Abstract
Background:
Preterm birth is associated with an increased risk of neonatal brain injury, which can lead to alterations in brain maturation. Despite being born without the most significant medical consequences of preterm birth, infants born early remain at increased risk for subtle brain injury that affects future neurodevelopment and functioning.
Aims:
To investigate the gray matter morphometry measures of cortical thickness, cortical surface area, and sulcal depth using MRI at 5 years of age in healthy children born preterm.
Study design:
Cohort study.
Subjects:
Participants were 52 children born preterm (< 33 weeks gestational age) and 37 children born full term.
Outcome measures:
Cortical segmentation and calculation of morphometry measures were completed using FreeSurfer version 5.3.0 and compared between groups using surface-based, voxel-wise analyses.
Results:
The preterm group had a significantly thinner cortex in temporal and parietal regions while cortical thickness was significantly larger within occipital and inferior frontal regions. Surface area was significantly reduced within the fusiform gyrus. Sulcal depth was significantly lower within the posterior parietal and inferior temporal regions but greater in the middle temporal and medial parietal regions.
Conclusions:
Regional differences were found between preschoolers born preterm and full term in cortical thickness, surface area, and sulcal depth. Cortical thickness differences primarily overlapped with regions found in previous studies of older children and adults. Differences in sulcal depth may represent additional areas of maturational differences in preterm children. These findings likely represent a combination of delayed maturation and permanent alterations caused by the perinatal processes associated with preterm birth.
Keywords: Preterm birth, Preschool, Gray matter, Cortical thickness, Surface area, Sulcal depth
Preterm birth is associated with an increased incidence of brain injury at birth that involves primarily the periventricular white matter and subcortical structures. This has been termed the “encephalopathy of prematurity” and is the primary determinant of neurodevelopmental difficulties in childhood following preterm birth [1]. Despite dramatic advances in neonatal care and increased survivability, children and young adults who were born preterm (< 33 gestational weeks) continue to show brain differences compared to their full term counterparts. These differences likely reflect the cascading effect of preterm birth on vulnerable brain systems throughout the course of brain development. There is debate regarding the impact of early exposure to the ex utero environment as well as injuries sustained either before or after delivery [2]. The third trimester, a period of rapid brain growth and changes in regional connectivity, is disrupted by preterm birth and the alteration of patterns of maturation of neurons and glial cells likely causes the long-term changes in cognitive and behavioral skills in these children. Rapid brain development continues through the preschool period [3] but few MRI studies have examined the impact of preterm birth during this critical developmental period. MRI studies of typical development suggest apparent cortical thickness decreases continually from preschool through early adulthood, while cortical surface area expands during early childhood and then gradually contracts during adolescence [4]. This pattern highlights the importance of deconstructing cortical volume into thickness and area [5].
MRI studies of older children and adolescents born preterm or with very low birthweight (VLBW) have shown what are presumed to be permanent changes in both gray and white matter. The first study to examine MRI measures of cortical thickness in VLBW adolescents found areas of thinner cortex primarily in the parietal lobes (pre- and post-central gyrus and supramarginal gyrus) and middle temporal gyrus [6,7]. The anterior cingulate, posterior inferior parietal regions, and middle temporal gyrus have also been found to be thinner than normal in other studies of older children and adolescents [6,8,9]. Other cortical areas are thicker than normal in studies of children, adolescents, and young adults, particularly within frontal and occipital regions [6,10-12].
Older children and young adults born preterm or VLBW are more likely to have reduced cortical surface area across a number of regions [9,13]. In school-age children, smaller surface area was found in the bilateral medial and lateral temporal lobes, inferior frontal lobes, and parietal/occipital regions [14]. Reduced surface area in orbitofrontal and transverse temporal regions was found in a small group of 3- to 4-year-old children [15], as well as older children and young adults [12,16,17].
The process of gyrification or cortical folding rapidly develops before 40 weeks gestation. Abnormalities in gyrification and reduced sulcal depth have been reported in some developmental disorders. Studies of preterm infants who undergo MRI scanning when they reach term-equivalent age suggest that preterm birth alters the timing and trajectory of the deepening of sulci [18]. In a study of cortical folding, preterm infants showed more shallow sulci than full term infants at term-equivalent age [19]. Examination of sulcal depth (or gyrification) in preterm children has been limited. Sulcal depth in 7-year-old preterm children was shallower in the superior temporal sulci and inferior portion of the pre- and post-central sulci compared with same-age full term children [20]. Another study found increased bilateral temporal lobe gyrification in the temporal lobes in 8-year-old preterm children [21]. The process of gyrification is related to sulcal depth and these measures may be the most sensitive to detecting damage in preterm children [22].
The purpose of this study was to characterize the brain structural properties of a group of healthy preschoolers born preterm with relatively benign neonatal health history. Here we compared measures of cortical thickness, surface area, and sulcal depth between preterm and full term children at preschool age. This same sample was included in our previous paper [23]. Based on the results from previous studies of older children and adolescents (reviewed above), we hypothesized that cortical thickness would be thinner than normal in the parietal and temporal lobes and thicker than normal in the medial and lateral frontal lobes and possibly within occipital regions. We also predicted the surface area in the temporal and parietal regions to be reduced. There is very little data about sulcal depth or gyrification, thus our investigation of sulcal depth was considered exploratory.
1. Method
1.1. Participants
The final sample was composed of 52 children born preterm and 37 children born full term. Children were enrolled and completed the study visits within six months of beginning kindergarten, which typically occurs at age five in the U.S. The preterm group was recruited primarily from the follow-up program for two neonatal intensive care units in San Diego (UC San Diego and Sharp Mary Birch). The purpose of this study was to investigate the development of children born preterm without significant neonatal brain injury. Therefore, none of the children had CNS injury (i.e., Grade 3–4 intraventricular hemorrhage, cystic periventricular leukomalacia, moderate-severe ventricular dilation), known genetic abnormalities likely to affect development, and/or acquired neurological disorder unrelated to preterm birth. In the final sample, two of the children had a history of necrotizing enterocolitis and three had bronchopulmonary dysplasia (with one who had both). The children born full term were recruited via the UC San Diego Center for Human Development database of parents who consented to be contacted if their children might qualify for a study. They had no history of neurological, psychiatric, or developmental disorders. Children with significant auditory or visual deficits and/or contraindications to MRI (e.g., pacemaker, metallic implants, recent dental procedures) were excluded. All children enrolled in the study were primarily English speaking and had a Full Scale IQ > 75 on the Wechsler Preschool and Primary Scale of Intelligence – Fourth Edition (WPPSI-IV) [24]. The Institutional Review Board at UC San Diego approved all procedures, and each participant's legal guardian gave written informed consent.
1.2. Brain imaging
Data were collected on a General Electric Discovery MR750 3.0 Tesla scanner with an 8-channel phased-array head coil at the Center for Functional MRI at UC San Diego. The full imaging protocol included: 1) a three-plane localizer; 2) a 3D T1-weighted inversion prepared RF-spoiled gradient echo scan using real-time prospective motion correction (PROMO) [25]; 3) a 3D T2-weighted variable flip angle fast spin echo scan for detection and quantification of white matter lesions and segmentation of CSF; 4) a high angular resolution diffusion imaging (HARDI) scan with 30-diffusion directions, and integrated B0 distortion correction (DISCO). All data were inspected for quality during collection and at all stages of processing.
Data were processed at the UC San Diego Center for Multimodal Imaging and Genetics (CMIG). Structural T1-weighted images were processed using gradient nonlinearity correction. Cortical and subcortical segmentation was completed using FreeSurfer automated segmentation in version 5.3.0 [26]. The imaging protocol and data processing stream were originally developed for studies involving young children as part of the Pediatric Imaging Neurocognition and Genetics project (PING; see Jernigan, Brown [27] for full details). Briefly, nonlinear transformation was used to correct for distortions caused by nonlinearity of the spatial encoding gradient fields and nonparametric nonuniform intensity normalization method was used to reduce the non-uniformity of signal intensity. The automated FreeSurfer pipeline was used for extraction of gray matter cortical thickness, cortical surface area, and sulcal depth [28]. Sulcal depth is measured as the distance from the deepest point of a sulcus to the mean height of the crown of the two adjacent gyri.
The final sample was composed of all the children enrolled in the study who were able to successfully complete the MRI scanning session with images of acceptable quality. Of the 105 children originally enrolled in the study, five preterm children and one full term child were unwilling to attempt the scanning procedure. Images were checked for movement or other scanner artifacts as well as errors in segmentation and registration by two trained experts. Each scan was assigned a number from 0 to 2 to signify the amount of motion in the scan by a technician blinded to group membership. A value of 0 indicated no motion artifact in the scan (11.5% of preterm, 24.3% of full term), a value of 1 indicated minimal artifact (76.9% of preterm, 73.0% of full term), and a value of 2 indicated moderate motion artifact but image quality still within acceptable limits (11.5% of preterm, 2.7% of full term). Significant motion artifacts were present in the images of three preterm and four full term children, therefore these were removed from the analyses. Additional subjects were removed due to significant errors in the FreeSurfer segmentation/reconstruction, which included two preterm children and one full term child. All scans were also reviewed by a neuroradiologist to inspect for brain abnormalities which led to one additional full term participant necessitating removal from the sample because of a brain abnormality. After these participants were removed from the sample, the final sample consisted of a total of 52 preterm and 37 full term children.
1.3. Statistical analyses
Statistical analyses were completed in SPSS, version 25 [29]. Demographic variables were compared between groups using Pearson χ2 and t-tests. A single socioeconomic status (SES) value was calculated for each child as a combination of parent-reported household income (4 levels) and years of maternal, or primary guardian, education (4 levels). This resulted in an SES value from 2 to 8 for each child, as in our previous publication [23].
Cortical thickness, surface area, and sulcal depth were compared between groups using a surface-based, voxel-wise generalized linear model (GLM) with sex and age at scan as covariates. This method uses FreeSurfer tools as well as custom processing tools to calculate a voxel-wise general linear model of groups. The model is false discovery rate corrected for p = .05. The GLM results are then overlaid on a FreeSurfer standard average brain surface.
Follow-up analyses utilized values derived from regions of interest (ROI) from the FreeSurfer automatic, sulcal-based parcellation [30] corresponding to the areas of significant difference on the voxel-wise surface map. Mean ROI values were compared between groups using ANCOVA controlling for sex and age at scan. Experts [31,32] have recommended interpreting overall patterns of significant effects, not just individual comparisons and significant results should be guided by predictions ordered from most to least important. Above all, investigators should focus on effect sizes. The accepted standard for the standardized Cohen's d is 0.20, 0.50, and 0.80 for small, medium, and large effects, respectively [33]. We therefore included Cohen's d in describing these results and focus on predictions of interest with medium and larger effects. Additional, follow-up partial correlations were conducted to determine the relationship between the gray matter metrics and birth characteristic of the preterm group including GA and birth weight.
2. Results
Group characteristics and mean values are presented in Table 1. There were no significant group differences for sex (χ2 = 0.067, p = .795), age (t = −0.447, p = .656), or handedness (χ2 = 2.24, p = .327), or SES (t = −0.452, p = .655). As expected, the preterm group had significantly lower gestational age at birth (t = −26.75, p < .001) and birthweight (t = −20.13, p < .001). WPPSI-IV Full Scale IQ scores were significantly lower in the preterm group (t = −2.36, p = .020), however the both group mean scores were in the average range. Motion artifact ratings were not significantly different between the groups (χ2 = 3.72, p = .155).
Table 1.
Participant characteristics.
| Variable | Preterm | Full term |
|---|---|---|
| Total subjects (n) | 52 | 37 |
| Sex: M/F (% female) | 30/24 (44.4%) | 19/17 (52.7%) |
| Age: Mean years (SD) | 5.29 (0.40) | 5.33 (0.31) |
| Dominant Hand (right/left/mixed) | 41/5/6 | 31/4/1 |
| GA: Mean (range) | 29.50 (24–32)* | 39.66 (38–41) |
| Birth Weight (g): Mean (SD) | 1354.80 (450.07)* | 3416.11 (512.38) |
| WPPSI-IV FSIQ | 101.85 (12.87)^ | 107.86 (9.46) |
| SES Composite: Mean (range) | 5.04 (2–8) | 5.19 (2–8) |
| Ethnicity (n) | ||
| African American | 2 | 1 |
| Asian | 4 | 6 |
| Caucasian | 26 | 12 |
| Hispanic/Latino | 14 | 8 |
| Mixed | 6 | 9 |
| African American/Caucasian | – | 2 |
| >American or Alaskan Native/Caucasian | 1 | 2 |
| Asian/Caucasian | 5 | 3 |
| Native Hawaiian or Pacific Islander/Caucasian | – | 1 |
Note. M/F: Male/Female; SD: Standard deviation; handedness not available for one full term child; GA: gestational age at birth in weeks; WPPSI-IV FSIQ: Wechsler Preschool and Primary Scale of Intelligence – Fourth Edition Full Scale IQ
significant difference between groups, p < .005
significant difference between groups, p < .05. Ethnicity based on self-report (one full term family declined to state).
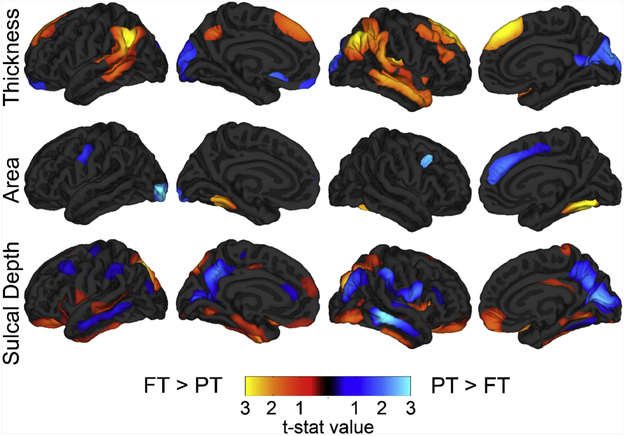
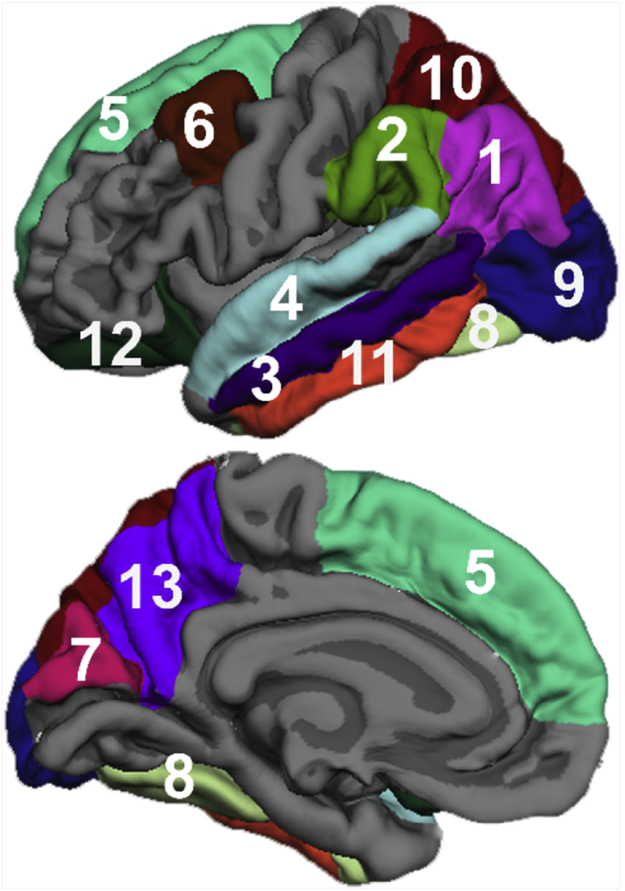
Fig. 1 presents the average statistical maps that compare the preterm and full term groups for cortical thickness, surface area, and sulcal depth. Follow-up analyses utilized values derived from regions of interest (ROI) from the FreeSurfer automatic, sulcal-based parcellation [30] corresponding to the areas of significant difference on the voxel-wise surface map. ROI values were compared between groups using ANCOVA controlling for sex and age at scan. Table 2 includes these follow-up comparisons and mean values for ROIs corresponding to regions on surface maps and Fig. 2 displays the corresponding ROIs on the left hemsphere surfaces.
Fig. 1.
Vertex-wise comparison of gray matter measures.
Note. Mean difference between preterm (PT) and full term (FT) groups corrected for false discovery rate = 0.05, projected onto the FreeSurfer average surface. Minimum threshold of p = .01 based on the t-statistic.
Table 2.
ROI values for areas shown to have significant between-group differences on the vertex-wise maps.
| Thickness | Preterm (M, sd) | Full term (M, sd) | F | P | Cohen's d |
|---|---|---|---|---|---|
| L inferior parietal | 2.88 (0.12) | 2.96 (0.12) | 11.875 | 0.001 | 0.749 |
| R inferior parietal | 2.94 (0.13) | 3.02 (0.12) | 9.502 | 0.003 | 0.670 |
| L supramarginal | 2.98 (0.14) | 3.07 (0.12) | 10.752 | 0.002 | 0.710 |
| R supramarginal | 3.01 (0.14) | 3.08 (0.12) | 6.036 | 0.016 | 0.532 |
| L middle temporal | 3.21 (0.16) | 3.32 (0.14) | 11.670 | 0.001 | 0.742 |
| R middle temporal | 3.25 (0.13) | 3.37 (0.14) | 16.547 | < 0.001 | 0.883 |
| L superior temporal | 3.18 (0.14) | 3.23 (0.14) | 2.713 | 0.103 | 0.358 |
| R superior temporal | 3.20 (0.13) | 3.27 (0.13) | 6.877 | 0.010 | 0.570 |
| L superior frontal | 3.30 (0.15) | 3.35 (0.14) | 2.318 | 0.132 | 0.333 |
| R superior frontal | 3.22 (0.18) | 3.30 (0.15) | 4.845 | 0.030 | 0.448 |
| R caudal middle frontal | 2.86 (0.17) | 2.94 (0.12) | 5.140 | 0.026 | 0.492 |
| L cuneus | 2.32 (0.26) | 2.22 (0.22) | 3.699 | 0.058 | 0.419 |
| R cuneus | 2.35 (0.24) | 2.23 (0.20) | 6.957 | 0.010 | 0.574 |
| Surface area | |||||
| Total L hemisphere | 82,097.65 (7921.16) | 81,644.73 (7239.12) | 0.095 | 0.758 | 0.063 |
| Total R hemisphere | 82,266.15 (8009.99) | 81,864.22 (7421.82) | 0.068 | 0.796 | 0.063 |
| L fusiform | 3083.79 (400.62) | 3292.35 (390.85) | 6.779 | 0.011 | 0.565 |
| R fusiform | 2973.06 (356.88) | 3220.38 (400.02) | 11.430 | 0.001 | 0.735 |
| L lateral occipital | 4981.50 (641.81) | 4699.46 (472.21) | 6.175 | 0.015 | 0.540 |
| R superior frontal | 7070.23 (895.38) | 6736.43 (749.70) | 4.155 | 0.045 | 0.444 |
| R caudal middle frontal | 2217.31 (398.32) | 2041.84 (365.52) | 5.016 | 0.028 | 0.487 |
| Sulcal depth | |||||
| L superior parietal | −0.0015 (0.055) | 0.0317 (0.033) | 10.661 | 0.002 | 0.707 |
| R superior parietal | −0.0521 (0.053) | −0.0070 (0.041) | 18.075 | < 0.001 | 0.921 |
| L inferior parietal | 0.0953 (0.046) | 0.0880 (0.039) | 0.589 | 0.445 | 0.168 |
| R inferior parietal | 0.0880 (0.037) | 0.0787 (0.034) | 1.353 | 0.248 | 0.255 |
| L supramarginal | 0.0512 (0.050) | 0.0269 (0.032) | 6.845 | 0.011 | 0.570 |
| R supramarginal | 0.1269 (0.059) | 0.0987 (0.048) | 5.800 | 0.018 | 0.523 |
| L middle temporal | −0.1056 (0.064) | −0.1480 (0.056) | 11.486 | 0.001 | 0.735 |
| R middle temporal | −0.1070 (0.067) | −0.1548 (0.045) | 14.339 | < 0.001 | 0.820 |
| L inferior temporal | −0.1154 (0.050) | −0.0646 (0.054) | 20.748 | < 0.001 | 0.988 |
| R inferior temporal | −0.1225 (0.054) | −0.0756 (0.049) | 17.547 | < 0.001 | 0.908 |
| L lateral orbitofrontal | 0.0057 (0.051) | 0.0272 (0.047) | 3.983 | 0.049 | 0.434 |
| R lateral orbitofrontal | 0.0286 (0.050) | 0.0494 (0.043) | 4.200 | 0.044 | 0.444 |
| R cuneus | −0.3297 (0.073) | −0.3622 (0.071) | 4.317 | 0.041 | 0.449 |
| L precuneus | 0.1782 (0.055) | 0.1550 (0.041) | 5.003 | 0.028 | 0.487 |
| R precuneus | 0.2115 (0.056) | 0.1724 (0.049) | 12.168 | 0.001 | 0.756 |
Note: Group comparisons controlling for sex and age at scan. ROI values extracted from the FreeSurfer Desikan parcellation. R: Right; L: Left. Thickness and sulcal depth measured in mm; area measured in mm2. M: mean; sd: standard deviation; F: F ratio results for the between-group ANCOVA controlling for sex and age at scan. Group differences with medium and large effect sizes are represented in bold.
Fig. 2.
Desikan atlas ROIs included in follow-up analyses.
Note. 1: Inferior parietal, 2: Supramarginal, 3: Middle temporal, 4: Superior temporal, 5: Superior frontal, 6: Caudal middle frontal, 7: Cuneus, 8: Fusiform, 9: Lateral occipital, 10: Superior parietal, 11: Inferior temporal, 12: Lateral orbitofrontal, 13: Precuneus.
The preterm group had significantly lower cortical thickness in the bilateral supramarginal and angular gyri, bilateral superior and middle temporal lobes, and bilateral superior and medial middle frontal regions. Additional areas of lower cortical thickness in the preterm group were found in the right hemisphere in lateral aspects of the frontal lobe. They also showed significantly greater cortical thickness in the cuneus and frontal pole.
Total surface area was not significantly different between groups (F [1,85] = 0.081, p = .776). Surface area was only significantly smaller in the preterm group in bilateral fusiform gyrus while the surface area was larger in the right medial frontal, occipital pole, and anterior cingulate regions.
Sulcal depth was smaller in the VPT group in the bilateral dorsal parietal lobes and ventral inferior frontal lobes. Sulcal depth was deeper in regions of the right medial temporal, and medial parietal lobes compared to the full term group.
Follow-up analyses were conducted to determine if gestational age at birth in the preterm group was correlated with the gray matter metrics of interest. Partial correlations were calculated using values extracted from regions of interest (ROI) from the FreeSurfer automatic parcellation based on areas with significant group differences in the voxel-wise surface maps. After controlling for sex and age at scan, there was a significant partial correlation between GA and thickness in the right middle temporal (r[48] = 0.370, p = .008) and left middle temporal (r[48] = 0.314, p = .026) regions. For sulcal depth, there were significant partial correlations between GA and the right precuneus (r[48] = −0.322, p = .022) and right middle temporal (r[48] = −0.438, p = .001) regions. Significant partial correlations between GA and surface area were found in the left fusiform gyrus region (r[48] = 0.330, r = 0.019).
3. Discussion
We found a number of group differences in gray matter cortical morphometry between this group of preschool age children born preterm and children born full term in thickness and sulcal depth, but less so in terms of surface area. The preterm group had thinner cortex bilaterally within the temporal, superior middle frontal, and parietal/occipital junction, and thicker cortex within the dorsal portion of the medial occipital cortex bilaterally. The preterm group also showed shallower sulcal depth in regions of the bilateral dorsal parietal lobes and ventral inferior frontal lobes, with deeper sulcal depth in regions of the right medial temporal, and medial parietal lobes.
The areas of thicker cortex in our study of 5-year-old preterm children may represent areas where they are lagging behind in this phase of development (i.e., apparent regressive gray matter changes in thickness and surface area), since typically developing children and adolescents show robust, cortex-wide and near-linear cortical thinning from ages 3 to 20 years. Previous studies have demonstrated a similar pattern of thicker cortex in the frontal and occipital lobes in older children and adolescents born preterm. These areas may undergo the regressive processes (e.g., synaptic pruning) at a slower pace than full term children from early childhood through adolescence [10]. We replicated some of the previous findings of thinner cortex in the parietal and temporal lobes seen in older VLBW children [14,34]. These results may indicate that the preterm group is lagging behind in some progressive/proliferative developmental processes that cause gray matter to measure thicker on MRI (e.g., cell production, dendritic arborization, synapse elaboration) than should ordinarily be occurring at this age [4]. Thinner than normal cortex may also reflect early “hyper pruning” that occurs during the neonatal period as a consequence of the encephalopathy of prematurity. Overall, it is likely this pattern of thinner and thicker cortical regions in the preterm group compared to the full term group represents interruptions or delays in the typical processes of cell proliferation, dendritic arborization, and/or cell pruning that occur across different brain regions in early childhood. The results from previous studies of older children and adolescents suggest that the neuroanatomical differences we see in this group of 5-year-olds are likely to continue as these children mature.
We found smaller surface area only in the bilateral fusiform region, and larger surface area in the right medial frontal cortex and left occipital pole. This stands in contrast to previous studies of older children and young adults born preterm where cortical surface area was smaller across a wider expanse (i.e., prefrontal, lateral and ventral temporal, and lateral and medial parietal regions [9,13,14]. This may reflect the impact of premature birth on myelination, dendritic connections, and corticogeneis that extends through childhood and adolescence [9]. Although reduced surface area has been reported as early as term [35], these discrepancies may also reflect our exclusion of children with more birth-related risk factors often associated with lower gestational age at birth (i.e., < 28 gestational weeks).
We did not find much overlap in the regions where there were group differences in cortical thickness and surface area. Cortical thickness is thought to be dependent on the processes of gray matter dendritic arborization and pruning [36] and the degree of myelination at the gray/white matter interface [37]. Our data are consistent with recent studies that used surface-based measurement methods which show that between the ages of 4 and 6, cortical thickness decreases the most within medial and polar occipital and prefrontal regions, as well as within parietal cortex, declining by about 2% each year from the earliest ages that were studied (i.e., starting at age 3) through early adulthood [5,38].
Surface area measurements were generally similar between the groups. It is interesting to note that regions where sulcal depth was deeper in the preterm group overlapped with regions where cortical thickness was lower than expected. Additional studies, particularly using longitudinal data, would likely be helpful in elucidating the course and potential causes of these results by measuring the trajectories of cortical morphometry as these children mature [13,14].
Group differences were found in cortical thickness and sulcal depth in the right middle temporal gyri, and both were significantly correlated with GA at birth. Reduced thickness in this region was also found in young adults born preterm [7]. Perhaps the right middle temporal gyrus is vulnerable to damage in the third trimester. Thus, structural differences when children are older corresponds with that early damage or developmental differences within this region related to preterm birth [39]. Reduced sulcal depth and increased gyrification within the temporal lobes was also reported in two previous studies [20,21] but what this reflects at a neurobiological level is not clear.
The preterm children included in this study were recruited to be “low-risk”, without significant neonatal brain injury. The mean gestational age at birth of this group was 29.5 weeks. These results may therefore not generalize to children with more serious brain injury or serious health complications related to premature birth. More significant effects on gray matter morphometry may be present in children with lower GA, particularly those born at < 28 weeks. Given the cross-sectional nature of this study, like most studies in the literature, we cannot fully answer the question of developmental trajectory in cortical thickness, surface area, and sulcal depth.
In summary, the results of this study indicated differences in cortical morphometry between preschool-age children who were born preterm and children born full term. At age 5, widespread differences were found in measures of cortical thickness and sulcal depth. These results may help elucidate the pattern of brain development in this preterm population from early infancy to the outcomes reported in older children and young adults.
Acknowledgements
We thank all the children and their families who participated in this study. In addition, Drs. Martha Fuller, Yvonne Vaucher, John Hesselink, Terry Jernigan, Joan Stiles, and Anders Dale for their collaboration on this research project; and Drs. Roger Bakeman, Sarah Mattson, and Carrie McDonald for consultation.
Funding sources
This work was supported by grants R01HD075865 and R01HD061414 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Declaration of competing interest
The authors declare no conflicts of interest.
References
- [1].Volpe JJ, Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances, Lancet Neurol. 8 (1) (2009) 110–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Penn AA, Gressens P, Fleiss B, Back SA, Gallo V, Controversies in preterm brain injury, Neurobiol. Dis. 92 (Pt A) (2016) 90–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Brown TT, Jernigan TL, Brain development during the preschool years, Neuropsychol. Rev 22 (4) (2012) 313–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jernigan TL, Brown TT, Bartsch H, Dale AM, Toward an integrative science of the developing human mind and brain: focus on the developing cortex, Developmental Cognitive Neuroscience 18 (2016) 2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Brown TT, Kuperman JM, Chung Y, Erhart M, McCabe C, Donald J. Hagler Jr, et al. , Neuroanatomical assessment of biological maturity, Curr. Biol 22 (18) (2012) 1693–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Martinussen M, Fischl B, Larsson HB, Skranes J, Kulseng S, Vangberg TR, et al. , Cerebral cortex thickness in 15-year-old adolescents with low birth weight measured by an automated MRI-based method, Brain 128 (Pt 11) (2005) 2588–2596. [DOI] [PubMed] [Google Scholar]
- [7].Bjuland KJ, Lohaugen GC, Martinussen M, Skranes J, Cortical thickness and cognition in very-low-birth-weight late teenagers, Early Hum. Dev 89 (6) (2013) 371–380. [DOI] [PubMed] [Google Scholar]
- [8].Nagy Z, Lagercrantz H, Hutton C, Effects of preterm birth on cortical thickness measured in adolescence, Cereb. Cortex 21 (2) (2011) 300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lax ID, Duerden EG, Lin SY, Mallar Chakravarty M, Donner EJ, Lerch JP, et al. , Neuroanatomical consequences of very preterm birth in middle childhood, Brain Struct. Funct 218 (2) (2013) 575–585. [DOI] [PubMed] [Google Scholar]
- [10].Mürner-Lavanchy I, Steinlin M, Nelle M, Rummel C, Perrig WJ, Schroth G, et al. , Delay of cortical thinning in very preterm born children, Early Hum. Dev 90 (9) (2014) 443–450. [DOI] [PubMed] [Google Scholar]
- [11].Nam KW, Castellanos N, Simmons A, Froudist-Walsh S, Allin MP, Walshe M, et al. , Alterations in cortical thickness development in preterm-born individuals: implications for high-order cognitive functions, Neuroimage 115 (2015) 64–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Solsnes AE, Grunewaldt KH, Bjuland KJ, Stavnes EM, Bastholm IA, Aanes S, et al. , Cortical morphometry and IQ in VLBW children without cerebral palsy born in 2003–2007, Neuroimage: Clinical 8 (2015) 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rimol LM, Bjuland KJ, Lohaugen GCC, Martinussen M, Evensen KAI, Indredavik MS, et al. , Cortical trajectories during adolescence in preterm born teenagers with very low birthweight, Cortex 75 (2016) 120–131. [DOI] [PubMed] [Google Scholar]
- [14].Sripada K, Bjuland KJ, Solsnes AE, Haberg AK, Grunewaldt KH, Lohaugen GC, et al. , Trajectories of brain development in school-age children born preterm with very low birth weight, Sci. Rep 8 (1) (2018) 15553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Phillips JP, Montague EQ, Aragon M, Lowe JR, Schrader RM, Ohls RK, et al. , Prematurity affects cortical maturation in early childhood, Pediatr. Neurol 45 (4) (2011) 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Grunewaldt KH, Fjortoft T, Bjuland KJ, Brubakk AM, Eikenes L, Haberg AK, et al. , Follow-up at age 10 years in ELBW children - functional outcome, brain morphology and results from motor assessments in infancy, Early Hum. Dev 90 (10) (2014) 571–578. [DOI] [PubMed] [Google Scholar]
- [17].Skranes J, Lohaugen GC, Martinussen M, Haberg A, Brubakk AM, Dale AM, Cortical surface area and IQ in very-low-birth-weight (VLBW) young adults, Cortex 49 (8) (2013) 2264–2271. [DOI] [PubMed] [Google Scholar]
- [18].Dubois J, Benders M, Cachia A, Lazeyras F, Ha-Vinh Leuchter R, Sizonenko SV, et al. , Mapping the early cortical folding process in the preterm newborn brain, Cereb. Cortex 18 (6) (2008) 1444–1454. [DOI] [PubMed] [Google Scholar]
- [19].Engelhardt E, Inder TE, Alexopoulos D, Dierker DL, Hill J, Van Essen D, et al. , Regional impairments of cortical folding in premature infants, Ann. Neurol 77 (1) (2015) 154–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhang Y, Inder TE, Neil JJ, Dierker DL, Alexopoulos D, Anderson PJ, et al. , Cortical structural abnormalities in very preterm children at 7 years of age, Neuroimage 109 (2015) 469–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kesler SR, Vohr B, Schneider KC, Katz KH, Makuch RW, Reiss AL, et al. , Increased temporal lobe gyrification in preterm children, Neuropsychologia 44 (3) (2006) 445–453. [DOI] [PubMed] [Google Scholar]
- [22].Shimony JS, Smyser CD, Wideman G, Alexopoulos D, Hill J, Harwell J, et al. , Comparison of cortical folding measures for evaluation of developing human brain, Neuroimage 125 (2016) 780–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hasler HM, Akshoomoff N, Mathematics ability and related skills in preschoolers born very preterm, Child Neuropsychol. 25 (2) (2019) 162–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wechsler D, Wechsler Preschool and Primary Scale of Intelligence, Fourth edition, Pearson Assessments, San Antonio, TX, 2012. [Google Scholar]
- [25].White N, Roddey C, Shankaranarayanan A, Han E, Rettmann D, Santos J, et al. , PROMO: real-time prospective motion correction in MRI using image-based tracking, Magn. Reson. Med 63 (1) (2010) 91–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, et al. , Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain, Neuron 33 (3) (2002) 341–355. [DOI] [PubMed] [Google Scholar]
- [27].Jernigan TL, Brown TT, Hagler DJ, Akshoomoff N, Bartsch H, Newman E, et al. , The pediatric imaging, neurocognition, and genetics (PING) data repository, Neuroimage 124 (2016) 1149–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fischl B, Sereno MI, Dale AM, Cortical surface-based analysis. II: inflation, flattening, and a surface-based coordinate system, Neuroimage 9 (2) (1999) 195–207. [DOI] [PubMed] [Google Scholar]
- [29].IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY:IBM Corp. [Google Scholar]
- [30].Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. , An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest, Neuroimage 31 (3) (2006) 968–980. [DOI] [PubMed] [Google Scholar]
- [31].Cohen J, Things I have learned (so far), Am. Psychol 45 (12) (1990) 1304–1312. [Google Scholar]
- [32].Wilkinson L, the Task Force on Statistical Inference, American Psychological Association, Science Directorate, Statistical methods in psychology journals: guidelines and explanations, Am. Psychol 54 (8) (1999) 594–604. [Google Scholar]
- [33].Cohen J, Statistical Power Analysis for the Behavioral Sciences, 2nd ed., Lawrence Erlbaum Associates, Mahwah, N.J, 1988. [Google Scholar]
- [34].Zhou L, Zhao Y, Liu X, Kuang W, Zhu H, Dai J, et al. , Brain gray and white matter abnormalities in preterm-born adolescents: a meta-analysis of voxel-based morphometry studies, PLoS One 13 (10) (2018) e0203498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Inder TE, Warfield SK, Wang H, Huppi PS, Volpe JJ, Abnormal cerebral structure is present at term in premature infants, Pediatrics 115 (2) (2005) 286–294. [DOI] [PubMed] [Google Scholar]
- [36].Huttenlocher PR, Morphometric study of human cerebral cortex development, Neuropsychologia 28 (6) (1990) 517–527. [DOI] [PubMed] [Google Scholar]
- [37].Sowell ER, Thompson PM, Leonard CM, Welcome SE, Kan E, Toga AW, Longitudinal mapping of cortical thickness and brain growth in normal children, J. Neurosci 24 (38) (2004) 8223–8231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Walhovd KB, Fjell AM, Giedd J, Dale AM, Brown TT, Through thick and thin: a need to reconcile contradictory results on trajectories in human cortical development, Cereb. Cortex 27 (2) (2017) 1472–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Nosarti C, Giouroukou E, Healy E, Rifkin L, Walshe M, Reichenberg A, et al. , Grey and white matter distribution in very preterm adolescents mediates neurodevelopmental outcome, Brain 131 (Pt 1) (2008) 205–217. [DOI] [PubMed] [Google Scholar]