Abstract
This paper measures the cyclicality of an important input into elderly health: informal care. Using independent survey measures of informal caregiving and care receipt over the past two decades, we find that informal care from adult children to their elderly parents is countercyclical. By contrast, informal care from spouses is procyclical among individuals in their sixties. We find little corresponding change in the use of formal care, highlighting the potential for unmet care needs across the business cycle. These findings suggest that informal health inputs may play an important role in the interpretation of the cyclicality of elderly mortality.
1. Introduction
A large literature demonstrates that mortality is sensitive to macroeconomic conditions (see Ruhm (2012) and Ruhm (2015) for reviews). Among several posited mechanisms driving this relationship, the role of health care inputs has emerged as an important channel. This channel may be particularly relevant for the elderly, whose health and mortality is more directly dependent on healthcare inputs. Studies have shown that specific healthcare inputs, including nursing home quality, nursing home and hospital staffing, and the willingness of providers to ‘ccept Medicare patients, exhibit cyclical patterns, which may translate directly to elderly mortality (Stevens, Miller, Page et al., 2015; Konetzka, Lasater, Norton et al., 2018; Mclnerney and M Ilor, 2 12; Antwi and Bowblis, 2018). These estimates, however, concentrate on inputs from the formal healthcare system. In this paper, we explore the cyclicality of an often overlooked input into elderly health and well-being: informal long-term care.
The need for long-term care is a reality of aging: recent estimates suggest that 70% of 65 year olds in the United States will require assistance with basic functions at some point in their life (Hagen, 2013). While many individuals receive long-term care through formal channels such as nursing homes or paid in-home care, over half of long-term care is provided informally by family and friends. However, many informal caregivers are working-age children and spouses who face heavy demands on their time, and informal caregiving can come with significant opportunity costs (Fahle and McGarry, 2017; Van Houtven, Coe, and Skira, 2013; Ettner, 1996; Maestas and Truskinovsky, 2018). Given the scale of informal care and its potential interaction with the large and rapidly growing formal market for long-term care, it is important to understand if and how this key health input fluctuates with macroeconomic conditions.
To investigate the cyclicality of informal care, we examine the effect of business cycles on the supply of informal caregiving and on the composition of long-term care received by the elderly. Business cycles may affect informal care directly by changing the time cost of providing care, as wages and employment opportunities increase when the economy expands. With more time in the labor force (and thus a higher opportunity cost of time), individuals have less time to devote to caring for their loved ones. However, economic fluctuations can also affect the amount of informal caregiving through a number of other channels. First, business cycles may affect household wealth, which could impact the affordability of different long-term care options. For instance, exogenous increases in elderly income have been shown to induce the elderly to shift away from informal care and nursing homes towards formal in-home care (Goda, Golberstein, and Grabowski, 2011; Tsai, 2015). On the other hand, decreases in elderly income have also been shown to push caregiving spouses nearing retirement age back into the labor market (Fadlon and Nielsen, 2017). Second, business cycles may affect the supply of formal care through the price of formal care: if formal care becomes more costly during an expansion due to, for example, increased labor costs of formal care workers or fewer nursing home beds, an individual may turn to family or friends for care instead. Finally, business cycles may impact the supply of formal care not only through the price but also the quality of formal care. If the quality of the workforce in nursing homes or in other professional direct care occupations declines during an expansion, individuals may prefer to receive care from family at home (Konetzka, Lasater, Norton et al., 2018; Cawley, Grabowski, and Hirth, 2006; Antwi and Bowblis, 2018). While the opportunity cost of time channel suggests that the supply of informal care should unambiguously decrease during economic expansions, the resource channel suggests that the effect may vary, and the price and quality of formal care channels suggest that informal caregiving should instead increase. The overall effect of business cycles on informal care is thus an empirical question.
To identify the effect of business cycles on informal care and other long-term care outcomes, we exploit annual variation in economic conditions (the unemployment rate) across states and over time. In our main analysis, we use the American Time Use Survey (ATUS) from 2003 through 2015 to examine the cyclicality of the provision of informal care and the Health and Retirement Study (HRS) from 1995 through 2012 to examine the cyclicality of the receipt of informal care. We consider the nature of the care that responds to the business cycle by looking separately at help with Activities of Daily Living (ADLs), which includes help with physical limitations such as bathing, getting out of bed, and feeding, and help with Instrumental Activities of Daily Living (IADLs), which includes help with transportation, grocery shopping, preparing meals, home maintenance, and taking medication. To understand the channels through which macroeconomic conditions affect informal care, we also examine heterogeneity by age, caregiver relationship, education, marital status, and gender, and additionally examine the effects of macroeconomic conditions on employment and retirement outcomes of potential caregivers. Finally, we use the HRS and other data sources to consider how the demand for formal care and health outcomes respond to economic conditions.
We find that informal caregiving is countercyclical. A one percentage point increase in the unemployment rate increases the overall probability of providing informal care by 0.8 percentage points from a base of 13 percent. This pattern is largely driven by less educated, male caregivers, whose employment opportunities were more affected by recent downturns than other demographic groups (Hoynes, Miller, and Schaller, 2012). Consistent with the opportunity cost of time channel, much of this effect is driven by care provided on weekdays. We find that this overall caregiving result is mirrored by an increase in the likelihood of receiving informal care among a relatively older sample, but not a relatively younger sample, of the elderly: a one percentage point increase in the unemployment rate increases the likelihood of receiving informal care by 0.5 percentage points for individuals 70 and over (from a base of 18 percent), while it decreases the likelihood of receiving informal care by 0.8 percentage points for individuals 60–69 (from a base of 9 percent). For the older sample, this effect is concentrated in an increase in care from adult children, while for the relatively younger sample this effect is concentrated in a decrease in care from spouses, consistent with a resource channel. These opportunity cost and resource channels are corroborated by procyclical employment effects of adult children and, conversely, countercyclical employment effects for spouses of 60–69 year olds, possibly driven by impacts on household resources. In all samples, the margin of informal care that is most sensitive to these economic fluctuations is help with IADLs, a less time-sensitive category of caregiving. We find little evidence that these changes in informal care are offset by, or possibly driven by, concurrent changes in the use of formal long-term care, or changes in health outcomes.
We show that a simple conceptual model of long-term care and family labor supply can generate comparative statics in line with our main results. In our model, an elderly individual uses long-term care and can either receive it on the formal market or informally from her adult child or working-age spouse. Each type of care is characterized by its quality and its price, which is an explicit market price for formal care and an implicit opportunity cost for informal care. We show that in this model, informal care hours are a function of the potential caregiver’s wage, the quality of formal care, the price of formal care, and family resources. When economic expansions increase the potential caregiver’s wage but not the other parameters of the model, informal care decreases. When economic expansions additionally affect family resources or the price or quality of formal care, the effect on informal care becomes ambiguous.
This paper makes three main contributions. First, our finding that informal care for those age 70 and over is largely countercyclical suggests an additional explanation for the effects of aggregate unemployment rates on health that is distinct from the effects of own unemployment on health (Ruhm, 2000; Stevens, Miller, Page et al., 2015).1 Stevens, Miller, Page et al. (2015) show that the increased mortality during economic booms for the period 1976–2006 is concentrated among elderly women and nursing home residents, and argue that the countercyclical quality of health care in nursing homes make nursing home residents particularly susceptible to these fluctuations.2 While showing a direct link between informal care and mortality is outside the scope of this paper, our results suggest that the availability of informal care (or lack thereof) may be an additional and complementary mechanism for this empirical relationship and point to broader consequences of the elasticity of informal care for elderly well-being.
Second, we provide new evidence on the link between labor supply and informal caregiving by showing that macroeconomic conditions, either through directly affecting one’s employment opportunities, or through alternative feedback mechanisms (such as wealth effects or quality of care effects), alter informal caregiving decisions. Our results expand on a literature that finds a negative relationship between individual labor supply opportunities and informal caregiving (Bolin, Lindgren, and Lundborg, 2008; Van Houtven, Coe, and Skira, 2013; He and McHenry, 2016; Fahle and McGarry, 2017). This literature uses a variety of instruments—often related to family characteristics—to deal with the endogeneity of individual caregiving decisions and labor supply decisions (e.g., Carmichael, Charles, and Hulme, 2010); our study, on the other hand, focuses on macroeconomic phenomena that are plausibly exogenous to individual choices. Our emphasis on macroeconomic conditions reveals results distinct from the existing literature because macroeconomic conditions can affect informal caregiving in ways other than through one’s own labor market changes (as our conceptual framework formalizes).
More closely related to our paper, Costa-Font, Karlsson, and Øien (2016) find that the Great Recession in Europe significantly increased the availability of informal care, particularly from informal caregivers outside the household.3 Their focus is cross-country variation in the severity of unemployment changes during the Great Recession in Europe, and its effects on informal care receipt among individuals over 50. Our paper also finds countercyclical informal care receipt, and expands on these findings by examining the effect of more general labor market fluctuations (not only the Great Recession) within the United States on a more extensive set of outcomes, including informal care provision, informal care receipt, the relationship of the caregiver, and the use of formal care. Furthermore, we provide a conceptual framework to interpret these macro-driven effects.
Finally, our paper contributes new evidence to the literature on time use and caregiving. Studies that focus on another major type source of “informal” care – childcare – typically find that the elasticity of time dedicated to childcare is low (Kimmel and Connelly, 2007; Guryan, Hurst, and Kearney, 2008). In contrast, our findings suggest that caring for other adults is much more elastic, particularly for care for IADLs. In addition, this paper uses the best data available to measure informal care and is one of the first to use time use diary data from the ATUS as a measure of the supply of informal long-term care. Our similar findings from the HRS, a survey designed specifically to measure informal care receipt, allows us to compare and, ultimately, validate the ATUS as a meaningful measure of informal caregiving.
In the next section, we briefly review long-term care in the United States, and Section 3 proposes a simple model for understanding the various margins of adjustment of long-term care to business cycles. Section 4 describes our data and methodology. Section 5 presents our results on the cyclicality of the provision and receipt of informal care and explores mechanisms including employment responses, while Section 6 presents the effects on the use of formal care and on the health of the elderly. We conclude in Section 7.
2. Long Term Care in the United States
Long-term care is defined as assistance provided to individuals with functional or cognitive limitations that allows them to to maintain an “optimal level of functioning” (Family Caregiver Alliance, 2015). This assistance includes help with Activities of Daily Living (ADLs), which are basic self-care tasks such as bathing, toileting, eating, and getting in and out of bed, as well as help with Instrumental Activities of Daily Living (IADLs) such as household chores, grocery shopping and food preparation, managing finances, and medication adherence. Over 70% of 65 year olds will require some assistance with functional limitations in their lifetimes (Hagen, 2013).4
We define formal care as care that is purchased, either directly by the recipient or by another entity such as an insurance company or a social program. There is a now a continuum of formal long-term care options: care can be provided in an institutional setting, such as a nursing home, in assisted living facilities, or in-home by direct care workers such as home health aides or personal aides. Currently 18% of formal long-term care recipients are in a nursing home or other type of institution, although this share has been falling over the last decade (Houser, Fox-Grange, and Ujvari, 2015). Labor is the primary input into most long-term care services, and hence staffing levels, staff qualifications, and turnover can have a large impact on the quality of care that nursing home residents receive (Cawley, Grabowski, and Hirth, 2006; Antwi and Bowblis, 2018; Bostick, Rantz, Flesner et al., 2006; Collier and Harrington, 2008; Lin, 2014; Chen and Grabowski, 2015). In part due to its labor-intensiveness, formal care is expensive, both for individuals and for public program budgets. The average annual cost for a semi-private room in a nursing home was $90,000 in 2018 (Genworth, 2018), and this cost has grown approximately 4.5 percent per year between 2002 and 2012. The average hourly wage for a home health aide in 2011 was $19 (Houser, Fox-Grange, and Ujvari, 2015). Private insurance covers only 5% of these costs on aggregate, while 60% are paid by Medicaid, a means tested public insurance program. The remaining 35% are paid out of pocket. In comparison to other health costs, over 10% of all health expenditures for all ages went towards long-term care in 2013 (Kaiser Commission on Medicaid and the Uninsured, 2015).
A potential substitute to formal long-term care services is informal care from family and friends. Indeed, the bulk of long-term care is provided informally, and a growing literature finds that many long-term care services are substitutes (Van Houtven and Norton, 2004; Charles and Sevak, 2005; Mommaerts, 2018), and family care in some contexts may be of higher quality (Coe, Guo, Konetzka et al., 2019). Among elderly individuals who receive care, around 60% of care is from informal caregivers, while 40% is formal (Mommaerts, 2016). Among informal care recipients, most married individuals receive care from spouses, while the majority of informal care to unmarried (mostly widowed) individuals is from adult children. While informal care is uncompensated, it can come with significant costs. A literature has documented a negative relationship between caregiving and various own employment outcomes in a range of settings (Van Houtven, Coe, and Skira, 2013; Ettner, 1996; Maestas and Truskinovsky, 2018; Bolin, Lindgren, and Lundborg, 2008; Carmichael, Charles, and Hulme, 2010; Carmichael and Charles, 2003; Heitmueller, 2007). A simple calculation of foregone wages places the dollar value of lost wages for informal caregivers at just over $500 billion dollars in 2012 (Chari, Engberg, Ray et al., 2015), though these costs can be significantly higher when accounting for dynamic concerns such as human capital depreciation (Skira, 2015; Coe, Skira, and Larson, 2018). In addition to the time costs of caring, informal care can also have negative consequences for caregiver physical and emotional health (Coe and Van Houtven, 2009).
To conceptualize the trade-offs inherent in long-term care to families and the role of macroeconomic conditions, the next section sketches a model that accounts for many of the key factors for families when making decisions about long-term care outlined in this section: whether to use formal or informal care, opportunity costs of time for informal caregivers, the need for resources, and the price and quality of formal care.
3. Conceptual Framework
We develop a simple model of family labor supply and long-term care decisions that highlights the mechanisms through which macroeconomic conditions may influence the use of informal care: changes to the opportunity cost of time, changes to the formal care market (price and quality of care), and changes in family resources, Medicaid eligibility, and distance to family. The model consists of an elderly individual and a potential caregiver (e.g., an adult child or a working-age spouse) who jointly derive utility from total consumption C, leisure L, and quality-weighted hours of long-term care Q, with the utility function U(C) + V(L) + W(Q), where U, V, and W are increasing and concave functions.5 The elderly individual can receive care informally and formally, with hours of informal care supplied by the potential caregiver hc and hours purchased on the market (formal care) hf at price Pf per hour. The overall quality-weighted care is given by:
in which the quality of formal care, Qf, is constant per hour, while the total quality of informal care is an increasing, concave function g in the number of hours of informal care.6 This captures the idea that the first hours of informal care are of higher quality than further hours of informal care due to, for example, caregiver fatigue. The relative quality of informal care to formal care can also capture preferences over the source of care (for example, if some individuals have a strong preference to stay out of a nursing home). We stress that this formulation does not assume one type of care is necessarily of higher relative quality, only that unpaid informal care is of diminishing marginal quality.
The potential caregiver can spend her total time L0 in three different ways: market work hm for a wage w, informal care hc, and leisure L so that L0 = L + hc + hm. The family can spend its resources, which consist of an initial endowment R and labor income of the potential caregiver whm, on consumption C and formal care Pfhf, so that C + Pfhf < R + whm. The family thus maximizes utility subject to the budget constraint, time constraint, and quality of care definition:
| (1) |
Given the importance of Medicaid in this context, it is worth noting that this framework implicitly captures Medicaid eligibility through the level of family resources R, out-of-pocket costs for individuals enrolled in Medicaid through a low price of formal care (i.e., Pf ≈ 0), and the quality of Medicaid-financed long-term care through a potentially different quality level of care Qf.
This simple framework allows us to analyze the basic trade-offs inherent to long-term care decisions. First, as in standard models of labor supply, the marginal rate of substitution between consumption and leisure is equal to the wage when or the corner solution of occurs when In other words, the potential caregiver will not work for a wage if the value of the marginal increase in non-work time is greater than the value of the marginal increase in consumption from working an extra hour. Note that this framework does not have “involuntary” unemployment; instead we conceptualize unemployment as the corner solution on working hours that results from low wages. In other words, involuntary unemployment and w = 0 are equivalent in this simple static model. Since nobody would choose to work at zero wage, this is effectively involuntary unemployment. Second, the interior solution for the optimal hours of informal care is given by:
| (2) |
This equation shows that the marginal benefit of an additional hour of informal care, which is equal to the additional gain in quality g′ (hc) weighted by the marginal utility of quality, must equal the lost hour of time (which could otherwise be spent on leisure or market work) weighted by the marginal utility of leisure.7 Incorporating the interior solutions for labor market hours and hours of formal care gives:
| (3) |
Equation (3) can provide insight into how changes in the macro-economic environment E may affect informal care. We begin by assuming that the economic environment only affects wage offers w (again, proxying unemployment as very low wage offers). In this environment, changes in E will only affect informal care provision for those who also supply hours to market labor. It will also depend on the worker’s labor supply elasticity and thus may affect some types of workers more than others. For example, older workers (e.g., spouses of individuals who need care) may be more willing to continue working with lower wages to build retirement savings than younger workers (e.g., adult children of individuals who need care), who may be more sensitive to wage changes (Hoynes, Miller, and Schaller, 2012). Thus, totally differentiating Equation (3) with respect to E (in which a higher value of E captures more favorable macroeconomic circumstances) gives the following expression for the elasticity of informal care with respect to economic conditions:
| (4) |
Since g(·) is increasing and concave, the right hand side of Equation (4) is negative if economic expansions manifest as higher wages Thus, the model predicts that informal care is countercyclical. For those at the corner solution of an economic contraction (i.e., a decrease in wages) could induce some individuals to begin providing informal care.
This result assumes that macroeconomic fluctuations only affect wages. If economic conditions additionally affect parameters of the formal care market, (e.g. prices or quality), this may also have an impact on the elasticities of informal and formal care.8 For example, if an economic expansion drives up formal care sector wages and hence the price of formal care or drives down the quality of formal care if it is more difficult to hire good workers during expansions then Equation (4) will include additional terms:
| (5) |
The first term in the round brackets is the effect of an economic expansion on informal care through employment (wage) effects (i.e., Equation (4)). The second and third terms are the indirect effects through changes in the price and quality of formal care, respectively. If then these terms exerts a positive effect on the elasticity of informal care with respect to economic conditions. Thus, while the basic model shows that there is an unambiguously negative effect of economic expansions on informal care, when we extend the model to include indirect effects through the parameters of the formal care market, the overall relationship becomes ambiguous.
We end with a discussion of the effects on informal care if other components of the model are affected by macroeconomic conditions, including resources, Medicaid eligibility, and proximity to family. First, if economic downturns reduce resources R (such as through a decrease in the value of savings accounts or housing assets), then the simple model suggests that informal care is only impacted if resources are so low that the potential caregiver must work more and provide less informal care in order to fund formal care expenses (in other words, if the family is at a corner solution and thus their reservation wage for working is very low). In a dynamic version of this model, a forward-looking agent may also choose to work more in response to a large reduction in R to better smooth consumption over time. Second, while Medicaid is not explicitly modeled in our framework, it can be approximated by low R and low Pf since Medicaid pays for formal care. Thus, if economic downturns increase the likelihood of Medicaid enrollment through a decrease in R (and subsequently a decrease in Pf), this may additionally cause an ambiguous effect of economic conditions on informal care. Finally, distance to family could be important for informal caregiving if the amount of hours one must spend to provide hc differs from hc (e.g., driving time) such that the budget constraint incorporates hD = f(D, hc) in the place of hc. Then, if macroeconomic conditions affect proximity to family, for example if adult children move closer to—or start coresiding with—parents (i.e., dD/dE > 0), and closer proximity makes the provision of hc less costly (i.e., dhD/dD > 0), then migration in response to macroeconomic fluctuations could also be a channel through which informal care reacts to business cycles.
In sum, a simple model of labor supply, informal care, and formal care predicts that macroeconomic conditions will affect the decision to use informal care. Specifically, the basic model shows that when the economy expands, informal care falls, but that the sign of this elasticity becomes ambiguous once we account for changes in formal care prices and quality, as well as resource effects. If downturns affect the opportunity cost of time for younger households (i.e., adult children) more strongly than older households (i.e., spouses), as Hoynes, Miller, and Schaller (2012) shows, affect the resources of older households more strongly than younger households, or impact the distance between parents and adult children more than between spouses (since spouses typically already live together), we would expect to see a more countercyclical effect on informal care from adult children and a potentially procyclical effect on care from spouses. In the next section, we turn to the data and empirical specification to test these theoretical predictions.
4. Data and Empirical Specification
To examine the effect of macroeconomic conditions on informal care, we use three main datasets: the American Time Use Survey for information on the provision of informal care, the Health and Retirement Study for information on the receipt of informal and formal care, and the Local Area Unemployment Statistics for our measure of macroeconomic conditions.
4.1. Caregivers
Our measure of informal caregiving comes from the American Time Use Survey (ATUS).9 The ATUS, which began in 2003, surveys a nationally representative sample of around 10,000 Americans from the Current Population Survey aged 15 and over each year about how they spend their time. Each respondent records their activities for a single 24 hour period in 15 minute intervals, and these activities are then classified into detailed time-use categories. The ATUS also includes basic demographic information about the respondent and other household members. Our sample consists of all ATUS respondents aged 18 and over from 2003 through 2015 for a total of over 160,000 observations. We drop individuals who report their occupation as direct care worker (such as personal aide, home health aide, or a nurse’s aide) since we cannot distinguish whether the time spent caring for someone is formal or informal for these individuals.
We construct three measures of caregiving: “ADL care,” “IADL care,” and any care. Individuals are defined as providing ADL care if any of the activities they list are classified as “Caring for another adult inside or outside the household,” which include providing physical or medical care and looking after an adult as a primary activity. Individuals are defined as providing IADL care if any of the activities they list are classified as “Helping another adult inside or outside the household,” which consist of housekeeping and maintenance, grocery shopping and food preparation, and help with transportation, distinct from doing such activities for oneself (see Appendix A for more details). Finally, individuals are defined as providing any (informal) care if they provide either ADL care or IADL care. An important qualification to this measure is that we cannot distinguish care to the elderly and care to non-elderly individuals. Given that two-thirds of long-term care recipients are age 65 and over, it is likely that the majority of the care we measure is for the elderly.
The ATUS provides a novel perspective on caregiving. Relying on time diaries means our caregiving measure may capture respondents who might not identify themselves as caregivers if asked directly. As a result we likely pick up individuals performing care activities who may not show up in other contexts. At the same time, because we identify care behavior from a snapshot of a single day of the week, we likely miss many regular caregivers who don’t provide care daily. We also know that the care recipient is an adult and whether they coreside with the caregiver, but we cannot otherwise identify the relationship of the care recipient. While these features suggest that our measure of informal caregiving may be noisy, it is nevertheless a rare source of annual, nationally representative caregiving information that captures 15 years of data.
Table 1 reports summary statistics for this ATUS sample. 13% of respondents report providing any type of care to another adult, of which the majority (9% overall) went to non-household members. Over 11% of respondents, or 84% of those who provided any care, provided help with IADLs. 3% of ATUS respondents, or just under a quarter of those providing any care, provided help with ADLs. While the majority of IADL care is provided to individuals outside the household, the majority of ADL care is providing to individuals within the household, reflecting that this more physically demanding and likely time-sensitive form of caregiving is provided to a coresident spouse or parent. Conditional on providing any care, respondents provided 52 minutes of care on the day in question, or 42 minutes for help with IADLs and 77 minutes for help with ADLs. Finally, in statistics not shown, ADL care appears to be more time-intensive: while just 27% of IADL care lasted 30 or more minutes on the survey day, almost 50% of ADL care did, and 33% lasted at least 60 minutes.
Table 1:
Summary statistics
| American Time Use
Survey |
Health and Retirement
Study |
|||||||
|---|---|---|---|---|---|---|---|---|
| Full sample |
Caregivers |
Full sample |
Informal care recipients |
Care from adult children |
Care from spouse |
Formal care recipients |
||
| Age | 46.3 | 45.9 | Age | 67.3 | 72.3 | 74.4 | 69.3 | 80.0 |
| Female | 0.51 | 0.54 | Female | 0.58 | 0.62 | 0.77 | 0.45 | 0.71 |
| White | 0.70 | 0.71 | White | 0.79 | 0.72 | 0.67 | 0.79 | 0.78 |
| Married | 0.57 | 0.58 | Married | 0.68 | 0.59 | 0.36 | 1.00 | 0.28 |
| High school or less | 0.44 | 0.44 | Less than high school | 0.28 | 0.48 | 0.53 | 0.42 | 0.42 |
| Employed | 0.65 | 0.61 | Any kids | 0.93 | 0.94 | 1.00 | 0.96 | 0.87 |
| Unemployed | 0.05 | 0.07 | Owns LTC policy | 0.11 | 0.07 | 0.06 | 0.09 | 0.09 |
| Not in labor force | 0.30 | 0.32 | Medicaid | 0.09 | 0.22 | 0.28 | 0.12 | 0.35 |
| Any care | 0.13 | 1.00 | Fair/poor health | 0.30 | 0.69 | 0.71 | 0.70 | 0.60 |
| Outside the house | 0.09 | 0.66 | IADL difficulty | 0.16 | 0.86 | 0.92 | 0.81 | 0.71 |
| Minutes/day (if any) | 52 | 52 | ADL difficulty | 0.18 | 0.71 | 0.74 | 0.70 | 0.69 |
| IADL care | 0.11 | 0.84 | Any informal care | 0.12 | 1.00 | 1.00 | 1.00 | 0.31 |
| Outside the house | 0.08 | 0.59 | Any help w/ IADLs | 0.12 | 0.75 | 0.81 | 0.71 | 0.72 |
| Minutes/day (if any IADL) | 42 | 42 | Any help w/ ADLs | 0.09 | 0.53 | 0.55 | 0.57 | 0.67 |
| ADL care | 0.03 | 0.23 | Nursing home resident | 0.02 | 0.00 | 0.00 | 0.00 | 0.36 |
| Outside the house | 0.01 | 0.07 | In-home formal care | 0.02 | 0.13 | 0.17 | 0.07 | 0.37 |
| Minutes/day (if any ADL) | 77 | 77 | Assisted living | 0.02 | 0.04 | 0.05 | 0.02 | 0.32 |
| Household income | 55,000* | 55,000* | Household income | 67,742 | 36,464 | 26,823 | 52,019 | 30,423 |
| Household size | 2.9 | 3.0 | Household wealth | 445,667 | 244,674 | 162,093 | 356,950 | 247,080 |
| N | 161,067 | 20,524 | N | 162,118 | 20,089 | 10,306 | 10,017 | 10,005 |
Note: Table reports means from the weighted sample of individuals aged 18 and over whose occupation is not related to caregiving from the pooled 2003–2015 American Time Use Survey (left) and the sample of individuals over 50 from the pooled 1995–2012 Health and Retirement Study (right). Household income in the ATUS is bracketed, and the statistic shown is the median bracket in the sample.
Table 1 also reports demographic characteristics for both the full sample and the subsample of caregivers. The full sample is 51% female, 70% white, and the average age is 46. 57% of respondents are married, just under 45% have a high school education or less, 65% are employed, and 32% are out of the labor force at the time of the survey. The subsample of caregivers is demographically similar to the full sample, but are slightly more likely to be female (54%), and less likely to be employed (61%).
4.2. Care Recipients
For our analysis on the receipt of long-term care, we use data from the Health and Retirement Study (HRS), a nationally representative longitudinal survey of individuals over age 50 that began in 1992 and continues biennially.10 The survey contains detailed questions about health, care receipt, wealth, income, and demographic and family information. Our sample consists of all respondents from 1995 (when care outcomes were first asked) to 2012. As with the caregiver analysis, we construct three measures of informal care: whether the respondent received any informal care, any informal ADL care, and any informal IADL care. We define informal care as care for an ADL or IADL limitation received outside of an institution that was uncompensated, ADL care as the subset of care involving help with dressing, walking, bathing, eating, getting in/out of bed, and toileting, and IADL care as the subset involving help with meal preparation, grocery shopping, making phone calls, taking medication, and managing money. We distinguish between sources of care: specifically, we separately identify care provided by adult children and care provided by spouses. We also construct four measures of formal care: whether the respondent received any formal care (defined as any care that was paid), whether the respondent resides in a nursing home, whether the respondent lives in an assisted living facility and makes use of at least one of the offered services, and whether the respondent received formal (paid) care in their home.11 All outcomes, with the exception of nursing home status and assisted living status, are reported in reference to the previous month. In addition, care outcomes were only ascertained if the respondent first reported difficulty performing an ADL or an IADL. As a result, this measure captures a notion of caregiving that responds to a specific need, and is thus a more restrictive definition of care than that in the ATUS, which has somewhat broader notions of ADL and IADL 12 care.12
Table 1 reports summary statistics for the full HRS sample, the sample of informal care recipients (12% of respondents), informal care recipients split by the source of their care (approximately half report receiving care from adult children, and half from spouses), and formal care recipients.13 Overall, the sample of care recipients looks more socioeconomically disadvantaged than the full HRS sample. They are older, more likely to be female, less likely to be white, married or to have a high school diploma. Their average household income and wealth are significantly lower than the full sample, they are also less likely to own a long-term care insurance policy, and more likely to be on Medicaid. They are also in poorer physical health: among informal care recipients, 86% (71%) report difficulty with at least one IADL (ADL), compared with 16% (18%) of the full sample. Those who receive spousal care are younger, more likely to be male, more educated, and less likely to be on Medicaid than those who receive care from their adult children. Care recipients are also more likely to receive informal care for IADL difficulties than ADL difficulties, mirroring the differential frequency of help provided by caregivers in the ATUS sample.
4.3. Empirical Specification
To identify the effect of macroeconomic conditions on informal care, we follow the standard approach in the literature on the cyclicality of mortality that exploits differences in economic conditions across states and over time (Ruhm, 2000). Our measure of macroeconomic conditions is the state-level annual unemployment rate, which is the average of the 12 monthly unemployment rates for each state. This measure is compiled from the Local Average Unemployment Statistics, which is produced by the Bureau of Labor Statistics. Our main set of regressions take the following form:
| (6) |
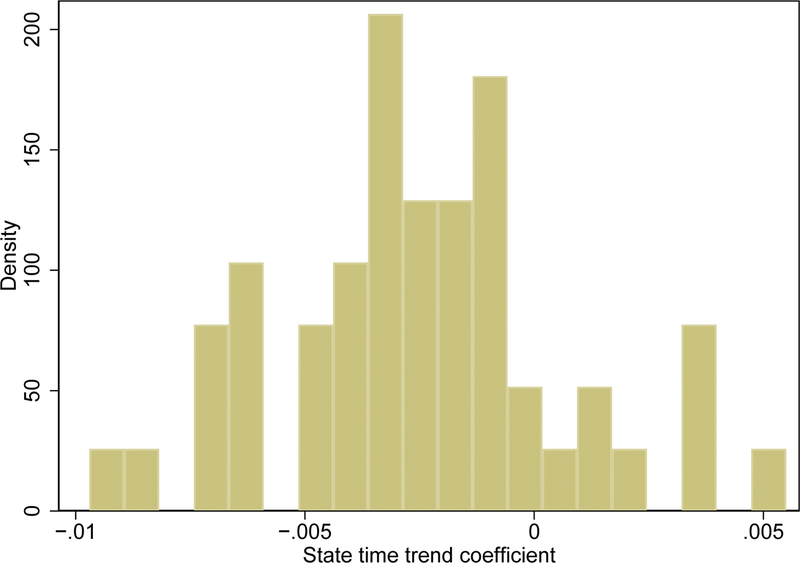
in which Yijt is an outcome variable of interest for individual i in state j in year t. αt and Sj are year and state fixed effects, respectively, t · δj are state linear time trends, and Xijt is a vector of demographic controls, including age, gender, education, marital status, race and ethnicity.14 We include state-specific time trends because caregiving and care receipt appear to follow differential trends by state.15 In addition to individual-level controls, we also control for the share of a state’s population that is aged 18–64 and over 65 as well as the log of the state’s annual Medicaid expenditures on older adults and people with physical disabilities and the log of the subset of those expenditures spent on home and community-based services (HCBS). These controls, in addition to state linear time trends, help address the concern that macroeconomic conditions may be correlated with care outcomes through changes in demographic characteristics and the Medicaid program of the state. Ejt is a measure of state j’s economic conditions in year t (i.e., the state annual unemployment rate), and γ is the coefficient of interest. We cluster at the state level, and the ATUS results are weighted using individual-level weights.16
5. Effect of Macroeconomic Conditions on Informal Care
This section reports the effect of macroeconomic conditions on both the likelihood of providing informal care and the likelihood of receiving informal care. As described in Section 4, we use the American Time Use Survey from 2003–2015 to measure informal care provision and the Health and Retirement Study from 1995–2012 to measure informal care receipt.
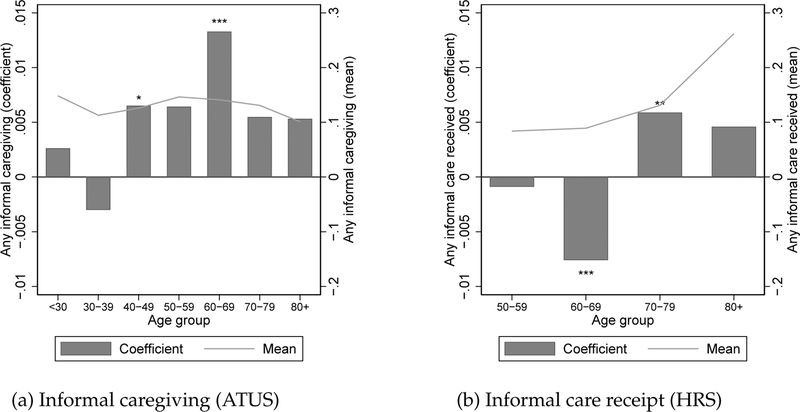
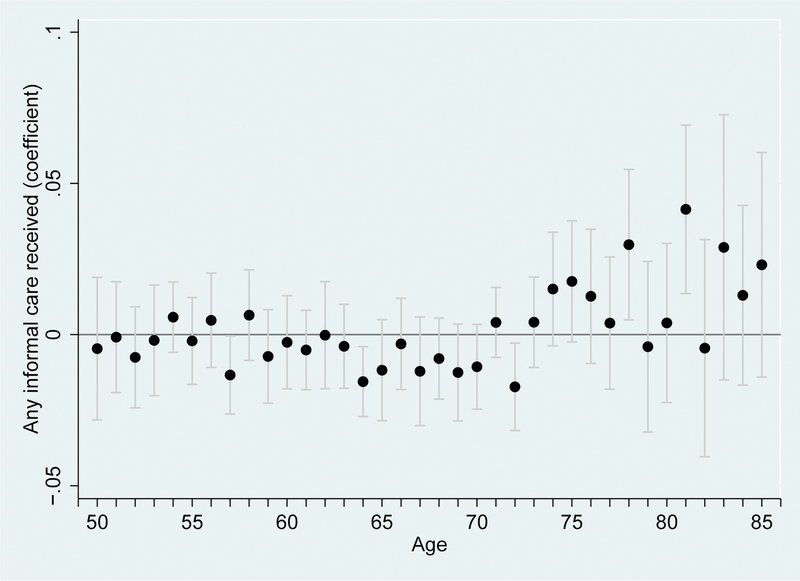
We begin by estimating Equation (6) across the age distributions of potential caregivers and care recipients. Figure 1 reports the γ coefficients for any informal care provision (Panel A) and any informal care receipt (Panel B) in ten-year age bins (dark gray bars corresponding to the left y-axis), as well as the average rate of informal care per bin (light gray lines corresponding to the right y-axis). We find that caregiving is largely countercyclical across the age distribution of potential caregivers starting around age 40: the peak at age 60–69 shows that a one percentage point increase in the unemployment rate increases informal caregiving by 1.3 percentage points. Care receipt, on the other hand, is countercyclical for individuals aged 70 and over, but procyclical for individuals in their sixties. Because of these stark differences in cyclicality by age of care recipients, our remaining analyses separately estimate effects for care recipients aged 60–69 and aged 70 and over.17 For care provision, we focus on the sample of potential caregivers aged 40 and
Figure 1:
Effect of macroeconomic conditions on informal care, by age
Notes: Bars denote coefficients on separate regressions of any informal caregiving in the ATUS in panel (a) and any informal care received in the HRS in panel (b) on the unemployment rate for each age group. All specifications are estimated using a linear probability model and control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. HRS regressions additionally control for number of children. The ATUS regressions additionally control for family size and are weighted using individual-level weights. Standard errors are clustered by state. Mean rates of caregiving and care receipt by age bin are denoted by the solid line. * p < 0.10, ** p < 0.05, *** p < 0.01
Table 2 reports the results of these age groupings for our main outcomes of interest. The first panel presents results for the ATUS sample of potential caregivers aged 40 and over, while the second and third panels present results for the HRS samples of potential care recipients aged 60–69 and aged 70 and over, respectively.18 Column (1) reports the pooled effects of Figure 1: a one percentage point increase in the unemployment rate increases the likelihood of informal caregiving in our sample by 0.79 percentage points. Given that the average rate of informal caregiving in this sample is 13.4%, this constitutes a 5.9% increase in the likelihood of providing informal care. This is consistent with a 0.48 percentage point increase in receipt of informal care for the sample aged 70 and over (a 2.6% increase), though it is in sharp contrast with the 0.76 percentage point decrease in care receipt for those aged 60–69 (an 8.5% decrease). These coefficients correspond to 134,000 more individuals 70 and over and 222,000 fewer individuals 60–69 being cared for informally in the United States in response to a one percentage point increase in the unemployment rate. In comparison, Stevens, Miller, Page et al. (2015) analogously finds a decrease in 4,600 deaths among individuals 70 and over (an effect that is 3.4% the size of the informal care effect for this age group).
Table 2:
Effects of macroeconomic conditions on informal caregiving and informal care receipt
| Type of care |
Source of care |
||||
|---|---|---|---|---|---|
| Any care (1) |
ADLs (2) |
IADLs (3) |
Children (4) |
Spouse (5) |
|
| Outcome: informal caregiving among 40+ | |||||
| Unemployment rate | 0.0079*** | 0.0028* | 0.0062*** | N/A | N/A |
| (0.0022) | (0.0015) | (0.0017) | |||
| Observations | 105741 | 105741 | 105741 | ||
| Mean dependent variable | 0.134 | 0.039 | 0.106 | ||
| Outcome: informal care receipt among 60–69 | |||||
| Unemployment rate | −0.0076*** | −0.0031* | −0.0061** | −0.0029 | −0.0060*** |
| (0.0026) | (0.0016) | (0.0025) | (0.0023) | (0.0017) | |
| Observations | 52530 | 52530 | 52530 | 52435 | 52530 |
| Mean dependent variable | 0.089 | 0.043 | 0.064 | 0.039 | 0.054 |
| Outcome: informal care receipt among 70+ | |||||
| Unemployment rate | 0.0048** | 0.0021 | 0.0055** | 0.0046** | 0.0007 |
| (0.0022) | (0.0013) | (0.0022) | (0.0018) | (0.0020) | |
| Observations | 62850 | 62850 | 62850 | 62778 | 62850 |
| Mean dependent variable | 0.182 | 0.079 | 0.142 | 0.103 | 0.077 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model. The first panel uses data from the ATUS sample, while the second and third panels use data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. HRS regressions additionally control for number of children a respondent has. The ATUS regressions additionally control for family size and are weighted using individual-level weights. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Informal care - and long-term care more generally - encompasses a wide range of activities and services, some of which may be more sensitive to economic fluctuations than others. Moreover, one potential reason for the differential effect of macroeconomic conditions between relatively younger and older care recipients is that their care needs differ and are differentially sensitive to business cycles. To investigate this, the next two columns distinguish between help with Activities of Daily Living (ADLs, column 2) and help with Instrumental Activities of Daily Living (IADLs, column 3). Over 10% of our potential caregiver sample provides help with IADLs, while fewer than 4% provide help with ADLs. This is mirrored by higher informal care recipiency rates for IADL care than ADL care for the elderly sample, and is consistent with the idea that ADL care is much more labor- and time-intensive than IADL care, and thus is a responsibility that many families cannot shoulder without paid help. The γ coefficients reveal that IADL care is also more sensitive to macroeconomic conditions than ADL care: a one percentage point increase in the unemployment rate significantly increases IADL caregiving by 0.6 percentage points, while it only increases ADL care by a marginally significant 0.3 percentage points. This pattern is mirrored in both samples of care recipients, and the effects are again opposite-signed for the 60–69 age group. Thus, differential care need by age does not appear to be a driver of the difference in sign between relatively older and younger care recipients.
We next examine the effect of macroeconomic conditions on the relationship of informal caregivers to recipients. Around half of informal care recipients in Table 1 receive care from their adult children, while the other half receive care from spouses. Given that individuals who receive care from adult children are typically older and more disadvantaged than those who receive care from spouses, the opposite-signed cyclicality effects could be associated with the source of care. To investigate this channel, the next two columns distinguish between any informal care by adult children (column 4) and informal care by spouses (column 5).19 The procylical patterns in informal care receipt among those aged 60–69 are indeed driven by spousal care: a one percentage point increase in the unemployment rate is associated with a 0.6 percentage point decrease in spousal care (or 11%) and an insignificant 0.3 percentage point decrease in care from adult children. Conversely, among those aged 70 and over, care from adult children increases by 0.5 percentage points (4.5%) and there is no effect on spousal care.
These results are robust to a range of alternative specifications and assumptions. Appendix Table 2 shows that the results are almost identical when we use an alternative definition that does not restrict receipt of informal care to community residents. Appendix Table 3 shows that the care receipt results are largely the same when weights are used when available (they are only available for nursing home residents starting in 2000), but slightly less precise given the smaller sample size. Next, our specification assumes that there are no cross-state migration responses. If there were, then we might attribute the wrong state unemployment rate (and other state covariates), which would create measurement error and thus bias the results toward no effect. We test for more general migratory responses in Appendix Table 4 and find no effects in either sample for whether the respondent lives near (within 10 miles), and only marginally significant effects on coresidence with an adult child for the 70 and over sample. This is consistent with Bitler and Hoynes (2015), which finds very small effects of the Great Recession on living arrangements of families. We also examine the effects of business cycles on attrition from the sample (including death) in Appendix Table 5. Attrition in response to the business cycle could introduce bias into our informal care estimates if less healthy individuals are more likely to attrit (through death, for example) or if healthier individuals become unemployed and as a result are less likely to attrit because they have more time to respond to surveys, but we find no evidence of this. Next, Appendix Table 6 uses the employment-to-population ratio as an alternative measure of macroeconomic conditions and finds results similar to our main specification. Appendix Table 7 examines the intensive margin of caregiving in the ATUS sample and finds effects on the unconditional minutes of caregiving per day, but not conditional on non-zero minutes of care. Similarly, Appendix Table 8 examines the intensive margin of care receipt in the HRS sample and finds effects on the unconditional hours of total care (informal and formal) per day for the 70 and over sample, but insignificant effects otherwise. Appendix Table 9 adds the lagged unemployment rate and finds that the effects largely load on the contemporaneous unemployment rate except for care receipt among the 70 and over population, for which the effects are less clear. Logit and probit results are reported in Appendix Table 10 and show similar effects. Finally, Appendix Table 11 shows that there are negligible effects for the subsamples without any ADL limitations, and much larger effects effects for the subsamples with ADL limitations.
These findings suggest that the provision and receipt of informal care is sensitive to macroeconomic fluctuations, particularly care for less time-intensive IADLs. While the overall caregiving effect is countercyclical, this masks significant heterogeneity by the age of the recipient and the relationship of the caregiver: care to relatively older individuals by adult children is strongly countercyclical, while care to relatively younger individuals by spouses is strongly procyclical. In the next section, we further break down the results to better understand the potential channels for these divergent effects.
5.1. Heterogeneous Effects
One predominant mechanism through which macroeconomic conditions may affect informal care is through the opportunity cost of time of potential caregivers (see Section 3).20 To investigate this channel, we examine the caregiving effects separately by educational attainment, day of the week surveyed, and gender of potential caregivers. Potential caregivers with low levels of education are more likely to face reduced employment opportunities during economic downturns (Hoynes, Miller, and Schaller, 2012), so if our main effects operate through an opportunity cost of time channel then we would expect low-educated caregivers to be more sensitive to economic fluctuations. Likewise, if the opportunity cost of time is higher on weekdays, then weekday caregiving may be more sensitive to economic fluctuations than weekend caregiving. Finally, although men are slightly less likely to provide informal care and their labor supply is typically less elastic than women’s labor supply, their employment is more likely to be affected by economic downturns (Hoynes, Miller, and Schaller, 2012), and thus we might expect their caregiving behavior to be more sensitive to economic conditions than female caregiving.
Table 3 reports these results. The first two columns report coefficients for each subsample, and the third column reports the p-value of the difference in coefficients across the two subsamples. The first panel reports the effect of the unemployment rate separately by educational attainment of potential caregivers. We report results separately for potential caregivers who never attended college and those who have at least some college experience. While around 13% of both groups provide informal care, the response of this care to macroeconomic conditions is very different: potential caregivers with no college experience increase the probability of caregiving by 1.5 percentage points (12%) in response to a one percentage point increase in the unemployment rate, compared to no response from those with at least some college experience, and these coefficients are statistically different. These differential findings by education are in line with an opportunity cost of time channel.
Table 3:
Heterogeneous effects of macroeconomic conditions on informal caregiving
| By education of potential caregiver | No college | College | P-value of difference |
| Unemployment rate | 0.0155*** | 0.0021 | [0.015] |
| (0.0040) | (0.0029) | ||
| Observations | 43750 | 61991 | |
| Mean dependent variable | 0.131 | 0.137 | |
| By day of week of interview | Weekdays | Weekends | P-value of difference |
| Unemployment rate | 0.0087*** | 0.0059* | [0.494] |
| (0.0027) | (0.0032) | ||
| Observations | 52976 | 52765 | |
| Mean dependent variable | 0.133 | 0.137 | |
| By gender of potential caregiver | Males | Females | P-value of difference |
| Unemployment rate | 0.011*** | 0.0057 | [0.399] |
| (0.0035) | (0.0036) | ||
| Gender-specific rates: | |||
| Male | 0.0070** | 0.0073** | |
| (0.0032) | (0.0031) | ||
| Female | 0.0011 | −0.0040 | |
| (0.0041) | (0.0049) | ||
| Observations | 46388 | 59353 | |
| Mean dependent variable | 0.121 | 0.146 | |
Notes: Data from the ATUS sample of individuals 40 and over. Each cell in the first two columns reports the coefficient on the state annual unemployment rate from a separate linear probability model, except the two rows with gender-specific rates, which are jointly estimated. The third column reports the p-value of the difference in coefficients between the first and second column. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, family size, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state, and are weighted using individual-level weights. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01.
The second panel reports the effect of the unemployment rate on caregiving separately during weekdays and weekends, and shows that business cycle effects are larger for care provided during weekdays. Specifically, a one percentage point increase in the unemployment rate increases weekday caregiving by a significant 0.85 percentage points, while the weekend increase is an insignificant 0.5 percentage points. While these effects are not statistically different, they are also suggestive of the opportunity cost of time channel.
The final panel shows results by gender using two different specifications per column: the first uses the overall unemployment rate, and the second uses separate gender-specific unemployment rates. Interestingly, the average rates of informal care do not differ dramatically by gender, with 15% of females and 12% of males providing informal care.21 Using the overall unemployment rate as the measure of macroeconomic conditions implies that informal care increases during downturns for both genders, but only significantly so for males: a one percentage point increase in the unemployment rate increases male caregiving by one percentage point and female caregiving by an insignificant 0.57 percentage points. If male employment is more affected by economic downturns, this result supports the opportunity cost of time as the primary channel through which business cycles affect informal caregiving. However, using gender-specific unemployment rates tests this more directly and suggests a more nuanced story: both male and female caregiving increase in response to the male unemployment rate but not the female unemployment rate. While the male caregiving result is consistent with an opportunity cost of time story, the female caregiving result suggests that female caregiving is not responding to a change in their own opportunity cost of time. Instead, this effect may be occurring through an alternative channel, such as a response to a change in resources or the price or quality of formal care. We further investigate the resource channel in Section 5.2 and the formal care channel in Section 6.
Table 4 reports effects on care recipients by education, marital status, and gender. While heterogeneous effects by the education of the caregiver are potentially indicative of an opportunity cost of time channel, heterogeneous effects by education of the care recipient may be more indicative of a resource channel. Here again, the source of care plays an important role. For instance, elderly individuals may experience negative resource shocks during downturns (McKernan, Ratcliffe, Steuerle et al., 2014), prompting them to substitute towards cheaper (and possibly informal) sources of care. However, among the relatively younger elderly, such a resource shock may instead prompt a spouse to remain in the labor force rather than take on caregiving responsibilities. This may be more relevant for individuals with lower resources to begin with, as proxied by education.22 The first panel, which reports effects separately for the 60–69 and 70 and over samples, shows that, conditional on age, those who never attended college are about twice as likely to report receiving informal care as those who have at least some college.23 Correspondingly, individuals who never went to college experience significant fluctuations in their informal care arrangements with the business cycle: low-educated individuals aged 60–69 are 1.3 percentage points (12%) less likely to receive informal care when the unemployment rate increases by one percentage point, while those aged 70 and over are one percentage point (4%) more likely to receive informal care. In contrast, there are negligible and insignificant effects for the more educated sample for either source of care. These results suggest a resource effect, but given the high correlation in education levels across generations, it is difficult to tease out this channel.
Table 4:
Heterogeneous effects of macroeconomic conditions on informal care receipt
| Age 60–69 | Age 70+ | |||||
|---|---|---|---|---|---|---|
| By education of potential care recipient | No college | College | P(diff) | No college | College | P(diff) |
| Unemployment rate | −0.0137*** | −0.0005 | [0.00] | 0.0096** | −0.0039 | [0.01] |
| (0.0036) | (0.0030) | (0.0039) | (0.0042) | |||
| Observations | 30987 | 21543 | 41068 | 21782 | ||
| Mean dependent variable | 0.113 | 0.054 | 0.211 | 0.126 | ||
| By marital status of potential care recipient | Married | Not married | P(diff) | Married | Not married | P(diff) |
| Unemployment rate | −0.0085*** | −0.0047 | [0.56] | 0.0034 | 00073* | [0.57] |
| (0.0028) | (0.0052) | (0.0037) | (0.0046) | |||
| Observations | 39289 | 13252 | 34396 | 28457 | ||
| Mean dependent variable | 0.084 | 0.103 | 0.163 | 0.204 | ||
| By gender of potential care recipient | Male | Female | P(diff) | Male | Female | P(diff) |
| Unemployment rate | −0.0089** | −0.0064* | [0.53] | 0.0034 | 0.0058* | [0.52] |
| (0.0035) | (0.0034) | (0.0044) | (0.0039) | |||
| Observations | 23404 | 29126 | 26141 | 36712 | ||
| Mean dependent variable | 0.078 | 0.097 | 0.165 | 0.193 | ||
Notes: Data from the HRS samples of individuals 60–69 (first three columns) and individuals 70 and over (last three columns). Aside from the columns reporting “P(diff)”, each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model. The “P(diff)” columns report the p-value of the difference in coefficients between the two columns to the left. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01.
The second and third panels of Table 4 distinguish between married and unmarried individuals and between gender, respectively. Given that spousal care drives the effects among the 60–69 sample and care from adult children drives the effects among the 70 and over sample, we expect to find that the effects are concentrated among married individuals for the younger sample and non-married (mostly widowed) individuals for the older sample. We find that this is largely the case, though the effects are not significantly different from one another: among married individuals aged 60–69, a one percentage point increase in the unemployment rate decreases informal care receipt by 0.8 percentage points (and an insignificant 0.4 percentage points for non-married individuals).24 For the 70 and over sample, informal care marginally increases by 0.7 percentage points for unmarried individuals (and by an insignificant 0.4 percentage points for married individuals). There are not significant differences in care receipt by gender: both men and women age 60–69 experience similar decreases in informal care during economic downturns (0.87 and 0.62 percentage points, respectively), while those age 70 and older experience increases (0.32 and 0.59 percentage points, respectively).
5.2. Employment and Retirement Effects
To gain a better understanding of the contrasting results between the younger and older sample of care recipients, and to further explore the opportunity cost and resource channels, we analyze the effect of macroeconomic conditions on employment and self-reported retirement of the spouses and adult children of the individuals in our HRS sample. Table 5 shows the effects on the share of adult children employed (first panel), the share of adult children who are employed part-time (second panel), whether the spouse is employed (third panel), whether the spouse is retired (fourth panel), and whether the respondent is employed (fifth panel), for the 60–69 year old HRS sample (first three columns) and the 70 and over sample (final three columns). Each age group is also broken down into subsamples that have ADL limitations and IADL limitations to better capture the respondents most in need of care. As one would expect, adult children are 0.6 to 1.1 percentage points less likely to be employed when the unemployment rate increases by one percentage point. This is equally true for the subsamples with limitations, particularly for the 70 and over sample. The second panel shows some evidence that some of these adult children substitute towards part-time work. This suggests that adult children have extra time to provide informal care during economic downturns because they are less likely to be working, and is consistent with a story in which aggregate labor market effects impact potential caregivers by changing the opportunity cost of time.
Table 5:
Effects of macroeconomic conditions on employment outcomes
| Age 60–69 |
Age 70+ |
|||||
|---|---|---|---|---|---|---|
| Sample: | Overall (1) |
ADL lim. (2) |
IADL lim. (3) |
Overall (4) |
ADL lim. (5) |
IADL lim. (6) |
| Outcome: share of kids employed | ||||||
| Unemployment rate | −0.0059** | −0.0028 | −0.0162 | −0.0104*** | −0.0130*** | −0.0106* |
| (0.0023) | (0.0076) | (0.0106) | (0.0024) | (0.0048) | (0.0059) | |
| Observations | 48983 | 6386 | 2790 | 57768 | 14323 | 9679 |
| Mean dependent variable | 0.790 | 0.722 | 0.703 | 0.743 | 0.656 | 0.636 |
| Outcome: share of kids employed part-time | ||||||
| Unemployment rate | 0.0021 | −0.0020 | 0.0115 | 0.0036** | 0.0025 | 0.0005 |
| (0.0024) | (0.0048) | (0.0078) | (0.0017) | (0.0046) | (0.0045) | |
| Observations | 46904 | 5981 | 2570 | 53273 | 12468 | 8270 |
| Mean dependent variable | 0.1045 | 0.1091 | 0.1191 | 0.1027 | 0.1200 | 0.1341 |
| Outcome: spouse employed | ||||||
| Unemployment rate | 0.0011 | 0.0234** | 0.0224 | −0.0001 | −0.0052 | −0.0003 |
| (0.0057) | (0.0089) | (0.0271) | (0.0032) | (0.0051) | (0.0112) | |
| Observations | 36712 | 4011 | 1754 | 32918 | 6134 | 3991 |
| Mean dependent variable | 0.430 | 0.363 | 0.345 | 0.162 | 0.124 | 0.109 |
| Outcome: spouse retired | ||||||
| Unemployment rate | −0.0027 | −0.0026 | −0.0183 | 0.0010 | 0.0118 | 0.0191* |
| (0.0045) | (0.0170) | (0.0276) | (0.0042) | (0.0091) | (0.0109) | |
| Observations | 36747 | 4017 | 1758 | 32944 | 6136 | 3993 |
| Mean dependent variable | 0.553 | 0.568 | 0.544 | 0.790 | 0.789 | 0.782 |
| Outcome: respondent employed | ||||||
| Unemployment rate | 0.0043 | −0.0057 | −0.0033 | −0.0049** | −0.0079*** | −0.0010 |
| (0.0038) | (0.0087) | (0.0105) | (0.0023) | (0.0027) | (0.0030) | |
| Observations | 52458 | 6903 | 3041 | 62780 | 15920 | 10733 |
| Mean dependent variable | 0.4128 | 0.1669 | 0.1506 | 0.1203 | 0.0369 | 0.0257 |
Notes: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on potential caregiver labor supply. The HRS sample is given in the column header. The dependent variables in the first two panels are the share of respondent’s children who are employed and employed part time, respectively. The dependent variables in the second two panels are an indicator for whether the respondent’s spouse works for pay and whether the spouse self-identifies as retired, respectively. The dependent variable in the final panel is an indicator for whether the respondent works for pay. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, the distribution of children ages, as well as state, year, and linear time trends by state.
p < 0.10,
p < 0.05,
p < 0.01.
The effects on spousal employment reveal a different story. Unlike the employment outcomes of adult children, spousal employment does not decrease during downturns. On the contrary, among the 60–69 samples with limitations, spousal employment actually increases by over two percentage points with a one percentage point increase in the unemployment rate. This does not appear in the older sample. The retirement results, while noisy, suggest that spouses are more likely to retire during downturns for the older sample, but not the younger sample. Overall, these differing spousal results for the 60–69 sample and 70 and over sample provide evidence of a channel through which the contrasting informal care results operate: the spouses of our 60–69 sample are less available for informal care because they are more likely to be working during downturns. Appendix Table 12 shows suggestive evidence that this may be the result of economic downturns leading to slightly larger decreases in wealth for this sample relative to the older sample.
Finally, in the last panel we examine a possible alternative channel behind the procyclical care receipt effects whereby the employment status of near-retirees directly affects their demand for informal care. For example, if a near-retiree is less likely to retire in response to declining economic conditions (perhaps due to an income effect), they may be less likely to demand (and subsequently receive) spousal help because they are more active and less likely to be home. The last panel shows no significant effect of the unemployment rate on respondent employment in the 60–69 sample. Further evidence against this channel is the robustness of our informal care results to: the inclusion of respondent employment status as controls (not shown), as well as to limiting the analysis to the HRS subsample that has multiple ADL limitations (Appendix Table 11), i.e., a serious degree of limitation that is unlikely to be affected by this channel. These results suggest that this “own employment” channel is unlikely to be a prominent mechanism for our procyclical effects among the 60–69 sample.
In sum, the employment analysis and informal care heterogeneity analysis show that the effects of macroeconomic conditions on informal care are concentrated among caregivers and care recipients with lower levels of education, and suggests that the resulting fluctuations in informal care operate through multiple channels.25 More generally, these results imply that these families do not fully smooth consumption of informal long-term care across business cycle shocks. In the next section, we explore whether these effects are mirrored in the formal care market for long-term care and whether they are also associated with health outcomes.
6. Effect of Macroeconomic Conditions on Formal Care and Health
The previous section showed that informal care provided by children increases during economic downturns, while informal care provided by spouses decreases. Another important source of long-term care is formally-provided care, either in one’s home or in a facility such as a nursing home or assisted living community. In some contexts, research has shown that formal care and informal care behave as substitutes (Charles and Sevak, 2005; Van Houtven and Norton, 2004, 2008; Mommaerts, 2018), while other work has shown that formal long-term care services do not respond to relative prices of care (Grabowski and Gruber, 2007). Thus, a natural question to ask in response to the finding that informal care use is sensitive to economic conditions is whether this is mirrored by a change in formal care.
To examine the effect of macroeconomic conditions on formal care, we use the HRS sample and focus on four outcomes: (1) whether the individual received any formal care in the previous month (defined as receiving any paid care or currently residing in a nursing home), (2) whether the individual currently resides in a nursing home, (3) whether the individual receives paid care in their home, and (4) whether the individual resides in a retirement community or assisted living facility and uses included services such as help with meals, transportation, ADLs, nursing care, or regular checks by staff or an emergency call button.26 The first four columns in Table 6 report the effects of the unemployment rate on formal care use by age group and finds largely null effects. The one exception is a small and marginally signficant increase in the use of assisted living facility services for the 60–69 sample. Overall, however, these results suggest that the cyclicality of informal care that we quantify is largely not driven by nor drives changes in the use of formal care.
Table 6:
Effect of macroeconomic conditions on the receipt of formal and informal care
| Formal care |
Any type (formal or informal) of
care |
||||||
|---|---|---|---|---|---|---|---|
| Any formal care | Nursing home resident | In home formal care | Assisted liv. resident | Any care | Any ADL care | Any IADL care | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Sample: age 60–69 | |||||||
| Unemployment rate | 0.0020 | 0.0004 | 0.0004 | 0.0015* | −0.0069** | −0.0030 | −0.0054** |
| (0.0013) | (0.0004) | (0.0008) | (0.0008) | (0.0027) | (0.0019) | (0.0027) | |
| Observations | 52530 | 52556 | 52530 | 52556 | 52532 | 52531 | 52506 |
| Mean dependent variable | 0.0241 | 0.0049 | 0.0101 | 0.0099 | 0.0982 | 0.0559 | 0.0800 |
| Sample: age 70 and over | |||||||
| Unemployment rate | −0.0002 | −0.0000 | 0.0003 | −0.0006 | 0.0044* | 0.0030* | 0.0051** |
| (0.0023) | (0.0014) | (0.0012) | (0.0016) | (0.0025) | (0.0018) | (0.0025) | |
| Observations | 62850 | 62885 | 62850 | 62885 | 62851 | 62848 | 62834 |
| Mean dependent variable | 0.1286 | 0.0518 | 0.0443 | 0.0396 | 0.2468 | 0.1567 | 0.2211 |
Notes: Data from the HRS samples of individuals 60–69 (first panel) and individuals 70 and over (second panel). Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01.
These findings, coupled with the cyclicality of informal care, implies that overall long-term care is also cyclical. Columns (4)–(6) report estimates of the effect of the unemployment rate on the likelihood that the elderly individual reports receiving any help, irrespective of the source. Consistent with the combined informal and formal care results, a one percentage point increase in the unemployment rate corresponds to a 0.7 percentage point decrease in the likelihood of receiving any care for the younger sample and a 0.4 percentage point increase in likelihood for the older sample. Despite the increase in the use of assisted living services and with the caveat that this only measures the extensive margin of care, these overall findings suggest that macroeconomic conditions affect overall levels of care rather than substitution between care sources.27
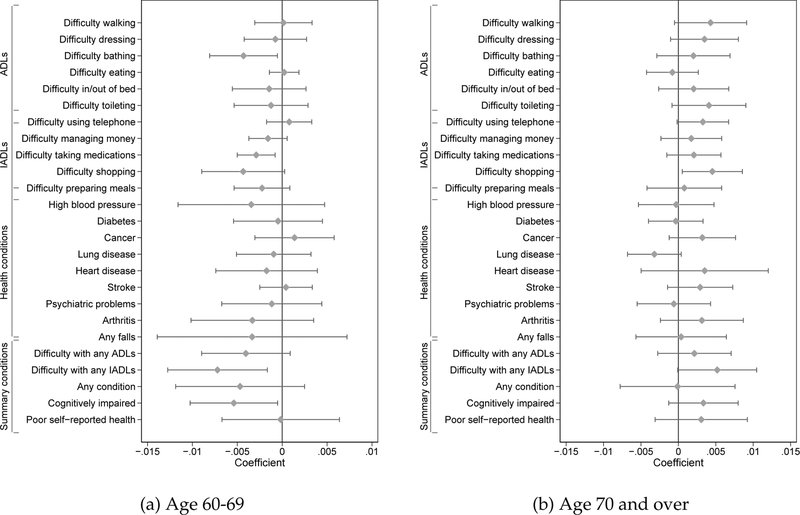
We next investigate whether macroeconomic conditions have a measurable effect on health outcomes that may be related to long-term care. Using the same samples in the HRS, we examine outcomes including difficulty with ADLs, difficulty with IADLs, a range of health conditions, falls, and summary measures including self-reported health. Figure 2 reports the effects of macroeconomic conditions on these outcomes for the 60–69 sample in Panel (a) and the 70+ sample in Panel (b), in which the x-axis is the magnitude of the coefficient, the dot is the point estimate, and the bars are the 95% confidence intervals. In general, most of the coefficients are small and insignificant, particularly for health conditions. The strongest effects, if any, stem from difficulty with IADLs, for which a downturn decreases the likelihood of reporting a difficulty for the 60–69 sample but increases the likelihood of reporting a difficulty for the 70 and over sample. As alluded to in Section 4.2, these effects could be evidence of a true relationship between business cycles and IADL limitations, or it could be that respondents are more likely to report difficulty with an activity if they are receiving help for it (and vice versa). If it is a true health effect, then this could be a second explanation for the procyclicality of informal care in this age group (in addition to spouses working more during downturns). However, the procyclical effect still appears even among the subsample of individuals that report ADL limitations (see Appendix Table 11) thus this health effect cannot be the full explanation. To provide more evidence on whether this is a true health effect, we additionally use health outcome data from the 2006–2015 American Community Survey and, following the same sample and estimation strategy, find negligible to null (0.1 percentage point or less) effects of business cycles on cognitive ability, ambulatory difficulty, difficulty living independently, difficulty with self-care, and vision or hearing difficulty for both age group (results reported in Appendix Table 15).28
Figure 2:
Effect of macroeconomic conditions on health outcomes
Notes: Data from the HRS samples of individuals 60–69 (Panel a) and individuals 70 and over (Panel b). Each point reports the coefficient on the state annual unemployment rate from a separate linear probability model in which the x-axis is the size of the coefficient and the y-axis is the outcome variable. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. 95% confidence intervals, clustered by state, are depicted by the line crossing through the respective point. See Appendix Table 13 for means of each variable in each sample.
While these null results apspear at odds with the literature that finds an effect of macroeconomic conditions on mortality (Ruhm, 2012, 2015), there are several potential explanations for this. First, recent work has found that the mortality effects have become muted in the more recent years that our data spans (McInerney and Mellor, 2012). Second, if elderly mortality is indeed driven by the quality of care in formal care settings, we might expect this to operate less through a gradual deterioration of health as proxied by changes in IADL limitations or increased diagnoses, and more through discrete health shocks and sudden death. These mainly null health results suggest, at least in the short term, that changes in informal care in response to economic fluctuations operate through non-health channels rather than through a response to the changing health of the elderly.29
More broadly, while we cannot show a direct link between our findings and the cyclicality of mortality literature, our finding that informal care responds to macroeconomic conditions is a new and complementary contribution to this literature. This finding, however, does not always align directly with the mortality results. For example, Stevens, Miller, Page et al. (2015) finds that most of the procyclical mortality effects are concentrated among nursing home residents, while our main focus is on community residents (though we see similar qualitative effects on informal care among nursing home residents; see Appendix Table 2). There are several interpretations of this collection of findings. One interpretation is simply that—although it also fluctuates with business cycles—informal care is not a channel through which the mortality effects operate. Another interpretation is that it is difficult to directly compare these results because (a) Stevens, Miller, Page et al. (2015) examine place of death, which is not necessarily indicative of care arrangements prior to death and (b) the timespans of the respective studies are slightly different (1979–2006 for Stevens, Miller, Page et al. (2015) and 1995–2012 for our HRS results) and thus may contribute to the differences. A third interpretation is that informal care may play a role in the mortality effects, but that the mortality effects due to informal care take longer to manifest (as in Coile, Levine, and McKnight (2014)). We leave the distinction between these interpretations to future research.
7. Discussion and Conclusions
The elderly consume healthcare from a variety of sources: acute medical services, formal long-term care services, and informal care from family members. While a growing literature aims to understand the role of economic conditions on health through the lens of the first two “formal” types of inputs, we show in this paper that it is also important to consider the role of informal care, which also fluctuates with changing macroeconomic conditions.
Our main finding is that informal caregiving is countercyclical. That these changes in informal care are not mirrored by shifts in the demand for nursing home or in-home care suggests that shifts in the quality or cost of formal care services are not the first-order reason for the informal care fluctuations. Instead, the concentration of our results among low-educated male caregivers on weekdays suggests that our results are a response to changes in opportunity costs for caregivers. However, we also find suggestive evidence that countercyclical female caregiving behavior is driven by alternative channels, as women do not appear to be responding to their gender-specific unemployment rate. We find that this countercyclical caregiving result is mirrored in the likelihood of receiving informal care for our relatively older sample of elderly, while for the relatively younger sample it is procyclical. These opposite-signed findings appear to be driven by our additional findings that the countercyclicality of informal care in our relatively older sample stems from care from adult children - whose labor market outcomes are more sensitive to business cycles – while the procyclicality of care in the younger sample stems from care from spouses - for whom resource considerations might be a more binding constraint given that they appear to work more during downturns.
These findings are not without limitations. First, the use of state-level annual unemployment rates as our measure of macroeconomic conditions may be geographically broader than the relevant macroeconomy and therefore introduce noise into our estimates. If this noise is assumed to be classical measurement error, our findings are attenuated estimates of the true effects. Second, our two main data sets (the HRS and the ATUS) may be capturing different margins of care. However, to our knowledge these are the best datasets to measure informal care over a meaningful timespan, and the extent to which our results overlap between datasets provides some confidence that they are picking up similar measures of care. Finally, an understudied yet potentially important source of informal “care” is regular visits to individuals in institutionalized care settings to ensure that they receive the proper medical and physical care. Our measure of informal care does not include this type of informal care, but it may be important to a patient’s well-being and is an interesting topic for future research.
More generally, our findings point to the complex ways in which families adjust long-term care arrangements to macroeconomic conditions. Formal care options do not substitute for informal care at this margin, suggesting the potential for unmet need, especially among low-income families. If this unmet need has negative consequences for well-being, as some research suggests, then our current reliance on a patchwork of informal and increasingly expensive formal care options will leave some groups underserved. A fruitful next step in this line of research is to further understand the welfare impacts of our findings for both the elderly and their caretakers. For example, informal care can be a productive use of time during economic downturns, but may have long-lasting deleterious effects if caregivers remain out of work long after the downturn. Future research to assess the magnitudes of these welfare consequences will be important factors for understanding and evaluating long-term care policy.
We thank Elizabeth Ananat, Long Hong, Lauren Jones, Nicole Maestas, Jen Mellor, Ross Milton, Edward Norton, Stephanie Rennane, Seth Sanders, Jeffrey Smith, Courtney Van Houtven, Alice Zulkarnain, and seminar participants at Boston College Center for Retirement Research, RAND, the 2018 AEA meetings, Census Bureau, Wayne State University, 2018 MHEC, 2018 SOLE, 2018 ASHEcon, and 2018 SEA for comments. Funding from the National Institute on Aging, through Grant Number T32-AG000186 to the National Bureau of Economic Research, is gratefully acknowledged.
Appendix A: Informal and Formal Care Measures
American Time Use Survey
We use the 2003 through 2015 American Time Use Survey (ATUS) to measure informal caregiving. The survey collects information about a particular day in the previous week, and asks respondents to report the activities they did during that day in 15 minute increments. Our key variables are what we call “ADL care”, “IADL care”, and “Any care” which is either ADL or IADL care. We define ADL care from the ATUS question about “Caring For & Helping Household Members” and “Caring For & Helping Non-Household Members”. Within the former, we exclude time spent caring and helping children, and focus on the following four broad categories from which the respondent could report spending a 15 minute increment doing:
- Caring For Household Adults
- Physical care for household adults
- Looking after a household adult (as a primary activity)
- Providing medical care to a household adult
- Obtaining medical and care services for a household adult
- Waiting associated with caring for household adults
- Caring for household adults, not elsewhere classified
- Helping Household Adults
- Helping household adults
- Organization and planing for household adults
- Picking up/dropping off household adult
- Waiting associated with helping household adults
- Helping household adults, not elsewhere classified
- Caring for Non-Household Adults
- Physical care for non-household adults
- Looking after non-household adults (as a primary activity)
- Providing medical care to a non-household adult
- Obtaining medical and care services for a non-household adult
- Waiting associated with caring for non-household adults
- Caring for non-household adults, not elsewhere classified
- Helping Non-Household Adults
- Housework, cooking, and shopping assistance for non-household adults
- House and lawn maintenance and repair assistance for non-household adults
- Animal and pet care assistance for non-household adults
- Vehicle and appliance maintenance/repair assistance for non-household adults
- Financial management assistance for non-household adults
- Household management and paperwork assistance for non-household adults
- Picking up/dropping off non-household adults
- Waiting associated with helping non-household adults
- Helping non-household adults, not elsewhere classified
Our measure of ADL care is constructed from the first and third broad categories, and our measure of IADL care is constructed from the second and fourth broad categories.
Health and Retirement Study
We use the 1995 through 2012 Health and Retirement Study (HRS) to measure informal care receipt and formal care receipt. While the HRS asks questions about caregiving as well, it is only for individuals aged 50 and over and the interval of time over which they reported caregiving activities is two years. Our key informal care variables, like the ATUS measures of informal caregiving, are “ADL care”, “IADL care”, and “Any care” which is either ADL or IADL care. For these categories, respondents were first asked if they had any difficulty with the following activities:
ADLs: walking across a room, dressing (including putting on socks and shoes), bathing or showering, eating (such as cutting up your food), getting in and out of bed, using the toilet (including getting up and down).
IADLs: making phone calls, managing money, taking medications, shopping for groceries, preparing a hot meal.
For each of these, respondents are asked whether they have difficulty with any of these activities (yes, no, “can’t do”, or “don’t do”), excluding any difficulties they expect to last less than three months.
Respondents are also asked if they receive help (if they report difficulty) and whether they use equipment for walking across a room and getting in and out of bed. For the help variables, they are first asked about “who most often helps” with each activity and then also asked about any other helpers. We categorize the relationships from the broader set of relationships as follows:
Spouse: spouse/partner, former spouse
Child: son, stepson, spouse/partner of a daughter, daughter, stepdaughter, spouse/partner of son, unlisted child or child-in-law, former step-child, former child-in-law
Other family: grandchild, father, father of spouse/partner, mother, mother of spouse/partner, respondent’s parents, brother, brother of spouse/partner, sister, sister of spouse/partner, other relative, spouse/partner of grandchild
Other, not paid: other individual (if not paid)
Formal help: organization, employee of institution, paid helper, professional, professional (specify), other individual (paid)
For each helper, respondents were then asked on how many days they received help from each helper during the last month, days per week, and hours per day. They were also asked if they were paid, and if so how much. We use these helper relationships to construct measures of spousal care, care from adult children, and paid in-home care over the last month. However, if they moved to a nursing home within the last month, they are coded as not receiving this other help (results do not change substantially if we do not make this restriction). The nursing home variable captures respondents who are in a nursing home or other health facility that provides all of the following services for its residents: dispensing of medication, 24-hour nursing assistance and supervision, personal assistance, and room and meals.
Appendix B: Appendix Figures and Tables
Appendix Figure 1:
Density of state time trend coefficients, ATUS sample
Note: Figure plots the distribution of coefficients of state-specific linear time trends from a regression model of binary provision of informal care on state fixed effects and state-specific linear time trends. Sample is individuals aged 40 and over in the ATUS.
Appendix Figure 2:
Effect of macroeconomic conditions on informal care receipt, by age
Note: Figure plots the coefficients and their 95% confidence intervals by age from a regression of any informal caregiving in the sample of individuals aged 40 and over in the ATUS. The specification is estimated using a linear probability model and controls for a quadratic in age, gender education, marital status, race and ethnicity, family size, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state, and is weighted using individual-level weights. Standard errors are clustered by state. * p < 0.10, ** p < 0.05, *** p < 0.01.
Appendix Table 1:
Effects of macroeconomic conditions on informal caregiving to parents in HRS
| Everyone |
Living parents |
|||||
|---|---|---|---|---|---|---|
| Any care (1) |
ADL care (2) |
IADL care (3) |
Any care (4) |
ADL care (5) |
IADL care (6) |
|
| Contemporaneous unemployment rate | −0.0010 | −0.0007 | −0.0004 | −0.0022 | −0.0008 | −0.0016 |
| (0.0015) | (0.0009) | (0.0011) | (0.0048) | (0.0033) | (0.0027) | |
| Observations | 155655 | 155750 | 155687 | 43117 | 43180 | 43139 |
| Mean dependent variable | 0.127 | 0.036 | 0.091 | 0.331 | 0.095 | 0.236 |
| Average unemployment rate | −0.0011 | −0.0007 | −0.0005 | −0.0006 | 0.0003 | −0.0011 |
| (0.0015) | (0.0009) | (0.0011) | (0.0044) | (0.0032) | (0.0026) | |
| Observations | 155655 | 155750 | 155687 | 43117 | 43180 | 43139 |
| Mean dependent variable | 0.127 | 0.036 | 0.091 | 0.331 | 0.095 | 0.236 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on informal caregiving using data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Informal caregiving is measured over the previous two years. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 2:
Effects of macroeconomic conditions on informal care receipt, alternative definitions of informal care
| Baseline definition | No restrictions | Not nursing home residents | Nursing home residents | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Sample: age 60–69 | ||||
| Unemployment rate | −0.0076*** | −0.0074*** | −0.0076*** | −.0323 |
| (0.0026) | (0.0027) | (0.0026) | (0.0695) | |
| Observations | 52530 | 52530 | 52272 | 258 |
| Mean dependent variable | 0.089 | 0.091 | 0.0889 | 0.527 |
| Sample: age 70 and over | ||||
| Unemployment rate | 0.0046** | 0.0047** | 0.0049** | 0.0075 |
| (0.0021) | (0.0023) | (0.0023) | (0.0128) | |
| Observations | 62850 | 62850 | 59590 | 3260 |
| Mean dependent variable | 0.182 | 0.217 | 0.191 | 0.682 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on informal caregiving using data from the HRS sample. The first column sets informal care to zero for nursing home residents; the second and fourth column relax that restriction. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 3:
Effects of macroeconomic conditions on informal care receipt, weighted
| Type of care |
Source of care |
||||
|---|---|---|---|---|---|
| Any care (1) |
ADLs (2) |
IADLs (3) |
Children (4) |
Spouse (5) |
|
| Outcome: care receipt among 60–69 | |||||
| Unemployment rate | −0.0071* | −0.0021 | −0.0053* | −0.0023 | −0.0051* |
| (0.0037) | (0.0022) | (0.0030) | (0.0021) | (0.0025) | |
| Observations | 51779 | 51779 | 51779 | 51689 | 51779 |
| Mean dependent variable | 0.081 | 0.040 | 0.058 | 0.032 | 0.051 |
| Outcome: care receipt among 70+ | |||||
| Unemployment rate | 0.0049* | 0.0021 | 0.0051* | 0.0041* | 0.0015 |
| (0.0025) | (0.0013) | (0.0027) | (0.0024) | (0.0019) | |
| Observations | 62223 | 62223 | 62223 | 62149 | 62223 |
| Mean dependent variable | 0.177 | 0.074 | 0.139 | 0.101 | 0.073 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model using data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state and are weighted using individual-level weights (nursing home weights only available for 2000 onwards). Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 4:
Effects of macroeconomic conditions on proximity to adult children in HRS
| Near or coresident | Near | Coresident | |
|---|---|---|---|
| (1) | (2) | (3) | |
| Sample: age 60–69 | |||
| Unemployment rate | −0.0017 | 0.0027 | −0.0049 |
| (0.0052) | (0.0054) | (0.0037) | |
| Observations | 49911 | 49911 | 52435 |
| Mean dependent variable | 0.630 | 0.550 | 0.218 |
| Sample: age 70 and over | |||
| Unemployment rate | −0.0014 | −0.0027 | 0.0046* |
| (0.0033) | (0.0035) | (0.0028) | |
| Observations | 60392 | 60392 | 62768 |
| Mean dependent variable | 0.620 | 0.556 | 0.167 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on proximity to adult children in the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. “Near” is measured as living within ten miles. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 5:
Effects of macroeconomic conditions on attrition in the HRS
| Any Attrition | Living, non response | Died | Proxy interview | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Sample: age 60–69 | ||||
| Unemployment rate | −0.0018 | −0.0011 | −0.0007 | 0.0008 |
| (0.0016) | (0.0011) | (0.0009) | (0.0021) | |
| Observations | 55328 | 55328 | 55328 | 53280 |
| Mean dependent variable | 0.037 | 0.013 | 0.024 | 0.066 |
| Sample: age 70 and over | ||||
| Unemployment rate | 0.0004 | −0.0001 | 0.0005 | 0.0005 |
| (0.0028) | (0.0013) | (0.0030) | (0.0026) | |
| Observations | 72799 | 72799 | 72799 | 63864 |
| Mean dependent variable | 0.123 | 0.017 | 0.109 | 0.118 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on a measure of attrition using data from the HRS sample, including any attrition (column 1), attrition but still alive (column 2), and death (column 3). All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 6:
Effects of employment-to-population ratio on informal caregiving and care receipt
| Type of care |
Source of care |
||||
|---|---|---|---|---|---|
| Any care (1) |
ADLs (2) |
IADLs (3) |
Children (4) |
Spouse (5) |
|
| Outcome: caregiving among 40+ | |||||
| Employment-to-population ratio | −0.0055** | −0.0015 | −0.0051 | N/A | N/A |
| (0.0023) | (0.0012) | (0.0021) | |||
| Observations | 105741 | 105741 | 105741 | ||
| Mean dependent variable | 0.134 | 0.039 | 0.106 | ||
| Outcome: care receipt among 60–69 | |||||
| Employment-to-population ratio | 0.0031 | 0.0032 | 0.0023 | 0.0025 | 0.0025 |
| (0.0021) | (0.0014) | (0.0018) | (0.0013) | (0.0018) | |
| Observations | 52530 | 52530 | 52530 | 52435 | 52530 |
| Mean dependent variable | 0.089 | 0.043 | 0.064 | 0.039 | 0.054 |
| Outcome: care receipt among 70+ | |||||
| Employment-to-population ratio | −0.0014 | −0.0008 | −0.0038 | −0.0044 | −0.0014 |
| (0.0030) | (0.0015) | (0.0027) | (0.0016) | (0.0025) | |
| Observations | 62850 | 62850 | 62850 | 62778 | 62850 |
| Mean dependent variable | 0.182 | 0.079 | 0.142 | 0.103 | 0.077 |
Note: Each cell reports the coefficient on the state annual employment-to-population ratio from a separate linear probability model. The first panel uses data from the ATUS sample, while the second and third panels use data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. HRS regressions additionally control for number of children a respondent has. The ATUS regressions additionally control for family size and are weighted using individual-level weights. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 7:
Effects of macroeconomic conditions on informal caregiving (ATUS), intensive margin
| Type of care |
|||
|---|---|---|---|
| Any care (1) |
ADLs (2) |
IADLs (3) |
|
| Outcome: Unconditional minutes per day | |||
| Unemployment rate | 0.636** | 0.206 | 0.423** |
| (0.302) | (0.185) | (0.194) | |
| Observations | 105741 | 105741 | 105741 |
| Mean dependent variable | 7.857 | 3.141 | 4.742 |
| Outcome: conditional minutes per day | |||
| Unemployment rate | 1.246 | 0.248 | 1.027 |
| (2.046) | (3.156) | (1.831) | |
| Observations | 13509 | 3363 | 11082 |
| Mean dependent variable | 58.70 | 81.47 | 44.81 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model using data from the ATUS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state and are weighted using individual-level weights. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 8:
Effects of macroeconomic conditions on formal and informal care receipt (HRS), intensive margin
| Unconditional
hours/day |
Conditional
hours/day |
|||||
|---|---|---|---|---|---|---|
| Any (1) |
Informal (2) |
Formal (3) |
Any (4) |
Informal (5) |
Formal (6) |
|
| Sample: age 60–69 | ||||||
| Unemployment rate | −0.0270 | −0.0323 | 0.0070 | 0.0571 | 0.0753 | 0.3994 |
| (0.0300) | (0.0300) | (0.0087) | (0.3125) | (0.3381) | (0.8561) | |
| Observations | 40907 | 40907 | 40907 | 3577 | 3378 | 388 |
| Mean dependent variable | 0.54 | 0.446 | 0.043 | 5.767 | 5.402 | 4.580 |
| Sample: age 70+ | ||||||
| Unemployment rate | 0.0585* | 0.0401 | 0.0081 | 0.1105 | 0.0350 | 0.4254 |
| (0.0315) | (0.0312) | (0.0157) | (0.1393) | (0.1672) | (0.3634) | |
| Observations | 52073 | 52073 | 52073 | 9860 | 9047 | 1988 |
| Mean dependent variable | 0.54 | 0.446 | 0.043 | 5.767 | 5.402 | 4.580 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model of hours of care receipt per day using data from the HRS sample, restricted to 2000 onward. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 9:
Effects of macroeconomic conditions on informal care receipt, including lag
| Type of care |
Source of care |
||||
|---|---|---|---|---|---|
| Any care (1) |
ADLs (2) |
IADLs (3) |
Children (4) |
Spouse (5) |
|
| Outcome: caregiving among 40+ | |||||
| Unemployment rate | 0.0078** | 0.0054** | 0.0042 | ||
| (0.0034) | (0.0022) | (0.0028) | |||
| Lagged unemployment rate | 0.0003 | −0.0040** | 0.0032 | N/A | N/A |
| (0.0034) | (0.0019) | (0.0030) | |||
| Observations | 105741 | 105741 | 105741 | ||
| Mean dependent variable | 0.134 | 0.039 | 0.106 | ||
| Outcome: care receipt among 60–69 | |||||
| Unemployment rate | −0.0093*** | −0.0036 | −0.0084*** | −0.0045 | −0.0065*** |
| (0.0032) | (0.0022) | (0.0028) | (0.0028) | (0.0019) | |
| Lagged unemployment rate | 0.0022 | 0.0004 | 0.0030 | 0.0020 | 0.0006 |
| (0.0020) | (0.0019) | (0.0018) | (0.0017) | (0.0017) | |
| Observations | 52530 | 52530 | 52530 | 52435 | 52530 |
| Mean dependent variable | 0.089 | 0.043 | 0.064 | 0.039 | 0.054 |
| Outcome: care receipt among 70+ | |||||
| Unemployment rate | −0.0010 | −0.0022 | 0.0020 | 0.0009 | −0.0018 |
| (0.0034) | (0.0019) | (0.0035) | (0.0031) | (0.0023) | |
| Lagged unemployment rate | 0.0074* | 0.0055** | 0.0046 | 0.0051* | 0.0030 |
| (0.0041) | (0.0022) | (0.0039) | (0.0028) | (0.0029) | |
| Observations | 62850 | 62850 | 62850 | 62778 | 62850 |
| Mean dependent variable | 0.182 | 0.079 | 0.142 | 0.103 | 0.077 |
Note: Each column-panel reports the coefficient on the contemporaneous and lagged state annual unemployment rate from a separate linear probability model. The first panel uses data from the ATUS sample, while the second and third panels use data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. HRS regressions additionally control for number of children a respondent has. The ATUS regressions additionally control for family size and are weighted using individual-level weights. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 10:
Effects of macroeconomic conditions on informal care, logit and probit
| Logit |
Probit |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of care |
Source of care |
Type of care |
Source of care |
|||||||
| Any care (1) |
ADLs (2) |
IADLs (3) |
Children (4) |
Spouse (5) |
Any care (6) |
ADLs (7) |
IADLs (8) |
Children (9) |
Spouse (10) |
|
| Outcome: caregiving among 40+ | ||||||||||
| Unemployment rate | 0.0672*** | 0.0809* | 0.0626*** | N/A | N/A | 0.0361*** | 0.0357** | 0.0326*** | N/A | N/A |
| (0.0191) | (0.0406) | (0.0181) | (0.0103) | 0.0182) | (0.0094) | |||||
| Observations | 105741 | 105741 | 105741 | 105741 | 105741 | 105741 | ||||
| Mean dependent variable | 0.134 | 0.039 | 0.106 | 0.134 | 0.039 | 0.106 | ||||
| Outcome: care receipt among 60–69 | ||||||||||
| Unemployment rate | −0.1093*** | −0.0957** | −0.1097** | −0.0851 | −0.1317*** | −0.0541*** | −0.0458** | −0.0498** | −0.0386 | −0.0633*** |
| (0.0375) | (0.0441) | (0.0481) | (0.0765) | (0.0368) | (0.0192) | (0.0203) | (0.0235) | (0.0354) | (0.0178) | |
| Observations | 51748 | 51748 | 51748 | 48458 | 51647 | 51748 | 51748 | 51748 | 48458 | 51647 |
| Mean dependent variable | 0.088 | 0.043 | 0.064 | 0.041 | 0.054 | 0.088 | 0.043 | 0.064 | 0.0412 | 0.054 |
| Outcome: care receipt among 70+ | ||||||||||
| Unemployment rate | 0.0316* | 0.0294* | 0.0471** | 0.0535** | 0.0129 | 0.0175* | 0.0143 | 0.0259** | 0.0300** | 0.0069 |
| (0.0161) | (0.0173) | (0.0204) | (0.0236) | (0.0333) | (0.0090) | (0.0087) | (0.0110) | (0.0124) | (0.0181) | |
| Observations | 62206 | 62206 | 62206 | 57473 | 62182 | 62206 | 62206 | 62206 | 57473 | 62182 |
| Mean dependent variable | 0.181 | 0.078 | 0.142 | 0.111 | 0.077 | 0.181 | 0.078 | 0.142 | 0.111 | 0.077 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate model (logit in columns 1–5 and probit in columns 6–10) using data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. State-year combinations in the HRS with fewer than 10 observations are dropped due to lack of convergence. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 11:
Effects of macroeconomic conditions on informal care receipt, by ADL limitations
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Sample: | No ADLs | 1 ADL | 2 ADLs | 1+ ADLs | 2+ ADLs | 3+ ADLs |
| Panel A: 60–69 sample | ||||||
| Unemployment rate | −0.0024* | −0.0359** | −0.0394 | −0.0287** | −0.0251* | −0.0198 |
| (0.0014) | (0.0167) | (0.0254) | (0.0142) | (0.0148) | (0.0201) | |
| Observations | 45600 | 3536 | 1532 | 6908 | 3372 | 1840 |
| Mean dependent variable | 0.027 | 0.334 | 0.589 | 0.494 | 0.661 | 0.721 |
| Panel B: 70+ sample | ||||||
| Unemployment rate | 0.0014 | 0.0064 | 0.0149 | 0.0128** | 0.0111 | 0.0095 |
| (0.0025) | (0.0108) | (0.0150) | (0.0061) | (0.0067) | (0.0121) | |
| Observations | 46888 | 6735 | 3191 | 15938 | 9203 | 6012 |
| Mean dependent variable | 0.075 | 0.409 | 0.578 | 0.497 | 0.561 | 0.551 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model using data from the HRS sample. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 12:
Effects of macroeconomic conditions on household resources
| Sample: | Full sample (1) |
ADL lim. (2) |
IADL lim. (3) |
|---|---|---|---|
| Age group: 60–69 | |||
| Unemployment rate | −13614*** | −882 | −10488 |
| (5541) | (10095) | (13488) | |
| Observations | 52556 | 6910 | 3045 |
| Mean dependent variable | 390793 | 191829 | 171562 |
| Age group: 70+ | |||
| Unemployment rate | −9764** | 81 | −8959 |
| (4007) | (4190) | (6595) | |
| Observations | 62885 | 15939 | 10748 |
| Mean dependent variable | 374518 | 245046 | 219688 |
Note: Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model on total household wealth using data from the HRS sample. Column (1) is the full sample in the age group, column (2) restricts the sample to individuals who report at least one ADL limitation, and column (3) restricts the sample to individuals who report at least one IADL limitation. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 13:
Means of health conditions in HRS sample
| Age 60–69 | Age 70 and over | |
|---|---|---|
| ADLs: Difficulty walking | 0.052 | 0.128 |
| ADLs: Difficulty dressing | 0.082 | 0.160 |
| ADLs: Difficulty bathing | 0.050 | 0.141 |
| ADLs: Difficulty eating | 0.023 | 0.0716 |
| ADLs: Difficulty in/out of bed | 0.058 | 0.098 |
| ADLs: Difficulty toileting | 0.046 | 0.102 |
| IADLs: Difficulty using telephone | 0.026 | 0.104 |
| IADLs: Difficulty managing money | 0.039 | 0.137 |
| IADLs: Difficulty taking medications | 0.024 | 0.076 |
| IADLs: Difficulty shopping | 0.068 | 0.179 |
| IADLs: Difficulty preparing meals | 0.043 | 0.142 |
| Health conditions: High blood pressure | 0.564 | 0.648 |
| Health conditions: Diabetes | 0.213 | 0.219 |
| Health conditions: Cancer | 0.119 | 0.196 |
| Health conditions: Lung disease | 0.108 | 0.124 |
| Health conditions: Heart disease | 0.215 | 0.353 |
| Health conditions: Stroke | 0.062 | 0.137 |
| Health conditions: Psychiatric problems | 0.186 | 0.158 |
| Health conditions: Arthritis | 0.598 | 0.693 |
| Summary conditions: Any falls | 0.263 | 0.358 |
| Summary conditions: Difficulty with any ADLs | 0.144 | 0.271 |
| Summary conditions: Difficulty with any IADLs | 0.108 | 0.246 |
| Summary conditions: Any condition | 0.192 | 0.236 |
| Summary conditions: Cognitively impaired | 0.062 | 0.150 |
| Summary conditions: Poor self-reported health | 0.271 | 0.352 |
Notes: Means of health conditions from the HRS samples of individuals 60–69 (column 1) and individuals 70 and over (column 2) that correspond to the regression estimates in Figure 2.
Appendix Table 14:
Effect of macroeconomic conditions on the receipt of formal and informal care, sample with 2+ ADLs
| Formal care |
Any type (formal or
informal) of care |
||||||
|---|---|---|---|---|---|---|---|
| Any formal care | Nursing home resident | In home formal care | Assisted liv. resident | Any care | Any ADL care | Any IADL care | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Sample: age 60–69 | |||||||
| Unemployment rate | 0.0208* | 0.0023 | 0.0042 | 0.0160*** | −0.0154 | −0.0104 | −0.0100 |
| (0.0120) | (0.0063) | (0.0081) | (0.0050) | (0.0154) | (0.0151) | (0.0170) | |
| Observations | 3372 | 3374 | 3372 | 3374 | 3374 | 3374 | 3374 |
| Mean dependent variable | 0.1892 | 0.0578 | 0.1047 | 0.0350 | 0.7501 | 0.6183 | 0.6020 |
| Sample: age 70 and over | |||||||
| Unemployment rate | −0.0016 | −0.0057 | 0.0022 | 0.0029 | 0.0076 | 0.0053 | 0.0043 |
| (0.0056) | (0.0061) | (0.0062) | (0.0053) | (0.0048) | (0.0063) | (0.0063) | |
| Observations | 9203 | 9204 | 9203 | 9204 | 9204 | 9204 | 9204 |
| Mean dependent variable | 0.4931 | 0.2702 | 0.2021 | 0.0524 | 0.8752 | 0.7847 | 0.7869 |
Notes: Data from the HRS samples of individuals 60–69 (first panel) and individuals 70 and over (second panel) who have difficulty with two or more ADLs. Each cell reports the coefficient on the state annual unemployment rate from a separate linear probability model. All specifications control for a quadratic in age, gender, education, marital status, race and ethnicity, number of children, share of the state population aged 18–64 and aged 65 and over, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Appendix Table 15:
Effect of macroeconomic conditions on health, American Community Survey
| Cognitive difficulty | Ambulatory difficulty | Indep. living difficulty | Self-care difficulty | Vision/hearing difficulty | |
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Panel A: Age 60–69 | |||||
| Unemployment rate | −0.0003 | −0.0009 | 0.0002 | 0.0001 | −0.0008 |
| (0.0003) | (0.0004) | (0.0003) | (0.0002) | (0.0004) | |
| Observations | 3520659 | 3520659 | 3520659 | 3520659 | 3520659 |
| Mean dependent variable | 0.0595 | 0.1534 | 0.0734 | 0.0457 | 0.0903 |
| Panel B: Age 70+ | |||||
| Unemployment rate | −0.0000 | 0.0012 | 0.0008 | 0.0010 | −0.0001 |
| (0.0004) | (0.0004) | (0.0004) | (0.0005) | (0.0005) | |
| Observations | 3522622 | 3522622 | 3522622 | 3522622 | 3522622 |
| Mean dependent variable | 0.1436 | 0.3173 | 0.2351 | 0.1425 | 0.2291 |
Notes: Data from 2006–2015 American Community Survey. Each cell reports results from a separate linear probability model. The independent variable of interest is the state annual unemployment rate and the dependent variables are indicators for whether the respondent has cognitive, ambulatory, independent living, self-care, and vision/hearing difficulty, respectively. All specifications are weighted using person weights and control for a quadratic in age, gender, education, marital status, race and ethnicity, state log expenditures on total Medicaid and Medicaid HCBS services for the older population and population with physical disabilities, as well as state, year, and linear time trends by state. Standard errors, clustered by state, are in parentheses.
p < 0.10,
p < 0.05,
p < 0.01
Footnotes
McInerney and Mellor (2012) find much less pro-cyclicality of elderly mortality; in fact, they argue that for the period 1994–2008 elderly mortality is countercyclical.
These findings are not uncontested: Konetzka, Lasater, Norton et al. (2018) find that the total number of nurses does not change during downturns, but the composition of nurses shifts “from more expensive registered nurses to less expensive licensed practical nurses,” suggesting that nursing home quality actually decreases during downturns.
Although it is not a focus of the paper, using the ATUS Aguiar, Hurst, and Karabarbounis (2013) similarly find that in the US about 5% of forgone work hours were allocated towards care for other adults during the Great Recession.
While our focus is the elderly population, one third of individuals with long-term care needs are below the age of 65 (Rogers and Komisar, 2003).
We use a joint utility function for simplicity, but this can easily be extended to individual utility functions for the individual and potential caregiver.
The quality parameter Q is similar in spirit to Blau and Robins (1988), who include care quality in a model of childcare and family labor labelply. An interesting, but more complicated extension would be to allow the quality of informal care depend not only on the hours of informal care, but also the hours of market work (to capture, for example, caregiver time stressors): g(hc, hm).
Alternatively, the corner solution of occurs when meaning that the marginal benefit of an extra hour of time for leisure or market work is greater than the marginal benefit of an extra hour of informal care.
For example, economic conditions may impact the quality of care through staffing. Cawley, Grabowski, and Hirth (2006) show that when the price of direct care workers increases, nursing homes substitute away from labor inputs and towards materials, increasing the morbidity and mortality risk of residents. Konetzka, Lasater, Norton et al. (2018) show that during economic downturns, nursing homes substitute away from more expensive labor (e.g. registered nurses) to lower cost labor (licensed practical nurses). They also argue that economic downturns affect nursing home revenue through demand for nursing home services, which could be another pathway through which economic conditions affect the quality of formal care services.
The Health and Retirement Study (HRS), which we use for the care receipt analysis, also contains measures of caregiving, but we do not use them for our main estimates because the reference period for caregiving spans the previous two years, whereas the ATUS spans a particular day in the previous week. Nevertheless, we discuss these results in Section 5.
We use both the raw HRS data files and the RAND HRS data files for our analysis.
If an individual reports receiving informal care and also lives in a nursing home, we code them as receiving only nursing home care. If an individual reports receiving informal care and also in-home paid care, we code them as receiving both. We discuss robustness of our results to alternative definitions in Section 5.
Given this question ordering in the survey, one concern is that respondents may be more likely to report difficulty with an activity if they are already receiving help for it. We discuss this possibility in Section 6.
There is some overlap between the informal and formal care recipient samples among individuals who receive both forms of care at home.
We do not include individual health status, because health is a potential outcome that could be affected by both macroeconomic conditions and the resulting informal care. We examine this in Section 6.
Appendix Figure 1 plots the distribution of these trends in the ATUS sample, and shows that slopes range from −0.01 to 0.005.
The HRS does not contain weights for nursing home residents until 2000, so our main specifications do not include weights. Additional results with cross-sectional weights (including nursing home weights when available) are discussed in Section 5.
Appendix Figure 2 shows a similar pattern by single year of age for care recipiency and in analogous figures (not shown) we confirm that this pattern holds for both help with IADLs and help with ADLs.
Appendix Table 1 reports results using caregiving measures from the HRS. These are not our preferred estimates because the measure spans two years and thus provides a very noisy measure of informal caregiving in response to the unemployment rate. Using two separate measures of macroeconomic conditions (the unemployment rate contemporaneous with the survey year and the average unemployment rate over the two years), we find no evidence of an effect of macroeconomic conditions on informal caregiving across the full HRS sample and the sample with living parents. However, we prefer our ATUS estimates due to the significantly narrower look-back window.
We are unable to reproduce this exercise in the caregiver sample, as the ATUS does not identify the recipient of the reported care.
For example, Carmichael, Charles, and Hulme (2010) and He and McHenry (2016) show that individual economic opportunites change the likelihood that somebody provides informal care to a family member.
This is in line with other estimates that suggest that 40% of family caregivers in the United States are men (AARP, 2015), despite the common perception that most informal care is provided by women.
On the other hand, those with very low resources may become eligible for Medicaid during a downturn, which may prompt them to substitute towards Medicaid-paid formal care.
This is in line with research that shows that disability is closely associated with education: conditional on age, individuals with less than a high school education are more than twice as likely to have difficulty with ADLs as high school graduates (Hagen, 2013).
One potential explanation for the countercyclical caregiving effects but procyclical care receipt effects among 60–69 year olds (as shown in Figure 1) is that individuals are too busy taking care of their parents to care for their spouses (we thank an anonymous referee for this point). However, this alternative “sandwich” generation idea does not seem borne out in the data: only 29% of 60–69 year olds that need care have parents or parents-in-law, and only 6.5% of their spouses provide care to those parents.
In results not shown, the majority of these heterogeneous effects load on care for IADLs rather than care for ADLs.
Appendix A describes our measure of formal care as “Formal help: organization, employee of institution, paid helper, professional, professional (specify), other individual (paid)”. It is unclear whether respondents include potential sources of paid help such as grocery delivery services, taxis, or house cleaners in their answers to these questions, although the job description of home aides or personal care aides often includes these services. Furthermore, we cannot be certain that our measure of nursing home care does not also capture post-acute care.
Results for individuals who have two or more ADL limitations (often a qualification for nursing home entry) in Appendix Table 14 are similar for nursing home residence and in-home formal care, but show larger effects on the use of assisted living services for the 60–69 sample.
We restrict the American Community Survey analysis to years 2006 and later because 2006 was the first year that includes the institutionalized population.
If we had estimated a meaningful relationship between economic conditions and health, it would have been difficult to identify whether informal care responds to a contemporaneous change in health or whether health responds to a contemporaneous change in informal care.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Corina Mommaerts, University of Wisconsin - Madison.
Yulya Truskinovsky, Wayne State University.
References
- AARP (2015). ‘Caregiving in the U.S.’ Research report.
- Aguiar M, Hurst E, and Karabarbounis L. (2013). ‘Time use during the great recession.’ American Economic Review, vol. 103(5): 1664–96. [Google Scholar]
- Antwi YA and Bowblis JR (2018). ‘The impact of nurse turnover on quality of care and mortality in nursing homes: Evidence from the great recession.’ American Journal of Health Economics, vol. 4(2): 131–163. [Google Scholar]
- Bitler M. and Hoynes H. (2015). ‘Living Arrangements, Doubling Up, and the Great Recession: Was This Time Different?’ American Economic Review, vol. 105(5): 166–70. [Google Scholar]
- Blau D. and Robins P. (1988). ‘Child-Care Costs and Family Labor Supply.’ The Review of Economics and Statistics, vol. 70(3): 374–81. [Google Scholar]
- Bolin K, Lindgren B, and Lundborg P. (2008). ‘Your next of kin or your own career?: Caring and working among the 50+ of Europe.’ Journal of Health Economics, vol. 27(3): 718–738. [DOI] [PubMed] [Google Scholar]
- Bostick JE, Rantz MJ, Flesner MK, and Riggs CJ (2006). ‘Systematic review of studies of staffing and quality in nursing homes.’ Journal of the American Medical Directors Association, vol. 7(6): 366–376. [DOI] [PubMed] [Google Scholar]
- Carmichael F. and Charles S. (2003). ‘The opportunity costs of informal care: does gender matter?’ Journal of Health Economics, vol. 22(5): 781–803. [DOI] [PubMed] [Google Scholar]
- Carmichael F, Charles S, and Hulme C. (2010). ‘Who will care? Employment participation and willingness to supply informal care.’ Journal of Health Economics, vol. 29(1): 182–190. [DOI] [PubMed] [Google Scholar]
- Cawley J, Grabowski DC, and Hirth RA (2006). ‘Factor substitution in nursing homes.’ Journal of Health Economics, vol. 25(2): 234–247. [DOI] [PubMed] [Google Scholar]
- Chari AV, Engberg J, Ray KN, and Mehrotra A. (2015). ‘The Opportunity Costs of Informal Elder-Care in the United States: New Estimates from the American Time Use Survey.’ Health Services Research, vol. 3(50): 871–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles KK and Sevak P. (2005). ‘Can family caregiving substitute for nursing home care?’ Journal of Health Economics, vol. 24(6): 1174–1190. [DOI] [PubMed] [Google Scholar]
- Chen MM and Grabowski DC (2015). ‘Intended and unintended consequences of minimum staffing standards for nursing homes.’ Health Economics, vol. 24(7): 822–839. [DOI] [PubMed] [Google Scholar]
- Coe NB, Guo J, Konetzka RT, and Van Houtven CH (2019). ‘What is the marginal benefit of payment-induced family care? Impact on Medicaid spending and health of care recipients.’ Health Economics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe NB, Skira MM, and Larson EB (2018). ‘A Comprehensive Measure of the Costs of Caring for a Parent: Differences According to Functional Status.’ Journal of the American Geriatrics Society, vol. 66(10): 2003–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe NB and Van Houtven CH (2009). ‘Caring for mom and neglecting yourself? The health effects of caring for an elderly parent.’ Health Economics, vol. 18(9): 991–1010. [DOI] [PubMed] [Google Scholar]
- Coile CC, Levine PB, and McKnight R. (2014). ‘Recessions, older workers, and longevity: How long are recessions good for your health?’ American Economic Journal: Economic Policy, vol. 6(3): 92–119. [Google Scholar]
- Collier E. and Harrington C. (2008). ‘Staffing characteristics, turnover rates, and quality of resident care in nursing facilities.’ Research in gerontological nursing, vol. 1(3): 157–170. [DOI] [PubMed] [Google Scholar]
- Costa-Font J, Karlsson M, and Øien H. (2016). ‘Careful in the Crisis? Determinants of Older People’s Informal Care Receipt in Crisis-Struck European Countries.’ Health Economics, vol. 25(S2): 25–42. [DOI] [PubMed] [Google Scholar]
- Ettner S. (1996). ‘The opportunity costs of elder care.’ Journal of Human Resources, vol. 31(1): 189–205. [Google Scholar]
- Fadlon I. and Nielsen TH (2017). ‘Family Labor Supply Responses to Severe Health Shocks’ Tech. rep, National Bureau of Economic Research. [Google Scholar]
- Fahle SP and McGarry KM (2017). ‘Caregiving and Work: The Relationship between Labor Market Attachment and Parental Caregiving.’ Working paper. [Google Scholar]
- Family Caregiver Alliance (2015). ‘Selected Long-Term Care Statistics.’ https://www.caregiver.org/selected-long-term-care-statistics. Accessed: 2018-01-29. [Google Scholar]
- Genworth (2018). ‘Cost of Care Survey 2018.’ https://www.genworth.com/aging-and-you/finances/cost-of-care.html. Accessed: 2019-02-22. [Google Scholar]
- Goda GS, Golberstein E, and Grabowski DC (2011). ‘Income and the utilization of long-term care services: Evidence from the Social Security benefit notch.’ Journal of Health Economics, vol. 30(4): 719–729. [DOI] [PubMed] [Google Scholar]
- Grabowski DC and Gruber J. (2007). ‘Moral hazard in nursing home use.’ Journal of Health Economics, vol. 26(3): 560–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guryan J, Hurst E, and Kearney M. (2008). ‘Parental education and parental time with children.’ Journal of Economic Perspectives, vol. 22(3): 23–46. [Google Scholar]
- Hagen SA (2013). Rising demand for long-term services and supports for elderly people. Congressional Budget Office. [Google Scholar]
- He D. and McHenry P. (2016). ‘Does formal employment reduce informal caregiving?’ Health Economics, vol. 25(7): 829–843. [DOI] [PubMed] [Google Scholar]
- Heitmueller A. (2007). ‘The chicken or the egg?: Endogeneity in labour market participation of informal carers in England.’ Journal of Health Economics, vol. 26(3): 536–559. [DOI] [PubMed] [Google Scholar]
- Houser A, Fox-Grange W, and Ujvari K. (2015). ‘Across The States: Profiles of Long-Term Care Services and Supports’ Tech. rep, AARP. [Google Scholar]
- Hoynes H, Miller DL, and Schaller J. (2012). ‘Who suffers during recessions?’ The Journal of Economic Perspectives, vol. 26(3): 27–47. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured (2015). ‘Medicaid and Long-Term Care Services and Supports: A Primer.’ Technical report. [Google Scholar]
- Kimmel J. and Connelly R. (2007). ‘Mothers’ time choices caregiving, leisure, home production, and paid work.’ Journal of Human Resources, vol. 42(3): 643–681. [Google Scholar]
- Konetzka RT, Lasater KB, Norton EC, and Werner RM (2018). ‘Are Recessions Good for Staffing in Nursing Homes?’ American Journal of Health Economics, vol. 4(4): 411–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H. (2014). ‘Revisiting the relationship between nurse staffing and quality of care in nursing homes: An instrumental variables approach.’ Journal of Health Economics, vol. 37: 13–24. [DOI] [PubMed] [Google Scholar]
- Maestas N. and Truskinovsky Y. (2018). ‘Caregiving and Labor Force Participation: New Evidence from the Time Use Survey.’ Working paper. [Google Scholar]
- Mclnerney M. and Mellor JM (2012). ‘Recessions and seniors’ health, health behaviors, and healthcare use: Analysis of the Medicare Current Beneficiary Survey.’ Journal of Health Economics, vol. 31(5): 744–751. [DOI] [PubMed] [Google Scholar]
- McKernan S-M, Ratcliffe C, Steuerle E, and Zhang S. (2014). ‘Disparities in wealth accumulation and loss from the great recession and beyond.’ American Economic Review, vol. 104(5): 240–44. [Google Scholar]
- Mommaerts C. (2016). ‘Long-Term Care Insurance and the Family.’ Working paper. [Google Scholar]
- Mommaerts C. (2018). ‘Are coresidence and nursing homes substitutes? Evidence from Medicaid spend-down provisions.’ Journal of Health Economics, vol. 59: 125–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers S. and Komisar H. (2003). ‘Who needs long-term care? Fact Sheet’ Long-Term Care Financing Project. Washington, DC: Georgetown University Press. [Google Scholar]
- Ruhm CJ (2000). ‘Are recessions good for your health?’ The Quarterly Journal of Economics, vol. 115(2): 617–650. [Google Scholar]
- Ruhm CJ (2012). ‘Understanding the relationship between macroeconomic conditions and health.’ The Elgar Companion to Health Economics, vol. 1. [Google Scholar]
- Ruhm CJ (2015). ‘Recessions, healthy no more?’ Journal of Health Economics, vol. 42: 17–28. [DOI] [PubMed] [Google Scholar]
- Skira MM (2015). ‘Dynamic wage and employment effects of elder parent care.’ International Economic Review, vol. 56(1): 63–93. [Google Scholar]
- Stevens AH, Miller DL, Page ME, and Filipski M. (2015). ‘The best of times, the worst of times: understanding pro-cyclical mortality.’ American Economic Journal: Economic Policy, vol. 7(4): 279–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai Y. (2015). ‘Social security income and the utilization of home care: Evidence from the Social Security notch.’ Journal of Health Economics, vol. 43: 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven CH, Coe NB, and Skira MM (2013). ‘The effect of informal care on work and wages.’ Journal of Health Economics, vol. 32(1): 240–252. [DOI] [PubMed] [Google Scholar]
- Van Houtven CH and Norton EC (2004). ‘Informal care and health care use of older adults.’ Journal of Health Economics, vol. 23(6): 1159–1180. [DOI] [PubMed] [Google Scholar]
- Van Houtven CH and Norton EC (2008). ‘Informal care and Medicare expenditures: Testing for heterogeneous treatment effects.’ Journal Of Health Economics, vol. 27(1): 134–156. [DOI] [PubMed] [Google Scholar]