Dear Editor,
We recently reviewed two papers (1,2) on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also termed coronavirus disease 2019 (COVID-19), with great interest to better identify the roles of radiologists in diagnosing this virus.
Shi et al. (1) reported that COVID-19 pneumonia may present with atypical manifestations such as hemoptysis and focal ground-glass opacity (GGO) with non-peripheral distribution in the left upper lobe on initial CT scans. Three days after admission, a small amount of pleural effusion was noted. Although CT findings of COVID-19 are often non-specific and would vary with the stages of the disease (3), hemoptysis and pleural effusion has been rarely reported in patients with COVID-19 infection to date. Huang et al. (4) found that hemoptysis occurred in only 5% of their patients. Fortunately, the patient's hemoptysis and CT findings improved. In addition to the case, we want to introduce a case of COVID-19 that required mechanical ventilation because of the rapid progression of pulmonary hemorrhage and hemoptysis (Fig. 1).
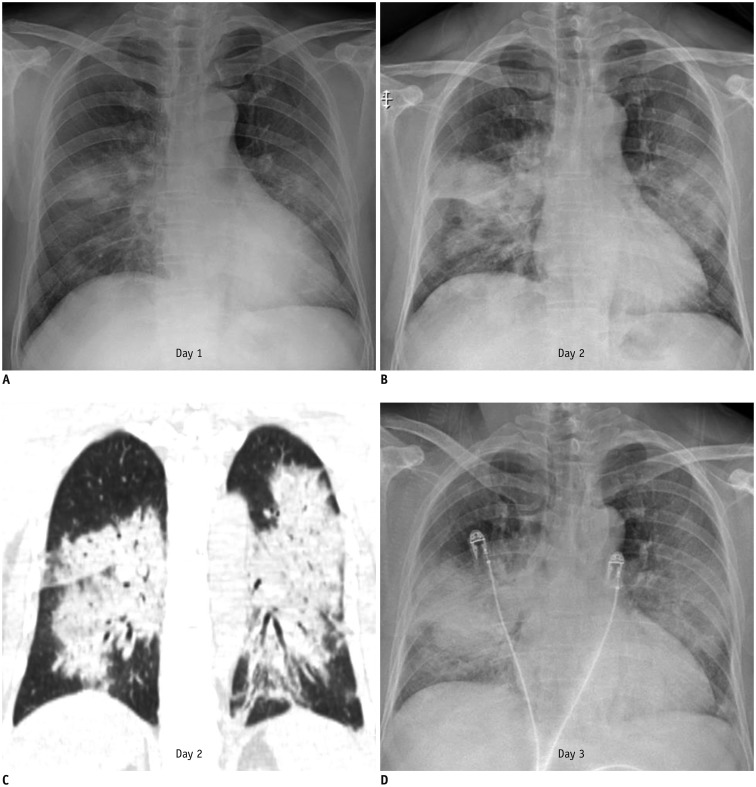
Fig. 1. Radiologic courses of 56-year-old patient with COVID-19.
56-year-old man who had cough, myalgia, and chillness for week was diagnosed with COVID-19 three days before admission.
A. He abruptly complained of hemoptysis and dyspnea, and chest radiograph showed bilateral consolidations and GGOs in both middle and left lower lung field. B–D. On day 2 and 3, chest radiographs and CT showed rapid progression of bilateral consolidations. COVID-19 = coronavirus disease 2019, GGO = ground-glass opacity
According to a recent summary from China, 81% of people with COVID-19 have mild disease and do not require hospitalization (5). However, 5% of all COVID-19 patients are critically ill, and the crude fatality ratio among people over 80 years of age was estimated at 21.9% in one study (6). CT findings mainly include bilateral consolidation and GGO, which may vary in its presentation according to the amount of time that has elapsed between symptom onset and CT scanning or the severity of the patients' condition. Therefore, it is vital to establish a method to identify which patients are likely to progress rapidly and require hospitalization. It is known that mortality increases with age, a higher Sequential Organ Failure Assessment score, elevated d-dimer levels, and the duration of viral shedding (7), but limited studies have focused on the role of radiologists in recognition of rapidly progressing cases of COVID-19.
Although CT findings in COVID-19 patients are variable, the detection rate of disease on CT is 98% (8). Li et al. (2) reported that reliable clinical diagnoses require complementary approaches to confirm COVID-19, such as CT in combination with real-time reverse-transcriptase polymerase chain reaction, which is currently the gold standard method for verifying SARS-CoV-2 infection. From a clinical perspective, CT features could be utilized as the first and most immediate reference for doctors to take necessary actions in vulnerable patients. Radiologic studies in patients suspected of having COVID-19 have mainly focused on chest radiographic or CT findings to differentiate COVID-19 from other bacterial diseases (9,10,11). However, it is also necessary for radiologists to recognize the importance of serial chest radiography and CT findings in the evaluation of the severity of patient disease progression.
Despite its high worldwide rate of diagnosis, people still afraid of COVID-19 because vaccines and adequate treatments have not been developed. Therefore, the course of the disease caused by COVID-19 infection is of particular interest. Clinical presentations of some patients are similar to SARS-CoV-1 infections. Patients with severe illness may develop acute respiratory distress syndrome (ARDS) and require intensive care unit admission and oxygen therapy. The time that elapses between hospital admission and ARDS onset is often as short as two or three days. At this stage, the mortality rate is high for COVID-19 infection; 15% of patients in this cohort died (4). It is often difficult to obtain a repeat CT scan in this short period, particularly in a negative pressure ward or an isolated area. However, the prognosis will likely be poor if a sudden progression of the disease is not detected on time. In this situation, repeated chest radiography twice a day would be helpful to detect the rapid deterioration of diagnosed patients and help clinicians identify patients who will go on to develop an ARDS.
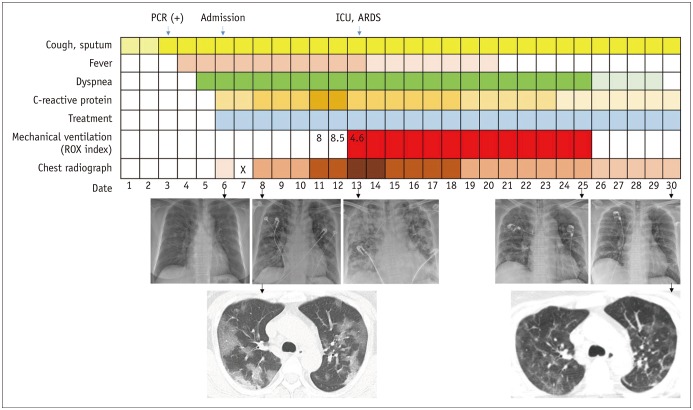
Figure 2 demonstrates the time course of the radiographic changes associated with symptoms and laboratory findings in a 51-year-old patient diagnosed with COVID-19. On the sixth day following symptom onset, the chest radiograph showed focal increased opacity in the right middle lung field but otherwise was normal. Two days later, follow-up chest radiography demonstrated rapid progression, which continued until day 13. The patient was finally intubated and showed a gradual improvement in clinical and radiologic findings after receiving mechanical ventilation. This case reminds us of the role of radiologists in rapidly progressive COVID-19 pneumonia. First, serial radiographic examinations are critical in the first 7–10 days after symptom onset. Yoon et al. (10) reported that four of nine patients did not initially show radiographic abnormalities. Because common CT findings of COVID-19 infection in the early stage are multiple regions of GGO in both lungs (1,3,4,8), chest radiography would be less critical for initial diagnosis. However, even if the symptoms and chest radiographic findings are not severe, we should be aware that some patients may experience a sudden deterioration. Thus, to identify rapidly progressing patients, follow-up chest radiography every one or two days should be recommended in symptomatic patients, especially those with persistent fever, even if the radiographs appear normal at first. Second, radiologists need to interpret chest radiographs to identify any slight changes carefully. Because COVID-19 most commonly appears as GGO, there is a possibility of misinterpretation due to changes in the degree of radiation exposure or patient positioning. Therefore, it is also essential for radiologists to ensure that chest radiography should be performed using standardized techniques.
Fig. 2. Clinical and radiologic courses from onset of symptoms of 51-year-old patient with COVID-19.
Darkly colored means that degree is severe. Low-grade fever, 37.5–38.2℃; high-grade fever, > 38.3℃; C-reactive protein elevation was divided into < 10, 10–19.9, 20–29.9, ≥ 30 mg/dL; lopinavir/ritonavir and hydroxychloroquine were used as treatment; haziness of chest radiograph was divided into < 10%, 10–49%, 50–69%, ≥ 70% of total lung involvement. ARDS = acute respiratory distress syndrome, ICU = intensive-care unit, PCR = polymerase chain reaction, ROX index = respiratory rate-oxygenation index (calculated as ratio of oxygen saturation/fraction of inspired oxygen)
In conclusion, the roles of radiologists are essential in not only the diagnosis but also in observation of progression in the treatment of patients with COVID-19 because radiologists are most familiar with the shading of GGO on chest CT scans and chest radiography. In addition, it is also necessary for radiologists to be aware of any clinical symptoms (persistent fever) or changes in various laboratory findings in patients with severe illness to ensure competent reading of radiography in COVID-19 infection.
References
- 1.Shi F, Yu Q, Huang W, Tan C. 2019 Novel Coronavirus (COVID-19) Pneumonia with Hemoptysis as the Initial Symptom: CT and Clinical Features. Korean J Radiol. 2020;21:537–540. doi: 10.3348/kjr.2020.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li D, Wang D, Dong J, Wang N, Huang H, Xu H, et al. False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: role of deep-learning-based CT diagnosis and insights from two cases. Korean J Radiol. 2020;21:505–508. doi: 10.3348/kjr.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 Feb 19; doi: 10.1148/radiol.2020200432. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 Feb 24; doi: 10.1001/jama.2020.2648. [Epub] [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) [Accessed March 5, 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 7.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes On Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology. 2020 Feb 13; doi: 10.1148/radiol.2020200370. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]