors linking Hp-I with the development and progression of NAFLD [3,46]. In this regard, human β-defensin-1, possibly serving as a biomarker of bacterial translocation in chronic liver disease, is induced by Hp-I. Hp-I also contributes to a low-grade inflammation by inducing the release of vasoactive and proinflammatory molecules, including interleukin (IL)-1, IL-6, IL-8, IL-10, IL-12, tumor necrosis factor-α, interferon-γ, eicosanoids (leukotrienes, prostaglandins), and acute phase proteins (C-reactive protein and fibrinogen), which are implicated in the pathophysiology of IR syndrome and NAFLD. Moreover, Hp-related induction of oxidative stress, atrophic gastritis-associated with vitamin B12/folate deficiency, apoptosis, and the possible downregulation of adiponectin, constitute other pathogenetic links between Hp-I and NAFLD [3,46]. Furthermore, Hp-related galectin-3 connected with MetS may play a role in the pathophysiology of MetS-related NAFLD and its extrahepatic complications, including chronic kidney, cardiovascular, and brain disorders; the number of galectin-3 positive liver cells is associated with NAFLD severity; galectin-3 binding protein is a potential marker of disease; and galectin-3 inhibitors may exhibit potential efficacy in advanced fibrosis/cirrhosis due to NASH. Finally, Hp-related MetS conditions are associated with dysmotility-induced microbiota dysbiosis, particularly small intestinal bacterial overgrowth (SIBO) playing a role in the pathogenesis of NAFLD; SIBO exhibits an effect on the structural and functional issues of the liver leading to greater prevalence of NAFLD. Notably, SIBO prevalence is higher in morbidly obese patients than in healthy populations and is connected with severe hepatic steatosis [47]. However, further large-scale relative studies are needed to elucidate in depth the aforementioned proposed pathogenetic mechanisms.
Although the use of both liver and gastric biopsies is a strength of this study, there are also certain limitations. First, the retrospective nature of the study renders it susceptible to record and recall bias. Second, as mentioned above, a cause–effect relationship cannot be shown. Third, the sample size was small, although it was sufficient to show robust statistical significance in major endpoints. Furthermore, information on previous use of proton pump inhibitors before obtaining gastric biopsies was not available. Last, the duration of Hp-I, which might have affected the results, remains unknown.
5. Conclusions
This study favors an association of active Hp-I on NAFLD severity in morbidly obese patients subjected to bariatric surgery. Most importantly, active Hp-I was independently associated with NASH and the presence of fibrosis. These findings warrant specifically designed clinical studies on the association between active Hp-I and NAFLD severity in obese, morbidly obese, and lean populations, as well as mechanistic studies investigating the potential pathogenetic links.
Abbreviations
BMI: Body-mass index; ED: Emergency department; FLIP: Fatty Liver Inhibition of Progression; GI: Gastrointestinal; Hba1: Glycated hemoglobin A1c; HOΜA-IR: Homeostatic model of assessment insulin resistance; Hp: Helicobacter pylori; Hp-I: Helicobacter pylori infection; IR: Insulin resistance; IL: Interleukin; MetS: Metabolic syndrome; NAFLD: Nonalcoholic fatty liver disease; NAS: NAFLD activity score; NASH: Nonalcoholic steatohepatitis; SAF: Steatosis, activity, and fibrosis; SIBO: Small intestinal bacterial overgrowth; T2DM: Diabetes mellitus type 2.
Author Contributions
Conceptualization, M.D., S.A.P., J.K.; methodology, M.D., S.A.P., J.K.; software, M.D., J.K.-R., A.P., S.A.P.; validation, D.S.S., A.K.E., J.K.; investigation, M.D., S.S., A.P., A.B.; resources, D.S.S., J.K.-R., A.K.E., D.S.S.; writing—original draft M.D., S.S., S.A.P, A.P.; writing—review and editing, M.D., S.S., S.A.P., J.K., A.B.; visualization, M.D., S.S.; supervision, D.S.S., A.K.E., J.K.; project administration, D.S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
M. Doulberis has received a travel grant by the Gilead Sciences Switzerland Sàrl. The other authors have no conflict of interest.
References
- 1.Polyzos S.A., Kountouras J. Helicobacter pylori infection and nonalcoholic fatty liver disease: Time for large clinical trials evaluating eradication therapy. Helicobacter. 2019;24:e12588. doi: 10.1111/hel.12588. [DOI] [PubMed] [Google Scholar]
- 2.Doulberis M., Kotronis G., Gialamprinou D., Kountouras J., Katsinelos P. Non-alcoholic fatty liver disease: An update with special focus on the role of gut microbiota. Metabolism. 2017;71:182–197. doi: 10.1016/j.metabol.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Doulberis M., Polyzos S.A., Papaefthymiou A., Katsinelos P., Kiosses C., Kountouras J. Treatment of nonalcoholic fatty liver disease: From adult trials to perspectives in the management of children and adolescents. Expert Opin. Pharmacother. 2020;21:247–275. doi: 10.1080/14656566.2019.1702967. [DOI] [PubMed] [Google Scholar]
- 4.Polyzos S.A., Kountouras J., Anastasiadis S., Doulberis M., Katsinelos P. Nonalcoholic fatty liver disease: Is it time for combination treatment and a diabetes-like approach? Hepatology. 2018;68:389. doi: 10.1002/hep.29897. [DOI] [PubMed] [Google Scholar]
- 5.Polyzos S.A., Kountouras J., Mantzoros C.S. Helicobacter pylori infection and nonalcoholic fatty liver disease: Are the four meta-analyses favoring an intriguing association pointing to the right direction? Metabolism. 2019;96:iii–v. doi: 10.1016/j.metabol.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Kountouras J., Doulberis M., Papaefthymiou A., Polyzos S.A., Touloumtzi M., Elisabeth V., Kapetanakis N., Liatsos C., Gavalas E., Katsinelos P. Helicobacter pylori infection and gastrointestinal tract cancer biology: Considering a double-edged sword reflection. Cell. Mol. Life Sci. 2019;76:2487–2488. doi: 10.1007/s00018-019-03106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malfertheiner P., Megraud F., O’morain C.A., Gisbert J.P., Kuipers E.J., Axon A.T., Hunt R. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66:6–30. doi: 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 8.Doulberis M., Kotronis G., Thomann R., Polyzos S.A., Boziki M., Gialamprinou D., Kountouras J. Impact of Helicobacter pylori on Alzheimer’s disease: What do we know so far? Helicobacter. 2018;23:e12454. doi: 10.1111/hel.12454. [DOI] [PubMed] [Google Scholar]
- 9.He C., Cheng D., Wang H., Wu K., Zhu Y., Lu N. Helicobacter pylori infection aggravates diet-induced nonalcoholic fatty liver in mice. Clin. Res. Hepatol. Gastroenterol. 2018;42:360–367. doi: 10.1016/j.clinre.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 10.Kim T.J., Sinn D.H., Min Y.W., Son H.J., Chang Y., Baek S.-Y., Ahn S.H., Lee H., Ryu S. A cohort study on Helicobacter pylori infection associated with nonalcoholic fatty liver disease. J. Gastroenterol. 2017;29:559–1210. doi: 10.1007/s00535-017-1337-y. [DOI] [PubMed] [Google Scholar]
- 11.Kang S.J., Kim H.J., Kim D., Ahmed A. Association between cagA negative Helicobacter pylori status and nonalcoholic fatty liver disease among adults in the United States. PLoS ONE. 2018;13:e0202325. doi: 10.1371/journal.pone.0202325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen C., Zhang C., Wang X., Zhang F., Zhang Z., Ma P., Feng S. Helicobacter pylori infection may increase the severity of nonalcoholic fatty liver disease via promoting liver function damage, glycometabolism, lipid metabolism, inflammatory reaction and metabolic syndrome. Eur. J. Gastroenterol. Hepatol. 2019 doi: 10.1097/MEG.0000000000001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abo-Amer Y.E.-E., Sabal A., Ahmed R., Hasan N.F.E., Refaie R., Mostafa S.M., Mohamed A.A., Khalil M., Elagawy W., Abd-Elsalam S. Relationship between helicobacter pylori infection and nonalcoholic fatty liver disease (Nafld) in a developing country: A cross-sectional study. Diabetes Metab. Syndr. Obes. Targets Ther. 2020;13:619–625. doi: 10.2147/DMSO.S237866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lecube A., Valladares S., López-Cano C., Gutiérrez L., Ciudin A., Fort J.M., Reñé J.M., Matias-Guiu X., De Torres I., Bueno M., et al. The Role of Morbid Obesity in the Promotion of Metabolic Disruptions and Non-Alcoholic Steatohepatitis by Helicobacter Pylori. PLoS ONE. 2016;11:e0166741. doi: 10.1371/journal.pone.0166741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu L.-J., Hao N.-B., Liu J.-J., Li X., Wang R.-L. Correlation between Helicobacter pylori Infection and Metabolic Abnormality in General Population: A Cross-Sectional Study. Gastroenterol. Res. Pract. 2018;2018:7410801. doi: 10.1155/2018/7410801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohammadifard M., Saremi Z., Rastgoo M., Akbari E. Relevance between Helicobacter pylori Infection and Non-Alcoholic Fatty Liver Disease in Birjand, Iran. J. Med. Life. 2019;12:168–172. doi: 10.25122/jml-2019-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erim T., Cruz-Correa M.R., Szomstein S., Velis E., Rosenthal R. Prevalence of Helicobacter pylori seropositivity among patients undergoing bariatric surgery: A preliminary study. World J. Surg. 2008;32:2021–2025. doi: 10.1007/s00268-008-9608-7. [DOI] [PubMed] [Google Scholar]
- 18.Okushin K., Takahashi Y., Yamamichi N., Shimamoto T., Enooku K., Fujinaga H., Tsutsumi T., Shintani Y., Sakaguchi Y., Ono S., et al. Helicobacter pylori infection is not associated with fatty liver disease including non-alcoholic fatty liver disease: A large-scale cross-sectional study in Japan. BMC Gastroenterol. 2015;15:25. doi: 10.1186/s12876-015-0247-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu Y.-Y., Cai J.-T., Song Z.-Y., Tong Y.-L., Wang J.-H. The associations among Helicobacter pylori infection, white blood cell count and nonalcoholic fatty liver disease in a large Chinese population. Medicine. 2018;97:e13271. doi: 10.1097/MD.0000000000013271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fan N., Peng L., Xia Z., Zhang L., Wang Y., Peng Y. Helicobacter pylori Infection Is Not Associated with Non-alcoholic Fatty Liver Disease: A Cross-Sectional Study in China. Front. Microbiol. 2018;9:73. doi: 10.3389/fmicb.2018.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang C., Guo L., Qin Y., Li G. Correlation between Helicobacter pylori infection and polymorphism of adiponectin gene promoter -11391G/A, superoxide dismutase gene in nonalcoholic fatty liver disease. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2016;41:359–366. doi: 10.11817/j.issn.1672-7347.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Baeg M.K., Yoon S.K., Ko S.-H., Noh Y.-S., Lee I.-S., Choi M.-G. Helicobacter pylori infection is not associated with nonalcoholic fatty liver disease. World J. Gastroenterol. 2016;22:2592–2600. doi: 10.3748/wjg.v22.i8.2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai O., Huang Z., Li M., Zhang C., Xi F., Tan S. Association between Helicobacter pylori Infection and Nonalcoholic Fatty Liver Disease: A Single-Center Clinical Study. Gastroenterol. Res. Pract. 2018;2018:8040262. doi: 10.1155/2018/8040262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abdel-Razik A., Mousa N., Shabana W., Refaey M., Elhelaly R., Elzehery R., Abdelsalam M., Elgamal A., Nassar M.R., Abu El-Soud A., et al. Helicobacter pylori and non-alcoholic fatty liver disease: A new enigma? Helicobacter. 2018;23:e12537. doi: 10.1111/hel.12537. [DOI] [PubMed] [Google Scholar]
- 25.Doğan Z., Filik L., Ergül B., Sarikaya M., Akbal E. Association between Helicobacter pylori and liver-to-spleen ratio: A randomized-controlled single-blind study. Eur. J. Gastroenterol. Hepatol. 2013;25:107–110. doi: 10.1097/MEG.0b013e3283590c10. [DOI] [PubMed] [Google Scholar]
- 26.Chen C.-X., Mao Y.-S., Foster P., Zhu Z.-W., Du J., Guo C.-Y. Possible association between Helicobacter pylori infection and nonalcoholic fatty liver disease. Appl. Physiol. Nutr. Metab. 2017;42:295–301. doi: 10.1139/apnm-2016-0499. [DOI] [PubMed] [Google Scholar]
- 27.Kim T.J., Lee H., Kang M., Kim J.E., Choi Y.-H., Min Y.W., Min B.-H., Lee J.H., Son H.J., Rhee P.-L., et al. Helicobacter pylori is associated with dyslipidemia but not with other risk factors of cardiovascular disease. Sci. Rep. 2016;6:38015. doi: 10.1038/srep38015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kountouras J., Mylopoulos N., Chatzopoulos D., Zavos C., Boura P., Konstas A.G.P., Venizelos J. Eradication of Helicobacter pylori may be beneficial in the management of chronic open-angle glaucoma. Arch. Intern. Med. 2002;162:1237–1244. doi: 10.1001/archinte.162.11.1237. [DOI] [PubMed] [Google Scholar]
- 29.Bedossa P., FLIP Pathology Consortium Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60:565–575. doi: 10.1002/hep.27173. [DOI] [PubMed] [Google Scholar]
- 30.Darma A., Nugroho B.S.T., Yoanna V., Sulistyani I., Athiyyah A.F., Ranuh R.G., Sudarmo S.M. Comparison of Helicobacter pylori stool antigen, salivary IgG, serum IgG, and serum IgM as diagnostic markers of H. pylori infection in children. Iran. J. Microbiol. 2019;11:206–211. doi: 10.18502/ijm.v11i3.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang T., Chen X., Xia C., Liu H., Yan H., Wang G., Wu Z. Association between Helicobacter pylori infection and non-alcoholic fatty liver disease in North Chinese: A cross-sectional study. Sci. Rep. 2019;9:4874. doi: 10.1038/s41598-019-41371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleiner D.E., Brunt E.M., Van Natta M., Behling C., Contos M.J., Cummings O.W., Ferrell L.D., Liu Y.-C., Torbenson M.S., Unalp-Arida A., et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 33.Nascimbeni F., Bedossa P., Fedchuk L., Pais R., Charlotte F., Lebray P., Poynard T., Ratziu V. Clinical validation of the FLIP algorithm and the SAF score in patients with non-alcoholic fatty liver disease. J. Hepatol. 2019 doi: 10.1016/j.jhep.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 34.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2005;28:S37–S42. doi: 10.2337/diacare.28.suppl_1.S37. [DOI] [PubMed] [Google Scholar]
- 35.Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 36.Polyzos S., Slavakis A., Koumerkeridis G., Katsinelos P., Kountouras J. Noninvasive Liver Fibrosis Tests in Patients with Nonalcoholic Fatty Liver Disease: An External Validation Cohort. Horm. Metab. Res. 2019;51:134–140. doi: 10.1055/a-0713-1330. [DOI] [PubMed] [Google Scholar]
- 37.Polyzos S.A., Kountouras J., Papatheodorou A., Patsiaoura K., Katsiki E., Zafeiriadou E., Zavos C., Anastasiadou K., Terpos E. Helicobacter pylori infection in patients with nonalcoholic fatty liver disease. Metabolism. 2013;62:121–126. doi: 10.1016/j.metabol.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 38.Sumida Y., Kanemasa K., Imai S., Mori K., Tanaka S., Shimokobe H., Kitamura Y., Fukumoto K., Kakutani A., Ohno T., et al. Helicobacter pylori infection might have a potential role in hepatocyte ballooning in nonalcoholic fatty liver disease. J. Gastroenterol. 2015;50:996–1004. doi: 10.1007/s00535-015-1039-2. [DOI] [PubMed] [Google Scholar]
- 39.Mantovani A., Turino T., Altomari A., Lonardo A., Zoppini G., Valenti L., Tilg H., Byrne C.D., Targher G. Association between Helicobacter pylori infection and risk of nonalcoholic fatty liver disease: An updated meta-analysis. Metabolism. 2019;96:56–65. doi: 10.1016/j.metabol.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 40.Ning L., Liu R., Lou X., Du H., Chen W., Zhang F., Li S., Chen X., Xu G. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: A systemic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2019;31:735–742. doi: 10.1097/MEG.0000000000001398. [DOI] [PubMed] [Google Scholar]
- 41.Zhou B.-G., Yang H.-J., Xu W., Wang K., Guo P., Ai Y.-W. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: A systematic review and meta-analysis of observational studies. Helicobacter. 2019;24:e12576. doi: 10.1111/hel.12576. [DOI] [PubMed] [Google Scholar]
- 42.Wijarnpreecha K., Thongprayoon C., Panjawatanan P., Manatsathit W., Jaruvongvanich V., Ungprasert P. Helicobacter pylori and Risk of Nonalcoholic Fatty Liver Disease. J. Clin. Gastroenterol. 2018;52:386–391. doi: 10.1097/MCG.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 43.Liu R., Liu Q., He Y., Shi W., Xu Q., Yuan Q., Lin Q., Li B., Ye L., Min Y., et al. Association between Helicobacter pylori infection and nonalcoholic fatty liver: A meta-analysis. Medicine. 2019;98:e17781. doi: 10.1097/MD.0000000000017781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polyzos S.A., Kountouras J., Zavos C., Deretzi G. The association between Helicobacter pylori infection and insulin resistance: A systematic review. Helicobacter. 2011;16:79–88. doi: 10.1111/j.1523-5378.2011.00822.x. [DOI] [PubMed] [Google Scholar]
- 45.Upala S., Jaruvongvanich V., Riangwiwat T., Jaruvongvanich S., Sanguankeo A. Association between Helicobacter pylori infection and metabolic syndrome: A systematic review and meta-analysis. J. Dig. Dis. 2016;17:433–440. doi: 10.1111/1751-2980.12367. [DOI] [PubMed] [Google Scholar]
- 46.Polyzos S.A., Kountouras J. Novel Advances in the Association Between Helicobacter pylori Infection, Metabolic Syndrome, and Related Morbidity. Helicobacter. 2015;20:405–409. doi: 10.1111/hel.12228. [DOI] [PubMed] [Google Scholar]
- 47.Sabaté J.-M., Jouët P., Harnois F., Mechler C., Msika S., Grossin M., Coffin B. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: A contributor to severe hepatic steatosis. Obes. Surg. 2008;18:371–377. doi: 10.1007/s11695-007-9398-2. [DOI] [PubMed] [Google Scholar]