Highlights
-
•
First COVID-19 outbreak in Spain.
-
•
A hotel guest from Italy presented to a hospital with symptoms of an acute respiratory infection.
-
•
The hotel was immediately placed under quarantine for 14 days.
-
•
Control measures employed to mitigate a large international cluster.
-
•
In total, eight hotel guests have been identified as Covid-19 cases.
Keywords: COVID-19, Outbreak, Hotel, Quarantine, Rapid response, Outbreak control
Abstract
Since the first accounts of SARS-CoV-2, authorities have encountered numerous unprecedented situations threatening public health. This rapid communication addresses events that led to the quarantining of a hotel in Tenerife, Spain and the effectiveness of the rapidly implemented control measures. In total, eight cases have been associated with the hotel. Due to the international nature of the guests, had these timely precautions not been in place, a multinational cluster might have formed.
Case description
On the 24th of February an individual travelling from at-risk regions in Italy presented to a hospital in Tenerife with symptoms of an acute respiratory infection that started on the 16th of February, the day before arriving in Spain. This individual was then tested and confirmed to have contracted COVID-19. Due to the prolonged exposure of this symptomatic index case to their travel group and other hotel guests, public health authorities quickly realized the potential threat and immediately placed the hotel under quarantine.
Aim
This rapid communication will focus on the management of cases and contacts of a confirmed case of SARS-CoV-2 associated with a hotel in southern Tenerife. The objective is the factual description of the first outbreak in Spain caused by a novel pathogen including timelines, lessons learned and recommendations.
Methods
Case definition
In Spain, the national Protocol for the Management of COVID-19 cases includes the guidelines on the surveillance and investigation of cases and their contacts by the National Surveillance Network. This is a dynamic document that was subject to changes based on the evolution of the epidemic in Spain. At the time of the outbreak the following definitions were used, which were based on the ECDC and WHO guidelines (Gobierno de España - Ministerio de Sanidad, 2020, European Center for Disease Prevention and Control, 2020, World Health Organisation (WHO), 2020):
-
•
Case under investigation:
-
1)
A patient with acute respiratory tract infection (sudden onset of at least one of the following: cough, fever, shortness of breath) AND with no other aetiology that fully explains the clinical presentation AND with a history of travel or residence in a country/area reporting local or community transmission during the 14 days prior to symptom onset (at that time China and four regions in Italy) OR
-
2)
A patient with any acute respiratory illness AND having been in close contact with a confirmed or probable COVID-19 case in the last 14 days prior to onset of symptoms OR
-
3)
A hospitalised patient with severe acute respiratory infection (pneumonia, acute respiratory distress syndrome, multi-organ failure, septic shock, admission to Intensive Care Unit or death) AND with no other aetiology that fully explains the clinical presentation.
-
•
Confirmed case: A person with laboratory confirmation i.e. positive PCR for SARS-CoV-2 and positive confirmatory PCR for an alternative gene.
-
•
Probable case: A case under investigation for whom tests for SARS-CoV-2 are inconclusive or for whom only one PCR was positive
-
•
Discarded case: A case under investigation for whom PCR was negative.
Epidemiological investigation
National protocols state that after a case is laboratory confirmed, the Public Health Authorities of the Autonomous Regions conduct interviews to identify people who have been in close contact with a symptomatic case. In this particular situation, in a hotel with more than 1000 staff and guests, and in which the magnitude of the outbreak was unknown when the first case was detected, active case finding was conducted, including PCR testing of close contacts of the index case. Moreover, PCR tests were performed on hotel guests that did not meet the ‘case under investigation’ definition but required a certificate that they were SARS-CoV-2 negative in order to travel.
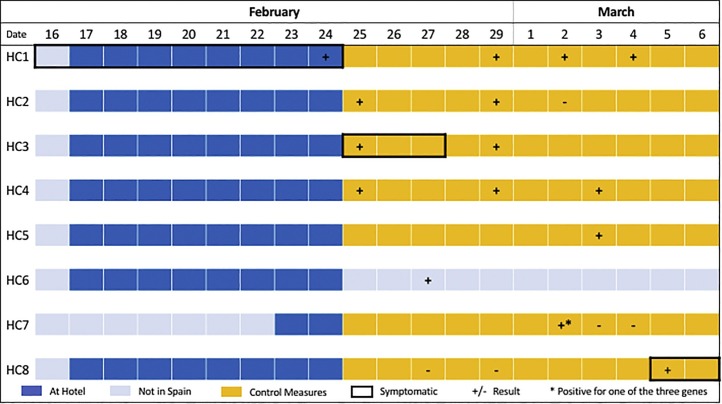
The clinical, epidemiological and laboratory data were compiled by the Public Health Authorities of the Canary Islands and were used to describe the evolution of the events related to the COVID-19 outbreak reported in Tenerife during the period of the quarantine, i.e. 24 February -10 March 2020. A timeline was created to present the main events, including the measures taken. Cases were numbered chronologically, i.e. HC1 indicates the first hotel case identified and HC8 the last one to date.
Results and discussion
Description of cases
The index case (Hotel case 1 or HC1) arrived in Tenerife on the 17th of February with their partner and a group of eight individuals that were considered close contacts in accordance with the protocol. Due to the prolonged exposure of the close contacts to HC1, the Public Health Authorities decided that it would be prudent to test them. Three close contacts, including HC1’s partner (HC2) tested positive for SARS-CoV-2 and were transferred to a local hospital, to be isolated. Of these individuals, only one, HC3, was symptomatic (fever), with symptoms starting from 25 February. The six close contacts who remained in isolation in their hotel rooms were continuously monitored. Four days later, a fifth member of the group (HC5) tested positive despite being asymptomatic and was hospitalised.
In the following days two other guests (HC6 and HC7) tested positive for SARS-CoV-2. There is very little information about HC6, as this case returned to their country of origin before the implementation of the control measures and tested positive upon their return. The seventh case (HC7) tested positive for SARS-CoV-2 during a screening required for their repatriation and was also hospitalised. HC7 initially tested positive for only one of the three genes assessed using the real-time (RT) PCR. Subsequent samples taken from HC7 then tested negative twice, and HC7 was discharged from the hospital on the 5th of March. On that day, the last case of this cluster was detected (HC8). The patient, who was part of the travel group from Italy, was symptomatic and had a positive PCR result after two prior negative PCR results (Figure 1 ).
Figure 1.
Timeline of cases detected at Hotel: HC stands for hotel case. The implementation of the control measures and hotel quarantine occured on the night of the 24th of February. The ‘+’ and ‘-’ refer to the dates samples were collected. Results may have been obtained on a later date, but on the indicated date the cases were positive/negative for SARS-CoV-2. HC6 left the hotel on the 24th, prior to the implementation of control measures.
Control measures
After the confirmation of HC1, on the 24th of February, Public Health Authorities immediately quarantined the hotel and no guests were permitted to leave the hotel grounds and no new guests were permitted access, the guests of the hotel were recommended to stay in their hotel room and their temperatures were recorded in the morning and evening every day.
A field clinic was established immediately outside of the hotel to organize daily activities, the medical needs of guests and the sampling of residents displaying any of the related symptoms. All guests that presented with any corresponding symptoms at the time were tested for SARS-CoV-2. Over the course of this investigation nine close contacts of HC1 and 24 casual contacts were advised to self-monitor (bi-daily temperature taken and communicated to the field clinic) for the duration of the incubation period (14 days). Throughout this process over 400 samples from hotel guests, hotel workers and other cases under investigation unrelated to the hotel were tested by PCR. The guests that were asymptomatic were permitted access to communal dining areas, hotel activities and evening entertainment using non-pharmaceutical precautions in accordance with local, national, ECDC and WHO guidelines (Gobierno de España - Ministerio de Sanidad, 2020, European Center for Disease Prevention and Control, 2020, World Health Organisation (WHO), 2020). Staff and guests were recommended to maintain personal distance, to wear masks, and to practice good hand hygiene. Hotel staff monitored themselves by taking their temperatures every morning and evening and were granted access to the hotel provided appropriate personal protective equipment (PPE) requirements were met.
Lessons learned
The situation described in this communication was epidemiologically, logistically and legally very challenging. The act of placing a private facility such as the hotel under quarantine is riddled with legal procedures and ramifications. The fact that the vast majority of the hotel guests were from abroad, further complicated matters. That being said, the measures implemented have proven effective in mitigating a situation that could have resulted in the formation of a cluster with potential for subsequent international transmission. As such, the authors of this paper believe the specific tools used to mitigate this outbreak were: (i) the rapid action taken to quarantine the hotel, (ii) the field clinic set up outside the hotel to work closely with the staff and guests of the hotel to monitor symptoms and have a direct line of communication, (iii) close collaboration between the field clinic, hospitals and the public health authorities, and finally (iv) specific recommendations provided to other hotels with information to guests regarding how to act if experiencing symptoms corresponding to COVID-19. The cooperation of the hotel staff in this situation was commendable; providing ongoing catering, cleaning and entertainment to the quarantined guests drastically improved the morale in the hotel, greatly facilitating guest cooperation with public health services.
One aspect that could have been improved is information shared internationally regarding guests that returned to their home country after the arrival of the index case but before the quarantine was put into place. A further complication was the specific repatriation requirements of the different countries of origin. While some required tests prior to repatriation, other countries performed tests on arrival. This spread some degree of uncertainty amongst the hotel guests.
Despite arguments early on, especially from the tourism sector, that the measures were exaggerated, the actions turned out to be justified and effective, especially during a time that the epidemic was at a very early stage and social alarm was limited. In any case, measures implemented need to be assessed on a case by case basis and recommendations should be adapted to each specific situation depending on the risk of exposure and relevant social, cultural, or sanitary aspects. Due to the prolonged exposure to a symptomatic index case in the hotel, it was impossible to ascertain the number of cases at the moment the control measures needed to be set in place. The collaboration and communication between the Public Health authorities and the hotel management were vital for controlling this outbreak. The lessons learned from the containment of the outbreak in this hotel were used to prevent further outbreaks of this nature in the Canary Islands.
Ethical statement
Ethical approval was not needed because the Public Health Authorities in the Canary Islands are able to access information for communicable disease outbreak investigations in the public interest.
Acknowledgements
The authors of this paper would like to thank laboratory and hospital staff as well as the staff of the field clinic that proved invaluable in the management of this situation. Further thanks is extended to the emergency services of the Canary Islands (SUC), the GAPTFE operating the field clinic, the Public Health Authorities of the Canary Islands and their tireless efforts to control this event. Finally, thank you to the Coordination Centre for Health Alerts and Emergencies (CCAES) of the Ministry of Health, the National Centre for Epidemiology (CNE) and the National Centre for Microbiology (CNM) of the Carlos III Institute of Health (ISCIII) and the ECDC for their continued support in making this study possible.
References
- European Center for Disease Prevention and Control . 2020. Case definition and European surveillance for COVID-19, as of 2 March 2020.https://www.ecdc.europa.eu/en/case-definition-and-european-surveillance-human-infection-novel-coronavirus-2019-ncov Available from: [Google Scholar]
- Gobierno de España - Ministerio de Sanidad Procedimiento de actuación frente a casos de infección por el nuevo coronavirus (SARS-CoV-2) Actualización. 2020 27.02.2020. [Google Scholar]
- World Health Organisation (WHO) 2020. Global Surveillance for human infection with coronavirus disease (COVID-19). Interim guidance. 27 February 2020.https://www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel-coronavirus-(2019-ncov) Available from: [Google Scholar]