Abstract
An 18-year-old woman with annular pancreas and duodenal duplication presented with recurrent acute pancreatitis and underwent a resection of duodenal duplication. However, the patient experienced recurrent abdominal pain after resection. Abdominal computed tomography and magnetic resonance imaging showed a dilatation of the peripheral pancreatic duct and stenosis and malformation of both the Wirsung's and Santorini's duct due to multiple stones. The modified puestow procedure was performed. The main pancreatic ducts in the body and tail were opened, and the intrapancreatic common bile duct was preserved. A Roux-en-Y pancreatico-jejunostomy was performed for reconstructing the pancreaticobiliary system after removing the ductal protein plug. The patient experienced no abdominal pain, no significant elevation of the serum amylase and lipase levels, and no stone formation during the 2 years of follow-up. This procedure is considered to be beneficial for pediatric patients with chronic pancreatitis due to annular pancreas and duodenal duplication.
Keywords: Modified puestow procedure, Lateral pancreatico-jejunostomy, Chronic pancreatitis, Recurrent abdominal pain, Duodenal duplication, Annular pancreas
INTRODUCTION
Chronic pancreatitis is rare in children. It causes progressive and irreversible destruction of the pancreas, resulting in both pancreatic exocrine and endocrine dysfunctions [1,2]. It is commonly unresponsive to conservative therapy. It causes severe disabling pain leading to analgesic addiction, dietary restrictions, school absences, and retardation of growth and development. Such morbidities warrant surgical interventions [1,2,3].
Since a variety of anatomical configurations may cause chronic pancreatitis, administration of the appropriate procedure requires accurate determination of the pancreatic anatomical structure [4,5]. Here, we report the case of a woman with chronic pancreatitis due to duodenal duplication and annular pancreas that was managed by the modified puestow procedure (MPP). Despite previous complete resection of duodenal duplication, impaired pancreatic juice flow led to stone formation and recurrent abdominal pain. Therefore, MPP with a longitudinal pancreatico-jejunostomy in the pancreatic head and body without coring of the pancreas's head was performed due to the annular pancreas, and it provided an excellent decompression of the pancreatic head.
CASE REPORT
An 18-year-old woman with recurrent acute pancreatitis presented with abdominal pain. Conservative treatment including antibiotics and dietary restrictions yielded no improvement. The patient had a history of intestinal malrotation and underwent Ladd procedure and appendectomy at 7 years of age. History of abdominal trauma, metabolic abnormality associated with pancreatitis, and family history of pancreatitis were denied.
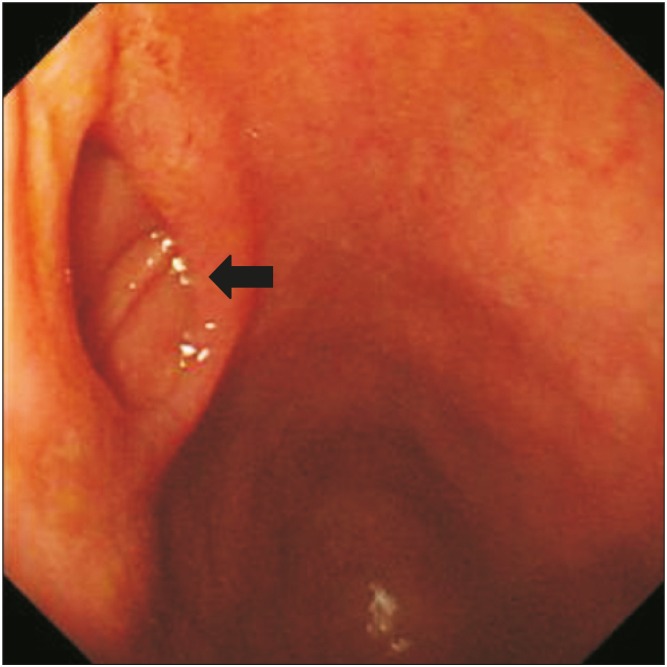
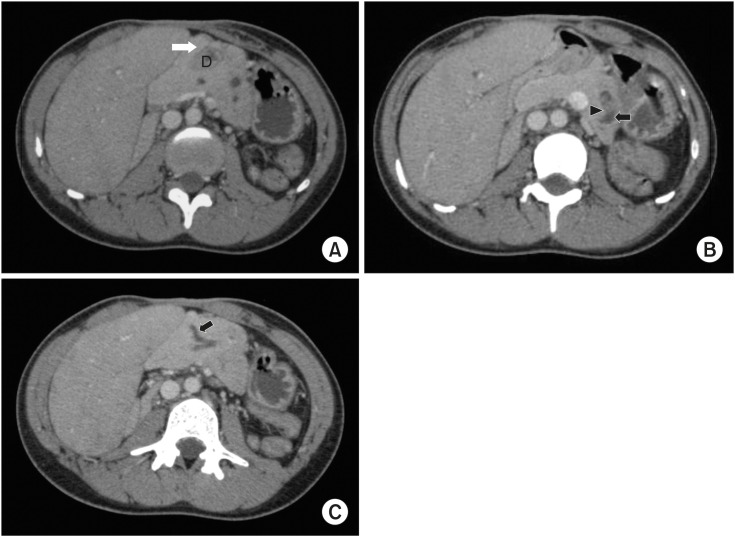
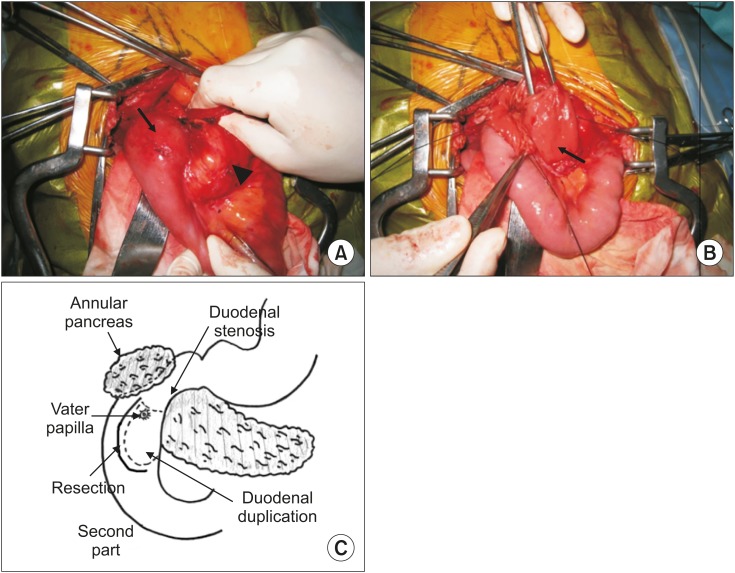
The initial laboratory findings revealed an elevation in pancreatic amylase (63–170 IU/L) and lipase (55–253 U/L). Other biochemical and tumor markers were unremarkable. Anti-nuclear antibody and anti-dsDNA antibody were negative. Endoscopic retrograde cholangiopancreatography could not be performed due to duodenal stenosis. Contrast study showed duodenal stenosis with duodenal duplication in the second portion, and this was confirmed by upper gastrointestinal endoscopy (Fig. 1). Abdominal computed tomography (CT) revealed annular pancreas, enlargement of the pancreatic duct (diameter 7.2 mm) with multiple defects, and intestinal malrotation (Fig. 2). Duodenal stenosis at the level of the Vater's papilla due to duodenal duplication along with annular pancreas was thought to be the cause of recurrent pancreatitis. She first underwent duodenal duplication resection. The operation revealed the annular pancreas to be an incomplete ring surrounding the lateral and posterior part of the duodenum (Fig. 3). In addition, intraoperative cholangiography showed dilatation of the pancreatic duct (figure not shown).
Fig. 1. Upper gastrointestinal endoscopy: Duodenal duplication was found in the second part of the duodenum (arrow).
Fig. 2. Abdominal computed tomography showed an annular pancreas with enlargement of the pancreatic duct. (A) Annular pancreas (white arrow) surrounding the duodenum (D); (B) Main pancreatic duct dilatation (arrow) with stones inside the dilatation area (arrow head); (C) Santorini's duct dilatation (arrow).
Fig. 3. Surgical findings in the first operation: An annular pancreas (arrow head) surrounding the lateral and posterior of duodenum; arrow indicates duodenal duplication (A); opening the anterior wall of the second duodenal portion revealed a duodenal duplication (arrow) (B); surgical findings including the position of the duodenal stenosis are illustrated in (C).
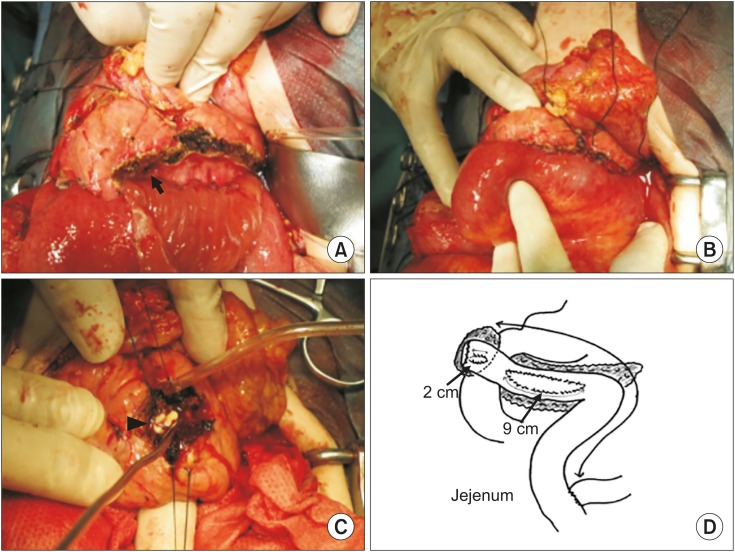
Following duodenal duplication resection, she experienced occasional recurrent abdominal pain. The serum lipase and amylase levels were 90–601 U/L and 144–481 U/L, respectively. Abdominal CT and magnetic resonance imaging showed peripheral pancreatic duct dilatation (diameter 9.2 mm) and stenosis. Multiple defects were found both in the Wirsung's duct and Santorini's ducts in the pancreatic head. MPP was chosen considering the complicated anatomy of the pancreaticobiliary system. Guided by ultrasonography, two separate longitudinal excisions were made to open the main pancreatic duct, about 9 cm and 2 cm in the body and tail, respectively. The intrapancreatic common bile duct was preserved. The spleen or distal part of the pancreas was not resected. Reconstruction of the pancreatobiliary system by Roux-en-Y pancreatico-jejunostomy was performed, followed by the removal of the ductal protein plug (Fig. 4). Histological examination showed mild fibrosis and a well-preserved islet and exocrine cells, with no specific inflammation or malignancy. The postoperative course was uneventful. She experienced no abdominal pain during 2 years of follow-up. Blood sugar and HbA1c were maintained within normal limits, with only slight elevation in the amylase and lipase levels. Follow-up abdominal CT showed mild pancreatic duct dilatation without any stone formation.
Fig. 4. Modified puestow procedure: (A) Longitudinal incision of the pancreatic duct; arrow head indicates Vater's papilla (B) Roex-en-Y reconstruction: anastomosis of the jejunum to the pancreas (C) Multiple pancreatic protein plugs (arrow head) in the pancreatic duct (D) Illustration of the operation.
DISCUSSION
A duodenal duplication is typically located at or near the duodenal papilla. The common bile and pancreatic ducts sometimes terminate in the wall of the duodenal duplication. Food residue may obstruct the pancreatic duct orifice resulting in pancreatitis [6]. It was unclear whether annular pancreas alone or in combination with duodenal duplication caused pancreatitis in our patient. The duodenal duplication located in front of the Vater's papilla was thought to have caused an obstruction which impaired the pancreatic juice flow. Food impaction formed a protein plug at the Vater's papilla causing pancreatic duct dilation. In our case, pancreatic duct dilation led to chronic pancreatitis with pancreatic plug formation. Recurrent acute pancreatitis episodes rendered the dilation irreversible.
Congenital duodenal duplication often causes duodenal obstruction; however, associated acute pancreatitis is very rare and has no standardized treatment. Previously, a case of acute pancreatitis due to duodenal duplication reported symptoms resolution following complete resection of duodenal duplication [6]. In our case, the initial resection of duodenal duplication failed to resolve the condition. In contrast, a report of duodenal atresia associated with chronic pancreatitis in a 2-year-old boy was successfully managed by Frey procedure [5]. We decided to perform MPP in our patient. This involved side-to-side anastomosis between the jejunal longitudinal opening and the longitudinally opened main pancreatic duct, while preserving the pancreatic gland in the body and tail. Unlike the previous Puestow procedure which requires distal pancreatectomy and splenectomy in addition to the longitudinal opening of the pancreatic duct, MPP conserves distal pancreas and spleen [7,8,9]. Due to the annular pancreas, we performed modified MPP.
The surgical procedures applied for treating chronic pancreatitis include the Puestow, Duval, Beger, and Frey procedures. The Frey procedure combines longitudinal pancreatico-jejunostomy and coring out of the pancreatic head, and it provides a good postoperative clinical course with zero mortality and low morbidity [10]. MPP is less invasive than the Frey procedure and involves a single anastomosis with no coring out of the pancreatic duct. In addition, studies comparing several procedures preferred MPP as a mainstay treatment for children with chronic pancreatitis. MPP is less invasive, has lower morbidity, and is considerably safer than other procedures. Moreover, it has been shown to increase the percentile body weight. In addition, it is cost effective and decreases length of hospital stay [3,11,12]. Thus, we performed MPP with a good postoperative outcome.
Our patient had no abdominal pain throughout the 2 years of follow-up. She had a normal blood sugar profile. There was no significant elevation in pancreatic enzymes, only mild pancreatic duct dilation, and no stones. Moreover, similar postoperative improvement of pancreatic function following MPP has been reported previously. These findings indicate that the MPP is effective for pediatric patients with chronic pancreatitis, even when the symptoms are caused by an annular pancreas and duodenal duplication.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Wang W, Liao Z, Li ZS, Shi XG, Wang LW, Liu F, et al. Chronic pancreatitis in Chinese children: etiology, clinical presentation and imaging diagnosis. J Gastroenterol Hepatol. 2009;24:1862–1868. doi: 10.1111/j.1440-1746.2009.05967.x. [DOI] [PubMed] [Google Scholar]
- 2.Rollins MD, Meyers RL. Frey procedure for surgical management of chronic pancreatitis in children. J Pediatr Surg. 2004;39:817–820. doi: 10.1016/j.jpedsurg.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 3.Clifton MS, Pelayo JC, Cortes RA, Grethel EJ, Wagner AJ, Lee H, et al. Surgical treatment of childhood recurrent pancreatitis. J Pediatr Surg. 2007;42:1203–1207. doi: 10.1016/j.jpedsurg.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Neblett WW, 3rd, O'Neill JA., Jr Surgical management of recurrent pancreatitis in children with pancreas divisum. Ann Surg. 2000;231:899–908. doi: 10.1097/00000658-200006000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okuyama H, Kubota A, Kawahara H, Shimizu Y, Watanabe T, Yamanaka H, et al. Frey procedure for chronic pancreatitis in a child with duodenal atresia and complex pancreaticobiliary disorders. Eur J Pediatr Surg. 2010;20:45–47. doi: 10.1055/s-0029-1202249. [DOI] [PubMed] [Google Scholar]
- 6.Alizai NK, Puntis JW, Stringer MD. Duodenal web presenting with acute pancreatitis. J Pediatr Surg. 1997;32:1255–1256. doi: 10.1016/s0022-3468(97)90696-5. [DOI] [PubMed] [Google Scholar]
- 7.O'Neil SJ, Aranha GV. Lateral pancreaticojejunostomy for chronic pancreatitis. World J Surg. 2003;27:1196–1202. doi: 10.1007/s00268-003-7238-7. [DOI] [PubMed] [Google Scholar]
- 8.Crombleholme TM, deLorimier AA, Way LW, Adzick NS, Longaker MT, Harrison MR. The modified Puestow procedure for chronic relapsing pancreatitis in children. J Pediatr Surg. 1990;25:749–754. doi: 10.1016/s0022-3468(05)80011-9. [DOI] [PubMed] [Google Scholar]
- 9.Ceppa EP, Pappas TN. Modified puestow lateral pancreaticojejunostomy. J Gastrointest Surg. 2009;13:1004–1008. doi: 10.1007/s11605-008-0590-z. [DOI] [PubMed] [Google Scholar]
- 10.Egawa S, Motoi F, Sakata N, Kitamura Y, Nakagawa K, Ohtsuka H, et al. Assessment of Frey procedures: Japanese experience. J Hepatobiliary Pancreat Sci. 2010;17:745–751. doi: 10.1007/s00534-009-0185-4. [DOI] [PubMed] [Google Scholar]
- 11.Chiu B, Lopoo J, Superina RA. Longitudinal pancreaticojejunostomy and selective biliary diversion for chronic pancreatitis in children. J Pediatr Surg. 2006;41:946–949. doi: 10.1016/j.jpedsurg.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 12.DuBay D, Sandler A, Kimura K, Bishop W, Eimen M, Soper R. The modified Puestow procedure for complicated hereditary pancreatitis in children. J Pediatr Surg. 2000;35:343–348. doi: 10.1016/s0022-3468(00)90037-x. [DOI] [PubMed] [Google Scholar]