ABSTRACT
Vitamin A is a fat-soluble essential nutrient obtained from plant- and animal-based sources that has roles in growth, vision, and metabolism. Vitamin A circulates mainly as retinol bound to retinol-binding protein 4 (RBP4), and is delivered to tissues and converted to retinoic acid, which is a ligand for several nuclear receptors. In recent years, aspects of vitamin A metabolism have been under scrutiny with regards to the development of metabolic and lifestyle diseases including cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and overweight and obesity in humans. Studies have mainly focused on RBP4 in this context, whereas the major circulating form, retinol, and the major bioactive form, retinoic acid, have been overlooked in this regard until recently. As one of the main roles of RBP4 is to deliver retinol to tissues for biological action, the associations of retinol and retinoic acid with these diseases must also be considered. In this review, we summarize and discuss recent and available evidence from human studies with focus on retinol, retinoic acid, and RBP4 and provide an overview of these crucial components of vitamin A metabolism in CVD, T2DM, and obesity. In summary, retinol was found to be both inversely and positively associated with CVD whereas the associations with T2DM and obesity were less clear. Although only a few studies have been published on retinoic acid, it was inversely associated with CVD. In contrast, serum RBP4 was mostly found to be positively associated with CVD, T2DM, and obesity. At present, it is difficult to ascertain why the reported associations differ depending on the compound under study, but there is a clear imbalance in the literature in disfavor of retinol and retinoic acid, which needs to be considered in future human studies.
Keywords: vitamin A, fat-soluble vitamins, cardiovascular disease, type 2 diabetes mellitus, overweight, obesity, epidemiology
Introduction
Vitamin A is a collective term comprising a group of fat-soluble compounds with essential biological activity ranging from phototransduction in photoreceptor cells of the retina to growth and development. An extensive overview of vitamin A absorption, metabolism, and functions can be found in (1). In brief, dietary vitamin A can be obtained from plant-based foods as provitamin A carotenoids (e.g. β-carotene) or animal-based foods as esterified retinol (retinyl esters). Following absorption, vitamin A is transported from intestinal mucosal cells, with chylomicrons as retinyl esters, to target tissues or the liver where it can be stored in hepatic stellate cells. Net mobilization of liver stores occurs in times of deficient dietary intake, and retinyl esters are hydrolyzed to release retinol which is subsequently bound to retinol-binding protein 4 (RBP4) and secreted into the circulation from hepatocytes where it binds to an additional transport protein, transthyretin. Once absorbed by target cells, retinol can be converted to either retinaldehyde, which is crucial for normal visual function, or further oxidized to retinoic acid, a ligand for nuclear retinoic acid receptors with a wide array of target genes in growth, development, and metabolism (2).
The vitamin A status of an individual is ideally assessed by quantifying liver stores, but given the impracticalities associated with this measure, other biochemical markers such as serum retinol and retinol isotope dilution can be applied (3, 4). A deteriorating vitamin A status remains a considerable public health concern in developing countries and supplementation prevents infectious diseases and child mortality (5, 6). For example, the prevalence of vitamin A deficiency exceeds 60% in some developing countries (7), whereas 0.26% are considered to be at risk in a representative US population (8). In societies where deficient intake is not a concern, emerging evidence over the last decades suggest that aspects of vitamin A metabolism, such as elevated concentrations of RBP4, are positively associated with obesity, type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), and overall mortality (9–12). However, even though the main function of RBP4 is to deliver retinol to target tissues where it can exert biological effects mainly as retinoic acid (1), retinol and retinoic acid have been largely overlooked in this context for unknown reasons until fairly recently. Thus, the overreaching aim of this review is to provide an overview of the existing literature from human populations and interventions that have linked aspects of vitamin A metabolism, including major circulating and bioactive metabolites to major lifestyle diseases including CVD, T2DM, and obesity. On a final note, we will discuss inconsistencies in the findings that challenge interpretation and outline the current knowledge gaps in the field that must be bridged in order to advance our understanding of vitamin A in relation to the above-mentioned diseases.
Literature search
The literature search was conducted between January and June 2019. PubMed was initially screened for relevant articles. The search for studies on RBP4 and CVD was limited to 2016 because Zabetian-Thargi reviewed the observational evidence on this relation in 2015 (11). The search terms included the following string [“plasma retinol”(TW) OR “plasma vitamin A”(TW) OR “serum retinol”(TW) OR “serum vitamin A”(TW) OR “serum retinol-binding protein 4”(TW) OR “plasma retinol-binding protein 4”(TW) OR “serum retinoic acid”(TW)] in combination with 1 of the following keywords: diabetes mellitus, type 2; type 2 diabetes mellitus; insulin resistance; stroke; cerebrovascular stroke; cardiovascular disease; coronary artery disease; myocardial infarction; obesity; fat mass; or body adiposity. The search was filtered to include adults only. Additional manual searches of study reference lists and study citation searches were performed. Titles and abstracts were screened for eligibility. We note that because this was not a systematic review, no strict inclusion criteria were applied, except that the studies were of epidemiological or interventional design and included populations that were either 1) initially healthy or 2) had developed or were at risk of CVD, T2DM, or obesity without any major and unrelated comorbidities. We did not record reasons for exclusions in a systematic manner.
Current Status of Knowledge
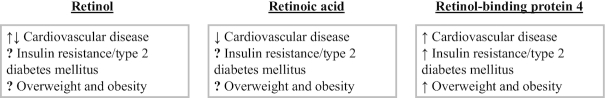
The main findings of this review are summarized in Figure 1.
FIGURE 1.
A summary of the main findings. Arrows indicate direction of disease associations; ↑, positive association; ↓, inverse association; ?, inconclusive or unknown association.
Vitamin A and CVD
A summary of studies included in this section can be found in Table 1 which lists study type, population, main findings, and relevant effect measures.
TABLE 1.
| First author and year | Study type and n | Method for quantification | Endpoint assessment | Population and country | Statistical methods and models | Main finding | Effect measure and size |
|---|---|---|---|---|---|---|---|
| Studies on retinol | |||||||
| De Keyser et al., 1992 (13) | Prospective cohort, n = 80 | HPLC | Recovery and mortality. Methods for ascertainment not given | Patients admitted with stroke, USA | Chi-square (recovery) and Fishers exact test (mortality) | Patients with retinol concentrations above 2.27 µmol/L had increased rates of recovery and decreased mortality | No effect sizes given |
| Omenn et al., 1996 (14) | Randomized controlled trial, n = 18,314 | — | Cardiovascular mortality, ascertained by evaluation of endpoint committee | Smokers, former smokers, and workers exposed to asbestos, Finland | Cox proportional hazards model with a single covariate (treatment group) | Participants receiving supplements of ß-carotene and retinyl palmitate had higher risk of CVD mortality | RR for CVD mortality: 1.26 (0.99, 1.61) |
| Bobbert et al., 2010 (15) | Cross-sectional study, n = 96 | HPLC | IMT, ascertained by ultrasound | 34 individuals with type 2 diabetes and 62 individuals with normal glucose tolerance, Germany | Unadjusted correlational analyses | RBP4 was positively, whereas retinol was inversely, correlated to carotid IMT | Pearson's r for RBP4 and IMT = 0.34. For retinol and IMT = –0.24 |
| Gey et al., 2010 (16) | Prospective case-control study, 150 cases, 285 controls | HPLC | CHD, ascertained by clinical examinations and autopsies (fatal CHD) | CVD-free men aged 50–59 y, Northern Ireland and France | Univariate conditional logistic regression | Increasing concentrations of plasma and lipid-standardized retinol were associated with lower risk of CHD | RR of CHD per SD increase in log-transformed retinol: 0.71 (0.57, 0.88). RR of CHD per SD increase in log-transformed lipid-standardized retinol: 0.65 (0.52, 0.81) |
| Brazionis et al., 2012 (17) | Prospective cohort study, n = 441 | HPLC | CVD mortality, obtained from the Victorian Cancer Registry and the Australian Bureau of Statistics | Community-dwelling older overweight adults where 45% had type 2 diabetes mellitus, Australia | Cox proportional hazards model adjusted for age, sex, diabetes, hypertension, self-reported heart condition, plasma values of cholesterol, triglycerides, homocysteine, CRP, α-carotene, β-carotene, β-cryptoxhantin, urinary albumin excretion rate, dietary vitamin A intakes | Participants in the upper (2.64 µmol/L) vs. lower tertile (1.57 µmol/L) had a lower risk of CVD mortality | HR of CVD mortality (upper vs. lower tertile): 0.27 (0.11, 0.68) |
| Min and Min, 2014 (18) | Prospective cohort study, n = 6069 | HPLC | CVD and CHD mortality were coded using ICD-10 codes. It was not reported where endpoint information was obtained from | Participants aged >50 y in the NHANES III, USA | Cox proportional hazards model adjusted for age, sex, ethnicity, education, smoking, BMI, disease history, plasma concentrations of total cholesterol, triglycerides, CRP, and β-carotene | Participants with retinol concentrations below 1.05 µmol/L and above 2.80 µmol/L had an increased risk of CVD and CHD mortality compared with participants within the range of 1.05 to 2.80 µmol/L | HR of CVD below 1.05 µmol/L vs. 1.05 to 2.80 µmol/L: 2.1 (1.1, 4.1). HR of CVD above 2.80 µmol/L vs. 1.05 to 2.80 µmol/L: 1.4 (1.2, 1.8). HR of CHD mortality 1.05 µmol/L vs. 1.05 to 2.80 µmol/L: 2.5 (1.2, 5.3). HR of CHD mortality above 2.80 µmol/L vs. 1.05 to 2.80 µmol/L: 1.5 (1.2, 2.0) |
| Olsen et al., 2017 (19) | Prospective cohort study, n = 4117 | LC-MS/MS | Acute myocardial infarction, obtained from the Western Norway Cardiovascular Disease Registry | Patients hospitalized for suspected coronary artery disease, Norway | Cox proportional hazards model adjusted for age, sex, smoking, CRP, number of stenotic vessels, left ventricular ejection fraction, hypertension, statin use at discharge from hospital, and estimated glomerular filtration rate | Serum retinol modified lipid-associated risk of AMI. Patients in the upper tertile (serum retinol >3.10 µmol/L). Patients hospitalized for suspected coronary artery disease had increased apoB-associated risk and decreased apoA-1-associated risk | HR per SD increase of apoB in the upper retinol tertile: 1.35 (1.11, 1.65). HR per SD increase apoB/apoA-1: 1.42 (1.16, 1.74). HR per SD increase in apoA-1: 0.87 (0.71, 1.05) |
| Olsen et al., 2018 (20) | Prospective cohort study, n = 2205 | LC-MS/MS | Acute myocardial infarction, obtained via record linkage to the Cardiovascular Disease in Norway project | Patients hospitalized for suspected coronary artery disease, Norway | Cox proportional hazards model adjusted for age, sex, smoking, estimated glomerular filtration rate, statin and aspirin prescription at discharge, fasting, and apoB | Serum retinol modified total homocysteine-associated risk of AMI. Patients in the upper tertile had increased total homocysteine-associated risk | HR per SD increase of total homocysteine in the upper retinol tertile: 1.25 (1.04, 1.53) |
| Yu et al., 2019 (21) | Prospective case-control study, n = 620 | LC-MS/MS | Stroke, obtained by clinical records and image data, reviewed and verified by endpoint committee | Men and women with hypertension, China | Conditional logistic regression model adjusted for BMI, smoking, alcohol intake, systolic and diastolic blood pressure, fasting blood glucose, plasma total cholesterol, triglycerides and HDL cholesterol, estimated glomerular filtration rate, and plasma folate, B12, and total homocysteine | Increasing retinol concentrations were inversely associated with first stroke | OR per 0.35 µmol/L increase in retinol: 0.92 (0.86, 0.97) |
| Studies on retinoic acid | |||||||
| Liu et al., 2016 (22) | Prospective cohort study, n = 1499 | ELISA validated against GC-MS | CVD mortality was defined as death attributable to ischemic CVD and sudden death, endpoints were obtained from Guangdong Provincial Center for Disease Control | Patients with verified coronary artery disease, China | Cox proportional hazards model adjusted for age, sex, BMI, smoking, diabetes, hypertension, estimated glomerular filtration rate, statin use, concentrations of total cholesterol, HDL, LDL, acute myocardial infarction, percutaneous intervention or coronary artery bypass graft at enrollment, left ventricular ejection fraction, serum CRP, and Gensini score | Increasing concentrations of retinoic acid was associated with a lower risk of CVD mortality | HR of CVD mortality per SD increase of retinoic acid: 0.68 (0.50, 0.85) |
| Tu et al., 2019 (23) | Prospective cohort study, n = 1530 | ELISA validated against LC-MS/MS | CVD mortality recorded according to the ICD-10 codes and verified by the Academic Research Consortium criteria. Study does not report from where endpoint information was obtained. | Patients admitted for first acute ischemic stroke, China | Logistic regression adjusted for age, sex, BMI stroke etiology, NIH Stroke Scale score, infarct volume, prestroke and acute treatment, vascular risk factors, HOMA-IR, plasma glucose, high-sensitivity CRP, homocysteine, IL-6, triglyceride, total cholesterol, HDL, and LDL | Increasing concentration of retinoic acid was associated with a lower risk of CVD mortality | HR of CVD mortality (quartile 2–4 vs. 1): 0.37 (0.28, 0.49) |
| Studies on RBP4 | |||||||
| Liu et al., 2016 (24) | Prospective cohort study, n = 950 | ELISA | CVD mortality, obtained from autopsy reports, hospital records, or death certificates | Men with type 2 diabetes mellitus, USA | Cox proportional hazards model adjusted for age, year of blood draw, BMI at age 21 y, physical activity, smoking, alcohol intake, diabetes duration, family history of myocardial infarction, aHEI score, use of aspirin or cholesterol-lowering medications, baseline history of hypertension, high cholesterol, angina, coronary artery bypass graft, myocardial infarction and stroke, estimated glomerular filtration rate, HDL, LDL, and CRP | A nonsignificant but clear trend for an inverse association for RBP4 and CVD mortality was observed during 22 y of follow-up | HR for CVD mortality in the upper tertile of RBP4: 0.73 (0.50, 1.07) |
| Zachariah et al., 2016 (25) | Cross-sectional study, n = 3305 | ELISA | Mean arterial pressure and carotid femoral pulse wave velocity ascertained by applanation tonometry | Community-dwelling adults, USA | Linear regression adjusted for age, sex, heart rate, height, antihypertensive treatment, total and HDL cholesterol, smoking, diabetes, body weight, estimated glomerular filtration rate, alcohol intake, blood glucose, and CRP | Increasing concentration of RBP4 was positively associated with mean arterial pressure and aortic stiffness | β for mean arterial pressure per SD increase in RBP4: 1.15 (0.78, 1.51).β for –1000/carotid femoral pulse wave velocity per SD increase in RBP4: 0.58 (–0.08, 1.25) |
| Liu et al., 2017 (26) | Prospective cohort study, n = 1683 | ELISA validated against Western blotting | Cardiovascular event, defined according to ICD-10 criteria, but no information on how endpoint information was obtained were given | General population, China | Cox proportional hazards model adjusted for age, sex, BMI, smoking status, systolic blood pressure, fasting blood glucose, prevalence of hypertension and diabetes mellitus, LDL, HDL, CRP, estimated glomerular filtration rate usage of aspirin, statins, ACE inhibitor, ARB, or β-blockers, and angriographically verified disease extent | Participants in the upper quartile of circulating RBP4 (>57.8 µg/mL) had an increased risk of major CVD events | HR of a major cardiovascular event in the upper RBP4 quartile (>57.8 µg/mL): 1.47 (1.19, 1.68) |
| Zhang et al., 2017 (27) | Case-control study, 160 cases and 160 controls | ELISA | Systolic and diastolic blood pressure, measured by a mercury sphygmomanometer | Prehypertensive cases, healthy controls, China | Partial correlation analyses were adjusted for age, sex, smoking status, and alcohol intake | Concentrations of RBP4 were higher in prehypertensive compared with controls. RBP4 was a significant predictor of blood pressure in the total sample | No effect sizes given for differences between groups. β for SBP per unit increase in RBP4 in the total sample: 0.27, SE: 0.04. β for DBP per unit increase in the total sample RBP4: 0.14, SE: 0.03 |
| Rist et al., 2018 (28) | Prospective case-control study, 471 cases and 471 controls | ELISA | Stroke, ascertained by review of medical records, death certificates, hospital records, or autopsy records | Stroke cases and healthy controls from the Nurses’ Health Study, USA | Conditional logistic regression adjusted for age, race/ethnicity, menopausal status, hormone use, smoking, date of sample collection, physical activity, BMI, aspirin use alcohol intake, aHEI score, history of diabetes, hypertension, coronary heart disease or revascularization and high cholesterol, log-transformed cholesterol ratio, and HbA1c | A nonsignificant inverse association was observed for increasing concentrations of RBP4 and risk of ischemic stroke | OR for ischemic stroke in the highest (>37.2 µg/mL) vs. lowest (<26.12 µg/mL) RBP4 quartile: 0.75 (0.48, 1.17) |
| Zhu et al., 2018 (29) | Prospective cohort study, n = 299 | ELISA with 1:100 dilution due to high concentrations | Functional outcome, ascertain by the modified Rankin Scale | Patients admitted for first ever stroke, China | Logistic regression adjusted for age, sex, BMI, infarct volume, NHI stroke score, acute treatment, atrial fibrillation, stroke syndrome, serum CRP, and fasting glucose | RBP4 was positively associated with poor functional outcome (high modified Rankin scale score) after first stroke | OR of modified Rankin scale score for functional outcome per unit increase in RBP4: 1.09 (1.06, 1.13) |
| Liu and Che, 2019 (30) | Case-control study, 323 cases and 323 controls | ELISA with 1:100 dilution due to high concentrations | Stroke, ascertained by diffusion-weighted imaging and/or computed tomography | Stroke cases and healthy controls, China | Stroke: logistic regression adjusted for including hypercholesterolemia, family history of stroke, alcohol intake, smoking, and serum concentrations of triglycerides, cholesterol, HDL, LDL, glucose, CRP, and homocysteine. Moderate-to-high stroke risk: logistic regression age, sex, traditional risk factors, prior and acute treatments, stroke syndrome, stroke subtype, SBP, DBP, and serum concentrations of triglycerides, cholesterol, HDL, LDL, glucose, CRP, and homocysteine | A positive association of RBP4 was observed for stroke risk. The association was particularly strong when RBP4 exceeded 39.7 µg/mL. RBP4 was further associated with stroke severity | OR of ischemic stroke per unit increase of RBP4: 1.03 (1.01, 1.04). In patients with RBP4 >39.7 µg/mL the OR was 4.12 (2.03, 5.45). OR of moderate-to-high stroke severity per unit increase of RBP4: 1.07 (1.05, 1.09) |
All effect measures are given as HR/OR/RR (95% CIs) unless otherwise noted.
ACE, angiotensin-converting enzyme; aHEI, alternative healthy eating index; AMI, acute myocardial infarction; ARB, angiotensin II receptor blocker; CHD, coronary heart disease; CRP, C-reactive protein; CVD, cardiovascular disease; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin; ICD, International Classification of Diseases; IMT, intima-media thickness; LC-MS/MS, liquid chromatography tandem mass spectrometry; RBP4, retinol-binding protein 4; SBP, systolic blood pressure.
Retinol and CVD
The associations observed for circulating concentrations of retinol and CVD are somewhat conflicting. One early study among first stroke patients suggested that those with higher circulating concentrations of retinol had increased rates of recovery and decreased mortality (no effect sizes given) (13). In contrast, results from the β-carotene and Retinol Efficacy Trial, which was designed to test whether β-carotene and retinyl ester supplementation could prevent cancer in smokers, former smokers, and workers exposed to asbestos, showed that supplementation resulted in a 26% increased risk of cardiovascular mortality in the intervention group compared with controls (14). From the observational studies that ensued, it has been difficult to establish a clear-cut relation between retinol and CVD. In a nested case-control study among nearly 10,000 initially CVD-free participants at baseline, 1 unit increase in log-transformed plasma retinol concentration was associated with a 29% decrease in coronary artery disease (CAD) (16). Similar findings were reported in an overweight but otherwise healthy population (17) where subjects in the upper retinol tertile (>2.64 µmol/L) had 73% lower risk of CVD mortality compared with subjects in the lower retinol tertile (<1.57 µmol/L). In 96 individuals with and without T2DM from the Metabolic Syndrome Berlin Potsdam cohort, retinol concentrations were weakly but inversely correlated to carotid artery intima-media thickness (Pearson's r = –0.24) (15), an important indicator of atherosclerotic progression. Finally, a recently published study among Chinese subjects at increased stroke risk, reported that risk of first stroke was lowered by 8% per 0.35 µmol/L increase in serum retinol (21). Collectively, these observational studies indicate that high compared with low plasma retinol concentrations are advantageous in terms of CVD, and it is appealing to conclude that the higher retinol in circulation the better in this context. However, this view has been challenged by findings from the NHANES III showing that both reduced and elevated retinol concentrations in plasma beyond a clinical reference range (1.05 to 2.80 µmol/L) increased the risk of CVD and mortality from coronary heart disease, thereby suggesting a U-shaped relation for plasma retinol and CVD (18). Additionally, recent results from a cohort consisting of patients hospitalized for suspected CAD indicate that retinol may modify the risk of incident CVD associated with established risk factors including apoB, apoA1, and total homocysteine. Specifically, patients with circulating concentrations of retinol exceeding 3.10 µmol/L exhibited 35% increased risk of CVD per 1 SD increase in apoB, and a 42% increased risk of CVD per 1 SD increase in the ratio of apoB relative to apoA-1. In addition, a 1 SD increase in apoA-1 concentration was associated with a 13% risk reduction (19). In a subsequent article from the same core population, it was shown that patients with circulating concentrations of retinol exceeding 3.20 µmol/L, a 1 SD increase in plasma total homocysteine concentration was associated with a 25% increased risk of CVD in 2205 patients with suspected CAD (20). Taken together, although the findings on the relation between serum retinol and CVD suggest that higher retinol concentrations may be beneficial compared with lower concentrations in terms of risk, elevated concentrations beyond the upper limit of the reference range, may be harmful in itself or affect CVD risk in other ways such as the reported effect modification on other risk factors.
Retinoic acid and CVD
At the time of the literature search, very few observational studies had addressed the relation between retinoic acid and CVD. One study among ∼1500 Chinese patients with angiographically verified CAD reported that CVD mortality was reduced by 32% for each SD increase in serum all-trans retinoic acid (22). A recently published study among 1530 acute ischemic stroke patients showed that patients in the upper 3 quartiles of circulating retinoic acid had a substantially reduced (63%) 6-mo CVD mortality compared with patients in the lowest quartile (23). Based on these findings, the authors cited experimental studies and speculated that retinoic acid may be considered in the treatment of CVD; however, there are some inherent problems with this statement. For example, isotretinoin, a synthetic retinoic acid isoform (13-cis retinoic acid), which is readily converted to all-trans retinoic acid in target cells, has been in clinical use for dermatological conditions for some time. One common side effect of isotretinoin treatment is dyslipidemia (31, 32) as well as elevation of plasma total homocysteine concentration as recently reviewed (33). Although these effects may 1) be transient, 2) depend on dosage, and/or 3) be due to differential effects of the 13-cis retinoic acid compared with all-trans retinoic acid, caution should be taken in making recommendations for retinoic acid usage in CVD treatment as risk factors may be aggravated as a result. At present, no trials have addressed potential treatment benefits of retinoic acid in the context of CVD or stroke prevention and more preclinical and observational evidence are needed before trials can commence.
RBP4 and CVD
In their review from 2015, Zabetian-Thargi and colleagues reported an association between RBP4 and CVD but called for more accurate observational and longitudinal studies on this association in order to establish a relation (11). Thus, we have limited the section of RBP4 to the observational studies that have surfaced since then, several of which are longitudinal by design.
In 3505 healthy, CVD-free individuals participating in the Framingham Third Generation Cohort, total RBP4 concentrations were positively correlated to mean arterial pressure [β (95% CI) for mean arterial pressure per SD increase in RBP4: 1.15 (0.78–1.51)] (25). Data from this cohort were clearly compatible with a positive correlation between RBP4 and aortic stiffness even though the reported CI crossed the null [β (95% CI) for –1000/carotid femoral pulse wave velocity per SD increase in RBP4: 0.58 (–0.08, 1.25)]. In a smaller cross-sectional study, RBP4 was postively correlated to systolic (Pearson's r = 0.47) and diastolic blood pressure (Pearson's r = 0.36) in prehypertensive Chinese individuals (27). In contrast, among 950 men with T2DM with 22 y of follow-up data, a clear trend for an inverse association was found for total RBP4 concentrations and cardiovascular mortality [HR (95% CI) for CVD mortality, 3rd versus 1st tertile: 0.73 (0.50, 1.07)] (24). In the context of stroke, 1 prospective case-control study based in the Nurses’ Health Study reported an overall inverse risk of stroke in the upper versus lower quartile of circulating RBP4, but the finding was inconclusive [OR: 0.75, 95% CI (0.48, 1.17)] (28). In contrast, 1 unit increase in RBP4 concentration was associated with a 3% increase in ischemic stroke risk, and a 7% increase in stroke severity in a Chinese population (30), and has been proposed as an independent predictor of poor short-term prognosis following first stroke (29). Finally, in an interdisciplinary study combining data from an initially healthy Chinese population and mice, it was first shown that subjects in the upper quartile of circulating RBP4 (>57.8 µg/mL) had a 47% increase in risk of major cardiovascular events (26). The authors then went on to show that apo-RBP4 (RBP4 not bound to retinol) can promote atheroslclerotic progression in the same manner that holo-RBP4 (RBP4 bound to retinol) can.
Vitamin A and T2DM
The literature concerning vitamin A metabolism and T2DM has been dominated by RBP4 since it was established as an adipokine in the early 2000s (34). Although some evidence points towards RBP4 having effects independently of its transport of retinol (26, 35), retinol and retinoic acid have been more or less neglected in this context even though the presumed main function of RBP4 is to deliver retinol to tissues where it can exert biological function. A summary of published studies including insulin resistance and T2DM follows below and the studies included in this section are summarized in Table 2.
TABLE 2.
| First author and year | Study type and n | Method for quantification | Endpoint assessment | Population and country | Statistical methods and models | Main finding | Effect measure and size |
|---|---|---|---|---|---|---|---|
| Studies on retinol and retinoic acid | |||||||
| Tavridou et al., 1997 (36) | Case-control study, 32 cases, 148 controls | HPLC | Impaired glucose tolerance, ascertained by an oral glucose tolerance test | 32 cases with impaired glucose tolerance, 148 healthy controls, UK | t-test | Subjects with impaired glucose tolerance had higher serum retinol than healthy controls (2.5 vs. 2.1 µmol/L) | Only P values and no effect sizes given |
| Abahusain et al., 1999 (37) | Case-control study, 107 cases, 143 controls | HPLC | Impaired glucose tolerance based on morning fasting glucose or an oral glucose tolerance test | 107 subjects with type 2 diabetes mellitus and 143 controls, Saudi Arabia | t-test | Serum retinol was similar between cases and controls, whereas serum and urine RBP4 were higher among cases | Only P values and no effect sizes given |
| Higuchi et al., 2015 (38) | Cross-sectional study, n = 951 | UPLC | Insulin resistance based on the HOMA-IR and the Matsuda Index | General population, Japan | Logistic regression adjusted for sex, age, physical activity, BMI, alcohol intake, and smoking | Subjects in the upper retinol quartile (3.1–5.2 µmol/L) were not more insulin resistant compared with lower quartiles | OR for insulin resistance in the upper retinol quartile: 0.86 (0.53, 1.40). OR for low insulin sensitivity in the upper retinol quartile: 0.89 (0.56, 1.43) |
| Kim et al., 2017 (39) | Prospective case-control study, 55 cases and 220 controls | UPLC | Incident T2DM was ascertained by fasting glucose or history of diabetes treatment | 55 cases with impaired fasting glucose at baseline and 220 healthy controls, South Korea | Logistic regression adjusted for age, fasting glucose and γ-glutamyl transpeptidase | Metabolomics analysis revealed that reinaldehyde, retinoic acid, and retinyl esters at baseline predicted incident type 2 diabetes | OR for incident T2DM associated with high (>2.76) vs. low (<2.76) retinoic acid/retinaldehyde ratio: 2.21 (1.13, 4.32) |
| Studies on RBP4 | |||||||
| Cho et al., 2006 (40) | Case-control study with 57 controls, 48 subjects with impaired glucose tolerance and 49 subjects with T2DM | ELISA | Impaired glucose tolerance, assessed by an oral glucose tolerance test | Individuals with normal or impaired glucose tolerance, or T2DM, South Korea | ANOVA and univariate Pearson's correlation | Log-transformed RBP4 was slightly higher among subjects with impaired glucose tolerance and type 2 diabetes compared with subjects with normal glucose tolerance. In subjects with normal glucose tolerance, fasting plasma glucose was moderately associated with RBP4 | Only P values and no effect sizes reported. Correlation between fasting plasma glucose and RBP4: Pearson's r = 0.37 |
| Graham et al., 2006 (41) | Case-control study in 3 subpopulations: group 1: 5 healthy controls, 7 obese without diabetes, and 9 obese with diabetes. Group 2: 20 controls with normal glucose tolerance, 20 subjects with impaired glucose tolerance, and 20 subjects with T2DM. Group 3: 26 nonobese relatives of subjects with T2DM | ELISA and Western blotting | Impaired glucose tolerance and T2DM was assessed by oral glucose tolerance tests | Lean, overweight, and obese subjects with and without T2DM, USA, Germany, and Sweden | Univariate Spearman rank correlations | In group 1, obese patients with and without diabetes had higher concentrations of RBP4. In group 2, serum RBP4 was higher among subjects with impaired glucose tolerance and T2DM compared with subjects with normal glucose concentrations. In group 3, serum RBP4 was positively correlated to fasting insulin | Correlation of RBP4 with fasting insulin in group 1: Spearman's r = 0.72. Correlation of RBP4 with glucose disposal rate in group 2: Spearman's r = –0.78. Correlation of RBP4 with fasting insulin in group 3: Spearman's r = 0.71 |
| Broch et al., 2007 (42) | Cross-sectional study, n = 107 | Nephelometry | Insulin response, ascertained by the insulin AUC the first 10 min after an intravenous glucose tolerance test | Nondiabetic men with a BMI ranging from 19 to 40, Spain | Univariate Pearson's correlation and multivariable linear regression model adjusted for BMI, age, and insulin sensitivity | RBP4 was inversely correlated to acute insulin response in the total population, and after a glucose load in obese subjects | Univariate correlation of RBP4 with insulin response: Pearson's r = –0.27. In a multivariable regression model, the standardized coefficient was –0.41 among obese subjects |
| Gavi et al., 2007 (43) | Cross-sectional study, n = 92 | ELISA | Insulin sensitivity, ascertained by a euglycemic insulin clamp | Subjects free of diabetes, USA | Univariate Pearson's correlation | Serum concentrations of RBP4 was inversely correlated to insulin sensitivity | Correlation between log-transformed RBP4 and insulin sensitivity: Pearson's r = 0.32 |
| Hahn et al., 2007 (44) | Case-control study in 200 cases and 64 controls | ELISA | Insulin resistance assessed by fasting glucose and the HOMA-IR | Women with PCOS, Germany | Univariate Spearman's correlation | No differences in RBP4 between cases and controls. Among women with PCOS. RBP4 was correlated to fasting glucose but not insulin sensitivity | Correlation for RBP4 with fasting glucose: Spearman's r = 0.14. Correlation for RBP4 with HOMA-IR: r = 0.09 |
| Promintzer et al., 2007 (45) | Cross-sectional study, n = 40 | Nephelometry validated against Western blotting | Insulin sensitivity and resistance ascertained by an oral glucose tolerance test and euglycemic insulin clamp | 20 subjects who were classified as insulin resistant and 20 subjects who were insulin sensitive, Austria | t-test | No associations between insulin sensitivity and RBP4. Plasma concentrations did not respond markedly to a clamp test or an oral glucose tolerance test | No effect sizes given |
| Qi et al., 2007 (46) | Cross-sectional study, n = 3289 | ELISA validated against Western blotting | Insulin resistance assessed by HOMA-IR | Participants residing in urban and rural areas of China | Partial Spearman's correlation analyses adjusted for age, sex, region, and residence | Weak partial correlation between RBP4 and fasting insulin and HOMA-IR | Correlation for RBP4 and fasting insulin and HOMA-IR: Spearman's r = 0.12 and 0.11, respectively |
| Stefan et al., 2007 (47) | Cross-sectional study, n = 75 | ELISA | Insulin sensitivity assessed by euglycemic insulin clamp and an oral glucose tolerance test | Subjects free of diabetes, Germany | Univariate Pearson's correlation analyses and multivariable regression analyses adjusted for sex, age, height, body fat, visceral fat, and intramyocellular lipid content | A moderate inverse correlation was observed for RBP4 and insulin sensitivity as measured by clamp and an oral glucose tolerance test. This was also seen in a multivariable regression model | Correlation between RBP4 and insulin sensitivity as measured by clamp: Pearson's r = –0.26 and as measured by an oral glucose tolerance test: Pearson's r: –0.25. In multivariable regression plasma RBP4 was inversely associated with insulin sensitivity as measured by an oral glucose tolerance test (β: -0.007, SE: 0.003) |
| Takebayashi et al., 2007 (48) | Case-control and single-arm intervention, 22 controls and 101 diabetic patients in the case-control study. 22 in the single-arm intervention | EIA | Insulin resistance, as assessed by HOMA-IR. Diabetic retinopathy ascertained by the Davis’ classification. RBP4 ascertained by EIA kit | Men and women hospitalized for diabetes and healthy controls, Japan | Simple linear regression for RBP4 and HOMA-IR. t-test for comparison of means | RBP4 not associated with insulin resistance but was higher in patients with diabetic retinopathy compared with patients without retinopathy. No changes in RBP4 were observed after 3 mo of pioglitazone treatment | R value for RBP4 and HOMA-IR (–0.16, SE not given).Only P values and no effect sizes given for differences according to diabetic retinopathy classification. Only P value and no effect sizes given for single-arm intervention |
| von Eynatten et al., 2007 (49) | Cross-sectional study, n = 365 | ELISA validated against Western blotting | Insulin resistance, as assessed by HOMA-IR | 126 subjects with T2DM, 143 subjects with coronary artery disease and 96 controls, Germany | Multivariable linear regression model adjusted for BMI, LDL, VLDL, history of hypertension, and HbA1c | No associations were observed for RBP4 and HOMA-IR | β for RBP4 and HOMA-IR in subjects with T2DM: –0.007; and with coronary artery disease: 0.09. SEs were not given |
| Diamanti-Kandarakis et al., 2008 (50) | Case-control study, 35 cases, 45 controls | ELISA | Insulin resistance as assessed by HOMA-IR | 35 women with PCOS and 45 health controls, Greece | Univariate Pearson's correlation | No correlation between RBP4 and insulin resistance | Correlation for RBP4 with insulin and HOMA-IR: Pearson's r = –0.09 and 0.026, respectively |
| Gomez-Ambrosi, et al., 2008 (51) | Cross-sectional, n = 42 | ELISA validated against Western blotting | Impaired glucose tolerance, ascertained by an oral glucose tolerance test | 11 lean, 10 obese with normal glucose tolerance, 11 obese with impaired glucose tolerance, and 10 obese with T2DM, Spain | t-test | No associations were observed for RBP4 and insulin resistance | No effect sizes given |
| Hutchison et al., 2008 (52) | Case-control 38 cases, 17 controls. Subsequent intervention with either metformin or oral contraceptive pill in PCOS subjects for 6 mo | Western blotting | Impaired glucose tolerance, ascertained by an oral glucose tolerance test | 38 overweight women with PCOS, 17 healthy controls, Australia. 19 were randomly assigned to metformin treatment and 19 to oral contraceptives in the intervention | ANOVA and bivariate Pearson's correlations | No associations between insulin resistance and RBP4. Insulin resistance improved and no changes were detected in RBP4 after treatment with metformin | No effect sizes given |
| Lewis et al., 2008 (53) | Prospective cohort study, n = 206 | ELISA | Insulin resistance assessed by HOMA-IR | Overweight subjects recruited from the general public and lipid outpatient clinic | Bivariate Spearman's correlation | No correlation between 36-mo change in insulin resistance and RBP4 | Correlation between change in plasma RBP4 and HOMA-IR: Spearman's r = 0.06 |
| Mohlig et al., 2008 (54) | Cross-sectional study, n = 110 | ELISA | Insulin sensitivity as assessed by HOMA-S% | Women with PCOS | Bivariate Spearman's correlation | RBP4 was inversely correlated to insulin sensitivity | Correlation for RBP4 and insulin sensitivity: Spearman's r = –0.29 |
| Bahr et al., 2009 (55) | Case-control, 19 cases, 20 controls | ELISA validated against Western blotting | Insulin resistance assessed by HOMA-IR | 19 with liver cirrhosis and 20 healthy controls, the Netherlands | Bivariate Spearman's correlation | No correlations were observed for RBP4 and insulin resistance in patients with liver cirrhosis | Correlation for RBP4 and HOMA-IR: Spearman's r = –0.05 |
| Chavez et al., 2009 (56) | Cross-sectional, n = 72 | ELISA | Whole-body and hepatic insulin sensitivity, assessed by an oral glucose tolerance test and euglycemic insulin clamp | 16 lean subjects with normal glucose tolerance, 17 obese subjects with normal glucose tolerance, and 39 subjects with impaired glucose tolerance or T2DM, USA | Bivariate Pearson's or Spearman's correlation | No correlations were observed for glucose disposal or hepatic insulin resistance | Correlation of plasma RBP4 with whole-body and hepatic insulin resistance: r (method not given) = 0.06 and 0.07, respectively |
| Erikstrup et al., 2009 (35) | Cross-sectional study, n = 233 | HPLC-MS (retinol), ELISA (RBP4) | Impaired glucose tolerance and T2DM, ascertained by an oral glucose tolerance test | Subjects with normal and impaired glucose tolerance as well as persons with T2DM, Denmark | 3-factor ANOVA | Plasma concentration of RBP4 was lower among T2DM subjects compared with subjects with normal glucose tolerance. Plasma concentrations of retinol were lower among T2DM subjects compared with subjects with both normal and impaired glucose tolerance. The ratio of RBP4 to retinol was higher among subjects with T2DM compared with subjects with normal glucose tolerance | Mean difference in RBP4 normal glucose tolerance vs. T2DM: 0.16 µmol/L (0.02, 0.30).Mean difference in retinol normal glucose tolerance vs. T2DM: 0.34 µmol/L (0.18, 0.49); impaired glucose tolerance vs. T2DM: 0.24 µmol/L (0.02, 0.45). Mean difference in RBP4/retinol ratio, T2DM vs. normal glucose tolerance: 0.09 (0.05, 0.13) |
| Lee et al., 2009 (57) | Cross-sectional study, n = 111 | ELISA | Insulin resistance assessed by HOMA-IR | Men and women from the general population aged >70 y, South Korea | Bivariate Pearson's correlation | RBP4 was positively correlated to insulin resistance. Particularly strong associations were found among the obese | Correlation for RBP4 and insulin resistance: Spearman's r = 0.31 in the total population, r = 0.47 among obese, and r = 0.16 among nonobese |
| Xu et al., 2009 (58) | Case-control study, 1032 cases and 753 controls | ELISA validated against Western blotting | Impaired glucose tolerance and T2DM assessed/ascertained by fasting blood glucose and/or an oral glucose tolerance test | Of cases, 508 had impaired glucose tolerance and 524 had newly diagnosed diabetes, China | Logistic regression models adjusted for age, sex, current smoking, current alcohol intake, family history of diabetes, BMI, waist/hip ratio, HOMA-IR, estimated glomerular filtration rate, serum concentrations of triglycerides, total cholesterol, HDL, and LDL | RBP4 was associated with an increased risk of impaired glucose regulation and T2DM | OR of impaired glucose regulation and T2DM for 1 µg/mL increase in RBP4: 1.01 (1.0, 1.02) and 1.02 (1.01, 1.04), respectively |
| Suh et al., 2010 (59) | Cross-sectional study, n = 73 | ELISA | Insulin resistance assessed by fasting blood glucose and HOMA-IR | Women free of diabetes, South Korea | Univariate Pearson's correlation. Multivariable models adjusted for age and fasting insulin | RBP4 was positively correlated with fasting glucose and insulin resistance | Correlation of RBP4 with fasting glucose: Pearson's r = 0.52. Correlation of RBP4 with HOMA-IR in women >50 y: r = 0.40. β for RBP4 and HOMA-IR in total population: 0.88, SE: 0.25 |
| Ulgen et al., 2010 (60) | Cross-sectional, n = 70 | ELISA | Insulin resistance assessed by HOMA-IR | 70 nondiabetic obese subjects, Germany | Multivariable linear regression adjusted for age and sex | No associations were observed for RBP4 and insulin sensitivity | β for RBP4 and HOMA-IR: –0.048. SE not given |
| Meisinger et al., 2011 (61) | Cross-sectional study, n = 2614 | Nephelometry | Prediabetes assessed by an oral glucose tolerance test | 2122 participants with normal glucose tolerance, 110 with impaired fasting glucose, 313 with impaired glucose tolerance, and 69 with combined impaired fasting glucose and impaired glucose tolerance, Germany | Multivariable logistic regression adjusted for age, sex, education, hypertension, smoking, physical activity, alcohol intake, BMI, total cholesterol, and HbA1c | Increasing concentrations of RBP4 were positively associated with odds of prediabetes | OR of prediabetes in the upper quartile (concentrations not given for the total population) of RBP4: 1.63 (1.17, 2.27) |
| Luft et al., 2013 (62) | Nested case-control study, 543 cases, 537 controls | ELISA | Incident T2DM was ascertained by physician report, use of antidiabetic medications and/or fasting glucose | 543 cases who developed diabetes, 537 healthy controls, USA | Cox proportional hazards model adjusted for age, race/center indicators, ethanol intake, ethanol intake2, smoking, BMI, BMI2, waist-to-hip ratio, estimated glomerular filtration rate, inflammation score, concentrations of adiponectin, leptin, triglycerides, triglycerides2, HDL, and nonesterified fatty acids, hypertension, family history of diabetes, serum insulin, and plasma glucose | Overall, there were no associations between RBP4 and incident diabetes. However, an interaction by sex was observed and an association was detected among women | Overall HR for T2DM: 3rd vs. 1st tertile of RBP4: 1.31 (0.82, 1.92). HR for T2DM in women: 3rd tertile (30.3–70.0 g/mL) vs. 1st tertile (8.8–23.9 g/mL): 1.74 (1.03, 2.94). HR for T2DM in men: 3rd tertile (35.2–52.9 g/mL) vs. 1st tertile (12.8–28.1 g/mL): 0.94 (0.51, 1.73) |
| Sun et al., 2014 (63) | Prospective cohort study, n = 2091 | ELISA | Incident T2DM ascertained by self-reported doctor-diagnosed T2DM or use of antidiabetic medication or assessment of fasting blood glucose at follow-up visit | The Nutrition and Health of Aging Population in China, general population aged 50–70 y | Sequential logistic regression adjusted for sex, age, region, residence, education, smoking, alcohol intake, physical activity, family history of diabetes, BMI, CRP, concentrations of adiponectin, triglycerides, HDL, γ-glutamyl transpeptidase and creatinine, HOMA-IR, hypertension, ferritin, blood fatty acids, intakes of total energy, fat, heme iron and retinol | Concentrations of RBP4 associated with risk of incident T2DM | RR of T2DM in the 4th (> 46.1 µg/mL) vs. 1st quartile (< 31.3 µg/mL) of RBP4: HR: 1.48 (1.06, 2.03) |
All effect measures are given as HR/OR/RR (95% CIs) unless otherwise noted.
CRP, C-reactive protein; EIA, enzyme immunoassay; HOMA-S%, homeostatic model assessment of insulin sensitivity; PCOS, polycystic ovary syndrome; RBP4, retinol-binding protein 4; T2DM, type 2 diabetes mellitus; UPLC, ultra-performance liquid chromatography.
Retinol, retinoic acid, insulin resistance, and T2DM
Although relatively scarce, some observational studies have assessed the relation between retinol and retinoic acid and diabetes. One case-control study found that serum retinol concentrations were normal in patients with T2DM and did not differ substantially from healthy controls (37). In a study where >900 subjects underwent an oral-glucose-tolerance test, insulin resistance did not differ by retinol quartiles (38). In contrast, 1 case-control study including subjects free of diabetes, but with impaired glucose tolerance, reported higher serum concentrations of retinol in cases compared with healthy controls with normal glucose tolerance (2.5 compared with 2.1 µmol/L) (36). More recently, a prospective case-control study examining metabolomic signatures including 55 prediabetic women and 220 healthy controls reported that several aspects of vitamin A metabolism were positively associated with 7-y incidence of T2DM (39). Using machine-learning techniques, the authors identified plasma retinyl esters, retinaldehyde, all-trans retinoic acid, and 4-hydroxy retinoic acid (a retinoic acid degradation product) as positively associated with incident T2DM. In addition, a high ratio of retinoic acid to retinaldehyde (≥2.76) was associated with a doubling in the 7-y risk of developing T2DM compared to those with a ratio ≤2.76. Adding the ratio to a predictive model including baseline fasting glucose, age, and γ-glutamyl transpeptidase increased the area under the receiver-operating characteristic curve from 0.809 to 0.840, indicating improved prediction of incident T2DM.
Collectively, the few studies that have been performed on retinol, retinoic acid, and diabetes are somewhat conflicting. One reason for the discrepancies observed between studies may be that serum retinol concentrations in established diabetes may be affected by increased urinary excretion observed in diabetic nephropathy (64).
RBP4, insulin resistance, and T2DM
One of the first human studies suggesting a role for RBP4 in insulin resistance and diabetes was published in 1999 (37). Although no effect sizes were given, this cross-sectional study reported that RBP4 concentrations were higher among cases with T2DM than in healthy controls. Later, a study published in the New England Journal of Medicine by Graham et al. reported that RBP4 correlated strongly with fasting insulin (Spearman's r = 0.72) and glucose disposal rate (r = –0.78) in a relatively small sample of subjects with either T2DM, impaired glucose tolerance, or obesity (41). This finding was succeeded by a considerable amount of research in human subjects that observed a positive association between RBP4, insulin resistance, and T2DM (40, 42–44, 46–48, 54, 57–59, 61) as well as candidate single nucleotide polymorphisms in Rbp4 associated with T2DM (65–68). The effect sizes initially reported by Graham in 2006 were large, whereas later studies found effects that were much more modest in size (see Table 2 for details). One explanation for these discrepant findings may be that the populations under study vary widely based on health condition, sample size, study type (cross-sectional or case-control), and the ethnicity of the included populations.
Some studies also report null or weak associations between RBP4 and insulin resistance (45, 49, 51, 56, 60) in different patient groups such as CAD (49), liver cirrhosis (55), and polycystic ovary syndrome (50, 52). Although it is plausible that the effects of RBP4 may vary with patient group, it should be pointed out that the studies showing null or weak findings generally enrolled fewer subjects (n <100) and may not be large enough to detect relevant effects. Another challenge with the research on the RBP4-T2DM association includes the lack of prospective data. However, in recent years, 2 longitudinal studies with 6 and 9 y of follow-up indicated that baseline concentrations of RBP4 were associated with incident T2DM independently of several other risk factors. Specifically, a nested case-control study enrolling 1080 subjects from the Atherosclerosis Risk in Communities cohort reported a 43% increased risk of incident diabetes in women, whereas results were less clear in men (62). In a Chinese population consisting of 2091 men and women aged between 50 and 70 y, subjects in the upper RBP4 quartile had a 48% increased risk of developing T2DM compared with subjects in the first quartile (63). In contrast, 1 prospective study with 3 y of follow-up showed that although insulin resistance increases over time in 206 obese subjects, RBP4 does not (53). This particular finding indicates that the association between insulin resistance and RBP4 may be confounded by other factors such as kidney function, which has previously been reported (69–74). On a final note, some pharmacological interventions for the treatment of T2DM and insulin resistance have demonstrated a concomitant decrease in RBP4 (48, 75, 76), but no drugs or trials have been designed to specifically target RBP4.
As for CVD, an important distinction that has yet to be fully elucidated is the potential differing effects of holo- and apo-RBP4 in the etiology of insulin resistance. Two studies have assessed this relation by utilizing either the ratio of retinol to RBP4 (77) or the ratio of RBP4 to retinol (35) in circulation, both of which indicate the relative amount of holo- and apo-RBP4. The retinol: RBP4 ratio was indeed lower in obese subjects (77). In addition, it was shown that although both total RBP4 and retinol were lower among patients with T2DM compared with healthy controls, the RBP4: retinol ratio was higher among these patients (35). Collectively, these studies indicate that RBP4 may exert effects independently of retinol.
Vitamin A and obesity
As for insulin resistance and T2DM, interest in metabolites related to vitamin A and obesity have mainly been centered on RBP4 in recent years. However, some evidence from human studies relating retinol to obesity also exist, although this relation is currently not clear. The studies discussed in this section are summarized in Table 3.
TABLE 3.
| First author and year | Study type and n | Method for quantification | Endpoint assessment | Population and country | Statistical methods and models | Main finding | Effect measure and size |
|---|---|---|---|---|---|---|---|
| Studies on retinol | |||||||
| Hogstrom et al., 2008, (78) | Prospective study, n = 73 | HPLC (retinol), radial immunodiffusion (RBP4) | Abdominal fat mass, assessed by DXA | Healthy Caucasian males, Sweden | Bivariate Pearson's correlations | Both retinol and RBP4 were correlated with abdominal fat mass | Correlation for retinol and RBP4 with abdominal fat mass: r = 0.22 and 0.26, respectively |
| Mills et al., 2008 (77) | Case-control, 76 cases, 41 controls | HPLC (retinol), ELISA (RBP4) | Body composition, assessed by BMI | Obese and nonobese men and women, USA | 1-factor ANOVA | The ratio of retinol to RBP4 was lower in obese compared with nonobese | No effect sizes given |
| Botella-Carretero et al., 2010 (79) | Cross-sectional study, n = 80 | HPLC | Morbid obesity, assessed by BMI | Caucasian patients with morbid obesity, Spain | Backwards stepwise linear regression ultimately including only BMI and male sex | Retinol was inversely associated with BMI | β-coefficient for the relation between BMI and retinol: –0.23 |
| Kanagasabai et al., 2019 (80) | Cross-sectional study, n = 2049 | HPLC | Metabolic syndrome criteria including BMI assessed at baseline visits, methods for ascertainment not given | Data from NHANES, general population, USA | ANOVA for between-group differences in retinol. Logistic regression adjusted for age, sex, ethnicity, education, income, smoking, alcohol intake, recreational physical activity, and BMI | Retinol was not associated with BMI alone, but with metabolic syndrome | No effect sizes given for retinol and BMI. Having retinol beyond a clinical reference range (details not given) was associated with increased odds of the metabolic syndrome: weighted OR: 2.10 (1.50, 2.92) |
| Studies on RBP4 | |||||||
| Haider et al., 2007 (81) | Nonrandomized intervention, n = 47 | ELISA | Change in body composition, assessed by BMI | 33 morbidly obese that underwent gastric banding surgery and 14 healthy subjects, Austria | Not specified | RBP4 was higher in morbidly obese compared with controls and decreased after surgery | No effect sizes given for difference between morbidly obese and controls at baseline. 6-mo weight loss decreased RBP4 by –0.7 +/- 0.6 |
| Jia et al., 2007 (76) | Cross-sectional study, n = 1033 and single- arm intervention with rosiglitazone in diabetic patients, n = 22 | RIA | Visceral fat mass, assessed by MRI | Han Chinese population with normal and impaired glucose tolerance as well as T2DM subjects. The single-arm intervention included men and women with newly diagnosed T2DM | Partial Spearman rank correlation adjusted for HOMA-IR. Treatment effect assessed by Wilcoxon signed rank test | Serum RBP4 was positively correlated to visceral fat mass in men and women. Rosiglitazone treatment reduced visceral fat mass and RBP4 | Correlation of RBP4 with visceral fat mass in men and women: Spearman's r = 0.17 and 0.22, respectively. No effect sizes given for the intervention |
| Klöting et al., 2007 (82) | Cross-sectional study, n = 196 | — | RBP4 mRNA assessed by qPCR in visceral and subcutaneous tissue | Lean and obese subjects, Germany | t-test | RBP4 mRNA was expressed to a greater extent in the visceral and subcutaneous adipose tissue of obese compared with lean subjects | No effect sizes for differences given |
| Lee et al., 2007 (83) | Cross-sectional study, n = 102 | EIA | Visceral fat mass, measured by DXA and CT | Healthy women aged between 21 and 67 y, South Korea | ANOVA and bivariate Pearson's correlation | RBP4 was higher among both nonobese and obese with visceral obesity compared with their counterparts without visceral adiposity. Nonobese with visceral obesity had higher concentrations of RBP4 than obese without visceral adiposity. Positive correlation between RBP4 and visceral fat mass measured by CT | No effect sizes given for comparisons. RBP4 was positively associated with visceral fat mass measured by CT: Pearson's r = 0.5 |
| Bajzova et al., 2008 (84) | Cross-sectional study, n = 59 | — | RBP4 mRNA assessed by qPCR in visceral and subcutaneous tissue | Caucasian women with BMI between 20 and 49 kg/m2, Czech Republic | t-test and bivariate Pearson's correlation | RBP4 was lower in visceral compared with subcutaneous fat and did not differ between subgroups according to BMI category. RBP4 mRNA was correlated with visceral fat content | Only P values and no effect sizes given. RBP4 mRNA correlated positively with visceral fat in the total population (Pearson's r: 0.35) |
| Tschoner et al., 2008 (85) | Nonrandomized single- arm intervention, n = 36 | ELISA | Body adiposity, assessed by waist circumference and visceral fat diameter determined by ultrasound | 36 morbidly obese undergoing bariatric surgery, Austria | ANOVA and bivariate Spearman's correlations | RBP4 decreased from before to 2 y after surgery. The change in RBP4 was positively correlated to change in waist circumference and visceral fat diameter | No effect sizes given for differences. Correlation of change in RBP4 with change in waist circumference and visceral fat diameter: Spearman's r = 0.36 and 0.42, respectively |
| Huang et al., 2012 (86) | Cross-sectional study, n = 709 | Western blotting | Body composition, assessed by BMI and waist circumference | Postmenopausal women, USA | Spearman's correlation adjusted for age, race, and smoking | No correlation between RBP4 and BMI or waist circumference | Correlation of RBP4 with BMI and waist circumference: Spearman's r = 0.02 and 0.04, respectively |
| Chang et al., 2015 (87) | Cross-sectional study, n = 106 | ELISA validated against Western blotting | Visceral fat, assessed by CT | Patients with nonalcoholic fatty liver disease, China | Stepwise linear regression adjusted for HDL | Visceral fat content was associated with serum RBP4 | Association of visceral fat with RBP4: Standardized β = 0.36. SE not given |
| Zachariah et al., 2017 (88) | Cross-sectional (n = 3777) and prospective cohort study (n = 2208) | ELISA | Overweight, obesity, and metabolic syndrome assessed by clinical examinations and existing definitions | Framingham Third Generation Cohort including subjects free of metabolic syndrome, USA | Logistic regression adjusted for age, sex, BMI, sex-standardized waist circumference, systolic and diastolic blood pressure, concentrations of HDL, glucose, and triglycerides | RBP4 was higher among overweight subjects and was associated with incident metabolic syndrome | No effect sizes given for differences. Subjects in the 4th quartile vs. 1st of log-transformed RBP4 had increased odds of metabolic syndrome: OR: 1.75 (1.12, 2.78) |
| Korek et al., 2018 (89) | Case-control study, 28 cases, 25 controls | ELISA | Obesity, assessed by BMI | Cases with obesity and no comorbidities, lean and healthy controls, Poland | Not specified | RBP4 concentrations were not different between cases or controls | No effect sizes given |
All effect measures are given as HR/OR (95% CIs) unless otherwise noted.
CT, computed tomography; EIA, enzyme immunoassay; RBP4, retinol-binding protein 4; RIA, radio immunoassay; T2DM, type 2 diabetes mellitus.
Retinol and obesity
One study comparing obese and nonobese subjects found no differences in circulating retinol between the 2 groups (77). Among 78 healthy males, serum retinol concentrations were moderately and positively correlated to abdominal fat mass (Pearson's r = 0.22) (78). In contrast, in a cohort of 85 morbidly obese subjects where the majority had nonalcoholic fatty liver disease, BMI was reported as a negative predictor of serum retinol (β per unit increase in BMI = –0.23) (79). This discrepancy is not surprising, considering that liver injury can impair the hepatic storage capacity of retinol and lead to lower circulating concentrations (90). Finally, 1 recently published study from the NHANES population showed that although serum retinol did not increase with increasing BMI, it increased with the number of metabolic syndrome criteria (80). In addition, serum retinol concentrations above clinical reference ranges that were not defined in the publication doubled the odds of having metabolic syndrome. Thus, the association of retinol with obesity remains elusive, but may depend on underlying disease (liver) or other conditions (metabolic syndrome).
RBP4 and obesity
Several human studies have shown that RBP4 concentrations in blood are related to body fat and differentially associated with various body fat compartments. One study among 196 participants reported that RBP4 is expressed at higher levels in visceral fat compared with subcutaneous fat depots and concluded that RBP4 may be a marker of intra-abdominal fat mass (82). This pattern has also been observed in epidemiological studies: a study among >1000 Chinese subjects reported that RBP4 concentrations were not associated with BMI but positively yet weakly correlated to visceral body fat among men (Spearman's r = 0.17) and women (Spearman's r = 0.22), respectively (76). In a population with nonalcoholic fatty liver disease, a positive and moderate association was observed for visceral fat and circulating RBP4 (SD increase in RBP4 per SD increase in visceral fat = 0.36), whereas no associations were observed for subcutaneous or hepatic fat (87). In 102 healthy women, RBP4 concentrations were strongly and positively correlated to visceral fat mass as measured by computed tomography (age and BMI-adjusted Pearson's r = 0.50), but not with total body fat as measured by DXA (age and BMI-adjusted Pearson's r = 0.02) (83). In 200 women with polycystic ovary syndrome, serum RBP4 concentrations were weakly but positively correlated to both BMI and waist circumference, which is a commonly used proxy for intra-abdominal fat (44). In addition, RBP4 was moderately and positively correlated to abdominal fat mass among healthy Caucasian males (Pearson's r = 0.26) (78).
Further strengthening the association between RBP4, fat mass, and obesity, some studies have shown that serum RBP4 responds to weight loss. Although no effect sizes were given, pharmacological treatment with rosiglitazone that resulted in visceral body fat reductions concomitantly reduced RBP4 (76). One study among morbidly obese individuals (BMI ∼46) that underwent gastric bypass showed that serum RBP4 concentrations were reduced 6 mo after surgery (81). Moreover, the reduction in waist circumference and visceral body fat after bariatric surgery in 36 subjects correlated positively with reductions in serum RBP4 (Spearman's r = 0.36 and 0.42, respectively) (85). In a prospective study among 2208 subjects in the Framingham Third Generation Cohort, participants in the 4th quartile of log-transformed serum RBP4 had a 75% increased risk of metabolic syndrome compared with those in the 1st quartile (88). Although these results seem convincing, not all studies show a positive association of RBP4 with obesity and/or fat mass. One study among 49 women with a BMI ranging from 20 to 49 kg/m2 found lower expression of RBP4 in visceral compared with subcutaneous fat depots and no association between serum RBP4 and adiposity (no effect sizes given) (84). In a cross-sectional study among 709 healthy postmenopausal women, serum RBP4 concentrations were not associated with either BMI or waist circumference (86), and 1 small case-control study found no relevant difference in serum RBP4 among obese compared with nonobese controls (89). Collectively, most, but not all, data point towards a meaningful association between RBP4 and particularly visceral fat mass.
Conclusion
Summary
The association between compounds related to vitamin A and lifestyle-related diseases have mainly focused on RBP4 in recent years. Considering the essential role of RBP4 in vitamin A metabolism, it is important to establish whether vitamin A metabolites show similar or discrepant associations with lifestyle diseases. In this review we show that both retinol and retinoic acid have been linked to common lifestyle diseases. Briefly, retinol has been both positively and negatively associated with CVD (13, 15–18, 21), T2DM (39), and the metabolic syndrome (80), and emerging evidence suggests that retinol can modify the relation of other common risk factors with CVD (19, 20). Less work has focused on circulating concentrations of retinoic acid and disease outcomes, but observational data indicate that it is inversely related to CVD in particular (22, 23), whereas the association with T2DM is less clear (39). For RBP4, the associations with T2DM (40–44, 46–48, 54, 57–59, 61–63, 65–68, 75, 91, 92) and obesity (44, 76, 78, 81–83, 85, 87, 88) are largely positive, although null findings and contrasting observations have been reported for these outcomes (45, 49–53, 55, 56, 60, 86, 89, 91). Finally, more evidence on the association between RBP4 and CVD is emerging (11, 24–30).
A note on interpretation
Study design and analysis
Several challenges remain in the interpretation of the findings in this review. In general, there was a greater tendency of smaller studies showing null or neutral results, indicating that power is an issue, particularly for case-control and cross-sectional studies (15, 36, 40, 41, 43, 45, 47, 50–52, 55, 56, 59, 60, 79, 78, 81, 84–86, 89). Most studies used adequate clinical endpoints (both surrogate and hard endpoints), but some lack rigorous reporting of results, omitting effect sizes and reporting P values only, which limits comparability. In addition, several studies categorized plasma/serum concentrations of metabolites into various quantiles which limits interpretability and generalization because the resulting cut-offs vary greatly from study to study. For example, the upper quartile cut-off for serum RBP4 in (26) was >57.8 µg/mL whereas it was >37.2 µg/mL in (28), making it difficult to compare findings because the definitions of e.g. “high” RBP4 were not consistent. Related to this, the choice of statistical methods used to obtain estimates or P values was not always adequately justified—or even specified—in the text (See Tables 1 –3 for details). For instance, several studies used data-driven methods for the building of multivariable models, and some studies reported only bivariate relations without adjusting for potential confounding factors both of which can introduce substantial bias (93). Finally, no studies reporting correlational analyses (i.e. Pearson's or Spearman's r) presented CIs and thus gave no indication of effect estimate uncertainty. These issues can limit the inference and interpretability of the reported observations.
Analytical considerations for RBP4
As exemplified by (83), measurement instruments may affect the precision of the observed associations, particularly for RBP4 and obesity. In addition, Graham et al. identified several drawbacks in the determination of plasma RBP4 among subjects with impaired glucose tolerance (94). Specifically, they reported that commercially available ELISA kits of various origin overestimate plasma concentrations of RBP4 in normoglycemic subjects, and underestimate RBP4 in subjects with impaired glucose tolerance compared with quantitative Western blotting. The lack of standardized and validated methods of quantification may introduce significant bias to the measurements and consequently impact results. The authors further recommend quantitative Western blotting as the gold standard of measuring RBP4 or that other methods are validated against Western blotting to ensure accurate measurements. Of the studies included in this review on the relation between RBP4 and insulin resistance, 2 studies used Western blotting to quantify RBP4 (41, 52), 4 studies used ELISA assays that were validated against Western blotting (46, 49, 51, 58), 3 studies used nephelometry (42, 45, 61), whereas the remainder of the studies used ELISA or other enzyme immunoassays for quantification (40, 43, 44, 47–50, 53–57, 59, 60, 62, 63). The discrepancies in the analytical methods used may introduce systematic bias that limits comparability and give biased results. Finally, although similar comparisons have not been performed for populations with CVD or obesity, the analytical challenges observed for RBP4 in subjects with impaired glucose tolerance may well apply to other populations and should be considered when interpreting these studies.
Future considerations and knowledge gaps
The interplay between RBP4, retinol, and retinoic acid
The data presented in this review suggest several knowledge gaps that need to be bridged and potential future research questions to be answered in order to advance our understanding of vitamin A in CVD, T2DM, and obesity (Table 4). One intriguing question is that although RBP4 and retinol are thought to circulate in a nearly 1:1 manner, RBP4 is more frequently and more strongly related to adverse disease outcomes. Specifically, RBP4 circulates in the body bound to retinol [holo-RBP4 (85%)], whereas the remaining portion circulates as apo-RBP4 (95), but it has not been resolved whether total RBP4 or 1 of its fractions (holo- or apo-RBP4) is the main culprit in associating with CVD, T2DM, and obesity. Furthermore, it is not known whether the effect of RBP4 is mediated through retinol or retinoic acid signaling. One study included in this review that provides some insight is the study by Liu et al. (26), where they used experimental methods to back-up their observational findings and demonstrated that apo-RBP4 can induce scavenging of oxidized LDL particles by macrophages and induce foam cell formation, a critical feature of atherosclerotic progression (96–98). However, evidence from patients with T2DM suggests that total RBP4 can reduce clearance of proatherogenic lipoprotein particles, indicating that both holo- and apo-RBP4 can exert adverse effects (99). Thus, it is difficult to ascertain whether RBP4 acts alone or in conjunction with vitamin A metabolites. One example that argues against the involvement of retinol and retinoic acid signaling in e.g. CVD is that some target genes of retinoic acid include the ATP-binding cassette A1 (100), which regulates cholesterol efflux from macrophages to HDL particles and is a process that is considered antiatherogenic (101). Moreover, a review has highlighted several potentially beneficial effects of retinoic acid signaling on the vasculature (102), and observational studies included in this review reported that circulating retinoic acid is inversely related to CVD outcomes (22, 23). Thus, these seemingly discrepant effects of RBP4 and retinol/retinoic acid on adverse health outcomes indicate that the effects associated with RBP4 may not involve retinol delivery to tissues and subsequent retinoic acid signaling. On the other hand, it is not certain that retinol and retinoic acid are mere innocent bystanders in this context as suggested by: 1) the study showing that products of retinol metabolism and signaling were prospectively related to the development of T2DM (39), 2) the partly positive association of retinol with incident CVD mortality (18) and metabolic syndrome (80), 3) our recent findings that serum retinol can modify the effects of common risk factors on CVD development (19, 20) and finally, 4) that pharmacological treatment with retinoic acid isoforms induce dyslipidemia (31, 32) and homocysteinemia (33), which are common risk factors for CVD in particular. Whether these potentially adverse effects of retinol and retinoic acid include RBP4 is currently not known although it has been proposed that the RBP4-retinol complex is involved in signaling pathways that are implicated in insulin resistance (103). In any case, whether RBP4 acts alone or mediates some of its effects through vitamin A metabolism remains an intriguing question in need of resolution in order to advance our understanding of vitamin A in the development of lifestyle diseases such as CVD, T2DM, and obesity.
TABLE 4.
Potential future research objectives
| Retinol-binding protein 4 | Establish if observed associations are causal |
| Establish if effects occur independently of vitamin A metabolism at large | |
| Retinol | Establish if disease associations observed for serum retinol are present for more sensitive markers of vitamin A status, including retinol isotope dilution |
| Replicate findings that retinol can interact with other risk factors, and establish if interactions occur independently of confounders, particularly inflammation | |
| Establish whether deficient vitamin A status contributes to the growing burden of lifestyle diseases in low- to middle-income countries | |
| Retinoic acid | Evidence on the link between retinoic acid and major lifestyle diseases is lacking. More studies are needed in order to establish associations |
| Establish standardized methods that accurately capture retinoic acid concentrations | |
| Establish clinical relevance |
Serum retinol—new hypotheses and old challenges
The finding that retinol can modify the risk relation of common risk factors such as apoB and total homocysteine with CVD has currently only been undertaken in patients with established CVD (19, 20). Although these findings suggest that there may be subgroups in the population with CVD where elevated retinol concentrations can be particularly harmful, the interaction of retinol with common risk factors of CVD and other diseases should be evaluated in other, preferably healthy cohorts. It would also be useful to assess whether these interactions are also present for RBP4 and retinoic acid in humans, especially considering there is data linking RBP4 to lipoprotein metabolism (11, 26, 99, 104) and retinoic acid to homocysteine metabolism (105–110).
Another issue in need of resolution is whether retinol is reflective of vitamin A, or whether the somewhat conflicting disease associations are results of confounding. Liver vitamin A stores are considered the gold standard for vitamin A status assessment (3, 4), but due to the difficulty of obtaining liver samples, other measures are regularly considered including serum retinol and retinol isotope dilution. Although serum retinol responds to deficient intake over time, Olson showed in 1984 that concentrations are generally kept under tight homeostatic control (111), and high-dose supplementation over time did not increase serum retinol (112). Utilization of serum retinol as a measure of vitamin A status can thus be problematic in affluent societies were vitamin A deficiency is not a major concern. The retinol isotope dilution method correlates strongly with liver stores (3, 4), and is indicative of vitamin A status both in deficiency and excess (4). However, no studies included in this review used this method for assessment of vitamin A status, and it is difficult to ascertain whether vitamin A status in itself was associated with disease, or if serum retinol concentrations and outcomes were influenced by other factors that confounded the observed disease associations. Notably, we have recently reported that strong determinants of retinol in circulation include serum creatinine, the sulfur amino acid cysteine, and some inflammatory markers, all of which are related to 1 or several lifestyle diseases (113) and are potential sources of confounding. Thus, in order to increase our understanding of whether vitamin A status is truly involved in underlying pathological mechanisms for major lifestyle diseases such as CVD, T2DM, and obesity, more sensitive markers of status, such as retinol isotope dilution, should be considered in the design and implementation of future studies.
On a final note, findings indicating that low serum retinol can increase the risk of CVD presents developing countries with a new public health challenge where vitamin A deficiency still prevails (15, 18). There is little data available addressing serum retinol and major lifestyle diseases in developing countries, but considering that the incidence of CVD, T2DM, and obesity is increasing, these countries are now increasingly faced with a double burden of disease (114, 115). Future epidemiological investigations in these populations must therefore take care to identify and adjust for appropriate confounding factors, as an association may arise simply due to the prevalence of both phenomena in these countries.
Disease, inflammation, and concurrent effects on retinol and RBP4
It is a well-established concept that inflammation can have profound effects on vitamin A metabolism, as reviewed extensively in (116, 117). Briefly, during the acute-phase response, serum concentrations of RBP4 diminish quickly, as do serum retinol as it binds to RBP4 in a nearly 1:1 molar ratio. The decline in RBP4 and serum retinol is attributed to reduced hepatic RBP4 synthesis and consequently reduced retinol transport capacity in circulation. Thus, the presence of inflammation can disrupt vitamin A homeostasis and falsely indicate vitamin A deficiency even if body stores are adequate (118). Lifestyle diseases including CVD, T2DM, and obesity are accompanied by chronic unresolved low-grade inflammation (119), which can theoretically influence vitamin A metabolism in these conditions. However, as highlighted in the present review, RBP4 concentrations are often elevated particularly in T2DM and obesity, and some studies even show weak but positive associations between RBP4 and C-reactive protein (CRP) in these conditions (30, 46, 48, 120). The data are less clear for retinol. It has been recommended that retinol concentrations should be adjusted for CRP concentrations in the presence of inflammation (118, 121), but no studies included in this review applied this adjustment. We note that decreases in RBP4 and retinol are usually seen at CRP concentrations exceeding 5–10 mg/L (118, 121), and of the studies included in the present review, many did not report CRP (13–15, 21, 27, 28, 36–45, 47, 49, 57, 59, 61, 61, 53, 55, 79, 78, 84, 85, 87, 89), only 4 showed that CRP exceeded 5 mg/L (23, 29, 51, 82), and 1 study reported that CRP exceeded 10 mg/L (86). It is thus difficult to ascertain whether the presence of low-grade inflammation present in CVD, T2DM, and/or obesity significantly affected serum RBP4 and retinol in these studies.
More research is needed on retinoic acid and disease
On a final note, from this work it seems clear that the associations of retinoic acid and diseases remain largely unexplored in human observational studies. There may be several reasons for this, 1 of which may be that retinoic acid determination requires highly sensitive and costly methods. Indeed, retinoic acid concentration in circulation is severalfold lower than abundant retinoids such as retinol, retinyl esters, and RBP4 (122). For example, there are still doubts that 9-cis retinoic acid is an endogenous ligand for retinoic X receptors in part because it is difficult to detect (12, 123). Thus, the quantification of all-trans retinoic acid and its isomers depends on highly sensitive assays that may be less cost-effective than the measurement of e.g. retinol. Thus, resource limitations may have played a significant role in assessing retinoic acid-disease relations. Another challenge is the potential within-person and between-person variability for retinoic acid. For example, it has been demonstrated that all-trans retinoic acid concentrations are subject to diurnal variation (124), and thus becomes notoriously difficult to measure accurately in a convenience sample (e.g. in patients admitted to a hospital at any time of day). The measurement error introduced by this variability may bias analyses and perhaps cause neutral findings to be discarded and unpublished, and it is difficult to establish disease associations unless highly standardized methods are used to account for this variation.
Outside experimental evidence showing that retinoic acid signaling may play an important role in the development of metabolic disease (12, 102), very few human studies have explored the relation between circulating retinoic acid concentrations and disease development in humans. However, 2 studies included in this review reported that all-trans retinoic acid concentrations were inversely associated with CVD outcomes (22, 23). Taken together, the methodological challenges summarized in the above paragraph and the promising findings on circulating retinoic acid and incident CVD, merits future studies to further elucidate and clarify the retinoic acid-disease association and establish clinical relevance.
Conclusions
The studies included in this review suggests that retinol, retinoic acid, and RBP4 are differentially associated with CVD, T2DM, and obesity. Although RBP4 concentrations are generally positively associated with CVD, T2DM, and obesity, retinol and retinoic acid show contrasting associations with lifestyle disease outcomes. Published studies largely focus on RBP4, and only a few of these studies include retinol measurements, and none include data on retinoic acid. Based on this imbalance in the literature, more observational evidence focusing on a broader aspect of vitamin A metabolism is warranted to ascertain whether RBP4 acts by itself or mediates effects through retinol metabolism and retinoic acid signaling. Some remaining challenges include: 1) utilizing more sensitive markers of vitamin A status to determine whether retinol in particular is truly associated with disease, 2) analytical and methodological considerations of retinoic acid and RBP4, and 3) more longitudinal studies for assessment of disease associations. Finally, potential interactions of retinol, retinoic acid, and RBP4 with common risk factors including lipid parameters and total homocysteine should be explored in relation to incident disease outcomes.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—TO: conceived the idea and drafted the manuscript; and both authors revised, read, and approved the final version of the manuscript.
Notes
Supported by the Institute of Medical Biosciences, University of Oslo, Oslo, Norway
Author disclosures: RB has a commercial interest in A/S Vitas, Norway. TO has no conflicts of interest.
Abbreviations used: CAD, coronary artery disease; CRP, C-reactive protein; CVD, cardiovascular disease; RBP4, retinol-binding protein 4; T2DM, type 2 diabetes mellitus.
References
- 1. Blomhoff R, Blomhoff HK. Overview of retinoid metabolism and function. J Neurobiol. 2006;66(7):606–30. [DOI] [PubMed] [Google Scholar]
- 2. Balmer JE, Blomhoff R.. Gene expression regulation by retinoic acid. J Lipid Res. 2002;43(11):1773–808. [DOI] [PubMed] [Google Scholar]
- 3. Tanumihardjo SA. Vitamin A: biomarkers of nutrition for development. Am J Clin Nutr. 2011;94(2):658S–65S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tanumihardjo SA, Russell RM, Stephensen CB, Gannon BM, Craft NE, Haskell MJ, Lietz G, Schulze K, Raiten DJ. Biomarkers of Nutrition for Development (BOND) – vitamin A review. J Nutr. 2016;146(9):1816S–48S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sommer A, Tarwotjo I, Djunaedi E, West KP Jr, Loeden AA, Tilden R, Mele L. Impact of vitamin A supplementation on childhood mortality. A randomised controlled community trial. Lancet. 1986;1(8491):1169–73. [DOI] [PubMed] [Google Scholar]
- 6. Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2017;3:CD008524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wirth JP, Petry N, Tanumihardjo SA, Rogers LM, McLean E, Greig A, Garrett GS, Klemm RD, Rohner F. Vitamin A supplementation programs and country-level evidence of vitamin A deficiency. Nutrients. 2017;9(3):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bird JK, Murphy RA, Ciappio ED, McBurney MI. Risk of deficiency in multiple concurrent micronutrients in children and adults in the United States. Nutrients. 2017;9(7):pii:E655. doi: 10.3390/nu9070655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wolf G. Serum retinol-binding protein: a link between obesity, insulin resistance, and type 2 diabetes. Nutr Rev. 2007;65(5):251–6. [DOI] [PubMed] [Google Scholar]
- 10. Mody N. Alterations in vitamin A/retinoic acid homeostasis in diet-induced obesity and insulin resistance. Proc Nutr Soc. 2017;76(4):597–602. [DOI] [PubMed] [Google Scholar]
- 11. Zabetian-Targhi F, Mahmoudi MJ, Rezaei N, Mahmoudi M. Retinol binding protein 4 in relation to diet, inflammation, immunity, and cardiovascular diseases. Adv Nutr. 2015;6(6):748–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blaner WS. Vitamin A signaling and homeostasis in obesity, diabetes, and metabolic disorders. Pharmacol Ther. 2019;197:153–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. De Keyser J, De Klippel N, Merkx H, Vervaeck M, Herroelen L. Serum concentrations of vitamins A and E and early outcome after ischaemic stroke. Lancet. 1992;339(8809):1562–5. [DOI] [PubMed] [Google Scholar]
- 14. Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH et al.. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334(18):1150–5. [DOI] [PubMed] [Google Scholar]
- 15. Bobbert T, Raila J, Schwarz F, Mai K, Henze A, Pfeiffer AF, Schweigert FJ, Spranger J. Relation between retinol, retinol-binding protein 4, transthyretin and carotid intima media thickness. Atherosclerosis. 2010;213(2):549–51. [DOI] [PubMed] [Google Scholar]
- 16. Gey KF, Ducimetiere P, Evans A, Amouyel P, Arveiler D, Ferrieres J, Luc G, Kee F, Bingham A, Yarnell J et al.. Low plasma retinol predicts coronary events in healthy middle-aged men: the PRIME Study. Atherosclerosis. 2010;208(1):270–4. [DOI] [PubMed] [Google Scholar]
- 17. Brazionis L, Walker KZ, Itsiopoulos C, O'Dea K. Plasma retinol: a novel marker for cardiovascular disease mortality in Australian adults. Nutr Metab Cardiovasc Dis. 2012;22(10):914–20. [DOI] [PubMed] [Google Scholar]
- 18. Min KB, Min JY.. Relation of serum vitamin A levels to all-cause and cause-specific mortality among older adults in the NHANES III population. Nutr Metab Cardiovasc Dis. 2014;24(11):1197–203. [DOI] [PubMed] [Google Scholar]
- 19. Olsen T, Vinknes KJ, Svingen GFT, Pedersen ER, Tell GS, Blomhoff R, Drevon CA, Ueland PM, Midttun O, Refsum H et al.. Cardiovascular disease risk associated with serum apolipoprotein B is modified by serum vitamin A. Atherosclerosis. 2017;265:325–30. [DOI] [PubMed] [Google Scholar]
- 20. Olsen T, Vinknes KJ, Svingen GF, Pedersen ER, Dhar I, Tell GS, Blomhoff R, Ueland PM, Midttun O, Refsum H et al.. The risk association of plasma total homocysteine with acute myocardial infarction is modified by serum vitamin A. Eur J Prev Cardiol. 2018;25(15):1612–20. [DOI] [PubMed] [Google Scholar]
- 21. Yu Y, Zhang H, Song Y, Lin T, Zhou Z, Guo H, Liu L, Wang B, Liu C, Li J et al.. Plasma retinol and the risk of first stroke in hypertensive adults: a nested case-control study. Am J Clin Nutr. 2019;109(2):449–56. [DOI] [PubMed] [Google Scholar]
- 22. Liu Y, Chen H, Mu D, Li D, Zhong Y, Jiang N, Zhang Y, Xia M. Association of serum retinoic acid with risk of mortality in patients with coronary artery disease. Circ Res. 2016;119(4):557–63. [DOI] [PubMed] [Google Scholar]
- 23. Tu WJ, Qiu HC, Zhang Y, Cao JL, Wang H, Zhao JZ, Liu Q, Zeng X. Lower serum retinoic acid level for prediction of higher risk of mortality in ischemic stroke. Neurology. 2019;92(15):e1678–e87. [DOI] [PubMed] [Google Scholar]
- 24. Liu G, Ding M, Chiuve SE, Rimm EB, Franks PW, Meigs JB, Hu FB, Sun Q. Plasma levels of fatty acid-binding protein 4, retinol-binding protein 4, high-molecular-weight adiponectin, and cardiovascular mortality among men with type 2 diabetes: a 22-year prospective study. Arterioscler Thromb Vasc Biol. 2016;36(11):2259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zachariah JP, Hwang S, Hamburg NM, Benjamin EJ, Larson MG, Levy D, Vita JA, Sullivan LM, Mitchell GF, Vasan RS. Circulating adipokines and vascular function: cross-sectional associations in a community-based cohort. Hypertension. 2016;67(2):294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu Y, Zhong Y, Chen H, Wang D, Wang M, Ou JS, Xia M. Retinol-binding protein-dependent cholesterol uptake regulates macrophage foam cell formation and promotes atherosclerosis. Circulation. 2017;135(14):1339–54. [DOI] [PubMed] [Google Scholar]
- 27. Zhang JX, Zhu GP, Zhang BL, Cheng YY. Elevated serum retinol-binding protein 4 levels are correlated with blood pressure in prehypertensive Chinese. J Hum Hypertens. 2017;31(10):611–5. [DOI] [PubMed] [Google Scholar]
- 28. Rist PM, Jimenez MC, Tworoger SS, Hu FB, Manson JE, Sun Q, Rexrode KM. Plasma retinol-binding protein 4 levels and the risk of ischemic stroke among women. J Stroke Cerebrovasc Dis. 2018;27(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhu YY, Zhang JL, Liu L, Han Y, Ge X, Zhao S. Evaluation of serum retinol-binding protein-4 levels as a biomarker of poor short-term prognosis in ischemic stroke. Biosci Rep. 2018;38(5):BSR20180786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liu C, Che Y. Retinol-binding protein 4 predicts lesion volume (determined by MRI) and severity of acute ischemic stroke. Neurotox Res. 2019;35(1):92–9. [DOI] [PubMed] [Google Scholar]
- 31. Bershad S, Rubinstein A, Paterniti JR, Le NA, Poliak SC, Heller B, Ginsberg HN, Fleischmajer R, Brown WV. Changes in plasma lipids and lipoproteins during isotretinoin therapy for acne. N Engl J Med. 1985;313(16):981–5. [DOI] [PubMed] [Google Scholar]
- 32. Staels B. Regulation of lipid and lipoprotein metabolism by retinoids. J Am Acad Dermatol. 2001;45(5):S158–67. [DOI] [PubMed] [Google Scholar]
- 33. Kim HJ, Lee SM, Lee JS, Lee SY, Chung EH, Cho MK, Lee SH, Kim JE. Homocysteine, folic acid, and vitamin B12 levels in patients on isotretinoin therapy for acne vulgaris: a meta-analysis. J Cosmet Dermatol. 2019. doi: 10.1111/jocd.13059. [DOI] [PubMed] [Google Scholar]
- 34. Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, Kotani K, Quadro L, Kahn BB. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature. 2005;436(7049):356–62. [DOI] [PubMed] [Google Scholar]
- 35. Erikstrup C, Mortensen OH, Nielsen AR, Fischer CP, Plomgaard P, Petersen AM, Krogh-Madsen R, Lindegaard B, Erhardt JG, Ullum H et al.. RBP-to-retinol ratio, but not total RBP, is elevated in patients with type 2 diabetes. Diabetes Obes Metab. 2009;11(3):204–12. [DOI] [PubMed] [Google Scholar]
- 36. Tavridou A, Unwin NC, Laker MF, White M, Alberti KG. Serum concentrations of vitamins A and E in impaired glucose tolerance. Clin Chim Acta. 1997;266(2):129–40. [DOI] [PubMed] [Google Scholar]
- 37. Abahusain MA, Wright J, Dickerson JW, de Vol EB. Retinol, alpha-tocopherol and carotenoids in diabetes. Eur J Clin Nutr. 1999;53(8):630–5. [DOI] [PubMed] [Google Scholar]
- 38. Higuchi K, Saito I, Maruyama K, Eguchi E, Mori H, Tanno S, Sakurai S, Kishida T, Nishida W, Osawa H et al.. Associations of serum beta-carotene and retinol concentrations with insulin resistance: the Toon Health Study. Nutrition. 2015;31(7–8):975–80. [DOI] [PubMed] [Google Scholar]
- 39. Kim M, Jee SH, Kim M, Yoo HJ, Kang M, Kim J, Lee JH. Serum vitamin A-related metabolite levels are associated with incidence of type 2 diabetes. Diabetes Metab. 2017;43(3):287–91. [DOI] [PubMed] [Google Scholar]
- 40. Cho YM, Youn BS, Lee H, Lee N, Min SS, Kwak SH, Lee HK, Park KS. Plasma retinol-binding protein-4 concentrations are elevated in human subjects with impaired glucose tolerance and type 2 diabetes. Diabetes Care. 2006;29(11):2457–61. [DOI] [PubMed] [Google Scholar]
- 41. Graham TE, Yang Q, Bluher M, Hammarstedt A, Ciaraldi TP, Henry RR, Wason CJ, Oberbach A, Jansson PA, Smith U et al.. Retinol-binding protein 4 and insulin resistance in lean, obese, and diabetic subjects. N Engl J Med. 2006;354(24):2552–63. [DOI] [PubMed] [Google Scholar]
- 42. Broch M, Vendrell J, Ricart W, Richart C, Fernandez-Real JM. Circulating retinol-binding protein-4, insulin sensitivity, insulin secretion, and insulin disposition index in obese and nonobese subjects. Diabetes Care. 2007;30(7):1802–6. [DOI] [PubMed] [Google Scholar]
- 43. Gavi S, Stuart LM, Kelly P, Melendez MM, Mynarcik DC, Gelato MC, McNurlan MA. Retinol-binding protein 4 is associated with insulin resistance and body fat distribution in nonobese subjects without type 2 diabetes. J Clin Endocrinol Metab. 2007;92(5):1886–90. [DOI] [PubMed] [Google Scholar]
- 44. Hahn S, Backhaus M, Broecker-Preuss M, Tan S, Dietz T, Kimmig R, Schmidt M, Mann K, Janssen OE. Retinol-binding protein 4 levels are elevated in polycystic ovary syndrome women with obesity and impaired glucose metabolism. Eur J Endocrinol. 2007;157(2):201–7. [DOI] [PubMed] [Google Scholar]
- 45. Promintzer M, Krebs M, Todoric J, Luger A, Bischof MG, Nowotny P, Wagner O, Esterbauer H, Anderwald C. Insulin resistance is unrelated to circulating retinol binding protein and protein C inhibitor. J Clin Endocrinol Metab. 2007;92(11):4306–12. [DOI] [PubMed] [Google Scholar]
- 46. Qi Q, Yu Z, Ye X, Zhao F, Huang P, Hu FB, Franco OH, Wang J, Li H, Liu Y et al.. Elevated retinol-binding protein 4 levels are associated with metabolic syndrome in Chinese people. J Clin Endocrinol Metab. 2007;92(12):4827–34. [DOI] [PubMed] [Google Scholar]
- 47. Stefan N, Hennige AM, Staiger H, Machann J, Schick F, Schleicher E, Fritsche A, Haring HU. High circulating retinol-binding protein 4 is associated with elevated liver fat but not with total, subcutaneous, visceral, or intramyocellular fat in humans. Diabetes Care. 2007;30(5):1173–8. [DOI] [PubMed] [Google Scholar]
- 48. Takebayashi K, Suetsugu M, Wakabayashi S, Aso Y, Inukai T. Retinol binding protein-4 levels and clinical features of type 2 diabetes patients. J Clin Endocrinol Metab. 2007;92(7):2712–9. [DOI] [PubMed] [Google Scholar]
- 49. von Eynatten M, Lepper PM, Liu D, Lang K, Baumann M, Nawroth PP, Bierhaus A, Dugi KA, Heemann U, Allolio B et al.. Retinol-binding protein 4 is associated with components of the metabolic syndrome, but not with insulin resistance, in men with type 2 diabetes or coronary artery disease. Diabetologia. 2007;50(9):1930–7. [DOI] [PubMed] [Google Scholar]
- 50. Diamanti-Kandarakis E, Livadas S, Kandarakis SA, Papassotiriou I, Margeli A. Low free plasma levels of retinol-binding protein 4 in insulin-resistant subjects with polycystic ovary syndrome. J Endocrinol Invest. 2008;31(11):950–5. [DOI] [PubMed] [Google Scholar]
- 51. Gomez-Ambrosi J, Rodriguez A, Catalan V, Ramirez B, Silva C, Rotellar F, Gil MJ, Salvador J, Fruhbeck G. Serum retinol-binding protein 4 is not increased in obesity or obesity-associated type 2 diabetes mellitus, but is reduced after relevant reductions in body fat following gastric bypass. Clin Endocrinol (Oxf). 2008;69(2):208–15. [DOI] [PubMed] [Google Scholar]
- 52. Hutchison SK, Harrison C, Stepto N, Meyer C, Teede HJ. Retinol-binding protein 4 and insulin resistance in polycystic ovary syndrome. Diabetes Care. 2008;31(7):1427–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lewis JG, Shand BI, Frampton CM, Elder PA, Scott RS. Plasma retinol-binding protein is not a marker of insulin resistance in overweight subjects: a three year longitudinal study. Clin Biochem. 2008;41(13):1034–8. [DOI] [PubMed] [Google Scholar]
- 54. Mohlig M, Weickert MO, Ghadamgahi E, Arafat AM, Spranger J, Pfeiffer AF, Schofl C. Retinol-binding protein 4 is associated with insulin resistance, but appears unsuited for metabolic screening in women with polycystic ovary syndrome. Eur J Endocrinol. 2008;158(4):517–23. [DOI] [PubMed] [Google Scholar]
- 55. Bahr MJ, Boeker KH, Manns MP, Tietge UJ. Decreased hepatic RBP4 secretion is correlated with reduced hepatic glucose production but is not associated with insulin resistance in patients with liver cirrhosis. Clin Endocrinol (Oxf). 2009;70(1):60–5. [DOI] [PubMed] [Google Scholar]
- 56. Chavez AO, Coletta DK, Kamath S, Cromack DT, Monroy A, Folli F, DeFronzo RA, Tripathy D. Retinol-binding protein 4 is associated with impaired glucose tolerance but not with whole body or hepatic insulin resistance in Mexican Americans. Am J Physiol Endocrinol Metab. 2009;296(4):E758–64. [DOI] [PubMed] [Google Scholar]
- 57. Lee JW, Im JA, Park KD, Lee HR, Shim JY, Lee DC. Retinol binding protein 4 and insulin resistance in apparently healthy elderly subjects. Clin Chim Acta. 2009;400(1–2):30–2. [DOI] [PubMed] [Google Scholar]
- 58. Xu M, Li XY, Wang JG, Wang XJ, Huang Y, Cheng Q, Huang HE, Li R, Xiang J, Tan JR et al.. Retinol-binding protein 4 is associated with impaired glucose regulation and microalbuminuria in a Chinese population. Diabetologia. 2009;52(8):1511–9. [DOI] [PubMed] [Google Scholar]
- 59. Suh JB, Kim SM, Cho GJ, Choi KM, Han JH, Taek Geun H. Elevated serum retinol-binding protein 4 is associated with insulin resistance in older women. Metabolism. 2010;59(1):118–22. [DOI] [PubMed] [Google Scholar]
- 60. Ulgen F, Herder C, Kuhn MC, Willenberg HS, Schott M, Scherbaum WA, Schinner S. Association of serum levels of retinol-binding protein 4 with male sex but not with insulin resistance in obese patients. Arch Physiol Biochem. 2010;116(2):57–62. [DOI] [PubMed] [Google Scholar]
- 61. Meisinger C, Ruckert IM, Rathmann W, Doring A, Thorand B, Huth C, Kowall B, Koenig W. Retinol-binding protein 4 is associated with prediabetes in adults from the general population: the Cooperative Health Research in the Region of Augsburg (KORA) F4 Study. Diabetes Care. 2011;34(7):1648–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Luft VC, Pereira M, Pankow JS, Ballantyne C, Couper D, Heiss G, Duncan BB; ARIC Investigators . Retinol binding protein 4 and incident diabetes–the Atherosclerosis Risk in Communities Study (ARIC Study). Rev Bras Epidemiol. 2013;16(2):388–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sun L, Qi Q, Zong G, Ye X, Li H, Liu X, Zheng H, Hu FB, Liu Y, Lin X. Elevated plasma retinol-binding protein 4 is associated with increased risk of type 2 diabetes in middle-aged and elderly Chinese adults. J Nutr. 2014;144(5):722–8. [DOI] [PubMed] [Google Scholar]
- 64. Gavrilov V, Harman-Boehm I, Amichay D, Tessler G, Shuster T, Friger M, Gorodischer R. Kidney function and retinol status in type 2 diabetes mellitus patients. Acta Diabetol. 2012;49(2):137–43. [DOI] [PubMed] [Google Scholar]
- 65. Craig RL, Chu WS, Elbein SC. Retinol binding protein 4 as a candidate gene for type 2 diabetes and prediabetic intermediate traits. Mol Genet Metab. 2007;90(3):338–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Munkhtulga L, Nakayama K, Utsumi N, Yanagisawa Y, Gotoh T, Omi T, Kumada M, Erdenebulgan B, Zolzaya K, Lkhagvasuren T et al.. Identification of a regulatory SNP in the retinol binding protein 4 gene associated with type 2 diabetes in Mongolia. Hum Genet. 2007;120(6):879–88. [DOI] [PubMed] [Google Scholar]
- 67. Kovacs P, Geyer M, Berndt J, Kloting N, Graham TE, Bottcher Y, Enigk B, Tonjes A, Schleinitz D, Schon MR et al.. Effects of genetic variation in the human retinol binding protein-4 gene (RBP4) on insulin resistance and fat depot-specific mRNA expression. Diabetes. 2007;56(12):3095–100. [DOI] [PubMed] [Google Scholar]
- 68. van Hoek M, Dehghan A, Zillikens MC, Hofman A, Witteman JC, Sijbrands EJ. An RBP4 promoter polymorphism increases risk of type 2 diabetes. Diabetologia. 2008;51(8):1423–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Cabre A, Lazaro I, Girona J, Manzanares J, Marimon F, Plana N, Heras M, Masana L. Retinol-binding protein 4 as a plasma biomarker of renal dysfunction and cardiovascular disease in type 2 diabetes. J Intern Med. 2007;262(4):496–503. [DOI] [PubMed] [Google Scholar]
- 70. Masaki T, Anan F, Tsubone T, Gotoh K, Chiba S, Katsuragi I, Nawata T, Kakuma T, Yoshimatsu H. Retinol binding protein 4 concentrations are influenced by renal function in patients with type 2 diabetes mellitus. Metabolism. 2008;57(10):1340–4. [DOI] [PubMed] [Google Scholar]
- 71. Chang YH, Lin KD, Wang CL, Hsieh MC, Hsiao PJ, Shin SJ. Elevated serum retinol-binding protein 4 concentrations are associated with renal dysfunction and uric acid in type 2 diabetic patients. Diabetes Metab Res Rev. 2008;24(8):629–34. [DOI] [PubMed] [Google Scholar]
- 72. Akbay E, Muslu N, Nayir E, Ozhan O, Kiykim A. Serum retinol binding protein 4 level is related with renal functions in type 2 diabetes. J Endocrinol Invest. 2010;33(10):725–9. [DOI] [PubMed] [Google Scholar]
- 73. Henze A, Frey SK, Raila J, Tepel M, Scholze A, Pfeiffer AF, Weickert MO, Spranger J, Schweigert FJ. Evidence that kidney function but not type 2 diabetes determines retinol-binding protein 4 serum levels. Diabetes. 2008;57(12):3323–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Murata M, Saito T, Otani T, Sasaki M, Ikoma A, Toyoshima H, Kawakami M, Ishikawa SE. An increase in serum retinol-binding protein 4 in the type 2 diabetic subjects with nephropathy. Endocr J. 2009;56(2):287–94. [DOI] [PubMed] [Google Scholar]
- 75. Derosa G, Maffioli P, Ferrari I, Palumbo I, Randazzo S, D'Angelo A, Cicero AF. Effects of one year treatment of sibutramine on insulin resistance parameters in type 2 diabetic patients. J Pharm Pharm Sci. 2010;13(3):378–90. [DOI] [PubMed] [Google Scholar]
- 76. Jia W, Wu H, Bao Y, Wang C, Lu J, Zhu J, Xiang K. Association of serum retinol-binding protein 4 and visceral adiposity in Chinese subjects with and without type 2 diabetes. J Clin Endocrinol Metab. 2007;92(8):3224–9. [DOI] [PubMed] [Google Scholar]
- 77. Mills JP, Furr HC, Tanumihardjo SA. Retinol to retinol-binding protein (RBP) is low in obese adults due to elevated apo-RBP. Exp Biol Med (Maywood). 2008;233(10):1255–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Hogstrom M, Nordstrom A, Nordstrom P. Retinol, retinol-binding protein 4, abdominal fat mass, peak bone mineral density, and markers of bone metabolism in men: the Northern Osteoporosis and Obesity (NO2) Study. Eur J Endocrinol. 2008;158(5):765–70. [DOI] [PubMed] [Google Scholar]
- 79. Botella-Carretero JI, Balsa JA, Vazquez C, Peromingo R, Diaz-Enriquez M, Escobar-Morreale HF. Retinol and alpha-tocopherol in morbid obesity and nonalcoholic fatty liver disease. Obes Surg. 2010;20(1):69–76. [DOI] [PubMed] [Google Scholar]
- 80. Kanagasabai T, Alkhalaqi K, Churilla JR, Ardern CI. The association between metabolic syndrome and serum concentrations of micronutrients, inflammation, and oxidative stress outside of the clinical reference ranges: a cross-sectional study. Metab Syndr Relat Disord. 2019;17(1):29–36. [DOI] [PubMed] [Google Scholar]
- 81. Haider DG, Schindler K, Prager G, Bohdjalian A, Luger A, Wolzt M, Ludvik B. Serum retinol-binding protein 4 is reduced after weight loss in morbidly obese subjects. J Clin Endocrinol Metab. 2007;92(3):1168–71. [DOI] [PubMed] [Google Scholar]
- 82. Klöting N, Graham TE, Berndt J, Kralisch S, Kovacs P, Wason CJ, Fasshauer M, Schon MR, Stumvoll M, Bluher M et al.. Serum retinol-binding protein is more highly expressed in visceral than in subcutaneous adipose tissue and is a marker of intra-abdominal fat mass. Cell Metab. 2007;6(1):79–87. [DOI] [PubMed] [Google Scholar]
- 83. Lee JW, Im JA, Lee HR, Shim JY, Youn BS, Lee DC. Visceral adiposity is associated with serum retinol binding protein-4 levels in healthy women. Obesity (Silver Spring). 2007;15(9):2225–32. [DOI] [PubMed] [Google Scholar]
- 84. Bajzova M, Kovacikova M, Vitkova M, Klimcakova E, Polak J, Kovacova Z, Viguerie N, Vedral T, Mikulasek L, Sramkova P et al.. Retinol-binding protein 4 expression in visceral and subcutaneous fat in human obesity. Physiol Res. 2008;57(6):927–34. [DOI] [PubMed] [Google Scholar]
- 85. Tschoner A, Sturm W, Engl J, Kaser S, Laimer M, Laimer E, Weiss H, Patsch JR, Ebenbichler CF. Retinol-binding protein 4, visceral fat, and the metabolic syndrome: effects of weight loss. Obesity (Silver Spring). 2008;16(11):2439–44. [DOI] [PubMed] [Google Scholar]
- 86. Huang G, Wang D, Khan UI, Zeb I, Manson JE, Miller V, Hodis HN, Budoff MJ, Merriam GR, Harman MS et al.. Associations between retinol-binding protein 4 and cardiometabolic risk factors and subclinical atherosclerosis in recently postmenopausal women: cross-sectional analyses from the KEEPS study. Cardiovasc Diabetol. 2012;11:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chang X, Yan H, Bian H, Xia M, Zhang L, Gao J, Gao X. Serum retinol binding protein 4 is associated with visceral fat in human with nonalcoholic fatty liver disease without known diabetes: a cross-sectional study. Lipids Health Dis. 2015;14:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zachariah JP, Quiroz R, Nelson KP, Teng Z, Keaney JF Jr, Sullivan LM, Vasan RS. Prospective relation of circulating adipokines to incident metabolic syndrome: the Framingham Heart Study. J Am Heart Assoc. 2017;6(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Korek E, Gibas-Dorna M, Checinska-Maciejewska Z, Krauss H, Lagiedo-Zelazowska M, Kolodziejczak B, Bogdanski P. Serum RBP4 positively correlates with triglyceride level but not with BMI, fat mass and insulin resistance in healthy obese and non-obese individuals. Biomarkers. 2018;23(7):683–8. [DOI] [PubMed] [Google Scholar]
- 90. Saeed A, Dullaart RPF, Schreuder T, Blokzijl H, Faber KN. Disturbed vitamin A metabolism in non-alcoholic fatty liver disease (NAFLD). Nutrients. 2017;10(1):E29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Al-Daghri NM, Al-Attas OS, Alokail M, Draz HM, Bamakhramah A, Sabico S. Retinol binding protein-4 is associated with TNF-alpha and not insulin resistance in subjects with type 2 diabetes mellitus and coronary heart disease. Dis Markers. 2009;26(3):135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Derosa G, Cicero AF, D'Angelo A, Fogari E, Maffioli P. Effects of 1-year orlistat treatment compared to placebo on insulin resistance parameters in patients with type 2 diabetes. J Clin Pharm Ther. 2012;37(2):187–95. [DOI] [PubMed] [Google Scholar]
- 93. VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34(3):211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Graham TE, Wason CJ, Bluher M, Kahn BB. Shortcomings in methodology complicate measurements of serum retinol binding protein (RBP4) in insulin-resistant human subjects. Diabetologia. 2007;50(4):814–23. [DOI] [PubMed] [Google Scholar]
- 95. Sporn MB, Roberts AB, Goodman DS. The retinoids: biology, chemistry, and medicine. 2nd ed New York: Raven Press, 1994. [Google Scholar]
- 96. Chistiakov DA, Melnichenko AA, Myasoedova VA, Grechko AV, Orekhov AN. Mechanisms of foam cell formation in atherosclerosis. J Mol Med (Berl). 2017;95(11):1153–65. [DOI] [PubMed] [Google Scholar]
- 97. Nicholson AC, Han J, Febbraio M, Silversterin RL, Hajjar DP. Role of CD36, the macrophage class B scavenger receptor, in atherosclerosis. Ann N Y Acad Sci. 2001;947:224–8. [DOI] [PubMed] [Google Scholar]
- 98. Yu XH, Fu YC, Zhang DW, Yin K, Tang CK. Foam cells in atherosclerosis. Clin Chim Acta. 2013;424:245–52. [DOI] [PubMed] [Google Scholar]
- 99. Verges B, Guiu B, Cercueil JP, Duvillard L, Robin I, Buffier P, Bouillet B, Aho S, Brindisi MC, Petit JM. Retinol-binding protein 4 is an independent factor associated with triglycerides and a determinant of very low-density lipoprotein-apolipoprotein B100 catabolism in type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2012;32(12):3050–7. [DOI] [PubMed] [Google Scholar]
- 100. Costet P, Lalanne F, Gerbod-Giannone MC, Molina JR, Fu X, Lund EG, Gudas LJ, Tall AR. Retinoic acid receptor-mediated induction of ABCA1 in macrophages. Mol Cell Biol. 2003;23(21):7756–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar NEmerging Risk Factors Collaboration; et al.; Emerging Risk Factors Collaboration . Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Rhee EJ, Nallamshetty S, Plutzky J. Retinoid metabolism and its effects on the vasculature. Biochim Biophys Acta. 2012;1821(1):230–40. [DOI] [PubMed] [Google Scholar]
- 103. Noy N. Vitamin A in regulation of insulin responsiveness: mini review. Proc Nutr Soc. 2016;75(2):212–5. [DOI] [PubMed] [Google Scholar]
- 104. Liu Y, Chen H, Wang J, Zhou W, Sun R, Xia M. Elevated retinol binding protein 4 induces apolipoprotein B production and associates with hypertriglyceridemia. J Clin Endocrinol Metab. 2015;100(5):E720–8. [DOI] [PubMed] [Google Scholar]
- 105. McMullen MH, Rowling MJ, Ozias MK, Schalinske KL. Activation and induction of glycine N-methyltransferase by retinoids are tissue- and gender-specific. Arch Biochem Biophys. 2002;401(1):73–80. [DOI] [PubMed] [Google Scholar]
- 106. Nieman KM, Rowling MJ, Garrow TA, Schalinske KL. Modulation of methyl group metabolism by streptozotocin-induced diabetes and all-trans-retinoic acid. J Biol Chem. 2004;279(44):45708–12. [DOI] [PubMed] [Google Scholar]
- 107. Ozias MK, Schalinske KL.. All-trans-retinoic acid rapidly induces glycine N-methyltransferase in a dose-dependent manner and reduces circulating methionine and homocysteine levels in rats. J Nutr. 2003;133(12):4090–4. [DOI] [PubMed] [Google Scholar]
- 108. Rowling MJ, McMullen MH, Schalinske KL. Vitamin A and its derivatives induce hepatic glycine N-methyltransferase and hypomethylation of DNA in rats. J Nutr. 2002;132(3):365–9. [DOI] [PubMed] [Google Scholar]
- 109. Rowling MJ, Schalinske KL.. Retinoid compounds activate and induce hepatic glycine N-methyltransferase in rats. J Nutr. 2001;131(7):1914–7. [DOI] [PubMed] [Google Scholar]
- 110. Rowling MJ, Schalinske KL.. Retinoic acid and glucocorticoid treatment induce hepatic glycine N-methyltransferase and lower plasma homocysteine concentrations in rats and rat hepatoma cells. J Nutr. 2003;133(11):3392–8. [DOI] [PubMed] [Google Scholar]
- 111. Olson JA. Serum levels of vitamin A and carotenoids as reflectors of nutritional status. J Natl Cancer Inst. 1984;73(6):1439–44. [PubMed] [Google Scholar]
- 112. Stauber PM, Sherry B, VanderJagt DJ, Bhagavan HN, Garry PJ. A longitudinal study of the relationship between vitamin A supplementation and plasma retinol, retinyl esters, and liver enzyme activities in a healthy elderly population. Am J Clin Nutr. 1991;54(5):878–83. [DOI] [PubMed] [Google Scholar]
- 113. Olsen T, Vinknes KJ, Blomhoff R, Lysne V, Midttun O, Dhar I, Ueland PM, Svingen GFT, Pedersen EKR, Drevon CA et al.. Creatinine, total cysteine and uric acid are associated with serum retinol in patients with cardiovascular disease. Eur J Nutr. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari AJ, Erskine H, Leung J, Santamauro D, Lund C, Aminde LN et al.. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Health. 2019;7(10):e1375–e87. [DOI] [PubMed] [Google Scholar]
- 115. N. C. D. Risk Factor Collaboration - Africa Working Group. Trends in obesity and diabetes across Africa from 1980 to 2014: an analysis of pooled population-based studies. Int J Epidemiol. 2017;46(5):1421–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Rubin LP, Ross AC, Stephensen CB, Bohn T, Tanumihardjo SA. Metabolic effects of inflammation on vitamin A and carotenoids in humans and animal models. Adv Nutr. 2017;8(2):197–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Raiten DJ, Sakr Ashour FA, Ross AC, Meydani SN, Dawson HD, Stephensen CB, Brabin BJ, Suchdev PS, van Ommen B, Group IC. Inflammation and Nutritional Science for Programs/Policies and Interpretation of Research Evidence (INSPIRE). J Nutr. 2015;145(5):1039S–108S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Stephensen CB, Gildengorin G. Serum retinol, the acute phase response, and the apparent misclassification of vitamin A status in the third National Health and Nutrition Examination Survey. Am J Clin Nutr. 2000;72(5):1170–8. [DOI] [PubMed] [Google Scholar]
- 119. Minihane AM, Vinoy S, Russell WR, Baka A, Roche HM, Tuohy KM, Teeling JL, Blaak EE, Fenech M, Vauzour D et al.. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br J Nutr. 2015;114(7):999–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Liu Y, Wang D, Li D, Sun R, Xia M. Associations of retinol-binding protein 4 with oxidative stress, inflammatory markers, and metabolic syndrome in a middle-aged and elderly Chinese population. Diabetol Metab Syndr. 2014;6(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Larson LM, Guo J, Williams AM, Young MF, Ismaily S, Addo OY, Thurnham D, Tanumihardjo SA, Suchdev PS, Northrop-Clewes CA. Approaches to assess vitamin A status in settings of inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) Project. Nutrients. 2018;10(8):1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kane MA, Napoli JL.. Quantification of endogenous retinoids. Methods Mol Biol. 2010;652:1–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Al Tanoury Z, Piskunov A, Rochette-Egly C. Vitamin A and retinoid signaling: genomic and nongenomic effects. J Lipid Res. 2013;54(7):1761–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Soderlund MB, Sjoberg A, Svard G, Fex G, Nilsson-Ehle P. Biological variation of retinoids in man. Scand J Clin Lab Invest. 2002;62(7):511–9. [DOI] [PubMed] [Google Scholar]