ABSTRACT
Excess salt intake contributes to hypertension and increased cardiovascular disease risk. Efforts to implement effective salt-reduction strategies require accurate data on the sources of salt consumption. We therefore performed a systematic review to identify the sources of dietary salt around the world. We systematically searched peer-reviewed and gray literature databases for studies that quantified discretionary (salt added during cooking or at the table) and nondiscretionary sources of salt and those that provided information about the food groups contributing to dietary salt intake. Exploratory linear regression analysis was also conducted to assess whether the proportion of discretionary salt intake is related to the gross domestic product (GDP) per capita of a country. We identified 80 studies conducted in 34 countries between 1975 and 2018. The majority (n = 44, 55%) collected data on dietary salt sources within the past 10 y and were deemed to have a low or moderate risk of bias (n = 75, 94%). Thirty-two (40%) studies were judged to be nationally representative. Populations in Brazil, China, Costa Rica, Guatemala, India, Japan, Mozambique, and Romania received more than half of their daily salt intake from discretionary sources. A significant inverse correlation between discretionary salt intake and a country's per capita GDP was observed (P < 0.0001), such that for every $10,000 increase in per capita GDP, the amount of salt obtained from discretionary sources was lower by 8.7% (95% CI: 5.1%, 12%). Bread products, cereal and grains, meat products, and dairy products were the major contributors to dietary salt intake in most populations. There is marked variation in discretionary salt use around the world that is highly correlated with the level of economic development. Our findings have important implications for the type of salt-reduction strategy likely to be effective in a country.
Keywords: salt, sodium, blood pressure, hypertension, salt-reduction, food policy, nutrition
Introduction
Hypertension-related cardiovascular disease is a leading cause of mortality and morbidity worldwide (1). A diet high in salt is one of the leading risk factors for high blood pressure. A Cochrane review of salt-reduction studies with a duration of ≥4 wk found that a reduction of 4.4 g in daily salt intake led to a decrease in blood pressure of 5.4/2.8 mm Hg in hypertensive individuals and 2.4/1.0 mm Hg in normotensive individuals (2). A more recent Cochrane review observed a reduction in blood pressure of 5.02/2.78 mm Hg in hypertensive individuals and 1.08/0.24 mm Hg in normotensive individuals (3). Despite the observed relation between salt intake and blood pressure, the health effects of salt intake continue to be debated (4). While most studies report a direct, progressive association between 24-h urinary salt excretion and all-cause mortality (5), others suggest a U- or J-shaped relation between morning fasting urinary salt and cardiovascular events (6), although inaccurate estimation of salt intake is a potential contributor to the J-shaped findings reported in such cohort studies (7, 8). Based on modelling data, approximately 3 million deaths and 70 million disability-adjusted life-years lost every year have been estimated to be due to excess salt consumption (9). Considering the strengths and limitations of available data, many scientists have concluded that excess salt consumption is harmful to health (10), and major health organizations and most governments around the world are actively implementing strategies to reduce population salt consumption (11).
The recent modelling estimates from the Global Burden of Disease data suggest a daily average salt intake in adults of 14 g (9), nearly 3 times the WHO's recommended intake of 5 g (14). Other studies have estimated lower intakes at 9–10 g/d (12, 13), which still substantially exceed WHO recommendations. Despite efforts to tackle the high dietary intake of salt across the globe (11, 15, 16), progress on this front remains slow. A variety of salt-reduction interventions exist, ranging from structural approaches such as taxation and reformulation, to individual-focused measures such as health education (11). Understanding the main sources of dietary salt in a country can help guide the choice of salt-reduction strategies that are most effective, equitable, rapid, and cost-saving (17). In particular, the proportion of dietary salt that is obtained from home cooking versus foods made outside the home is an important consideration, as interventions targeted to the more common pattern of salt consumption are likely to be most effective. For instance, reformulation strategies are likely to be more effective in countries where a large proportion of dietary salt comes from packaged foods and food prepared outside the home, whereas salt substitution may be more effective in countries where there is extensive use of discretionary salt.
At present, there are no reviews quantifying the sources of dietary salt globally. Our aim was therefore to conduct a systematic review of the literature to identify the sources of dietary salt in all countries with available data. Our study was conducted under the premise that salt reduction is not only possible but also beneficial (18). We hypothesized that the majority of dietary salt in high-income nations would be obtained from packaged foods and meals eaten outside the home and in low- and middle-income countries from salt added during cooking or at the table.
Methods
Search strategy
A systematic search of peer-reviewed and gray literature published up to 8 February 2019 was conducted. The systematic review followed the PRISMA guidelines; a protocol for the study has not previously been published. The following databases since their inception were used: MEDLINE, EMBASE, Scopus, TRoPHI, LILACS, Central, Cinahl Plus, Global Health, Allied and Complementary Medicine Database, and the WHO International Clinical Trials Registry Platform. Detailed search terms used are provided in the Supplemental Methods and included “diet*,” “sodium” or “salt,” and “source*” or “intake” or “ingest*” or “consum*” or “survey” and “food” or “cook” or “product*” or “add*” or “table” or “discretionary.” Only studies published in English and Spanish were included, and no studies published in other languages were identified. Reference lists of eligible studies were scanned to identify additional relevant publications. In parallel, a search using these terms was conducted in OpenGrey, WHO, World Action on Salt and Health, and Institute of Medicine databases to identify pertinent gray literature.
Inclusion and exclusion criteria
All studies that provided 1) quantitative estimates of discretionary and nondiscretionary sources of salt or 2) information about the various food groups contributing to dietary salt intake were included. For intervention studies, only baseline data on dietary salt sources were included. Exclusion criteria included studies in pregnant women, those investigating the amount of salt consumed by a population without quantification of the dietary sources, and commentaries and opinions. Articles were not excluded because of age, sex, study design, sample size, sampling methodology, or geographical location. Titles and abstracts of retrieved articles were evaluated by 1 investigator (SB) who was not blinded to authors, institutions, or manuscript journals. If an abstract did not provide adequate information about inclusion and exclusion criteria, the full text was evaluated to determine study eligibility.
Data extraction
Titles and abstracts identified in the initial search (n = 5542) were screened, and studies that did not meet the inclusion and exclusion criteria were excluded (n = 5409). Full texts of the remaining studies (n = 133) were obtained and screened again based on the inclusion and exclusion criteria. An electronic data extraction form was used to extract relevant data from the remaining included studies (74 peer-reviewed and 6 gray literature sources) (Figure 1). Key data extracted included the following: geographical location of the study, years of data collection, method of dietary salt assessment, sample size, average age, percentage of dietary salt obtained from discretionary versus nondiscretionary sources, and contribution of different food groups to dietary salt intake. Discretionary salt intake was defined as salt added to food during preparation at home or at the table. Full-text screening and data extraction were performed by 2 investigators (SB and MM), with any disagreements resolved by discussion to reach consensus.
FIGURE 1.
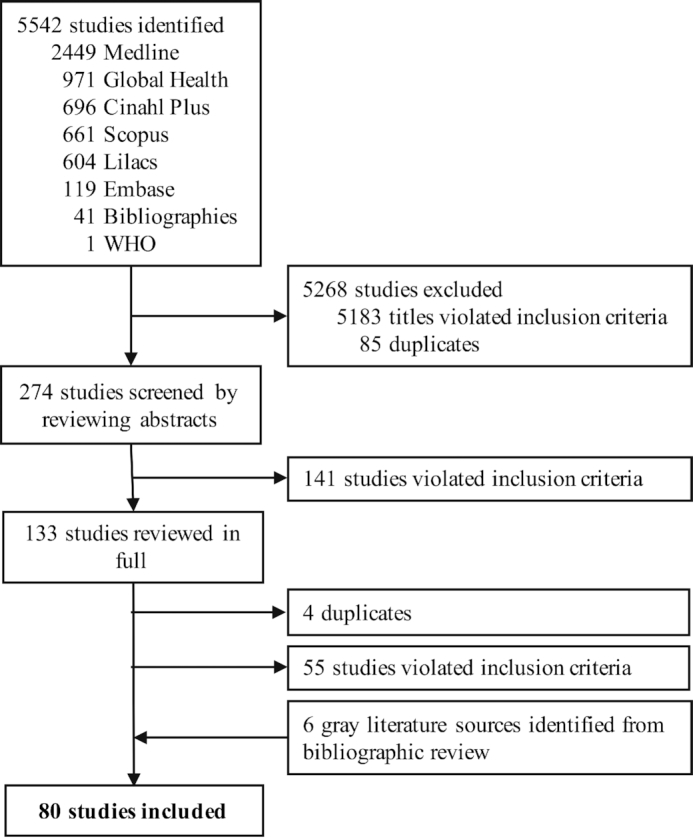
Flow diagram for the screening and inclusion of publications in the systematic review that investigated the sources of dietary salt.
The following major food groups were included in our data extraction as they were commonly reported across studies and were major contributors to salt intake: “bread and bakery products”; “beverages (nonalcoholic)”; “cereal and grain products”; “confectionary”; “convenience foods”; “dairy”; “eggs”; “meat and meat alternatives”; “oils and oil emulsions”; “sauces, dressings, spreads and dips”; “seafood and seafood products”; “snack foods”; “sugars, honey and related products”; “vegetables, fruits, nuts, and legumes”; and “other.” In instances where reported sources of salt overlapped with ≥2 categories listed above, or in instances where discrete categories could not be delineated, the values were reported under the category that likely contributed most to the daily salt intake, based on similar studies available in that country. For example, if a study reported that 30% of daily salt was obtained from bread and bakery products and cereal and grain products combined, and if other studies from that country showed that bread and bakery products contributed to daily salt intake more than cereal and grain products, then this 30% contribution to daily salt intake was reported under the “bread and bakery products” category. If sodium intake (milligrams per day) was reported, it was converted to salt (grams per day) by dividing by 1000 and multiplying by 2.54 [the ratio of the molecular weight of sodium chloride (58.44) to the molecular weight of sodium (23)].
Study quality assessment
The quality of each study was assessed by 3 parameters: relevance, representativeness, and risk of bias. Relevance was ascertained by how recently the data were collected, and studies fit into 1 of 4 categories: “within the past 5 years,” “between 5 and 10 years ago,” “between 10 and 15 years ago,” and “more than 15 years ago.” Relevance to the modern context was deemed to be an appropriate index of quality given the rapid nutrition transition occurring in many developing nations that is associated with changes in dietary patterns and therefore sources of dietary salt (19, 20). The representativeness, and hence generalizability, of the data in each study was judged to fit into 1 of 5 categories: “probably representative of the national population,” “probably representative of a subnational population,” “probably representative of urban regions,” “probably representative of rural regions,” and “probably not representative.” In this classification scheme, “subnationally representative” implies characteristic of a state or region within a country. To determine the risk of bias, we adapted a tool for cross-sectional studies developed by Hoy and colleagues (21) and scored the studies as having “low,” “moderate,” or “high” risk of bias. The tool evaluated each study's methodology by assessing, among other things, the sampling technique and internal validity (21). Studies with scores of 0 to 2 were judged as having a low risk of bias, 3 to 5 as having a moderate risk of bias, and 6 to 7 as having a high risk of bias.
Data analysis
Given the large variability in methodologies and the heterogeneity of populations studied within a country, no meta-analysis was performed to obtain pooled estimates across studies. Exploratory linear regression analysis was conducted to assess whether the level of discretionary salt intake is related to the level of economic development between countries, assessed by the annual gross domestic product (GDP) per capita. For this analysis, as well as for determining the discretionary salt intake and sources of salt in a country, if multiple estimates from different studies were available for a country, 1 study was chosen according to the following hierarchy: 1) the study was representative of the national population, 2) the study had the most recent available data, and 3) the study had the lowest risk of bias. For instance, if no nationally representative data were available for a country, then the study with the most recent available data was chosen. The GDP data for each country were obtained from the World Bank website (https://data.worldbank.org/) for the year of data collection.
Data are presented as means  SDs unless stated otherwise. World maps were created using Excel (Microsoft; 2018). All statistical analyses were performed in Prism 6 (GraphPad Software, Inc; 2015).
SDs unless stated otherwise. World maps were created using Excel (Microsoft; 2018). All statistical analyses were performed in Prism 6 (GraphPad Software, Inc; 2015).
Results
Study characteristics
The 80 included studies (22–101) were conducted between 1975 and 2018 and represented 34 countries across 6 continents (Supplemental Table 1). Forty-four studies (55%) collected data on dietary salt sources within the past 10 y; 33 studies (41%) had data >10 y old, and 3 studies (4%) did not provide information about when data were collected (Table 1). Only 32 (40%) studies were judged to be nationally representative, whereas close to half of all studies (n = 38, 48%) were deemed to be not representative of any particular population groups (Table 1). While most studies were conducted in adults aged ≥18 y (n = 40, 50%), some were conducted exclusively in children and adolescents (n = 12, 15%) and generally included both males and females (n = 48, 56%). The sample size ranged from as few as 20 individuals to >1 million. The majority of studies had low (n = 32, 40%) or moderate (n = 43, 54%) risk of bias, with only 3 studies (3.8%) having a high risk of bias (Table 1, Supplemental Table 2).
TABLE 1.
Summary of the quality-assessment metrics for included studies investigating the sources of dietary salt across the globe1
| Continent | |||||||
|---|---|---|---|---|---|---|---|
| Africa | Asia | Europe | North America | Oceania | South America | Total | |
| Year of data collection | |||||||
| Last 5 y | 0 | 5 | 3 | 2 | 0 | 1 | 11 |
| 5–10 y ago | 1 | 7 | 9 | 6 | 7 | 3 | 33 |
| 10–15 y ago | 0 | 0 | 2 | 7 | 4 | 0 | 13 |
| >15 y ago | 1 | 4 | 6 | 6 | 0 | 1 | 18 |
| Missing | 0 | 1 | 1 | 0 | 1 | 0 | 3 |
| Total | 2 | 17 | 21 | 21 | 12 | 5 | 78 |
| Representativeness | |||||||
| National | 0 | 6 | 7 | 11 | 5 | 2 | 31 |
| Subnational | 0 | 2 | 0 | 0 | 0 | 1 | 3 |
| Urban | 1 | 2 | 0 | 1 | 1 | 1 | 6 |
| Rural | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Not representative | 1 | 6 | 14 | 9 | 6 | 1 | 37 |
| Total | 2 | 17 | 21 | 21 | 12 | 5 | 78 |
| Risk of bias | |||||||
| Low risk | 0 | 8 | 7 | 8 | 4 | 4 | 31 |
| Moderate risk | 2 | 9 | 13 | 10 | 8 | 0 | 42 |
| High risk | 0 | 0 | 1 | 1 | 0 | 1 | 3 |
| Unknown risk | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Total | 2 | 17 | 21 | 21 | 12 | 5 | 78 |
Discretionary salt intake
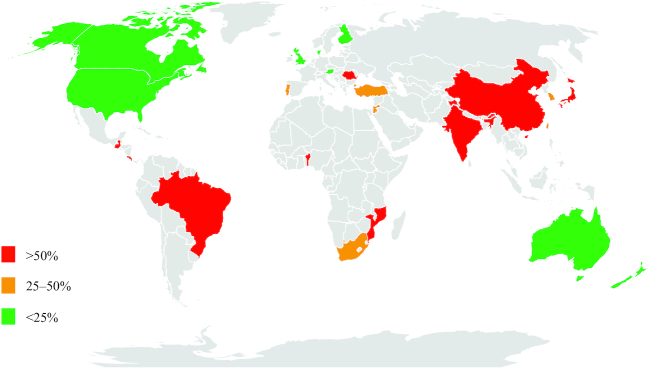
Thirty-three studies provided an estimate of discretionary salt intake (Supplemental Table 3). The average daily salt intake of adults in these studies ranged from 5.2 to 15.5g/day. The % of discretionary salt intake classified into three categories (low, <25%; medium, 25–50%; and high, >50%) is shown in Figure 2, and detailed quantitative estimates are provide in Supplemental Table 3. Populations in Brazil, China, Costa Rica, Guatemala, India, Japan, Mozambique, Romania and possibly Benin appear to obtain more than half of their daily salt during cooking or at the table. Populations in Jordan, Portugal, South Korea, Taiwan, and Turkey appear to receive between 25 and 50% of their daily salt from discretionary sources. On the other hand, discretionary salt intake in Australia, Austria, Canada, Denmark, Finland, New Zealand, the United Kingdom, and the United States of America accounts for less than 25% of daily salt intake.
FIGURE 2.
Contribution of discretionary sources to total dietary salt intake around the globe. Green, <25% of dietary salt from discretionary sources; amber, 25–50% of dietary salt from discretionary sources; red, >50% of dietary salt from discretionary sources. No published data were available for countries shaded in gray. Values for discretionary salt intake are given in Supplemental Table 3.
Exploratory analysis of discretionary salt intake as a function of economic development
An inverse correlation was observed between the GDP per capita of a country and the proportion of daily salt intake from discretionary sources, such that for every $10,000 GDP per capita, the proportion of daily salt obtained from discretionary sources was lower by approximately 8.7% (95% CI 5.1% to 12%) (Figure 3).
FIGURE 3.
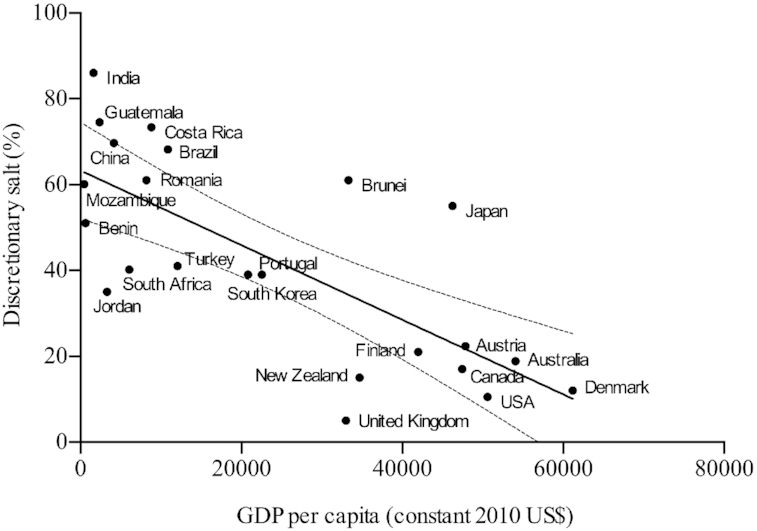
Daily discretionary salt intake (% of total salt intake) as a function of per capita GDP. The per capita GDP figures, expressed in constant 2010 US dollars, were obtained for the year when data were collected for each study. A statistically significant linear regression fit (solid line) was found (F = 25.3, P < 0.0001) with an R2 of 0.55 and slope equal to −0.00087 (95% CI: −0.0012, −0.00051). The 95% CI of the regression line in depicted by the dashed lines. GDP, gross domestic product.
Sources of salt
The proportion of dietary salt from various food groups across countries and studies is provided in Supplemental Table 4 and depicted in Supplemental Figure 1. Individual food groups contributing to daily salt intake in countries for which data were available are shown in more detail in Supplemental Figure 2. Some food groups, including bread and bakery products, cereals and grains, meat products, and dairy products were found to be significant contributors to daily salt intake across multiple countries and continents. In many European countries and the USA, the proportion of daily salt from bread or bakery products ranged from 25 to 40%. Cereals and grains contributed up to 24% of daily salt intake, with highest levels noted in China and Brazil. Meat products provided up to 31% of daily salt in the USA; meat also provided a substantial source of daily salt in some European and South American countries, and in Australia and New Zealand (range 4 to 16%). Dairy products accounted for up to 15% of daily salt intake in Argentina and New Zealand, and between 1 and 13% in other countries. A significant proportion of salt (44%) came from sauces and dressings in Japan, a finding unique within the countries with data available for this analysis.
Discussion
In this systematic review, we found that only 34 countries had data on dietary salt intake patterns and of these, only 24 had data on discretionary salt intake. The proportion of salt entering the diet from discretionary sources varied substantially between countries and continents. We identified countries where discretionary salt represents a large proportion of overall daily salt intake, including Brazil, China, Costa Rica, Guatemala, India, Japan, Mozambique, and Romania. Exploratory analyses suggest a strong inverse relation between the proportion of salt obtained from discretionary sources and a country's per capita GDP. While there were no obvious regional patterns in the food sources of dietary salt, bread and bakery products, cereal and grain products, meat products, and dairy products appeared to be the main global contributors to daily salt intake.
Key strengths of the study include its comprehensive search strategy, the large number of studies identified and included, the diversity of countries represented, and the overall low or moderate risk of bias of the included studies. This study builds on the systematic review by Menyanu et al. (102) that reported the contribution of selected food categories to daily salt intake in 7 low- and middle-income countries. In addition to providing a more up-to-date review on the topic, our study extends the findings of Menyanu et al. by including globally available data encompassing a greater number of countries, quantifying the proportion of dietary salt from discretionary versus nondiscretionary sources, identifying individual dietary categories contributing to daily salt intake, and assessing the quality of the available data.
Effective population-level salt reduction is likely to require implementation of multifaceted strategies tailored to a local context (103). Salt-reduction policies exist on a spectrum from interventions targeted at individuals, such as dietary advice and education campaigns, to structural approaches, such as product reformulation and salt substitution, and economic regulations, such as taxation (11). Our results, by providing a comprehensive and up-to-date “map” of current evidence related to the dietary sources of salt, highlight gaps in the data and may also aid policymakers to direct limited resources toward the predominant dietary salt source in a given setting. Food-reformulation policies and efforts have been consistently targeted towards bread, meat, dairy, sauces and dressings, and convenience foods in many countries, an approach supported by our findings (104, 105). Furthermore, increasing the availability of salt substitutes or reducing their costs is likely to be appropriate in countries where discretionary salt intake is high, to facilitate the use of these products in daily cooking (106–108). Our findings identified a specific set of countries with a high discretionary salt intake where more widespread use of salt substitutes may be prioritized. Additional research in these countries should also further evaluate the potential of salt substitutes to lower blood pressure.
Our exploratory analysis suggested an association between a country's economic development and the discretionary salt intake of its population, possibly capturing the effect of nutrition transition on changing salt-consumption behaviors (109). Most of the urban middle-class population in India, for example, have more access to a variety of convenience foods including processed, ready-to-eat foods as they undergo a rapid epidemiologic, demographic, and nutrition transition (107, 110, 111). Our findings highlight the potential to use a country's per capita GDP to impute its population's discretionary salt intake, although such an approach will require further validation in a larger dataset.
Several limitations of the study should be noted. Many countries lacked recent studies, and those that collected data >10 y ago may have limited relevance to the modern context. This is important given the rapid nutrition transitions, changing lifestyles and dietary trends, and implementation of new and updated food policy initiatives (19, 109–112). The majority of the identified studies did not assess salt consumption among nationally representative samples. While this might be viewed as reducing the generalizability of the findings at first glance, from a policy and intervention perspective it might be more important to understand the sources of salt by region (e.g., north versus south India). The results from the preliminary association analysis with a country's GDP should be interpreted cautiously given the potential for ecologic bias; the results could be confounded by factors such as varying methodologies (e.g., dietary recall, lithium-labelling), demographic characteristics, and representativeness of the populations studied within and between countries. Another limitation of the present study is the substantial variation in how different investigators categorized various foods, making it difficult to directly compare food categories within and between countries. Given the lack of readily available demographic data for many studies and variable representativeness of the populations studied, we were unable to perform secondary analyses of salt intakes for subpopulations within each country. Finally, some recent reports have challenged the widely held view of most major health organizations and governments of the health benefits of salt reduction (6, 113). Our study does not attempt to address this ongoing controversy; rather, it was conducted to identify key sources of dietary salt across the globe to help guide the design and implementation of salt-reduction policies. Our study was based on the premise that population salt-reduction interventions are possible and likely to reduce hypertension and cardiovascular disease burden.
A number of research recommendations emerge from this review. More studies are needed that incorporate nationally representative populations. Researchers should also aim to deploy more consistent methods—for instance, related to dietary survey methods and categorization of foods—to provide a more harmonized view of the landscape of salt consumption across the globe. While low- and middle-income countries suffer the highest prevalence and burden of hypertension (114), our findings suggest that data related to dietary sources of salt are particularly lacking in these counties, which should be urgently addressed in future studies. Emerging evidence has identified specific neurons in the control of salt appetite regulation (115). These findings indicate the need for additional investigations to assess the relative influence of endogenous regulatory pathways and the external food environment on salt-consumption behavior, which will determine the likelihood of success of policies targeting the reduction of salt intake.
To our knowledge, this is the first systematic review investigating the sources of dietary salt across the globe. This study identified countries where more than half of the daily salt intake comes from salt added during cooking or at the table, including Brazil, China, Costa Rica, Guatemala, India, Japan, Mozambique, and Romania. Globally, bread and bakery products, cereal and grain products, meat, and dairy products appear to be the main contributors to daily salt intake and represent key food groups that should be targeted for salt-reformulation efforts.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—SB and MM: conducted the research; SB: analyzed the data and had primary responsibility for final content; SB, MM, and JHW: drafted the manuscript; and all authors: provided critical review and feedback for the manuscript, contributed to the research design, and read and approved the final manuscript.
Notes
MEH and LJA received support from Resolve to Save Lives from Vital Strategies.
Author disclosures: The authors report no conflicts of interest.
Supplemental Methods, Supplemental Tables 1–4, and Supplemental Figures 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
References
- 1. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF et al.. Global burden of hypertension and systolic blood pressure of at least 110 to 115mm Hg, 1990–2015. JAMA. 2017;317(2):165–82. [DOI] [PubMed] [Google Scholar]
- 2. He FJ, Li JF, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 3. Graudal NA, Hubeck‐Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022 doi:10.1002/14651858.CD004022.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trinquart L, Johns DM, Galea S. Why do we think we know what we know? A metaknowledge analysis of the salt controversy. Int J Epidemiol. 2016;45(1):251–60. [DOI] [PubMed] [Google Scholar]
- 5. Cook NR, Appel LJ, Whelton PK. Sodium intake and all-cause mortality over 20 years in the trials of hypertension prevention. J Am Coll Cardiol. 2016;68(15):1609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mente A, O'Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, Lear S, Ah STL, Wei L, Diaz R et al.. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392(10146):496–506. [DOI] [PubMed] [Google Scholar]
- 7. He FJ, Campbell NRC, Ma Y, MacGregor GA, Cogswell ME, Cook NR. Errors in estimating usual sodium intake by the Kawasaki formula alter its relationship with mortality: implications for public health. Int J Epidemiol. 2018;47(6):1784–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. He FJ, Ma Y, Campbell NRC, MacGregor GA, Cogswell ME, Cook NR. Formulas to estimate dietary sodium intake from spot urine alter sodium-mortality relationship. Hypertension. 2019;74(3):572–80. [DOI] [PubMed] [Google Scholar]
- 9. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. He FJ, MacGregor GA.. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15(6):371–7. [DOI] [PubMed] [Google Scholar]
- 11. Trieu K, Neal B, Hawkes C, Dunford E, Campbell N, Rodriguez-Fernandez R, Legetic B, McLaren L, Barberio A, Webster J. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One. 2015;10(7):e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens. 2013;26(10):1218–23. [DOI] [PubMed] [Google Scholar]
- 13. Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi PL, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D et al.. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization. Guideline: sodium intake for adults and children. Geneva (Switzerland): World Health Organization; 2012. [PubMed] [Google Scholar]
- 15. World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva (Switzerland): World Health Organization; 2013. [Internet] [cited 2019 Oct 6].Available from: https://www.who.int/nmh/publications/ncd-action-plan/en/. [Google Scholar]
- 16. World Health Organization. The Thirteenth General Programme of Work, 2019–2023. Geneva (Switzerland): World Health Organization; 2018. [Internet] [cited 2019 Oct 6].Available from: https://www.who.int/about/what-we-do/thirteenth-general-programme-of-work-2019-2023. [Google Scholar]
- 17. Frieden TR, Bloomberg MR.. Saving an additional 100 million lives. Lancet. 2018;391(10121):709–12. [DOI] [PubMed] [Google Scholar]
- 18. He FJ, Brown M, Tan M, MacGregor GA. Reducing population salt intake—an update on latest evidence and global action. J Clin Hypertens. 2019;21(10):1596–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Misra A, Singhal N, Sivakumar B, Bhagat N, Jaiswal A, Khurana L. Nutrition transition in India: secular trends in dietary intake and their relationship to diet-related non-communicable diseases. J Diabetes. 2011;3(4):278–92. [DOI] [PubMed] [Google Scholar]
- 20. Ibrahim MM. Hypertension in developing countries: a major challenge for the future. Curr Hypertens Rep. 2018;20(5):38. [DOI] [PubMed] [Google Scholar]
- 21. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. [DOI] [PubMed] [Google Scholar]
- 22. Melse-Boonstra A, Rozendaal M, Rexwinkel H, Gerichhausen MJ, van den Briel T, Bulux J, Solomons NW, West CE. Determination of discretionary salt intake in rural Guatemala and Benin to determine the iodine fortification of salt required to control iodine deficiency disorders: studies using lithium-labeled salt. Am J Clin Nutr. 1998;68(3):636–41. [DOI] [PubMed] [Google Scholar]
- 23. Queiroz A, Damasceno A, Jessen N, Novela C, Moreira P, Lunet N, Padrao P. Urinary sodium and potassium excretion and dietary sources of sodium in Maputo, Mozambique. Nutrients. 2017;9(8):830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Charlton KE, Steyn K, Levitt NS, Zulu JV, Jonathan D, Veldman FJ, Nel JH. Diet and blood pressure in South Africa: intake of foods containing sodium, potassium, calcium, and magnesium in three ethnic groups. Nutrition. 2005;21(1):39–50. [DOI] [PubMed] [Google Scholar]
- 25. Kamis Z, Idros RA, Tamin S, Yaakub R, Rahman IA, King OS, Kassim N. Dietary sources of sodium and socio-demographics correlate of sodium intake in Brunei Darussalam using 24 hours urinary sodium excretion. Brunei Intl Med J. 2016;12(2):60–9. [Google Scholar]
- 26. Anderson CAM, Appel LJ, Okuda N, Brown IJ, Chan QE, Zhao LC, Ueshima H, Kesteloot H, Miura K, Curb JD et al.. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110(5):736–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99(2):334–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Liu Z, Ho SC, Tang N, Chan R, Chen Y, Woo J. Urinary sodium excretion and dietary sources of sodium intake in Chinese postmenopausal women with prehypertension. PLoS One. 2014;9(8):e104018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tian HG, Hu G, Dong QN, Yang XL, Nan Y, Pietinen P, Nissinen A. Dietary sodium and potassium, socioeconomic status and blood pressure in a Chinese population. Appetite. 1996;26(3):235–46. [DOI] [PubMed] [Google Scholar]
- 30. Zhao F, Zhang P, Zhang L, Niu W, Gao J, Lu L, Liu C, Gao X. Consumption and sources of dietary salt in family members in Beijing. Nutrients. 2015;7(4):2719–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Johnson C, Santos AJ, Sparks E, Raj ST, Mohan S, Garg V, Rogers K, Maulik KP, Prabhakaran D, Neal B et al.. Sources of dietary salt in north and south India estimated from 24 hour dietary recall. Nutrients. 2019;11(2):318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nair S, Bandyopadhyay S.. Sodium intake pattern in West Indian population. Indian J Community Med. 2018;43(2):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ravi S, Bermudez OI, Harivanzan V, Kenneth Chui KH, Vasudevan P, Must A, Thanikachalam S, Thanikachalam M. Sodium intake, blood pressure, and dietary sources of sodium in an adult south Indian population. Ann Glob Health. 2016;82(2):234–42. [DOI] [PubMed] [Google Scholar]
- 34. Asakura K, Uechi K, Masayasu S, Sasaki S. Sodium sources in the Japanese diet: difference between generations and sexes. Public Health Nutr. 2016;19(11):2011–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Okuda N, Okayama A, Miura K, Yoshita K, Saito S, Nakagawa H, Sakata K, Miyagawa N, Chan Q, Elliott P et al.. Food sources of dietary sodium in the Japanese adult population: the International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Eur J Nutr. 2017;56(3):1269–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shimbo S, Imai Y, Yasumoto M, Yamamoto K, Kawamura S, Kimura K, Watanabe T, Sato R, Iwami O, Ikeda M. Quantitative identification of sodium chloride sources in Japanese diet by 24-hour total food duplicate analysis. J Epidemiol. 1993;3(2):77–82. [Google Scholar]
- 37. Takimoto H, Saito A, Htun NC, Abe K. Food items contributing to high dietary salt intake among Japanese adults in the 2012 National Health and Nutrition Survey correspondence. Hypertens Res. 2018;41(3):209–12. [DOI] [PubMed] [Google Scholar]
- 38. Al-Wa'l T, Takruri H.. Sodium and potassium intakes in a sample of students and employees in the University of Jordan aged (20–40 years) using 3-day food diaries. Nutr Food Sci. 2016;46(1):43–50. [Google Scholar]
- 39. Lee HS, Duffey KJ, Popkin BM. Sodium and potassium intake patterns and trends in South Korea. J Hum Hypertens. 2013;27(5):298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Song DY, Park JE, Shim JE, Lee JE. Trends in the major dish groups and food groups contributing to sodium intake in the Korea National Health and Nutrition Examination Survey 1998–2010. Korean J Nutr. 2013;46(1):72–85. [Google Scholar]
- 41. Wu SJ, Chang YH, Chang HY, Pan WH. Food sources of dietary calcium, phosphorus, iron, and sodium: Nutrition and Health Survey in Taiwan (NAHSIT) 1993–1996. Nutr Sci J. 2001;26(3):142–58. [Google Scholar]
- 42. Erdem Y, Akpolat T, Derici Ü, Şengül Ş, Ertürk Ş, Ulusoy Ş, Altun B, Arıcı M. Dietary sources of high sodium intake in Turkey: SALTURK II. Nutrients. 2017;9(9):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hasenegger V, Rust P, Konig J, Purtscher AE, Erler J, Ekmekcioglu C. Main sources, socio-demographic and anthropometric correlates of salt intake in Austria. Nutrients. 2018;10(3):311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Andersen L, Rasmussen LB, Larsen EH, Jakobsen J. Intake of household salt in a Danish population. Eur J Clin Nutr. 2009;63(5):598–604. [DOI] [PubMed] [Google Scholar]
- 45. Eloranta AM, Venalainen T, Soininen S, Jalkanen H, Kiiskinen S, Schwab U, Lakka TA, Lindi V. Food sources of energy and nutrients in Finnish girls and boys 6–8 years of age—the PANIC study. Food Nutr Res. 2016;60:32444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pietinen P. Sources of sodium in the Finnish diet. Agr Food Sci. 1981;53(5):275–84. [Google Scholar]
- 47. Reinivuo H, Valsta LM, Laatikainen T, Tuomilehto J, Pietinen P. Sodium in the Finnish diet: II. Trends in dietary sodium intake and comparison between intake and 24-h excretion of sodium. Eur J Clin Nutr. 2006;60(10):1160–7. [DOI] [PubMed] [Google Scholar]
- 48. Meneton P, Lafay L, Tard A, Dufour A, Ireland J, Menard J, Volatier JL. Dietary sources and correlates of sodium and potassium intakes in the French general population. Eur J Clin Nutr. 2009;63(10):1169–75. [DOI] [PubMed] [Google Scholar]
- 49. Magriplis E, Farajian P, Pounis GD, Risvas G, Panagiotakos DB, Zampelas A. High sodium intake of children through ‘hidden’ food sources and its association with the Mediterranean diet: the GRECO study. J Hypertens. 2011;29(6):1069–76. [DOI] [PubMed] [Google Scholar]
- 50. Seidler T, Ksiazek J, Sobczak A. Determining levels of mineral consumption from foodstuff sources in the daily diets of adolescent students living in Kamien Pomorski: a pilot study. Rocz Panstw Zakl Hig. 2013;64(4):309–15. [PubMed] [Google Scholar]
- 51. Polonia JJ, Magalhaes MT, Senra D, Barbosa L, Silva JA, Ribeiro SM. Association of 24-h urinary salt excretion with central haemodynamics and assessment of food categories contributing to salt consumption in Portuguese patients with hypertension. Blood Press Monit. 2013;18(6):303–10. [DOI] [PubMed] [Google Scholar]
- 52. Goncalves C, Abreu S, Padrao P, Pinho O, Graca P, Breda J, Santos R, Moreira P. Sodium and potassium urinary excretion and dietary intake: a cross-sectional analysis in adolescents. Food Nutr Res. 2016;60:29442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Soptica F, Ciric AI, Niculita P, Zugravu CA. Consumption volume and salt levels call for substantive reformulation action on Romania's foremost staple food: bread. Ann Food Sci Technol. 2012;13(2):223–30. [Google Scholar]
- 54. Jovičić-Bata J, Grujičić M, Rađen S, Novaković B. Sodium intake and dietary sources of sodium in a sample of undergraduate students from Novi Sad, Serbia. Vojnosanitetski Pregled. 2016;73(7):651–6. [DOI] [PubMed] [Google Scholar]
- 55. Ribic CH, Zakotnik JM, Seljak BK, Policnik R, Blaznik U, Mis NF, Eržen I, Ji C, Cappucio FP. Estimation of sodium availability in food in Slovenia: results from household food purchase data from 2000 to 2009. Zdravstveno Varstvo. 2014;53(2):209–19. [Google Scholar]
- 56. Cuadrado-Soto E, Peral-Suarez A, Aparicio A, Perea JM, Ortega RM, Lopez-Sobaler AM. Sources of dietary sodium in food and beverages consumed by Spanish schoolchildren between 7 and 11 years old by the degree of processing and the nutritional profile. Nutrients. 2018;10(12):E1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Guallar-Castillon P, Munoz-Pareja M, Aguilera MT, Leon-Munoz LM, Rodriguez-Artalejo F. Food sources of sodium, saturated fat and added sugar in the Spanish hypertensive and diabetic population. Atherosclerosis. 2013;229(1):198–205. [DOI] [PubMed] [Google Scholar]
- 58. Mesias M, Seiquer I, Navarro MP. Ingesta de sodio en la dieta de un colectivo de adolescentes [Sodium intake in the diet of a group of adolescents]. Ars Pharmaceutica. 2010;51(Suppl 3):145–52. [Google Scholar]
- 59. Rios-Leyvraz M, Bovet P, Bochud M, Genin B, Russo M, Rossier MF, Tabin R, Chiolero A. Estimation of salt intake and excretion in children in one region of Switzerland: a cross-sectional study. Eur J Nutr. 2019;58(7):2921–8. [DOI] [PubMed] [Google Scholar]
- 60. Farrimond S, Ainsworth P, Piper B. The contribution of discretionary salt to total salt intake. J Consum Stud Home Econ. 1995;19(2):135–43. [Google Scholar]
- 61. Marrero NM, He FJ, Whincup P, MacGregor GA. Salt intake of children and adolescents in South London: consumption levels and dietary sources. Hypertension. 2014;63(5):1026–32. [DOI] [PubMed] [Google Scholar]
- 62. Sanchez-Castillo CP, Warrender S, Whitehead TP, James WP. An assessment of the sources of dietary salt in a British population. Clin Sci. 1987;72(1):95–102. [DOI] [PubMed] [Google Scholar]
- 63. Asaad G, Chan CB.. Food sources of sodium, saturated fat, and added sugar in the Physical Activity and Nutrition for Diabetes in Alberta (PANDA) trial. Appl Physiol Nutr Metab. 2017;42(12):1270–6. [DOI] [PubMed] [Google Scholar]
- 64. Fischer PWF, Vigneault M, Huang R, Arvaniti K, Roach P. Sodium food sources in the Canadian diet. Appl Physiol Nutr Metab. 2009;34(5):884–92. [DOI] [PubMed] [Google Scholar]
- 65. Mulder KA, Zibrik L, Innis SM. High dietary sodium intake among young children in Vancouver, British Columbia. J Am Coll Nutr. 2011;30(1):73–8. [DOI] [PubMed] [Google Scholar]
- 66. Shah BG, Giroux A, Belonje B. Sodium and potassium content of the Canadian diet. Nutr Res. 1982;2(6):669–74. [Google Scholar]
- 67. Yu YH, Farmer A, Mager D, Willows N. Dietary sodium intakes and food sources of sodium in Canadian-born and Asian-born individuals of Chinese ethnicity at a Canadian university campus. J Am Coll Health. 2014;62(4):278–84. [DOI] [PubMed] [Google Scholar]
- 68. Blanco-Metzler A, Claro RM, Heredia-Blonval K, Rodriguez IC, Montero-Campos MdLA, Legetic B, L'Abbe MR. Baseline and estimated trends of sodium availability and food sources in the Costa Rican population during 2004–2005 and 2012–2013. Nutrients. 2017;9(9):1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Carballo de la Espriella M, Morales Palma G. Fuentes alimentarias de sal: sodio en mujeres, Costa Rica [Food sources of salt/sodium in women, Costa Rica]. Rev Costarric Salud Pública. 2011;20(2):90–6. [Google Scholar]
- 70. Colin-Ramirez E, Espinosa-Cuevas A, Miranda-Alatriste PV, Tovar-Villegas VI, Arcand J, Correa-Rotter R. Food sources of sodium intake in an adult Mexican population: a sub-analysis of the SALMEX study. Nutrients. 2017;9(8):810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Agarwal S, Fulgoni VL 3rd, Spence L, Samuel P. Sodium intake status in United States and potential reduction modeling: an NHANES 2007–2010 analysis. Food Sci Nutr. 2015;3(6):577–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Centers for Disease Control and Prevention. Vital signs: food categories contributing the most to sodium consumption—United States, 2007–2008. MMWR Morb Mortal Wkly Rep. 2012;61(5):92–8. [PubMed] [Google Scholar]
- 73. Cotton PA, Subar AF, Friday JE, Cook A. Dietary sources of nutrients among US adults, 1994 to 1996. J Am Diet Assoc. 2004;104(6):921–30. [DOI] [PubMed] [Google Scholar]
- 74. Drewnowski A, Rehm CD.. Sodium intakes of US children and adults from foods and beverages by location of origin and by specific food source. Nutrients. 2013;5(6):1840–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Fulgoni VL 3rd, Agarwal S, Spence L, Samuel P. Sodium intake in US ethnic subgroups and potential impact of a new sodium reduction technology: NHANES Dietary Modeling. Nutr J. 2014;13(1):120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Harnack LJ, Cogswell ME, Shikany JM, Gardner CD, Gillespie C, Loria CM, Zhou X, Yuan K, Steffen LM. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ko J, Timmerman GM, Kim KB, Kim MT. Food sources of sodium in Korean Americans with type 2 diabetes: implications for cardiovascular disease. J Transcult Nurs. 2019;30(2):154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Institute of Medicine. Strategies to reduce sodium intake in the United States. Henney J, Taylor C, Boon C, editors. Washington (DC): National Academies Press; 2010. [PubMed] [Google Scholar]
- 79. Mattes RD, Donnelly D.. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10(4):383–93. [DOI] [PubMed] [Google Scholar]
- 80. Morgan KJ, Zabik ME, Stampley GL. Amount and food sources of sodium intake by children. Nutr Res. 1985;5(3):239–52. [Google Scholar]
- 81. Morgan KJ, Zubik ME, Stampley GL. Amount and food sources of sodium intake by individuals 62 years and older. J Nutr Elder. 1985;4(4):23–38. [Google Scholar]
- 82. US Department of Health and Human Services; USDA. 2015–2020 Dietary guidelines for Americans. 8th ed Washington (DC); 2015. [Internet] [cited 2019 Oct 6].Available from: https://health.gov/dietary guidelines/2015/guidelines/. [Google Scholar]
- 83. Australian Bureau of Statistics. Australian Health Survey: nutrition first results—food and nutrients 2011–12. Canberra (Australia): Commonwealth of Australia; 2014. [Internet] [cited 2019 Oct 6].Available from: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0072011-12?OpenDocument. [Google Scholar]
- 84. Charlton K, Yeatman H, Houweling F, Guenon S. Urinary sodium excretion, dietary sources of sodium intake and knowledge and practices around salt use in a group of healthy Australian women. Aust N Z J Public Health. 2010;34(4):356–63. [DOI] [PubMed] [Google Scholar]
- 85. Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Sources of sodium in Australian children's diets and the effect of the application of sodium targets to food products to reduce sodium intake. Br J Nutr. 2011;105(3):468–77. [DOI] [PubMed] [Google Scholar]
- 86. Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross-sectional study. BMJ Open. 2013;3(2):e002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Grimes CA, Riddell LJ, Campbell KJ, Beckford K, Baxter JR, He FJ, Nowson CA. Dietary intake and sources of sodium and potassium among Australian schoolchildren: results from the cross-sectional Salt and Other Nutrients in Children (SONIC) study. BMJ Open. 2017;7(10):e016639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Keogh JB, Lange K, Hogarth R, Clifton PM. Foods contributing to sodium intake and urinary sodium excretion in a group of Australian women. Public Health Nutr. 2013;16(10):1837–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Margerison C, Riddell LJ, Wattanapenpaiboon N, Nowson CA. Dietary sources and meal distribution of sodium and potassium in a sample of Australian adults. Nutr Diet. 2013;70(4):294–9. [Google Scholar]
- 90. McMahon E, Webster J, O'Dea K, Brimblecombe J. Dietary sodium and iodine in remote Indigenous Australian communities: will salt-reduction strategies increase risk of iodine deficiency? A cross-sectional analysis and simulation study. BMC Public Health. 2015;15(1318). doi:10.1186/s12889-015-2686-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Nowson C, Lim K, Land M-A, Webster J, Shaw JE, Chalmers J, Flood V, Woodward M, Grimes C. Salt intake and dietary sources of salt on weekdays and weekend days in Australian adults. Public Health Nutr. 2018;21(12):2174–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. O'Halloran SA, Grimes CA, Lacy KE, Nowson CA, Campbell KJ. Dietary sources and sodium intake in a sample of Australian preschool children. BMJ Open. 2016;6(2):e008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Villani AM, Clifton PM, Keogh JB. Sodium intake and excretion in individuals with type 2 diabetes mellitus: a cross-sectional analysis of overweight and obese males and females in Australia. J Human Nutr Diet. 2012;25(2):129–39. [DOI] [PubMed] [Google Scholar]
- 94. Eyles H, Shields E, Webster J, Ni Mhurchu C. Achieving the WHO sodium target: estimation of reductions required in the sodium content of packaged foods and other sources of dietary sodium. Am J Clin Nutr. 2016;104(2):470–9. [DOI] [PubMed] [Google Scholar]
- 95. Elorriaga N, Gutierrez L, Romero IB, Moyano DL, Poggio R, Calandrelli M, Mores N, Rubinstein A, Irazola V. Collecting evidence to inform salt reduction policies in Argentina: identifying sources of sodium intake in adults from a population-based sample. Nutrients. 2017;9(9):E964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Perin MS, Cornelio ME, Oliveira HC, Sao-Joao TM, Rheaume C, Gallani M-CBJ. Dietary sources of salt intake in adults and older people: a population-based study in a Brazilian town. Public Health Nutr. 2019;22(8):1388–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Sarno F, Claro RM, Levy RB, Bandoni DH, Monteiro CA. [Estimated sodium intake for the Brazilian population, 2008–2009]. Rev Saude Publica. 2013;47(3):571–8. [DOI] [PubMed] [Google Scholar]
- 98. Souza AdM, Bezerra IN, Pereira RA, Peterson KE, Sichieri R. Dietary sources of sodium intake in Brazil in 2008–2009. J Acad Nutr Diet. 2013;113(10):1359–65. [DOI] [PubMed] [Google Scholar]
- 99. Gaitan Charry DA, Estrada A, Argenor Lozano G, Manjarres LM. Alimentos fuentes de sodio: analisis basado en una encuesta nacional en Colombia. [Food sources of sodium: analysis based on a national survey in Colombia.] 2015;32(5):2338–45. [DOI] [PubMed] [Google Scholar]
- 100. Office for National Statistics and Ministry of Agriculture, Fisheries and Food. National Food Survey, 2000. 2nd ed UK Data Service; 2004; [cited 2019 Oct 6]. doi:10.5255/UKDA-SN-4512-1, https://beta.ukdataservice.ac.uk/datacatalogue/studies/study?id=4512. [Google Scholar]
- 101. National Cancer Institute. Sources of sodium among the U.S. population, 2005–2006. Bethesda (MD): National Cancer Institute; 2010. [Internet] [cited 2019 Oct 6].Available from: https://epi.grants.cancer.gov/diet/foodsources/sodium/#citation. [Google Scholar]
- 102. Menyanu E, Russell J, Charlton K. Dietary sources of salt in low- and middle-income countries: a systematic literature review. Int J Environ Res Public Health. 2019;16(12):E2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hyseni L, Elliot-Green A, Lloyd-Williams F, Kypridemos C, O'Flaherty M, McGill R, Orton L, Bromley H, Cappuccio FP, Capewell S. Systematic review of dietary salt reduction policies: evidence for an effectiveness hierarchy?. PLoS One. 2017;12(5):e0177535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Kloss L, Meyer JD, Graeve L, Vetter W. Sodium intake and its reduction by food reformulation in the European Union—a review. NFS J. 2015;1:9–19. doi.org/10.1016/j.nfs.2015.03.001. [Google Scholar]
- 105. Jaenke R, Barzi F, McMahon E, Webster J, Brimblecombe J. Consumer acceptance of reformulated food products: a systematic review and meta-analysis of salt-reduced foods. Crit Rev Food Sci Nutr. 2017;57(16):3357–72. [DOI] [PubMed] [Google Scholar]
- 106. China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese: a randomized, controlled trial. J Hypertens. 2007;25(10):2011–8. [DOI] [PubMed] [Google Scholar]
- 107. Shao S, Hua YC, Yang Y, Liu XJ, Fan JR, Zhang A, Xiang JL, Li MJ, Yan LJL. Salt reduction in China: a state-of-the-art review. Risk Manag Healthcare Policy. 2017;10:17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015;33(8):1509–20. [DOI] [PubMed] [Google Scholar]
- 109. Du S, Lu B, Zhai F, Popkin BM. A new stage of the nutrition transition in China. Public Health Nutr. 2002;5(1a):169–74. [DOI] [PubMed] [Google Scholar]
- 110. Shetty PS. Nutrition transition in India. Public Health Nutr. 2002;5(1a):175–82. [DOI] [PubMed] [Google Scholar]
- 111. Hu D, Reardon T, Rozelle S, Timmer P, Wang H. The emergence of supermarkets with Chinese characteristics: challenges and opportunities for China's agricultural development. Dev Policy Rev. 2004;22(5):557–86. [Google Scholar]
- 112. Reardon T, Timmer CP, Barrett CB, Berdegué J. The rise of supermarkets in Africa, Asia, and Latin America. Am J Agric Econ. 2003;85(5):1140–6. [Google Scholar]
- 113. O'Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang XY, Liu LS, Yan H, Lee SF, Mony P, Devanath A et al.. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371(7):612–23. [DOI] [PubMed] [Google Scholar]
- 114. Irazola VE, Gutierrez L, Bloomfield G, Carrillo-Larco RM, Dorairaj P, Gaziano T, Levitt NS, Miranda JJ, Ortiz AB, Steyn K et al.. Hypertension prevalence, awareness, treatment, and control in selected LMIC communities: results from the NHLBI/UHG Network of Centers of Excellence for Chronic Diseases. Glob Heart. 2016;11(1):47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Lowell BB. New neuroscience of homeostasis and drives for food, water, and salt. N Engl J Med. 2019;380(5):459–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.