Abstract
Objective
Recreational legalization of cannabis may influence the medical use by patients. When only medical access was legally available in Canada, 4.3% of rheumatology patients reported use. With the current recreational legalization, we have reexamined the prevalence and characteristics of medical cannabis use in this same rheumatology setting.
Methods
Consecutively attending rheumatology patients participated in an onsite survey comprising the following two questionnaires: 1) demographic and disease information completed by the rheumatologist and 2) patient anonymous questionnaire of health status, cannabis use (recreational and/or medicinal), and characteristics of cannabis use.
Results
Of 1047 attendees from June to August 2019, with 1000 participating, medical cannabis had been used by 12.6% of patients (95% confidence interval 10.7%‐14.8%), with half continuing use for mostly pain relief. Discontinuation was due to lack of effect in 57% of patients and side effects in 28% of patients. Ever medical users were younger (61.2 vs. 64.9 years; P = 0.006), more likely unemployed/disabled (16.7% vs. 5.9%; P < 0.001), and had more previous (47.6% vs. 25.5%; P < 0.001) and current recreational cannabis use (17.5% vs. 3.1%; P < 0.001) than nonusers. Most patients used multiple methods of administration, including smoking, vaporizing, and using oral oil preparations, but were poorly knowledgeable of product content, which was bought solely via the legal medical route by only 20%, and only one‐third disclosed their use to the rheumatologist.
Conclusion
Medical cannabis use has tripled for rheumatology patients since recreational legalization, with users being younger, not working, and having recreational cannabis experience. Concerning issues are the poor knowledge of the product being used, access via the nonmedical route, and nondisclosure to the physician.
Introduction
Canadian patients have had legal access to medical cannabis via a Health Canada regulated program since 2001, with a requirement for physician oversight. Initially cannabis was available to persons with restricted diagnoses, but this restriction was lifted in 2014 to allow access for patients without need to identify their diagnoses. Relief of chronic musculoskeletal pain is one of the most frequent reasons patients report use of medical cannabis. In October 2018, Canadian regulations changed, and cannabis was legalized as a recreational product, with access allowed for persons over the age of 18 years (1). In this context, it can be anticipated that both interest in cannabis as a treatment and actual medicinal cannabis use by patients could change (2).
In a 2014 survey of 1000 consecutive unselected rheumatology attendees, we reported that 4.3% of patients had ever used medical cannabis, with 2.8% continuing use (3). This first reported survey of cannabis use among a large cohort of rheumatology patients with a physician confirmed diagnosis identified medical cannabis users as mostly younger, unemployed men who were diagnosed with osteoarthritis and had self‐reported poorer global well‐being. Recreational cannabis experience was reported for most, with almost half reporting concurrent medical and recreational use.
In this new climate of Canadian full legalization of cannabis, we have questioned whether the characteristics of medical cannabis use have changed from observations 5 years ago. Both cannabis use and harms related to cannabis use have been shown to increase following recreational legalization of cannabis (4, 5). Our hypothesis was that patients would be more willing to try cannabis for medical reasons, and if so, we were interested to know how cannabis was accessed.
This follow‐up study, which was conducted in the same setting as that used in 2014 and using the same methods, is a next step toward understanding the prevalence of the use of medical cannabis in the setting of the full legalization of cannabis. The primary objective was to assess the overall prevalence of medical cannabis use, with a secondary objective to assess patient characteristics and knowledge of the product being used. The study was conducted in the same rheumatology setting and with the same methods as those used in 2014.
Patients and Methods
In this observational study, all consecutive rheumatology patients who were referred to or attended a university‐affiliated outpatient rheumatology practice (staffed by three rheumatologists) for routine follow‐up between mid‐June and mid‐August 2019 were invited to participate. Patients were not preselected based on disease or disease status and were eligible for inclusion if they were aged at least 18 years, able to complete a questionnaire in English or French, and willing to sign an informed consent form. The study comprised two questionnaires, one physician‐completed and the other patient‐completed, numerically tagged to the consent form and completed at the time of the clinic visit.
The physician questionnaire recorded demographic information (sex, age, work status), rheumatic diagnosis, comorbidities, current pharmacologic treatments for the rheumatic disease, current/past cigarette use, and physician global assessment (PGA) of disease status (a 10‐cm visual analog scale [VAS] [0 very good; 10 very bad]).
The anonymous patient‐completed questionnaire comprised the following: current pain in the past 7 days (10‐cm VAS [0 no pain; 10 most severe pain]), patient global assessment (PtGA) of health status (10 cm VAS [0 very well; 10 very poorly]), ever and current recreational cannabis use, ever and current medical cannabis use, and if cannabis was ever used, the number of times, (less than 10 times or 10 or more times). If medical cannabis was discontinued, the reason for discontinuation was recorded as either not effective, side effects, cost, or other reasons. If medical cannabis had never been used, patients reported whether they would consider future use and whether use had been suggested by family/friends, medical person, media, or other.
Information about cannabis for all users (medical, recreational, or both) included the following: 1) method of use (smoked, vaporized, oil/capsules, edibles, topical application or other); 2) daily amount in g/d or ml/d; concentration of Δ9‐tetrahydrocannabinol (THC) and cannabidiol (CBD); and 3) access via medical prescription, a store (legal recreational, illegal medical dispensary, illegal recreational outlet), the internet, a friend, the street, or other. Symptoms treated were identified as pain, fatigue, poor sleep, anxiety, or other. Side effects included drowsiness, feeling high, fatigue, lack of energy, lack of motivation, or other. The benefit of cannabis was assessed by the question, “How much does cannabis help you with your symptoms?” and scored on a 10‐cm VAS (0 not at all; 10 very much).
The study received ethics approval from the Institutional Review Board Services in Ontario, Canada, an independent research ethics board, and all participants provided written informed consent.
Descriptive statistics, including the mean and SD for continuous variables and frequency distributions for categorical variables, were produced for all variables. The 95% confidence intervals (CIs) around the point estimate of the prevalence of cannabis use were calculated based on the normal approximation method. In addition to the overall results, stratified analyses by ever use of cannabis for medical reasons and, among ever users, by current use, were conducted. Between‐group comparisons were conducted with the independent‐samples t test for continuous variables and the Fisher's exact test for categorical variables, using a significance level set a priori of P < 0.05.
Given the descriptive nature of the study, sample size requirements were based on feasibility and the precision of the prevalence estimate. With an estimated doubling of the medical cannabis use compared with prior to legalization (1), a sample size of approximately 1000 patients would provide an absolute precision of less than 2%, which was judged as clinically meaningful.
All analyses were conducted using SPSS Version 24.0 (IBM Corporation).
Results
During the 2‐month study period, 1047 patients attended the rheumatology clinic; 34 patients were excluded, 13 declined to participate, and 1000 composed the study cohort (Figure 1).
Figure 1.
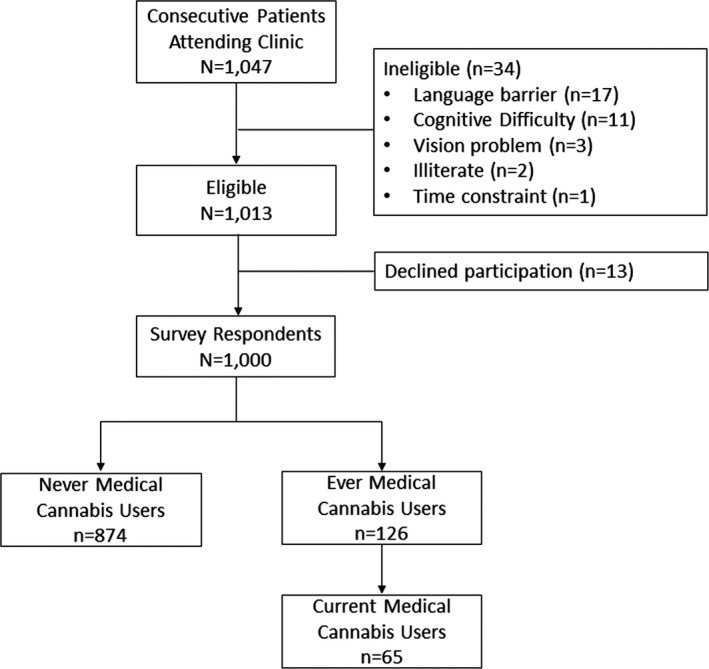
Flow Diagram.
Ever use of medical cannabis was reported by 126 (12.6%; 95 CI 10.7%‐14.8%) patients, with 65 (6.5%; 95% CI 5.1%‐8.2%) patients reporting current medical use (Table 1). Recreational cannabis, either past or current, was reported by 283 (28.3%; 95% CI 25.6%‐31.2%) patients, with 49 (4.9%; 95% CI 3.7%‐6.4%) patients reporting current recreational use. Of the 49 current recreational users, 22 (44.9%) reported using cannabis for both medicinal and recreational purposes.
Table 1.
Demographic and disease‐related information for 1000 rheumatology patients
| Characteristics | All Patients (N = 1000) | Never Medical Cannabis Users (n = 874) | Ever Medical Cannabis Users (n=126) | P a |
|---|---|---|---|---|
| Demographics | ||||
| Age, mean (SD), y | 64.4 (13.8) | 64.9 (13.7) | 61.2 (14.7) | 0.006 |
| Female sex, n (%) | 724 (72.4) | 626 (71.6) | 98 (77.8) | 0.166 |
| Employment, n (%) | <0.001 | |||
| Full‐time | 298 (29.8) | 258 (29.5) | 40 (31.7) | … |
| Part‐time | 69 (6.9) | 56 (6.4) | 13 (10.3) | … |
| Unemployed | 15 (1.5) | 11 (1.3) | 4 (3.2) | … |
| Disabled | 58 (5.8) | 41 (4.7) | 17 (13.5) | … |
| Student | 9 (0.9) | 9 (1.0) | 0 (0.0) | … |
| Retired | 551 (55.1) | 499 (57.1) | 52 (41.3) | … |
| Unemployed/disabled | 73 (7.3) | 52 (5.9) | 21 (16.7) | <0.001 |
| Rheumatic diseases | ||||
| Inflammatory arthritis,b n (%) | 621 (62.1) | 541 (61.9) | 80 (63.5) | 0.769 |
| Rheumatoid arthritis | 308 (30.8) | 277 (31.7) | 31 (24.6) | 0.122 |
| Psoriatic arthritis | 100 (10.0) | 84 (9.6) | 16 (12.7) | 0.269 |
| Ankylosing spondylitis | 72 (7.2) | 55 (6.3) | 17 (13.5) | 0.008 |
| SLE | 23 (2.3) | 21 (2.4) | 2 (1.6) | 0.757 |
| PMR | 72 (7.2) | 62 (7.1) | 10 (7.9) | 0.713 |
| Gout | 17 (1.7) | 15 (1.7) | 2 (1.6) | >0.999 |
| Other | 36 (3.6) | 32 (3.7) | 4 (3.2) | >0.999 |
| Osteoarthritis,c n (%) | 427 (42.7) | 374 (42.8) | 53 (42.1) | 0.923 |
| Small joints | 163 (16.3) | 145 (16.6) | 18 (14.3) | 0.606 |
| Large joints | 232 (23.2) | 204 (23.3) | 28 (22.2) | 0.822 |
| Spine | 175 (17.5) | 151 (17.3) | 24 (19.0) | 0.617 |
| Soft tissue rheumatism, n (%) | 227 (22.7) | 191 (21.9) | 36 (28.6) | 0.111 |
| Fibromyalgia | 117 (11.7) | 90 (10.3) | 27 (21.4) | 0.001 |
| Tendonitis/bursitis | 121 (12.1) | 110 (12.6) | 11 (8.7) | 0.244 |
| Other rheumatic condition, n (%) | 109 (10.9) | 93 (10.6) | 16 (12.7) | 0.449 |
| Comorbid conditions, n (%) | ||||
| Cardiovascular | 394 (39.4) | 346 (39.6) | 48 (38.1) | 0.771 |
| Pulmonary | 64 (6.4) | 54 (6.2) | 10 (7.9) | 0.437 |
| Gastrointestinal | 194 (19.4) | 166 (19.0) | 28 (22.2) | 0.400 |
| Neurological | 49 (4.9) | 43 (4.9) | 6 (4.8) | 0.939 |
| Endocrine | 300 (30.0) | 273 (31.2) | 27 (21.4) | 0.029 |
| Mood disorder | 117 (11.7) | 96 (11.0) | 21 (16.7) | 0.074 |
| Other psychiatric disorder | 9 (0.9) | 6 (0.7) | 3 (2.4) | 0.093 |
| Other comorbid condition | 62 (6.2) | 58 (6.6) | 4 (3.2) | 0.166 |
| Medications for rheumatic diseases | ||||
| Number of medication types for rheumatic disease, mean (SD) | 1.3 (1.0) | 1.1 (0.9) | 2.0 (1.3) | <0.001 |
| Non‐steroidal anti‐inflammatory drug use, n (%) | 276 (27.6) | 234 (26.8) | 42 (33.3) | 0.136 |
| Disease‐modifying anti‐rheumatic drug use, n (%) | 323 (32.3) | 285 (32.6) | 38 (30.2) | 0.612 |
| Biologic use, n (%) | 155 (15.5) | 126 (14.4) | 29 (23.0) | 0.017 |
| Opioids use, n (%) | 76 (7.6) | 56 (6.4) | 20 (15.9) | 0.001 |
| Tranquilizer use, n (%) | 24 (2.4) | 17 (1.9) | 7 (5.6) | 0.023 |
| Antiepileptic use, n (%) | 95 (9.5) | 70 (8.0) | 25 (19.8) | <0.001 |
| Antidepressant use, n (%) | 70 (7.0) | 54 (6.2) | 16 (12.7) | 0.014 |
| Steroid use, n (%) | 150 (15.0) | 126 (14.4) | 24 (19.0) | 0.182 |
| Cannabis pharmaceutical, n (%) | 22 (2.2) | 6 (0.7) | 16 (12.7) | <0.001 |
| Cannabis herbal, n (%) | 34 (3.4) | 4 (0.5) | 30 (23.8) | <0.001 |
| Disease assessment, mean (SD) | ||||
| PGA (0‐10) | 2.6 (2.1) | 2.5 (2.0) | 3.5 (2.2) | <0.001 |
| PtGA (0‐10) | 3.7 (2.9) | 3.5 (2.9) | 4.8 (2.9) | <0.001 |
| Pain VAS, cm | 4.4 (3.0) | 4.2 (3.0) | 5.7 (2.8) | <0.001 |
| Cigarette use, n (%) | 0.002 | |||
| Nonsmoker | 636 (63.6) | 570 (65.2) | 66 (52.4) | … |
| Past smoker | 242 (24.2) | 209 (23.9) | 33 (26.2) | … |
| Current smoker | 114 (11.4) | 89 (10.2) | 25 (19.8) | … |
| Missing | 8 (0.8) | 6 (0.7) | 2 (1.6) | … |
| Cannabis use | ||||
| Recreational, n (%) | ||||
| Ever use | 283 (28.3) | 223 (25.5) | 60 (47.6) | <0.001 |
| Current use | 49 (4.9) | 27 (3.1) | 22 (17.5) | <0.001 |
| Medical, n (%) | ||||
| Ever used >10 times | 82 (8.2) | NA | 82 (65.1) | NA |
| Current medical use | 65 (6.5) | NA | 65 (51.6) | NA |
| If never used, consider medical use | NA | 466 (53.3) | NA | NA |
| Current cannabis use (any reason)e | ||||
| Current use, n (%) | 94 (9.4) | 27 (3.1) | 67 (53.2) | <0.001 |
| Method of herbal cannabis use,d n (%) | ||||
| Smoke | 44 (48.4)e | 17 (68.0)f | 27 (40.9)g | 0.033 |
| Vaporize | 23 (26.4)e | 3 (12.0)f | 21 (31.8)g | 0.066 |
| Oil/capsules | 34 (37.4)e | 0 (0.0)f | 34 (51.5)g | <0.001 |
| Edible | 25 (27.5)e | 4 (16.0)f | 21 (31.8)g | 0.189 |
| Rub | 4 (4.4)e | 0 (0.0)f | 4 (6.1)g | 0.572 |
| Current herbal cannabis use (medical reasons) | ||||
| Relief of symptoms (0‐10),h mean (SD) | NA | NA | 6.7 (2.5) | NA |
Abbreviation: NA, not applicable; PGA, Physician Global Assessment; PMR, polymyalgia rheumatica; PtGA, Patient Global Assessment; SLE, systemic lupus erythematosus; VAS, visual analog scale.
Significant (P < 0.05) P values indicated in bold. Missing category is not included in the comparison.
Patients may have had more than one type of inflammatory arthritis.
Patients may have had more than one type of osteoarthritis.
Patients may have used more than one method of herbal cannabis.
Proportions are based on the number of patients currently using herbal cannabis for any reason (all patients: n = 94; current recreational herbal cannabis users: n = 49; current medical herbal cannabis users: n = 65), excluding three patients who had missing method(s) of use.
Proportions are based on the number of patients in the never medical cannabis users group currently using herbal cannabis for recreational purposes (n = 27), excluding two patients who had missing method(s) of use.
Proportions are based on the number of patients in the ever medical cannabis users group currently using herbal cannabis for any reason (n = 67), excluding one patient who had missing method(s) of use.
Among patients using herbal cannabis for medical reasons; minimum (0) represents no relief, and maximum (10) represents maximum relief.
Demographic and disease information for the whole study cohort is shown in Table 1. There were 724 (72.4%) women, with a mean (± SD) age of 64.4 ± 13.8 years, and over 60% were not currently employed. The most prevalent diagnosis was inflammatory rheumatic disease in 62% of patients, followed by osteoarthritis in 43%, fibromyalgia in 12%, and tendonitis/bursitis in 12%, with some patients having more than one condition. Cardiovascular disease was present in 39% of patients, with 13% having a mood disorder or other psychiatric condition.
Ever medical cannabis users were younger (61.2 vs. 64.9 years; P = 0.006) and more likely to be unemployed or disabled (16.7% vs. 5.9%). Cigarette smoking and recreational cannabis use, both past and current, were significantly more common for ever medical users. The only rheumatic diseases that differed between groups were ankylosing spondylitis and fibromyalgia, which were more common in ever users (13.5% vs. 6.3% [P = 0.008] and 21.4% vs. 10.3% [P = 0.001], respectively). Drug treatments for the rheumatic disease differed significantly between ever medical cannabis users and nonusers, with greater use of the following in ever users: biologic disease modifying antirheumatic drugs (23.0% vs. 14.4%; P = 0.017), opioids (15.9% vs. 6.4%; P = 0.001), antiepileptics (19.8% vs. 8.0%; P < 0.001), antidepressants (12.7% vs. 6.2%; P = 0.014), tranquilizers (5.6% vs. 1.9%; P = 0.023), and pharmaceutical cannabis medicine (12.7% vs. 0.7%; P < 0.001). Of the 94 (9.4%) current cannabis users (both medical and recreational), the treating physician had knowledge of cannabis use for 34 (35.4%) patients. Parameters for global health as assessed by PGA and PtGA and pain VAS were significantly worse for ever users vs. nonusers. Over half of patients who had never used medical cannabis stated that they would be willing to consider use.
Medical cannabis was discontinued by 61 (48.4%) of the 126 ever medical users (Table 2). Those discontinuing use were older, less current cigarette smokers, and had less past/current recreational cannabis use. Global health status as measured by PGA and PtGA as well as pain VAS did not differ between current medical users or those discontinuing use. Reasons for discontinuation were lack of effect in 35 (57%) patients, side effects in 17 (28%), and cost in 7 (12%); 12 (20%) patients reported other reasons for discontinuation, including symptom improvement, family/religious disapproval, and inability to smoke cannabis.
Table 2.
Characteristics of 127 ever medical cannabis users
| Characteristics | Current Users (n = 65) | Discontinued Use (n = 61) | P a |
|---|---|---|---|
| Female sex, n (%) | 48 (73.8) | 50 (82.0) | 0.293 |
| Age, mean (SD), y | 57.6 (14.0) | 65.0 (14.6) | 0.004 |
| Employment, n (%) | 0.270 | ||
| Full‐time | 21 (32.3) | 19 (31.1) | … |
| Part‐time | 7 (10.8) | 6 (9.8) | … |
| Unemployed | 3 (4.6) | 1 (1.6) | … |
| Disabled | 12 (18.5) | 5 (8.2) | … |
| Student | 0 (0.0) | 0 (0.0) | … |
| Retired | 22 (33.8) | 30 (49.2) | … |
| Employment: unemployed/disabled, n (%) | 15 (23.1) | 6 (9.8) | 0.057 |
| Rheumatic diseases, n (%) | |||
| Inflammatory arthritis | 41 (63.1) | 39 (63.9) | >0.999 |
| Rheumatoid arthritis | 13 (20.0) | 18 (29.5) | 0.301 |
| Psoriatic arthritis | 10 (15.4) | 6 (9.8) | 0.427 |
| Ankylosing spondylitis | 9 (13.8) | 8 (13.1) | >0.999 |
| SLE | 2 (3.1) | 0 (0.0) | 0.497 |
| PMR | 4 (6.2) | 6 (9.8) | 0.521 |
| Gout | 1 (1.5) | 1 (1.6) | >0.999 |
| Other | 3 (4.6) | 1 (1.6) | 0.620 |
| Osteoarthritis | 26 (40.0) | 27 (44.3) | 0.719 |
| Small joints | 9 (13.8) | 9 (14.8) | >0.999 |
| Large joints | 11 (16.9) | 17 (27.9) | 0.198 |
| Spine | 13 (20.0) | 11 (18.0) | 0.824 |
| Soft tissue rheumatism | 19 (29.2) | 17 (27.9) | >0.999 |
| Fibromyalgia | 16 (24.6) | 11 (18.0) | 0.394 |
| Tendonitis/bursitis | 4 (6.2) | 7 (11.5) | 0.354 |
| Other rheumatic condition | 8 (12.3) | 8 (13.1) | >0.999 |
| Number of comorbid condition types, mean (SD) | 1.2 (1.0) | 1.1 (1.0) | 0.704 |
| Number of medication types for rheumatic disease, mean (SD) | 2.3 (1.4) | 1.6 (1.1) | 0.002 |
| Tobacco use, n (%) | 0.022 | ||
| Nonsmoker | 29 (44.6) | 37 (60.7) | … |
| Past smoker | 16 (24.6) | 17 (27.9) | … |
| Current smoker | 19 (29.2) | 6 (9.8) | … |
| Missing | 1 (1.5) | 1 (1.6) | … |
| Cannabis recreational, n (%) | |||
| Ever | 42 (64.6) | 18 (29.5) | <0.001 |
| Current | 20 (30.8) | 2 (3.3) | <0.001 |
| PGA (0‐10), mean (SD) | 3.6 (2.4) | 3.4 (2.0) | 0.545 |
| PtGA (0‐10), mean (SD) | 4.7 (2.8) | 4.9 (3.0) | 0.736 |
| Pain VAS, mean (SD), cm | 5.8 (2.6) | 5.6 (3.0) | 0.697 |
Abbreviation: PGA, Physician Global Assessment; PMR, polymyalgia rheumatica; PtGA, Patient Global Assessment; SLE, systemic lupus erythematosus; VAS, visual analog scale.
Significant (P < 0.05) P values indicated in bold. Missing category is not included in the comparison.
Of the 65 current medical cannabis users, about half were inhaling or using oils, with 43 (66%) patients using multiple methods of administration. Of the 31 (48%) patients who were inhaling (smoking or vaporizing) cannabis, the daily quantity or molecular content was provided by 14 and 4 patients, respectively. Of the 34 (52%) patients using liquid oils and/or capsules, the daily quantity or molecular content was provided by 20 patients each for oils and/or capsules. Cannabis was bought via the legal medical route by 13 (20%) patients, from a commercial outlet (either legal or illegal) by 17 (26.2%) patients, the internet by 22 (33.8%) patients, and a noncommercial avenue (friends, family, or the street) by 26 (40%) patients, with 18 (27.7%) patients accessing cannabis by multiple avenues. The daily amount and molecular concentrations of medical cannabis were poorly reported and mostly unknown. When reported, those smoking cannabis used between 0.5 and 3 g/d, with THC content up to 20% (if known), but 20 of the 27 smokers were not knowledgeable of the daily amount or content. Those vaporizing reported use of 0.5 to 1.5 g/d, with a report of more CBD content, and 8 of the 21 did not provide further information. Those using oils reported use of 0.5 to 20 ml/d, with a report of more CBD or equal THC/CBD content, or otherwise did not specify.
Overall symptom relief for medical/recreational cannabis users was 6.7 ± 2.5, with pain relief reported by 45 (69%) patients, improved sleep by 8 (12%), improved fatigue by 10 (15%), and improved mood by 5 (8%); 48 (74%) patients reported multiple symptom relief. Side effects were reported by 40 (61.5%) patients, with cognitive effects (drowsiness, fatigue, or lack of motivation) reported by 23 (35%), anxiety by 17 (26%), and lack of motivation by 13 (20%); 17 (26%) patients reported more than one adverse effect.
Discussion
This study provides real‐world information about medical cannabis use by rheumatology patients in the setting of cannabis recreational legalization, with information on patient characteristics, perceived effects, method and amount of use, access to product, and reasons for discontinuation. We report that 12.6% of 1000 unselected patients with a rheumatologist‐confirmed diagnosis of a spectrum of rheumatic diseases had ever used medical cannabis, with just over half continuing use. Discontinuation was mostly due to lack of effect, side effects, and cost. Ever medical users were mostly women in their 60s, with about half having previous experience with recreational cannabis. Pain relief was the most prevalent reason for use, but side effects were reported by 61% of users. Only 20% of medical users accessed cannabis entirely by the legal medical route, with most obtaining cannabis by various nonmedical routes, including the black market. It is therefore understandable and alarming that only a small minority of patients had knowledge of the molecular content or the daily amount of product used. Inhalation was the method of use for almost half of users, with two‐thirds using multiple methods of administration. The treating physician was aware of any cannabis use in only about one‐third of patients.
Several issues arising from this study deserve attention. Firstly, the method of access to cannabis is concerning. Most (80%) medical users were purchasing all or at least a portion of cannabis via a nonmedical route, with many reporting purchase via a personal contact, store/outlet, or the black market. Reasons for access via the nonmedical route may be multiple. The legal process to obtain medical cannabis can be cumbersome. A medical document authorizing use is submitted to a cannabis grower, who may then advise about strain and dosing and who arranges delivery of the product by postal service to a home address. Storefront assess is clearly simpler. Cost is also a plausible reason for nonmedical access. Medical cannabis is not reimbursed by public or private insurers for rheumatic complaints and is almost twice the price of black‐market cannabis. The average cost of medical cannabis is about $9.5/g, with patients reporting a monthly cost of between 100 and 300 Canadian dollars. Nonmedical cannabis, especially cannabis that is illegally bought, has risks associated with nonregulated products, with unknown molecular content and potential for contamination by other substances or infecting organisms.
Secondly, familiarity with smoking cigarettes or cannabis may have played a role for many patients in choosing inhalation as the method of administration. This is concerning in view of the large body of literature specifically addressing the added risks of smoking for patients with inflammatory rheumatic diseases (6). Vaping has, to date, been considered safer than smoking, but this study was conducted just prior to the publication on the emergence of severe respiratory illness related to vaping (7). Therefore, it is possible that patients perceived vaping as less harmful than smoking but preferred the more familiar method of inhalation. Furthermore, the effect of cannabis occurs within a few minutes of inhalation, which would give an immediate effect on symptoms in the moment.
Thirdly, the treating physician was unaware of any cannabis use for two‐thirds of the patients. Stigma may still be a factor in nondisclosure, but the widespread media coverage of cannabis may have prompted patients to self‐medicate without medical advice. Recreational cannabis legalization has allowed a cultural change, with cannabis no longer taboo, less risk of prosecution, and easier access. Furthermore, over half of nonusers would consider future medical cannabis use. Cannabis is now a Canadian household commodity and is offered by friends or family as a suggested therapy for medical illness.
Our current findings differ considerably from our earlier study in 2014. As anticipated, there has been a tripling in the numbers of patients using medical cannabis to almost 13%, and characteristics of patients have shifted toward an older, mostly female population with more prevalent inflammatory arthritis. We previously observed users to be mostly younger, unemployed men with osteoarthritis. Another notable change is that recreational cannabis experience was reported by about half of ever medical users in 2019, whereas this percentage was 80% in 2014. According to Statistics Canada's National Cannabis survey for the fourth quarter of 2019, cannabis for any reason had been used in the past 3 months by 16.7% of those surveyed, with half (about 8%) reporting use for medical reasons (8, 9). In contrast, only 1% of the Canadian population were registered with Health Canada as users of medical cannabis at that same time, emphasizing that most medical cannabis is accessed via the nonmedical route (10). Our findings that 6.5% of patients were current medical cannabis users align with the Canadian survey data. We also perceive that there is less of a blur between medicinal and recreational use, with some patients clearly identifying their use as one or the other or both. It could be argued that patients in our original study underreported medical cannabis use. As the prevalence of recreational ever use was similar in the two studies, we contend that the findings of the present study are reliable.
Previous surveys reporting on the efficacy of medical cannabis in chronic pain conditions generally report patient satisfaction with use, improved pain and psychological well‐being, and only limited side effects (11, 12, 13, 14, 15, 16, 17, 18). It is noteworthy that almost half of users in this present cohort had discontinued cannabis use, giving lack of effect or side effects as their reason for discontinuation. Those continuing use perceived benefits in multiple domains, but there were no differences in PGA, PtGA, or pain VAS between those continuing and discontinuing use. Furthermore, over 60% of current medical users reported some side effects. Our present finding of discontinuation of use is more likely reflective of real‐world experience because many studies reporting favorable effects may be subject to bias, with study settings often in designated cannabis clinics or with data from cannabis dispensaries. Alternately, compliance and success with use may be better when a patient is followed by a qualified health care professional with guidance about products and dosing, such as reported by clinics in Israel (18).
We believe that Canadian cannabis recreational legalization has influenced medical cannabis use with increased tolerance for use, social acceptability, removal of stigma, and perception of safety. Widespread media coverage, easier access, less risk of prosecution, and more affordable product on the illegal market are also influential factors. Cannabis is not innocuous, and use has implications for both patient and societal safety. Lacking long‐term studies in patients populations with comorbidities and concomitant medication use, safety issues have been recently highlighted by the National Academies of Sciences, Engineering, and Medicine and extend from the immediate risks of impaired cognition, psychomotor control, and memory to the long‐term risks for psychological and pulmonary health (19, 20).
Limitations must be considered. Although the study was anonymous, some patients may have refrained from acknowledging cannabis use. The information provided about cannabis used, including molecular content and daily amount used, was limited, likely because most cannabis was accessed via a nonmedical route. Additional information that is pertinent but unavailable included the baseline levels of symptoms prior to initiating cannabis, duration of cannabis use for all medical users, and treatment adjustments related to cannabis use. This is a single‐setting study that included only patients seen in a specialist rheumatology clinic; therefore results may not be reflective of a broader patient population and cannot be extrapolated to other countries where recreational cannabis is illegal or where medical cannabis is prescribed by physicians and/or is reimbursed by public or private insurers (21). A strength is that we have repeated a previous study, using the same methods, in a similar setting at two distinct time points, namely before and after recreational cannabis legalization. This information can be seen as a snapshot of the real‐world experience of patient use of medical cannabis, using a natural experimental setting.
We report a tripling of medical cannabis use in a cohort of rheumatology patients compared with 5 years ago, confirming our hypothesis that cannabis recreational legalization increases medical use. Almost 1 in 10 patients had tried cannabis as a therapy. Unlike many reports attesting to efficacy, we found that almost half of patients discontinued use after a mostly self‐administered trial. There are concerns about prevalent inhalation of cannabis, access via the nonmedical route, health risks for immunocompromised patients, and poor patient knowledge of daily amount or molecular content of the cannabis. Physicians must be aware that many patients may be self‐medicating with cannabis and that they are at risk for acute and chronic adverse effects that may be amplified by the underlying disease and prescribed medications. Our findings suggest that physicians may no longer be the gatekeepers for patients regarding cannabis use, with prevalent use slipping outside the bounds of ideal clinical care.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Fitzcharles had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Fitzcharles, Rampakakis, Sampalis, Shir, Cohen, Starr, Häuser.
Acquisition of data
Fitzcharles, Cohen, Starr.
Analysis and interpretation of data
Fitzcharles, Rampakakis, Sampalis, Shir, Häuser.
Supported by The Louise and Alan Edwards Foundation.
No potential conflicts of interest relevant to this article were reported.
References
- 1. Government of Canada . Cannabis laws and regulations. URL: https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/laws-regulations.html.
- 2. Hall W, Stjepanovic D, Caulkins J, Lynskey M, Leung J, Campbell G, et al. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet 2019;394:1580–90. [DOI] [PubMed] [Google Scholar]
- 3. Ste‐Marie PA, Shir Y, Rampakakis E, Sampalis JS, Karellis A, Cohen M, et al. Survey of herbal cannabis (marijuana) use in rheumatology clinic attenders with a rheumatologist confirmed diagnosis. Pain 2016;157:2792–7. [DOI] [PubMed] [Google Scholar]
- 4. Jones J, Nicole Jones K, Peil J. The impact of the legalization of recreational marijuana on college students. Addict Behav 2018;77:255–9. [DOI] [PubMed] [Google Scholar]
- 5. Carliner H, Brown QL, Sarvet AL, Hasin DS. Cannabis use, attitudes, and legal status in the U.S.: a review. Prev Med 2017;104:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chang K, Yang SM, Kim SH, Han KH, Park SJ, Shin JI. Smoking and rheumatoid arthritis. Int J Mol Sci 2014;15:22279–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Christiani DC. Vaping‐induced lung injury. N Engl J Med 2020;382:960–2. [DOI] [PubMed] [Google Scholar]
- 8. Rotermann M. What has changed since cannabis was legalized? Health Rep 2020;31:11–20. [DOI] [PubMed] [Google Scholar]
- 9. Statistics Canada . National cannabis survey. 2019. URL: https://www.canada.ca/en/health-canada/services/drugsmedication/cannabis/research-data/medical-purpose.html.
- 10. Government of Canada . Data on cannabis for medical purposes. 2019. URL: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey%26SDDS=5262.
- 11. Grella CE, Rodriguez L, Kim T. Patterns of medical marijuana use among individuals sampled from medical marijuana dispensaries in los angeles. J Psychoactive Drugs 2014;46:267–75. [DOI] [PubMed] [Google Scholar]
- 12. Harris D, Jones RT, Shank R, Nath R, Fernandez E, Goldstein K, et al. Self‐reported marijuana effects and characteristics of 100 San Francisco medical marijuana club members. J Addict Dis 2000;19:89–103. [DOI] [PubMed] [Google Scholar]
- 13. Ilgen MA, Bohnert K, Kleinberg F, Jannausch M, Bohnert AS, Walton M, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend 2013;132:654–9. [DOI] [PubMed] [Google Scholar]
- 14. Lucas P, Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: a survey of authorized medical cannabis patients. Int J Drug Policy 2017;42:30–5. [DOI] [PubMed] [Google Scholar]
- 15. Nunberg H, Kilmer B, Pacula RL, Burgdorf J. An analysis of applicants presenting to a medical marijuana specialty practice in California. J Drug Policy Anal 2011;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zaller N, Topletz A, Frater S, Yates G, Lally M. Profiles of medicinal cannabis patients attending compassion centers in rhode island. J Psychoactive Drugs 2015;47:18–23. [DOI] [PubMed] [Google Scholar]
- 17. Walsh Z, Callaway R, Belle‐Isle L, Capler R, Kay R, Lucas P, et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy 2013;24:511–6. [DOI] [PubMed] [Google Scholar]
- 18. Abuhasira R, Schleider LB, Mechoulam R, Novack V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. Eur J Intern Med 2018;49:44–50. [DOI] [PubMed] [Google Scholar]
- 19. Kalant H. Adverse effects of cannabis on health: an update of the literature since 1996. Prog Neuropsychopharmacol Biol Psychiatry 2004;28:849–63. [DOI] [PubMed] [Google Scholar]
- 20. National Academies of Sciences, Engineering, and Medicine . The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington (DC): The National Academies Press; 2017. [PubMed] [Google Scholar]
- 21. Krcevski‐Skvarc N, Wells C, Hauser W. Availability and approval of cannabis‐based medicines for chronic pain management and palliative/supportive care in Europe: a survey of the status in the chapters of the European Pain Federation. Eur J Pain 2018;22:440–54. [DOI] [PubMed] [Google Scholar]


